Abstract
Purpose
To determine the feasibility of using an accelerometer to characterize physical activity patterns (PA) surrounding chronic obstructive pulmonary disease (COPD) exacerbations (AECOPD) in patients with COPD for 16 weeks.
Methods
Patients with COPD (n = 8) wore the RT3®, a triaxial accelerometer (Stayhealthy, Monrovia, CA) during waking hours and kept daily symptom diaries. The mean vector magnitude unit (VMU) per minute was calculated by dividing the total VMU for the day by the number of minutes the device was worn. Descriptive statistics were used and plots were made showing PA for each subject with AECOPD markers based on symptom diaries and health resource utilization.
Results
Sample characteristics were: age 71 ± 4; 5 Females; forced expiratory volume in one second (FEV1)% predicted: 40% ± 16%; FEV1/forced vital capacity: 45 ± 7; and Medical Research Council dyspnea scale: 2.3 ± 0.9. Overall adherence to the monitoring protocol was 97.6% (Range 92%–100%) while adherence to wearing the device for at least 10 hours per day was 91.5% (Range 75%–99%). Mean vector magnitude units per minute was 117.8 ± 47 (Range 61.4–184.1). Seven exacerbations were captured over a total of 896 person-days of monitoring. There were substantial intra-individual fluctuations in daily PA during both the stable state and with outpatient treated exacerbations.
Conclusions
Patients with COPD were able to adhere to a 16-week activity monitoring protocol and reported a willingness to wear such a device for an extended period of time if the data yield important and useful information for themselves and their health provider. Future work will need to focus first, on validating other promising devices that produce higher quality PA data and second, replicate this monitoring protocol with a larger sample of COPD patients over a longer period.
Introduction
Frequent exacerbations of chronic obstructive pulmonary disease (COPD) can lead to considerable declines in functioning and increased health care costs (CitationNIH 2003). There is no generally accepted definition for acute exacerbations of COPD (AECOPD) though most studies use the criteria of worsening symptoms accompanied by a change in the medical regimen (CitationPauwels et al 2004). While the follow-up of patients after AECOPD has primarily focused on the resolution of symptoms, improvement in lung function and gas exchange, and changes in inflammatory biomarkers (CitationSeemungal et al 2001; CitationAaron et al 2002), investigations into the precise patterns of physical activity recovery following AECOPD have been minimal or notably absent.
Findings from studies that rely on caregiver report or retrospective recall suggest that patients have considerable functional impairment after AECOPD, especially those episodes that require hospitalizations (CitationConnors et al 1996; CitationGarcia-Aymerich et al 2003). CitationConnors and colleagues (1996) found that more than 50% of patients hospitalized for an AECOPD continued to require assistance with their activities of daily living (ADL) six months after discharge. A lower level of self-reported physical activity was strongly associated with increased risk of hospital readmissions for an AECOPD in one recent prospective study (CitationGarcia-Aymerich et al 2003). Qualitative interviews in another study showed that AECOPD have a negative impact on ADL in 91% of the sample with more than half of these patients stopping activities altogether during their AECOPD (CitationVogelmeier et al 2004).
Electronic devices such as accelerometers are suitable for long term monitoring and are capable of detecting and recording daily activities that are likely difficult for patients to recall and quantify with typical self-reports (CitationMatthews et al 2002). Accelerometers have been used on a short-term basis, anywhere from one (CitationCoronado et al 2003; CitationBehnke et al 2005) to five days (CitationSteele et al 2003; CitationPitta et al 2005), often to validate self-reports of physical activity or prescribed exercise. It is important to note that patients who experienced AECOPD have typically been excluded from physical activity monitoring studies. Therefore, the purpose of this exploratory study was to determine the feasibility and acceptability of using an accelerometer device to characterize physical activity patterns surrounding outpatient-treated acute exacerbations of COPD (AECOPD) over a 4-month period.
