Abstract
Therapy with bronchodilators forms the pharmacologic foundation of the treatment of patients with COPD. Bronchodilators can significantly lessen dyspnea, increase airflow, improve quality of life, and enhance exercise performance. While bronchodilators decrease airway resistance and lessen dynamic hyperinflation in patients with COPD, they have not been shown to alter the rate of decline in FEV1 over time, or improve patient survival. Fairly recently, a long-acting, once-daily anticholinergic medication, tiotropium bromide, has been developed which may improve symptom management in COPD patients. This paper reviews anticholinergic pharmacologic therapy for patients with COPD focusing on tiotropium bromide, and discusses treatment strategies based on disease stage. It is important to recognize that while bronchodilators improve symptoms, a multimodality treatment approach including respiratory and rehabilitative therapy, nutrition services, psychosocial counseling, and surgical care, is often necessary for the best possible care of patients with COPD.
Introduction
Chronic obstructive pulmonary disease (COPD) is an enormous health threat that currently ranks as the fourth leading cause of morbidity and mortality in the US (CitationNational Heart, Lung, and Blood Institute 1998), and is the only major disease with increasing mortality (CitationBenson and Marano 1998; CitationCenters for Disease Control and Prevention 1999). In the year 2000, COPD accounted for over 1.5 million visits to emergency departments in the US (CitationMannino et al. 2002). The prevalence of COPD is also exploding internationally. By the year 2020, the World Bank and the World Health Organization project that COPD will rank fifth as a cause of worldwide disability (CitationMurray and Lopez 1997a, Citation1997b, Citation1997c). Given the increasing patient population, there has been a great push to develop medications that will appreciably affect the care of patients with this devastating and costly disease (CitationCroxton et al 2003).
Anticholinergic medications are a class of drugs that have long been used to improve symptomatology of patients with COPD (CitationGross 1988; CitationDollery 1991; CitationBauer 1992). A new inhaled anticholinergic medication, tiotropium bromide (Boehringer Ingelheim, Ingelheim, Germany), is now being used in this patient population. This medication appears to be more effective in treating patients with COPD compared with older anticholinergics. This review will discuss the pharmacology of anticholinergic bronchodilators focusing on tiotropium bromide, and discuss treatment strategies based on disease stage.
Methods
A Cochrane Database and MEDLINE search from 1966 to October 2005, and a search of the PubMed database using the terms COPD, emphysema, tiotropium, anticholinergic, and autonomic nervous system was performed. Bibliographies of identified articles were then reviewed for further references. Non-English, and non-human studies were excluded. Bibliographies of review articles were examined and original research was then systematically evaluated.
Pharmacology of the autonomic nervous system
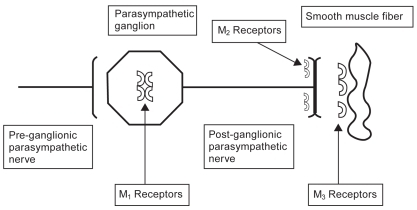
The autonomic nervous system through cholinergic nerve fibers is responsible for mediating mucus secretion and bronchial smooth muscle tone in the lung. Branches of the vagus nerve innervate muscarinic cholinergic (M) receptors in parasympathetic ganglia in the lung using acetylcholine as the primary neurotransmitter. No less than 5 muscarinic cholinergic receptor subtypes (M1–M5) have been identified in the lung. M1 and M3 mediate bronchoconstriction and mucus production. M2 is a presynaptic postganglionic autoreceptor in small airways that inhibits the M1 and M3 receptors via negative feedback mechanisms (). Stimulation of the M2 receptor inhibits cholinergic action in the lung, so agonism of this receptor leads to inhibition of bronchoconstriction. At this time, the M4 and M5 receptors have poorly understood function in the lung (CitationMak et al 1993; CitationBarnes 1993a, Citation1993b; CitationBarnes et al. 1997; CitationZuWallack 2004).
