Abstract
An exacerbation of chronic obstructive pulmonary disease (COPD) is the most common respiratory condition necessitating admission to hospital. Many of these are relatively mild in nature and as a consequence, there is increasing interest in immediate and early discharge of patients with nonsevere exacerbations. Following initial assessment, “hospital at home” or “assisted discharge” schemes enable suitable patients with COPD to be discharged into the community earlier than normally anticipated. The putative implication is that substantial financial savings can be made in addition to increasing the availability of in-patient beds, without compromising patient care or satisfaction. We highlight the current literature which has evaluated the role of hospital at home and assisted discharge schemes and discuss our own “real life” service operating in a large teaching hospital in Scotland.
Introduction
Chronic obstructive pulmonary disease (COPD) is a common cause of morbidity and mortality encompassing large numbers of individuals in both developed and less well developed countries. It can place a significant burden upon patients, families, society, and primary and secondary care providers alike. Estimates suggest that COPD will become the world’s third leading cause of mortality and the fifth most common cause of serious morbidity over the next 20 years (CitationPauwels et al 2001).
An exacerbation of COPD is defined as a sustained worsening of respiratory symptoms that is acute in onset and usually requires a patient to seek medical help or alter medication. The deterioration must also be more severe than the usual variation experienced by the individual on a daily basis (CitationNCCCC 2004). Exacerbations of COPD are the most common respiratory cause for hospital admission and account for around 10% of all medical admissions in the United Kingdom (CitationPearson et al 1994; CitationAshton et al 1995). This translates into over 90 000 patients hospitalized each year, with the mean duration of stay estimated at 11 days (CitationLAIA 2003). As a consequence, this has wide reaching financial implications for secondary care providers and is likely to be implicated in increased hospital bed occupancy and rates of hospital-acquired infections. Any intervention which successfully hastens patient recovery and discharge from hospital can therefore be seen to be advantageous in the overall management of COPD. Indeed, previous data evaluating an assisted discharge service in 241 stable elderly medical patients demonstrated a 24% reduction in cost compared with acute hospital care (CitationCoast et al 1998).
In recent years, there has been growing interest in the use of schemes which permit patients with relatively mild exacerbations of COPD to be cared for at home. This involves selected patients being managed at home after either initial assessment in hospital and immediate discharge, or after several days of in-patient care. This evidence-based review highlights the current literature regarding the use of hospital at home and assisted discharge schemes for patients with exacerbations of COPD. We also illustrate our own personal experience of the everyday running of such a scheme.
All authors carried out a comprehensive literature search looking for relevant articles published up to April 2006 using Medline, Clinical Evidence, and the Cochrane library. The following keywords were used in the search: chronic obstructive pulmonary disease, management, exacerbations, early support discharge schemes, assisted discharge, hospital at home, and randomized controlled trial. Relevant fully published articles were then selected and extracted.
Definition
The two commonly used strategies which facilitate the rapid discharge of patients back into the community are termed “hospital at home” and “early” or “assisted” discharge. Hospital at home involves patients being initially evaluated in a rapid respiratory assessment unit in hospital. These units (often based in accident emergency or medical admission wards) aim to identify individuals with mild exacerbations of COPD who can be safely managed at home and as a consequence are not generally admitted to hospital. Early or assisted discharge schemes allow suitable patients to be discharged before they have fully recovered from an acute exacerbation, usually within several days after admission to hospital. In both schemes, patients remain under the care of the hospital consultant, although General Practitioners are informed that their patient is back in the community. Multidisciplinary team assessment frequently takes place in both schemes and patients are discharged with appropriate medical treatment. Nursing support is arranged at home for a variable length of time and facilitates the identification of deterioration in clinical condition and readmission to hospital if necessary. The putative inference is that such schemes could result in reductions in length of hospital stay and potential financial savings without compromising patient care and satisfaction or adversely affecting subsequent readmission rates or mortality.