Methods
Patients who met the following criteria were enrolled: 1) Moderate to severe stable COPD (forced expiratory volume in one second [FEV1]%<50% and FEV1/forced vital capacity [FVC]<70%) confirmed by spirometry; 2) Experienced at least two AECOPD that were treated on an outpatient basis in the previous 12 months; 3) Absence of illnesses such as bronchiectasis, active malignancies or other end stage diseases; 4) Ability to speak, read and write English; and 5) No plans to engage in any new physical activities over the next 4 months. Subjects were recruited directly from an academic medical center and Veteran’s Administration chest clinics and referrals from a COPD support group. We anticipated that if moderate to severely ill patients with COPD who had at least 2 outpatient-treated AECOPD in the previous 12 months were recruited, they would potentially experience at least one AECOPD within the 4-month monitoring time frame (CitationSeemungal et al 2000; CitationGarcia-Aymerich et al 2003). The study protocol was approved by the institutional review board and each subject gave informed written consent.
The first author made visits to subjects’ homes to obtain written consent, perform spirometry, administer baseline paper-pencil questionnaires, demonstrate appropriate use of the activity monitor, and instruct on completion of a daily symptom diary. Subjects wore the RT3® tri-axial accelerometer (Stayhealthy, Monrovia, CA, USA) during waking hours by clipping the device to the waist area, on the nondominant side, upon awakening and removing it when they retired to bed for approximately 112 consecutive days. Subjects completed a daily paper-pencil symptom diary. Two telephone calls were made within the first week to ensure that subjects did not have any difficulty wearing the device. Biweekly visits to subjects’ homes or to other mutually agreed places were made to obtain symptom diaries, download the physical activity data to a laptop computer, record health resource use, install fresh batteries, and provide a small honorarium. Subjects received a brief telephone call on alternate weeks to encourage adherence. Data were collected from April 2004 to May 2005.
The pager-size RT3® measured physical activity in three dimensions: anteroposterior, vertical, and mediolateral. The device sampled movements at a rate of 10Hz and analog-to-digital converted data were recorded every second and then summed to produce 1-minute movement epochs of vector magnitude units (VMU). An earlier model of this device (TriTrac®, Stayhealthy, Monrovia, CA, USA) was tested in patients with COPD who participated in pulmonary rehabilitation and concurrent validity was established (CitationSteele et al 2003). We operationally defined COPD exacerbations as a sustained worsening of at least two major symptoms (dyspnea, sputum volume, and sputum purulence) or increase in one major and one minor symptom (wheezing, cough, sore throat, and nasal discharge/congestion) for at least two consecutive days and accompanied by changes in the medical regimen (CitationSeemungal et al 2000; CitationPauwels et al 2004). A prescription for or self-directed treatment with a course of oral prednisone or antibiotics were considered a change in the usual medical regimen. Improvements in symptoms for at least 3 consecutive days (“better” rating on the symptom diary) indicated the start of recovery. The Medical Research Council (MRC) dyspnea scale (CitationFletcher et al 1959) and the Seattle Obstructive Lung Disease Questionnaire (SOLDQ) were administered at baseline (CitationTu et al 1997). Exit interviews were conducted during the final home visit to assess acceptability of the protocol and other difficulties not previously identified.
Physical activity data were converted into a Microsoft Excel (Microsoft, Redmond, WA, USA) file for data reduction and analysis. The mean VMU per minute was calculated by dividing the total VMU for the day by the number of minutes the device was worn. We did not remove time spent riding in a motor vehicle since unpublished data showed inconsequential differences in mean VMU calculations (Steele pers comm). We included data for which subjects wore the devices at least 10 waking hours. Adherence data were calculated as a percentage of the number of days the device was worn out of 112 days. Plots were made of the physical activity data for each subject with AECOPD noted on the plots based on the symptom diaries and medications used.