Figure 1 Pulmonary muscarinic cholinergic receptors. M1 and M3 receptors mediate bronchoconstriction and mucus production in the lung. M2 receptors inhibit M1 and M3 receptors via negative feedback. Ipratropium inhibits all three muscarinic receptors. Tiotropium quickly dissociates from the M2 receptor but continues to antagonize the M1 and M3 receptor. Thus, tiotropium blocks bronchoconstriction and allows inhibition of bronchoconstriction to continue. The slow dissociation of tiotropium from the M1 and M3 receptors accounts for its long half-life.
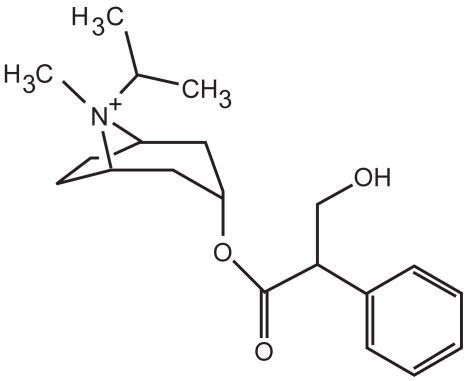
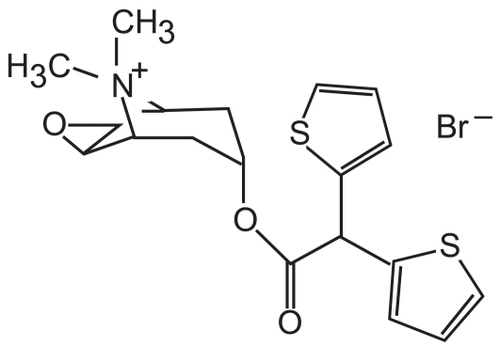
Older anticholinergic medications, such as ipratropium (), block the M1, M2, and M3 receptors. Specifically, these medications decrease the bronchoconstrictive action of the M1 and M3 receptors, but also block the inhibitory action of the M2 receptor. Ipratropium then dissociates fairly quickly from these receptors. Thus, ipratropium is a weak bronchodilator because of its relatively short half-life compared with newer anticholinergics, and because of its inhibitory action on the M2 receptor. A new anticholinergic called tiotropium bromide () has been developed which also antagonizes M1, M2, and M3 receptors. However, tiotropium quickly dissociates from the M2 receptor, and thus its net effect is that of a selective M1 and M3 antagonist. Tiotropium, therefore, blocks the bronchoconstrictive action of the M1 and M3 muscarinic receptors while allowing M2 inhibition of bronchoconstriction to continue. Slow dissociation of tiotropium from the M1 and M3 receptors accounts for its long half-life.
Anticholinergic medications
Ipratropium
Anticholinergic medications () are some of the most common medications used in the treatment of COPD and have been used safely for decades (CitationAnthonisen et al 1994). They are available for delivery by both metered dose inhaler and nebulizer. Their duration of action varies between 4 and 36 hours. Most anticholinergics, such as ipratropium, are quaternary ammonium derivatives that have difficulty crossing the blood–brain barrier and are poorly absorbed in the body (CitationFerguson 2000). The quaternary ammonium structure likely enhances their efficacy and minimizes the side-effects that beleaguer β-agonists. These medications have been shown to diminish the sense of dyspnea, and mucus hypersecretion via their inhibition of the cholinergic system (CitationGhafouri et al 1984). Anticholinergics have also been shown to improve oxyhemoglobin saturation with sleep (CitationMartin et al 1999; CitationMcNicholas et al 2004), and provide similar, or greater, bronchodilation compared with β2-agonists (CitationKarpel 1991; CitationCOMBIVENT Inhalation Aerosol Study Group 1994; CitationRennard et al 1996). Data suggest that in some patients who have COPD, ipratropium may be effective when β2-agonists are not effective (CitationBraun and Levy 1991). Anticholinergics have a reasonable safety profile, and are not prone to receptor downregulation or tachyphylaxis (CitationRennard et al 1996). However, these medications may be associated with an increased number of adverse cardiovascular events in patients with COPD (CitationAnthonisen et al 2002).