Trials evaluating the effects of hospital at home or assisted discharge
Six randomized controlled trials have examined the effects of hospital at home or assisted discharge schemes in patients with exacerbations of COPD in terms of readmission rates, mortality, quality of life, or length of hospital stay () (CitationShepperd et al 1998; CitationCotton et al 2000; CitationDavies et al 2000; CitationSkwarska et al 2000; CitationOjoo et al 2002; CitationHernandez et al 2003). After discharge into the community, patients in the six studies (range of mean forced expiratory volume in one second [FEV1] 0.69–1.1L) were followed up for a minimum of 2 weeks and a maximum of 12 weeks. In all of them, criteria such as those suggested by the British Thoracic Society (CitationNCCCC 2004), were followed to ensure that patients did not have adverse clinical parameters or social circumstances which might have indicated that in-patient care was more appropriate. It is also important to note that in all of the studies, a significant number of patients needed to be screened so suitable patients with mild exacerbations of COPD without serious concomitant disease processes or adverse social circumstances were identified (). For example, in one of the studies with the greatest number of randomized patients, 718 individuals with a diagnosis of exacerbation of COPD over an 18 month period, were assessed for inclusion and only 184 (26%) were considered suitable (CitationSkwarska et al 2000). Reasons for patients not being eligible for study entry included presence of adverse clinical parameters (chest radiograph abnormality, confusion, impaired level of consciousness, pH <7.35; 50%), serious medical co-morbidity (19%), refusal to participate (3%), and adverse social circumstances (2%).
Table 1 Demographics and results of randomized controlled trials evaluating the use of hospital at home or assisted discharge schemes
Mortality and need for readmission
All six trials measured mortality rates and need for readmission between patients incorporated into either hospital at home or assisted discharge schemes versus those receiving conventional hospital-based care (CitationShepperd et al 1998; CitationCotton et al 2000; CitationDavies et al 2000; CitationSkwarska et al 2000; CitationOjoo et al 2002; CitationHernandez et al 2003). No significant differences were observed between groups although it is important to point out that the follow-up period was limited to a maximum of 12 weeks.
Reducing length of in-patient stay
The effectiveness in terms of reduced length of hospital stay was specifically evaluated in two randomised controlled trials (CitationCotton et al 2000; CitationHernandez et al 2003). In one study (CitationCotton et al 2000), 41 patients with a nonsevere exacerbation of COPD were randomly allocated to early discharge and 40 were allocated to conventional in-patient management. Patients were visited on the day after admission by a specialist respiratory nurse and at intervals considered appropriate thereafter. Those in the early discharge group had a mean hospital stay of 3.2 days (range 1–16 days) while those in the conventional group had a mean stay of 6.1 days (range 1–13 days). In another study, CitationHernandez and colleagues (2003) evaluated the effects of randomly assigning 222 patients with COPD to either conventional in-patient care or immediate or early discharge. The desired period of follow-up was chosen by a respiratory nurse with a maximum of 5 visits at home permitted over an 8 week period with unlimited telephone access. Conventional care resulted in a greater length of hospital stay amounting to 4.2 days versus 1.7 days in the early discharge group (p < 0.001 for the difference).
Acceptability
Hospital at home and assisted discharge schemes have been shown to be acceptable both to patients and healthcare workers. On the completion of their randomized controlled trial, CitationSkwarska and colleagues (2000) obtained questionnaires on general satisfaction with their assisted discharge scheme. Sixty nine percent of patients treated at home and 55% of their General Practitioners responded to questionnaires. The vast majority of patients (95%) were “completely satisfied” with the service and 90% felt that they had been cared for “just as well or better” at home than they would have been in hospital. Moreover, all General Practitioners who responded were satisfied with the provision of domiciliary support for patients with mild exacerbations of COPD, while 65% felt that doing so did not increase their workload. In another study, satisfaction scores demonstrated similar mean scores for home management (92%) versus conventional hospital based management (88%) (CitationOjoo et al 2002). In the study by CitationHernandez and colleagues (2003), patients managed at home also had a higher satisfaction score than those assigned to hospital care.
Effects upon quality of life
Effects upon health-related quality of life were assessed in three trials (CitationShepperd et al 1998; CitationDavies et al 2000; CitationHernandez et al 2003). In one study, the St George’s respiratory questionnaire (SGRQ) was assessed during the first week of the exacerbation and after 3 months of follow up (CitationDavies et al 2000), with no significant differences observed between groups. In another study (CitationHernandez et al 2003), there was a greater, although statistically nonsignificant (p = 0.05) improvement in SGRQ score in patients treated at home than in the control group. CitationShepperd and colleagues (1998) obtained questionnaires on general health status and respiratory health status at the beginning and following 3 months of follow up. There were no signicant differences in scores between individuals managed at home compared with those receiving conventional in-patient care.