Results
Nine subjects were screened with eight (5 women and 3 men) who enrolled and completed the study. Subjects had a mean age of 71 ± 4, FEV1% predicted of 40% ± 16%, FEV1/FVC ratio of 45 ± 7, and MRC dyspnea score of 2.3 ± 0.9. A majority of the subjects were Caucasian (88%), attended at least some college (63%), and were retired (88%). Baseline SOLDQ scores were 38.8 ± 14.9, 69.6 ± 20.3, 75.0 ± 21.7, and 64.1 ± 10.4 for the physical, emotional functioning, coping skills, and treatment satisfaction scales, respectively.
Overall, mean adherence to the 112-day monitoring protocol was 97.6% (range 92%–100%) while adherence to wearing the device for at least 10 hours per day was slightly less at 91.5% (range 75%–99%). There were two incidents of battery failure with two different devices; a total of 23 days of data were lost. The adherence rate was impressive especially in light of the consistent report by subjects that remembering to wear the device was most challenging. One subject commented, “I would see the pager on my kitchen table and would pass by it repeatedly during the day but somehow it doesn’t cross my mind to clip it on until later when I all of sudden realize that I should be doing that”.
The daily average VMU per minute for the sample was 117.8 ± 47 (range 61.4–184.1). Seven AECOPD were captured over 896 person-days of monitoring. Two subjects experienced two AECOPD each and three other subjects each experienced one episode. We primarily relied on visual analyses of graphical plots since no meaningful statistical analyses could reliably be performed on the physical activity data from a relatively few number of AECOPD events and with the degree of intra- and inter-individual, day-to-day variability that we observed. Data for one relatively less disabled 72-year old female subject who did not have any AECOPD during the 4 month is shown in . shows data for a 75-year old male subject who had three episodes of greater symptoms than usual and one meeting our AECOPD criteria. Similar to the other four subjects who experienced at least one AECOPD, there was a tendency for decreased activity when increased symptoms were logged. However, there were no consistent downward trends in activity before, during, or after AECOPD that were remarkably different from the day-to-day variability.
Figure 1 Physical activity data for a 72-year old female subject who did not have an AECOPD during the study. The shaded band represents the 25th and 75th percentile. The dashed line shows the mean VMU/minute.
Abbreviations: AECOPD, acute exacerbations of chronic obstructive pulmonary disease; VMU, vector magnitude unit.
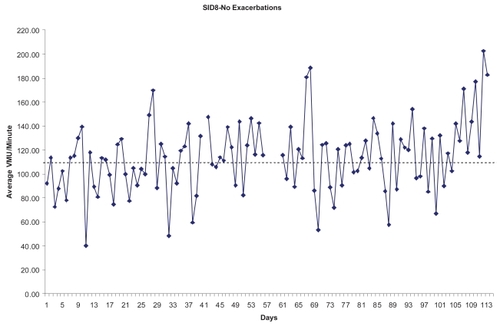
Figure 2 Physical activity data for a 75-year old male subject who reported two episodes of increased symptoms and a third that was accompanied by medical treatment. The shaded band represents the 25th and 75th percentile. The dashed line shows the mean VMU/minute.
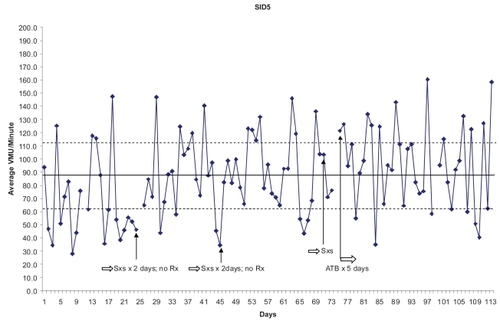
Discussion
This exploratory study showed that patients with COPD were willing and able to undergo 4 months of continuous physical activity monitoring, the longest recording duration that we are aware of in the COPD literature. We found that the RT3® device captured substantial intra-individual fluctuations in daily physical activity. Finally, the preliminary data suggest that patients who experienced AECOPD and were treated at home did not have noticeable changes in their physical activity patterns before, during, or after the AECOPD episode that was distinguishable from their usual day-to-day variability.