Table 1 Anticholinergics used in the management of COPD
Combining ipratropium with long-acting β2-agonists may also have additive benefits for patients. CitationVan Noord et al (2000) studied salmeterol compared with salmeterol plus ipratropium. The study found that both salmeterol alone or in combination with ipratropium improved bronchodilation compared with placebo, but the combination of the medications appeared to elicit a greater bronchodilator response and improvement in FEV1 than salmeterol alone. CitationDorinsky et al (1999) found that the combination of ipratropium and albuterol was superior to either medication alone in identifying patients with reversibility on spirometric testing of pulmonary function.
Tiotropium
Tiotropium, with its extremely long duration of action, avoids one of the main limitations of first-generation anticholinergic medications – the necessity of frequent dosing. CitationCasaburi et al (2002) showed that once-daily tiotropium, compared with placebo, improved bronchodilation, dyspnea scores, health status scores, and decreased COPD exacerbations and hospitalizations. The primary adverse side-effect observed in the study was dry mouth. In a fairly short 12-week study in patients with COPD, tiotropium was shown to provide a higher post-dose FEV1, and higher peak and FVC, compared with salmeterol (CitationBriggs et al 2005). In a 6-month study of tiotropium compared with salmeterol, tiotropium produced a greater degree of bronchodilation, reduction in dyspnea scores, and improvement in health-related quality of life (CitationDonohue 2002). In a longer 1-year study, CitationVincken et al (2002) demonstrated diminished salbutamol use and improvement in peak expiratory flow rates. Compared with ipratropium, tiotropium appeared to reduce the number of exacerbations, increase the time to a first exacerbation, and increase the time to first hospitalization in patients with COPD. Quality of life scores were also improved. More recently, a randomized, placebo-controlled study of tiotropium in mostly male veterans with COPD showed a decrease in exacerbation rate compared with placebo. While the effect was small, it was statistically significant (CitationNiewoehner et al 2005). At this time, it is not known whether this effect would also be seen in women.
Anticholinergics and exercise tolerance
Numerous studies have demonstrated improvements in exercise tolerance in patients with COPD with the use of anticholinergic medications (CitationSpence et al 1993). CitationHay et al (1992) studied the use of oxitropium in patients with COPD. The study showed significant improvements in breathlessness and walking distance, and an increased FEV1 with its use. Improvements in walking distances and symptoms were unrelated to changes in either FEV1 or FVC, which may suggest that routine reversibility testing is not a good predictor of symptomatic benefit in patients with COPD.
CitationTsukino et al (1998) investigated the combined effect of theophylline with ipratropium. The study found that both ipratropium and theophylline improved exercise tolerance but combination therapy with the two medications produced greater improvements in pulmonary function and exercise capacity than either drug alone. In this study the average serum theophylline levels were around 18.3 μg/mL, which increases the risk of adverse side-effects.
CitationCasaburi et al (2005) showed that the combination of tiotropium in combination with pulmonary rehabilitation improved treadmill endurance and reduced dyspnea scores compared with rehabilitation alone. These effects seemed to be sustained for at least 3 months after the rehabilitation course was completed. CitationMaltais et al (2005) demonstrated that tiotropium improved symptom-limited exercise tolerance compared with placebo in COPD patients up to 8 hours following dosing.
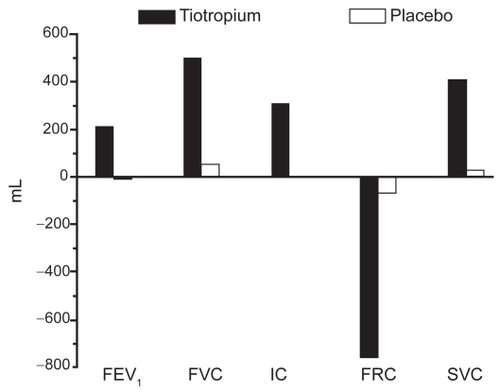
Tiotropium also appears to reduce lung hyperinflation at rest and during exertion (CitationCelli et al 2003; CitationMaltais et al 2005). This may be an important effect as dynamic hyperinflation likely contributes to the sense of dyspnea that often limits exercise in COPD patients (CitationO’Donnell et al 1998; CitationTaube et al 2000). Following 4 weeks of therapy, tiotropium clearly improves lung volumes compared with placebo () (CitationCelli et al 2003).