Cost effectiveness
An indirect cost calculation carried out in Lothian, Scotland showed that the cost of an early supported discharge scheme was £877 versus £1753 for a hospital admission due to an acute exacerbation of COPD (CitationSkwarska et al 2000). In a randomized controlled trial comparing the cost of hospital at home care versus in-patient hospital care for patients recovering from hip replacement, knee replacement, and hysterectomy, elderly medical patients and COPD, there were signicantly greater healthcare costs for home managed patients with the latter (CitationShepperd et al 1998), although the numbers of patients included were small (n = 32). However, in a larger study (n = 222), the overall cost for an 8 week hospital at home service was 62% that of the cost of conventional in-patient management (CitationHernandez et al 2003). An Australian study of patients with an exacerbation of COPD (n = 25) primarily evaluated the comparative cost of home-based care with traditional in patient care. The group randomized to home care cost 30% less (p < 0.01 for the difference) than those who received in-patient management (CitationNicholson et al 2001).
Our own experience
Aberdeen Royal Infirmary is a large teaching hospital (n = 952 acute admission beds) situated in the North East of Scotland with a catchment population of 523,400 patients (city centre population 212,200). Due to the practical difficulties of traveling long distances and possible need for re-admission, individuals with mild exacerbations of COPD are only considered suitable for assisted discharge if they live within a 30-mile radius of the base hospital. All data from patients enrolled into our early discharge scheme are stored electronically in a secure database accessible only by passwords known exclusively by relevant staff. The data shown in illustrates the numbers of patients entered into our own assisted discharge scheme between January 2002 to December 2005 and shows that only a relatively small proportion required readmission to hospital. As can be observed from , many patients were willing to be incorporated into our assisted discharge scheme during subsequent re-admissions to hospital.
Table 2 Numbers of patients (mean age 72 years) with mild exacerbations of COPD entered into our own assisted discharge scheme and frequency of readmission to hospital
Table 3 Numbers of patients having single and repeat episodes of assisted discharge for mild exacerbations of COPD over a 3 year period
Patient suitability
Patients are firstly assessed in hospital by a specialist registrar or consultant in respiratory medicine. This varies between several hours after arrival in an acute admission ward to several days of in-patient care in a general medical or respiratory ward. During this contact period, clinical condition along with laboratory and radiology results are assessed, treatment optimized, and overall suitability discussed with both the patient and nursing staff. It is not necessary for a given patient to be under the direct care of, or have previous contact with, a respiratory physician. Factors which prevent patients from being discharged earlier from our own hospital are shown in .
Table 4 Clinical features and social circumstances considered unsuitable for entering patients into our own assisted discharge scheme
Community management and follow up
Prior to starting our service in 2001, all General Practitioners were provided with written information outlining the assisted discharge scheme (). The General Practitioners of all patients entering the scheme are informed by fax on the day of their discharge back into the community. This also allows changes in treatment, diagnosis and results of investigations to be communicated. Thereafter, General Practitioners only become involved in a patients’ care if a nonrespiratory problem is encountered throughout the subsequent assisted-discharge period.
Figure 1 Algorithm describing proposed protocol for entering patients into assisted hospital discharge.
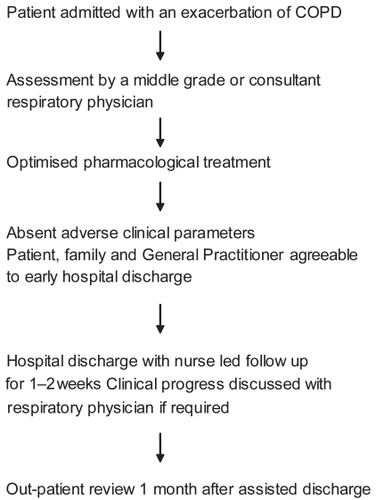
After discharge from hospital, nursing advice — by home visit or by telephone — is available on a 24 hour basis for a minimum of 7 to a maximum of 14 days. If required, oxygen cylinders and nebulizers are given for short-term use during this period, the use of which is monitored by respiratory specialist nurses. Currently, a team of 7 nurses are available to conduct the daily visits which take place at an agreed time suitable for all relevant parties. During home visits, patients’ physiological observations (temperature, blood pressure, pulse, respiratory rate, oxygen saturation, and peak expiratory flow rate) are recorded and the patients’ progress discussed. When necessary, intravenous antibiotics are administered and venepuncture carried out to check, for example, aminoglycoside levels. If at anytime during assisted hospital discharge a patients’ progress is considered unsatisfactory, re-admission to hospital can be arranged by the nurse directly to the respiratory ward (). All individuals entered into the scheme are given an appointment to be reviewed at a respiratory out-patient clinic 1 month following assisted discharge.