Our main goal was to assess if patients with moderate to severe COPD would wear an unobtrusive monitoring device that could potentially yield useful information about their health over an extended period. The overall adherence rate was quite remarkable considering the challenges that other investigators typically face when accelerometer devices are used for brief periods to ascertain exercise participation (CitationDubbert et al 2002). The high adherence rate could be attributed to our weekly contact, but also that a majority of the subjects were retired and very conscientious in implementing routines to help them remember to wear the device. This finding should provide some measure of support to researchers to further explore the possible use of like devices to passively monitor and detect dynamic changes in patients’ physical functioning over time.
Aside from the extraneous artifact that typically accompany accelerometry recordings, the variability in day-to-day physical activity was, to some degree expected, since previous reports described patients’ experiences of “good” and “bad” days. The findings from two studies that used an accelerometer (CitationPitta et al 2005) and pedometer (CitationSchonhofer et al 1997) for shorter monitoring periods confirm our observations. The mean coefficient of variation for walking time in 18 patients with COPD over five days was 28% ± 14% and was as high as 89% ± 35% with lying time. The degree of variability was not associated with disease severity or age (CitationPitta et al 2005). The report by CitationSandland and colleagues (2005) of no significant differences in mean activity counts within subjects over a seven day window were probably reflective of intra-individual variations. One group of investigators actually reported strikingly similar patterns of variability in daily self-reported health status over the course of a year for patients who were discharged from a hospital for AECOPD (CitationVerbrugge et al 1989). The tremendous within-subjects variation in accelerometry-derived activity data may perhaps have significant drawbacks for use, both as a reliable summary outcome measure from therapies and as a potential “marker” for early identification of AECOPD or delayed functional recovery after an AECOPD.
Though very preliminary, our findings suggest that patients whose AECOPD are milder and are managed outside of a hospital did not have visible changes in their physical activity pattern before, during, or after their AECOPD episodes. Only one study presented in the form of an abstract actually measured physical activity in patients with COPD during AECOPD but regrettably, those AECOPD episodes, presumably more severe, were treated in a hospital (CitationPitta et al 2004). Patients were monitored on days 2 and 7 of their hospitalization and 1 month after discharge for 12 hours using a tri-axial activity monitor worn on a belt with a second sensor attached to the leg. Unlike the RT3, the leg sensor provided a second positioning coordinate, allowing the device to differentiate between different positions. These patients walked significantly less and spent more time in the lying position one month after discharge compared with stable, but unmatched COPD patients. Although matching can account for a limited number of factors that influence physical activity, comparisons of activity patterns should ideally be made using patients’ previous stable states which we have attempted to do. The work by CitationDonaldson and colleagues (2005) partially supports our observations. They found that in a cohort of patients with COPD who were followed over an 8-year period had rapid recoveries from outpatient-treated AECOPD as measured by self-reports of time spent outdoors. It is important to note that our sample may not be characteristic of the general COPD population since three of the four unique AECOPD occurred in three subjects who were on a stable self-directed exercise regimen for more than 6 months prior to enrolling in the study. Also, the RT3, designed to be worn at the waist, does not have adequate specificity in capturing decrements in certain other potentially important ADL that may be negatively impacted by AECOPD.
Conclusions
Our findings suggest that patients with COPD will wear a pager-sized accelerometer that continuously tracks their physical activity over time, both during the stable state and with AECOPD episodes. The results of this study extend current knowledge regarding the comparable within-subjects variability in physical activity associated with outpatient-treated AECOPD as in the stable state. A major caveat to our observations is that the sample was rather small with few events and we were not able to subject the data to rigorous statistical tests. However, we recommend additional work in this area, first, identifying a simple device, unhampered by sophisticated data reduction and analysis algorithms that yield reliable ambulatory physical activity data and secondly, conduct of a larger study to document the natural pattern of physical activity across the illness continuum including periods of stable illness, during AECOPD, and recovery from these acute events. An understanding of these specific activity patterns might aid in the development of more timely and responsive interventions aimed at minimizing functional declines in this patient population.