Figure 4 Tiotropium improves lung volumes compared with placebo. Reproduced from CitationCelli B, ZuWallack R, Wang S, et al. 2003. Improvement in resting inspiratory capacity and hyperinflation with tiotropium in COPD patients with increased static lung volumes. Chest, 124:1743–8. Copyright © 2003, with permission from CHEST.
Recently, combination therapies using tiotropium have been shown to be beneficial in the treatment of patients with COPD. Citationvan Noord et al (2005) have demonstrated that tiotropium produces a greater improvement in daytime FEV1 than formoterol. Interestingly, night-time change in FEV1 was not different between the two medications. However, combination therapy with the two medications (with daily dosing) improved FEV1 to the greatest extent. While combination therapy appears to be a trend in caring for patients with more advanced disease, it is important to recognize that individual and combination pharmacologic medications are expensive, add significantly to the cost of healthcare, and have not been found to alter the overall decline in lung function seen in patients with COPD. Additional studies will be necessary to determine the best combination(s) of bronchodilators in the treatment of patients with COPD.
The staging of COPD
Various respiratory societies, including the American Thoracic Society (ATS) and the European Respiratory Society (ERS), have developed staging systems to help identify patients at risk for COPD and to aid in standardization of therapies and clinical trials. The ATS guidelines for staging COPD are shown in (CitationATS 1995). “Stage 0” disease describes a smoker with normal spirometry who has symptoms of chronic mucus production or cough. “Stage I” or “Mild COPD” describes the patient with objective spirometric evidence of airflow obstruction. Their FEV1/FVC ratio is < 70%, and their post-bronchodilator FEV1 is ≥ 80% of predicted. They may or may not have symptoms of airflow obstruction, chronic bronchitis, or dyspnea. “Stage II” or “Moderate COPD” is characterized by typical symptoms, airflow obstruction with the FEV1/FVC ratio < 70%, and the FEV1 between 30% and 80% of predicted. It is considered “IIA” disease if the FEV1 is ≥ 50% of predicted, and “IIB” disease if the FEV1 falls between 30% and 50% of predicted. “Stage III” or “Severe COPD” is characterized by appropriate symptomatology, a FEV1/FVC ratio < 70%, and a FEV1 < 30% of predicted. Evidence of respiratory failure or cor pulmonale, with a FEV1 < 50% of predicted, is also consistent with “Severe” disease.
Table 2 Stages of COPD
Treatment according to disease stage
Spirometry should be used to help identify and stage patients with COPD as their treatment is often predicated upon disease stage () (CitationLipson 2004). However, following stable patients with multiple repeat spirometric tests may not be useful (CitationWilt et al 2005). “At risk” patients must refrain from cigarette smoking, and should obtain annual influenza vaccination and should be vaccinated with the pneumococcal vaccine every 5 years. Bronchodilator therapy on an “as needed” basis with short-acting bronchodilators may be used for managing mild COPD patients (CitationVathenen et al 1988).
Figure 5 Treatment of COPD by stage. Reproduced from CitationLipson DA. 2004. Redefining treatment in COPD: new directions in bronchodilator therapy. Treat Respir Med, 3:89–95. Erratum in Treat Respir Med, 3:181. Copyright © 2004, with permission from Adis International Ltd.