Patient satisfaction
All patients embarking on their initial episode of assisted discharge are asked to fill in a satisfaction questionnaire. Of those questionnaires returned between 2002–2005, more than 90% felt that their “overall satisfaction with the service provided at home” was between 8–10 on a 10 point scale.
Funding
In December 2001, funding of £86,000 was initially allocated from the Scottish Executive’s Winter Planning Initiative. This agreed amount was given to pilot an early assisted discharged scheme for 3 months for patients admitted to hospital with an exacerbation of COPD. Following the success of the pilot, NHS Grampian continued to fund the service on a “non-recurring basis”. In 2005, this service was integrated into respiratory medicine with recurring annual funding of £200,000.
Conclusion
Current randomized controlled trials evaluating hospital at home or assisted discharge schemes for patients with mild exacerbations of COPD suggest that they do not result in patients requiring readmission and are not associated with an increased mortality rate over a 12 week period. Moreover, patients generally find them an acceptable alternative to hospital admission although it is important to point out that many patients with an exacerbation of COPD are not suitable for inclusion in such schemes. Several of the studies high-lighted in this review have also shown considerable financial savings as compared with conventional in-patient care.
In a meta-analysis of randomized controlled trials (n = 754 patients), CitationRam and colleagues (2004) evaluated the overall efficacy of hospital at home schemes. This demonstrated that hospital readmission (relative risk [RR] 0.89, 95% confidence interval [CI] 0.72 to 1.12) and mortality rates (RR 0.61, 95% CI 0.36 to 1.05) were not significantly different when hospital at home or assisted discharge schemes were compared with standard in-patient care. As anticipated, substantial financial savings were made along with the increased availability of in-patient beds. It is important to point out that in the same meta-analysis (CitationRam et al 2004), only 1 out of every 4 patients presenting to hospital were eligible for inclusion, although it possible that due to strict study entry requirements, this figure may not be completely reflective of “real life”.
Despite these clear advantages, hospital at home or assisted discharge services are not generally in widespread use in hospitals throughout the UK. For example, a postal questionnaire was sent to consultants in 223 different respiratory departments in the UK in 1999. Although over 90% of consultants were aware of early discharge schemes, in only 16% of departments was such a service in place with difficulty in securing adequate funding the main reason for not having one (CitationJohnson et al 2001). However, in a UK-based national COPD audit in 2003, 44% of hospitals did in fact have an immediate or early discharge service of some sort available (CitationQuantril et al 2005). Greater emphasis should perhaps be made of such schemes in national published guidelines in addition to provision of a suggested working framework (CitationNCCCC 2004). Indeed, it is increasingly important that all practicing respiratory physicians and health authorities are made aware of the existence of hospital at home and assisted hospital discharge schemes and of the potential financial savings involved.
Our own experience and data suggests that assisted hospital discharge schemes can result in reductions in the length of hospital stay for patients with COPD, as the mean length of stay in our hospital is now 4 days. Moreover, we have also extended our service to incorporate patients with other chronic respiratory disorders such as bronchiectasis, interstitial lung disease, and chronic asthma (CitationCurrie et al 2005). We feel that part of the success of our own scheme is related to the meticulous screening and appropriate selection of patients for inclusion (). It is known that the mortality from COPD on admission to hospital is closely linked to the degree of acidosis (CitationWarren et al 1980) and presence of concomitant medical disorders (CitationSeneff et al 1995; CitationConnors et al 1996). As a consequence, patients with a pH <7.35 are not considered suitable for assisted hospital discharge, although we do not exclude patients with other medical disorders such as ischemic heart disease, diabetes mellitus or cardiac failure who are considered to be clinically stable. However, it is important to note that one patient with end-stage COPD died while on our own assisted discharge scheme, although this may not have been preventable with in-patient care.
In conclusion, hospital at home and assisted discharge schemes facilitate a safe and effective means by which to discharge patients with mild exacerbations of COPD back into the community and may result in potential financial savings and reductions in bed occupancy. We have also shown that such schemes —which have been shown to be effective in the realms of randomized controlled trials — can be successfully incorporated into the “real life” management of patients. It is important that templates determining which patients may be safely incorporated into assisted discharge schemes are formulated and that they are delivered by appropriately qualified nursing and medical personnel. Factors which are associated with re-admission to hospital or patient dissatisfaction also require to be audited frequently. Perhaps in the future, hospital at home and assisted discharge schemes can be linked up with intensive pulmonary rehabilitation programmes and encouragement of patients to maintain as high a level of physical activity in their daily life as possible, both of which are known to have benefits in the overall management of COPD (CitationGarcia-Aymerich et al 2003; CitationNCCCC 2004).