Acknowledgements
Supported by University of Washington School of Nursing Research and Intramural Funding Program and K12 HD049100 from the National Institutes of Health Roadmap/National Institute of Child Health and Human Development to Dr. Nguyen.
References
- AaronSDVandemheenKLClinchJJ2002Measurement of short-term changes in dyspnea and disease-specific quality of life following an acute COPD exacerbationChest1216889611888946
- BehnkeMWewelARKirstenD2005Exercise training raises daily activity stronger than predicted from exercise capacity in patients with COPDRespir Med997111715878487
- ConnorsAFJrDawsonNVThomasC1996Outcomes following acute exacerbation of severe chronic obstructive lung disease. The SUPPORT investigators (Study to Understand Prognoses and Preferences for Outcomes and Risks of Treatments)Am J Respir Crit Care Med1544 Pt 1959678887592
- CoronadoMJanssensJPDe MuraltB2003Walking activity measured by accelerometry during respiratory rehabilitationJ Cardiopulm Rehabil233576414512781
- DonaldsonGCWilkinsonTMHurstJR2005Exacerbations and time spent outdoors in chronic obstructive pulmonary diseaseAm J Respir Crit Care Med1714465215579723
- DubbertPMCooperKMKirchnerKA2002Effects of nurse counseling on walking for exercise in elderly primary care patientsJ Gerontol A Biol Sci Med Sci57M7334012403802
- FletcherCMElmesPFairbairnA1959The significance of respiratory symptoms and the diagnosis of chronic bronchitis in a working populationBMJ251472576613823475
- Garcia-AymerichJFarreroEFelezMA2003Risk factors of readmission to hospital for a COPD exacerbation: a prospective studyThorax58100512554887
- MatthewsAECOPDAinsworthBEThompsonRW2002Sources of variance in daily physical activity levels as measured by an accelerometerMed Sci Sports Exerc3413768112165695
- [NIH] NIH National Heart, Lung and Blood Institute2003Global initiative for chronic obstructive lung disease: global strategy for the diagnosis, management and prevention of chronic obstructive pulmonary disease workshop reportWashington, DCNIH Publication No# 2701
- PauwelsRCalverleyPMBuistAS2004COPD exacerbations: the importance of a standard definitionRespir Med989910714971871
- PittaFTroostersTSpruitMA2004Physical activity level in hospitalized and stable COPD patientsAm J Respir Crit Care Med169A769
- PittaFTroostersTSpruitMA2005Characteristics of physical activities in daily life in chronic obstructive pulmonary diseaseAm J Respir Crit Care Med171972715665324
- SandlandCJSinghSJCurcioA2005A profile of daily activity in chronic obstructive pulmonary diseaseJ Cardiopulm Rehabil25181315931024
- SchonhoferBArdesPGeibelM1997Evaluation of a movement detector to measure daily activity in patients with chronic lung diseaseEur Respir J102814199493666
- SeemungalTHarper-OwenRBhowmikA2001Respiratory viruses, symptoms, and inflammatory markers in acute exacerbations and stable chronic obstructive pulmonary diseaseAm J Respir Crit Care Med16416182311719299
- SeemungalTADonaldsonGCBhowmikA2000Time course and recovery of exacerbations in patients with chronic obstructive pulmonary diseaseAm J Respir Crit Care Med16116081310806163
- SteeleBGBelzaBHunzikerJ2003Monitoring daily activity during pulmonary rehabilitation using a triaxial accelerometerJ Cardiopulm Rehabil231394212668936
- TuSPMcDonellMBSpertusJA1997A new self-administered questionnaire to monitor health-related quality of life in patients with COPD. Ambulatory Care Quality Improvement Project (ACQUIP) InvestigatorsChest112614229315792
- VerbruggeLMBalabanDJ1989Patterns of change in disability and well-beingMed Care273 SupplS128472921883
- VogelmeierCPartridgeMRStahlE2004Burden of exacerbations in COPD: the patient’s perspectiveAm J Respir Crit Care Med169A769