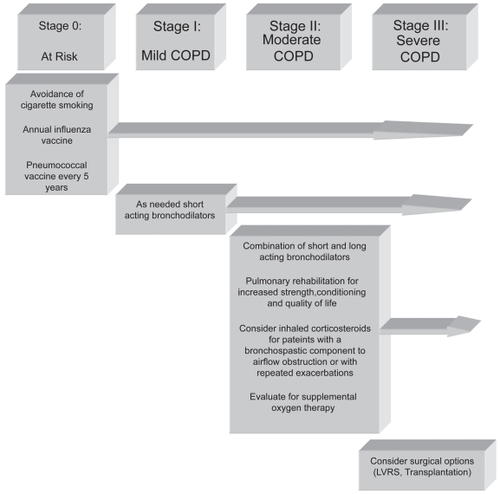
A combination of short- and long-acting bronchodilators is often used to treat moderate emphysema. Inhaled anticholinergic medications and combinations of short- and long-acting β2-agonists are standard treatments. Inhaled corticosteroids may be useful for patients with more severe disease, or those patients with a partially reversible, bronchospastic component to airflow obstruction. These medications may also be useful in patients who have repeated exacerbations (CitationBurge et al 2000; CitationThe Lung Health Study Research Group 2000; CitationSin and Tu 2001; CitationHattotuwa et al 2002). Medications combining an inhaled steroid and a long-acting β-agonist, such as fluticasone and salmeterol, may also be useful in this patient population (CitationMahler et al 2002).
Pulmonary rehabilitation is an important addition to pharmacologic therapy in patients with COPD because severe dyspnea leads to a sedentary lifestyle, subsequent deconditioning, and muscle weakness (CitationACCP/AACVPR Pulmonary Rehabilitation Guidelines Panel 1997). Pulmonary rehabilitation increases strength, quality of life, sense of well-being, and exercise tolerance. It is also useful in breaking the vicious cycle of progressive debilitation in patients with advanced lung disease (CitationFishman 1994; CitationCelli 1997; CitationATS 1999).
All patients with moderate COPD should be evaluated for the need for supplemental oxygen. Patients who exhibit oxyhemoglobin desaturation at rest, or with exertion, should be prescribed supplemental oxygen to maintain oxyhemoglobin saturations greater than 90%. Long-term oxygen therapy, in COPD patients who require it, has been shown to improve survival, exercise tolerance, and quality of life (CitationNocturnal Oxygen Therapy Trial Group 1980; CitationMedical Research Council Working Party 1981; CitationTarp and Celli 1995). A patient requires supplemental oxygen if they demonstrate an oxyhemoglobin saturation ≤ 88% or a PaO2 ≤ 55 mmHg. Additionally, an oxyhemoglobin saturation < 89% or a PaO2 < 60 mmHg also qualifies a patient for supplemental oxygen if there is evidence of cor pulmonale, a hematocrit > 56%, dependent edema, or other signs suggestive of heart failure.
The treatment of severe COPD is equivalent to that of moderate disease, except patients in this stage should also be evaluated for potential surgical treatments such as lung volume reduction surgery or lung transplantation (CitationCooper et al 1996; CitationSciurba et al 1996; CitationArcasoy and Kotloff 1999; CitationCriner et al 1999; CitationGeddes et al 2000; CitationFlaherty et al 2001; CitationKotloff et al 2001; CitationNational Emphysema Treatment Trial Research Group 2001, Citation2003).
Conclusions
Anticholinergic medications are safe and useful adjuncts in the care of patients with COPD. While they have not been shown to alter the rate of decline in the FEV1, or alter survival, they improve exercise tolerance, dynamic hyperinflation, and breathlessness. These medications improve quality of life measures and reduce the risk of exacerbation (CitationBarr et al 2005). Newer anticholinergics, such as tiotropium, have the added advantage of once-daily dosing and more specific cholinergic receptor targets.
Clearly, the best treatment of COPD remains smoking cessation and abstinence from smoking. Evaluation and care of the patient with COPD must include respiratory and rehabilitative therapy, nutrition services, psychosocial counseling, and evaluation for the need for long-term oxygen therapy. Physicians, and persons charged with caring for patients with COPD, await the development of novel therapies that will further improve survival, and the quality of the lives of patients with lung disease.