Acknowledgement
The authors would like to thank Mrs Jackie Fiddes, coordinator at chest clinic C, for her help with data collection.
References
- AshtonCMFergusonJAGoldacreMJ1995In-patient workload in medical specialties: 2. Profiles of individual diagnoses from linked statisticsQJM88661727583080
- CoastJRichardsSHPetersTJ1998Hospital at home or acute hospital care? A cost minimisation analysisBMJ316180269624074
- ConnorsAFJrDawsonNVThomasC1996Outcomes following acute exacerbation of severe chronic obstructive lung disease. The SUPPORT investigators (Study to Understand Prognoses and Preferences for Outcomes and Risks of Treatments)Am J Respir Crit Care Med154959678887592
- CottonMMBucknallCEDaggKD2000Early discharge for patients with exacerbations of chronic obstructive pulmonary disease: a randomized controlled trialThorax55902611050257
- CurrieGPMackenzieMDouglasG2005Assisted hospital discharge in patients with chronic respiratory disordersQJM98541215994170
- DaviesLWilkinsonMBonnerS2000“Hospital at home” versus hospital care in patients with exacerbations of chronic obstructive pulmonary disease: prospective randomised controlled trial”BMJ3211265811082090
- Garcia-AymerichJFarreroEFelezMA2003Risk factors of readmission to hospital for a COPD exacerbation: a prospective studyThorax58100512554887
- HernandezCCasasAEscarrabillJ2003Home hospitalisation of exacerbated chronic obstructive pulmonary disease patientsEur Respir J21586712570110
- JohnsonMKFlaniganUFuldJ2001Hospital at home services for acute exacerbation of chronic obstructive pulmonary disease: a survey of British practiceHealth Bull (Edinb)591637012664756
- LAIA2003Trends in COPDLondonlung asthma information agency, St George’s hospital medical school (No. 1)
- [NCCCC] National Collaborating Centre for Chronic Conditions2004Chronic obstructive pulmonary disease. National clinical guideline on management of chronic obstructive pulmonary disease in adults in primary and secondary careThorax59Suppl 11232
- NicholsonCBowlerSJacksonC2001Cost comparison of hospital- and home-based treatment models for acute chronic obstructive pulmonary diseaseAust Health Rev24181711842709
- OjooJCMoonTMcGloneS2002Patients’ and carers’ preferences in two models of care for acute exacerbations of COPD: results of a randomised controlled trialThorax57167911828049
- PauwelsRABuistASCalverleyPM2001Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease. NHLBI/WHO Global Initiative for Chronic Obstructive Lung Disease (GOLD) Workshop summaryAm J Respir Crit Care Med16312567611316667
- PearsonMGLittlerJDaviesPD1994An analysis of medical workload—evidence of patient to specialist mismatchJ R Coll Physicians Lond2823047932319
- QuantrilSJHoskerHAnsteyK2005Efficacy and organisation of early discharge schemes for acute exacerbations of chronic obstructive pulmonary disease: analysis from the 2nd UK COPD auditThorax60Suppl 2S96
- RamFSWedzichaJAWrightJ2004Hospital at home for patients with acute exacerbations of chronic obstructive pulmonary disease: systematic review of evidenceBMJ32931515242868
- SeneffMGWagnerDPWagnerRP1995Hospital and 1-year survival of patients admitted to intensive care units with acute exacerbation of chronic obstructive pulmonary diseaseJAMA274185277500534
- ShepperdSHarwoodDGrayA1998Randomised controlled trial comparing hospital at home care with inpatient hospital care. II: cost minimisation analysisBMJ316179169624069
- ShepperdSHarwoodDJenkinsonC1998Randomised controlled trial comparing hospital at home care with inpatient hospital care. I: three month follow up of health outcomesBMJ3161786919624068
- SkwarskaECohenGSkwarskiKM2000Randomized controlled trial of supported discharge in patients with exacerbations of chronic obstructive pulmonary diseaseThorax559071211050258
- WarrenPMFlenleyDCMillarJS1980Respiratory failure revisited: acute exacerbations of chronic bronchitis between 1961–68 and 1970–76Lancet1467706102193