Disclosures
Grant Support: NIH K23 HL04486. The author has no conflict of interest to declare.
References
- ACCP/AACVPR Pulmonary Rehabilitation Guidelines Panel1997Pulmonary rehabilitation: Joint ACCP/AACVPR evidence-based guidelinesChest1121363969367481
- [ATS] American Thoracic Society1995Statement: Standards for the diagnosis and care of patients with chronic obstructive pulmonary diseaseAm J Respir Care Med152Suppl77121
- [ATS] American Thoracic Society1999Official Statement: Pulmonary rehabilitation-1999Am J Respir Crit Care Med15916668210228143
- AnthonisenNRConnettJEKileyJP1994Effects of smoking intervention and the use of an inhaled anticholinergic bronchodilator on the rate of decline of FEV1. The Lung Health StudyJAMA27214975057966841
- AnthonisenNRConnettJEEnrightPL2002Lung Health Study Research Group. Hospitalizations and mortality in the Lung Health StudyAm J Respir Crit Care Med166333912153966
- ArcasoySMKotloffRM1999Medical progress: lung transplantationN Engl J Med34010819110194239
- BarnesPJMuscarinic receptor subtypes in airways1993aEur Resp J632831
- BarnesPJMuscarinic receptor subtypes in airways1993bLife Sci5252178441331
- BarnesPJHaddadEBRousellJ1997Regulation of muscarinic M2 receptorsLife Sci601015219121342
- BarrRGBourbeauJCamargoCA2005Tiotropium for stable chronic obstructive pulmonary diseaseThe Cochrane Database of Systematic Reviews2 Art. No. CD002876.pub210.1002/14651858.CD002876.pub2.
- BauerR1992The pharmacology of oxitropium bromideRev Contemp Pharmacother3197203
- BensonVMaranoMA1998Current estimates from the National Health Interview Survey, 1995Vital Health Stat 1019914289914773
- BraunSRLevySF1991Comparison of ipratropium bromide and albuterol in chronic obstructive pulmonary disease: a three-center studyAm J Med91S2832
- BriggsDDJrCovelliHLapidusR2005Improved daytime spirometric efficacy of tiotropium compared with salmeterol in patients with COPDPulm Pharmacol Ther1839740416179215
- BurgePSCalverleyPMJonesPW2000Randomised, double blind, placebo controlled study of fluticasone propionate in patients with moderate to severe chronic obstructive pulmonary disease: the ISOLDE trialBMJ320129730310807619
- CasaburiRMahlerDAJonesPW2002A long-term evaluation of once-daily inhaled tiotropium in chronic obstructive pulmonary diseaseEur Respir J192172411866001
- CasaburiRKukafkaDCooperCB2005Improvement in exercise tolerance with the combination of tiotropium and pulmonary rehabilitation in patients with COPDChest1278091715764761
- CelliB1997Is pulmonary rehabilitation an effective treatment for chronic obstructive pulmonary disease? YesAm J Respir Crit Care Med15578139117007
- CelliBZuWallackRWangS2003Improvement in resting inspiratory capacity and hyperinflation with tiotropium in COPD patients with increased static lung volumesChest1241743814605043
- Centers for Disease Control and Prevention1999Achievements in Public Health, 1900–1999: decline in deaths from heart disease and stroke – United States, 1900–1999MMWR CDC Surveill Summ4864956
- COMBIVENT Inhalation Aerosol Study Group1994In chronic obstructive pulmonary disease, a combination of ipratropium and albuterol is more effective than either agent alone. An 85-day multicenter trialChest1051411198181328
- CooperJDPattersonGASandersonRS1996Results of 150 consecutive bilateral lung volume reduction procedures in patients with severe emphysemaJ Thorac Cardiovasc Surg1121319308911330
- CrinerGJCordovaFCFurukawaS1999Prospective randomized trial comparing bilateral lung volume reduction surgery to pulmonary rehabilitation in severe chronic obstructive pulmonary diseaseAm J Respir Crit Care Med16020182710588623
- CroxtonTLWeinmannGGSeniorRM2003Clinical research in chronic obstructive pulmonary disease. needs and opportunitiesAm J Respir Crit Care Med1671142912684252
- DolleryCDolleryC1991Oxitropium bromideTherapeutic drugsEdinburghLivingstone16870
- DonohueJFvan NoordJABatemanED2002A 6-month, placebo-controlled study comparing lung function and health status changes in COPD patients treated with tiotropium or salmeterolChest122475512114338
- DorinskyPMReisnerCFergusonGT1999The combination of ipratropium and albuterol optimizes pulmonary function reversibility testing in patients with COPDChest1159667110208193
- FergusonGT2000Update on pharmacologic therapy for chronic obstructive pulmonary diseaseClin Chest Med217233811194782
- FishmanAP1994Pulmonary rehabilitation research: NIH workshop summaryAm J Respir Crit Care Med149825338118655
- FlahertyKRCameroonEACurtisJL2001Short-term and long-term outcomes after bilateral lung volume reduction surgery: prediction by quantitative CTChest11913374611348937
- GeddesDDaviesMKoyamaH2000Effect of lung-volume-reduction surgery in patients with severe emphysemaN Engl J Med3432394510911005
- GhafouriMAPatilKDKassI1984Sputum changes associated with the use of ipratropium bromideChest86387936236043
- GrossNJ1988Ipratropium bromideN Engl J Med319486942970009
- HattotuwaKLGizyckiMJAnsariTW2002The effects of inhaled fluticasone on airway inflammation in chronic obstructive pulmonary disease: a double-blind, placebo-controlled biopsy studyAm J Respir Crit Care Med1651592612070058
- HayJGStonePCarterJ1992Bronchodilator reversibility, exercise performance and breathlessness in stable chronic obstructive pulmonary diseaseEur Respir J5659641628722
- KarpelJP1991Bronchodilator responses to anticholinergic and beta-adrenergic agents in acute and stable COPDChest9987161672634
- KotloffRMHansen-FlaschenJLipsonDA2001Apical perfusion fraction as a predictor of short term functional outcome following bilateral lung volume reduction surgeryChest12016091511713142
- LipsonDA2004Redefining treatment in COPD: new directions in bronchodilator therapyTreat Respir Med38995 Erratum in Treat Respir Med, 3:18115182210
- The Lung Health Study Research Group2000Effect of inhaled triamcinolone on the decline in pulmonary function in chronic obstructive pulmonary diseaseN Engl J Med3431902911136260
- MahlerDAWirePHorstmanD2002Effectiveness of fluticasone propionate and salmeterol combination delivered via the diskus device in the treatment of chronic obstructive pulmonary diseaseAm J Respir Crit Care Med16610849112379552
- MakJCHaddadEBBuckleyNJ1993Visualization of muscarinic M4 mRNA and M4 receptor subtype in rabbit lungLife Sci53150188412514
- MaltaisFHamiltonAMarciniukD2005Improvements in symptom-limited exercise performance over 8 h with once-daily tiotropium in patients with COPDChest12811687816162703
- ManninoDMHomaDMAkinbamiLJ2002Chronic obstructive pulmonary disease surveillance – United States, 1971–2000MMWR Surveill Summ51116
- MartinRJBartelsonBLSmithP1999Effect of ipratropium bromide treatment on oxygen saturation and sleep quality in COPDChest11513384510334150
- McNicholasWTCalverleyPMALeeA2004Long-acting inhaled anticholinergic therapy improves sleeping oxygen saturation in COPDEur Resp J2382531
- Medical Research Council Working Party1981Long-term domiciliary oxygen therapy in chronic hypoxic cor pulmonale complicating chronic bronchitis and emphysemaLancet168166110912
- MurrayCJLopezAD1997aRegional patterns of disability-free life expectancy and disability-adjusted life expectancy: Global Burden of Disease StudyLancet3491347529149696
- MurrayCJLopezAD1997bGlobal mortality, disability, and the contribution of risk factors: Global Burden of Disease StudyLancet3491436429164317
- MurrayCJLopezAD1997cAlternative projections of mortality and disability by cause 1990–2020: Global Burden of Disease StudyLancet34914985049167458
- National Emphysema Treatment Trial Research Group2001Patients at high risk of mortality from lung volume reduction surgeryN Engl J Med34510758311596586
- National Emphysema Treatment Trial Research Group2003A randomized trial comparing lung-volume–reduction surgery with medical therapy for severe emphysemaN Engl J Med34820597312759479
- National Heart, Lung, and Blood Institute1998Morbidity and mortality: Chartbook on cardiovascular, lung, and blood diseasesBethesda, MDUS Department of Health and Human Services, Public Health Service, NIH
- Nocturnal Oxygen Therapy Trial Group1980Continuous or nocturnal oxygen therapy in hypoxemic chronic obstructive lung diseaseAnn Int Med9339186776858
- NiewoehnerDERiceKCoteC2005Prevention of exacerbations of chronic obstructive pulmonary disease with tiotropium, a once-daily inhaled anticholinergic bronchodilator. A randomized trialAnn Int Med1433172616144890
- O’DonnellDELamMWebbKA1998Measurements of symptoms, lung hyperinflation, and endurance during exercise in chronic obstructive pulmonary diseaseAm J Respir Crit Care Med1581557659817708
- RennardSISerbyCWGhafouri1996Extended therapy with ipratropium is associated with improved lung function in patients with COPD. A retrospective analysis of data from seven clinical trialsChest11062708681667
- SciurbaFCRogersRMKeenanRJ1996Improvement in pulmonary function and elastic recoil after lung-reduction surgery for diffuse emphysemaN Engl J Med334109598598868
- SinDDTuJV2001Inhaled corticosteroids and the risk of mortality and readmission in elderly patients with chronic obstructive pulmonary diseaseAm J Respir Crit Care Med164580411520719
- SpenceDPHayJGCarterJ1993Oxygen desaturation and breathlessness during corridor walking in chronic obstructive pulmonary disease: effect of oxitropium bromideThorax481145508296259
- TarpSPCelliBR1995Long-term oxygen therapyN Engl J Med333710147637750
- TaubeCLehnigkBPaaschK2000Factor analysis of changes in dyspnea and lung function parameters after bronchodilation in chronic obstructive pulmonary diseaseAm J Respir Crit Care Med1622162010903244
- TsukinoMNishimuraKIkedaA1998Effects of theophylline and ipratropium bromide on exercise performance in patients with stable chronic obstructive pulmonary diseaseThorax53269739741369
- VathenenASBrittonJREbdenP1988High-dose inhaled albuterol in severe chronic airflow limitationAm Rev Respir Dis13885052462383
- van NoordJAde MunckDRBantjeTA2000Long-term treatment of chronic obstructive pulmonary disease with salmeterol and the additive effect of ipratropiumEur Respir J158788510853852
- van NoordJAAumannJ-LJanssensE2005Comparison of tiotropium once daily, formoterol twice daily and both combined once daily in patients with COPDEur Resp J2621422
- VinckenWvan NoordJAGreefhorstAPDutch/Belgian Tiotropium Study Group2002Improved health outcomes in patients with COPD during 1 year’s treatment with tiotropiumEur Respir J192091611871363
- WiltTJNiewoehnerDKimC2005Use of spirometry for case finding, diagnosis, and management of chronic obstructive pulmonary disease (COPD)Evidence Report/Technology Assessment, nr 121:1–7 AHRQ Publication No 05-E017-2Rockville, MD, USAAgency for Healthcare Research and Quality
- ZuWallackARZuWallackRL2004Tiotropium bromide, a new once-daily inhaled anticholinergic bronchodilator for chronic-obstructive pulmonary diseaseExpert Opin Pharmacother518273515264997