Abstract
If patients are to participate fully in their care and in the management of a long term condition such as chronic obstructive pulmonary disease, good communication is essential. However, not all patients are able to use the written word and we need to be aware of the size of this problem and its implications for the way in which we give information and conduct medical consultations. The impact of health literacy on outcomes can be considerable and improvements can be made by being aware of the problem, offering information in several different forms, and by reinforcing the spoken word with pictorial images.
Introduction
Good communication is essential within the healthcare system. If patient centered care is to be developed within a partnership of care between a patient and a healthcare professional, the sharing of medical information needs to be fully comprehensible by all. This necessitates an awareness of the range of literacy skills possessed by our patients, the impact of reduced health literacy skills and its impact upon access to healthcare. In this review we have addressed the size of the problem, its identification, its impact, and how to minimize the effect of reduced health literacy.
What is health literacy?
Health literacy is defined as the ability to read, understand and act on health care information. In more detail, health literacy is the degree to which individuals have the capacity to obtain, process and understand basic health information and services required to make appropriate health decisions (CitationUS Department of Health and Human Services 2000). According to the United States (US) National Adult Literacy Survey (NALS) in 1992, 21% of those surveyed in the US scored in the lowest of 5 skill levels (CitationKirsch et al 1993). In the UK approximately 16% of adults have literacy skills lower than that attained by the average 11 year old (CitationThe Skills for Life Survey 2003).
Diminished health literacy is a widespread problem which affects people of all social classes and all ethnic groups. Impaired health literacy has been shown to be worse amongst the elderly and amongst low-income populations (CitationWolf et al 2005) and more recently, the 2003 National Assessment of Adult Literacy has shown that, more than 75 million adults in the US have only basic or less than basic health literacy (CitationKutner 2006). A US systematic review of 85 studies showed there was no association with gender but a positive association with level of education, ethnicity and age (CitationPaasche-Orlow et al 2005). This may or may not be the same in other countries.
In terms of how this relates to how patients manage their care, one study looked at how much patients understand about taking their medication and showed that between 67.1% and 91.1% of patients surveyed correctly understood the medicine label instructions, with those with the lowest literacy scoring the lowest (CitationDavis et al 2006). Just over a third could say how many tablets should be taken when given a written label containing the instructions “Take two tablets by mouth twice daily”.
Patients with limited health literacy skills have been shown to report poorer overall health and they are less likely to make use of screening and they present in later stages of disease. They are more likely to be hospitalized, have an overall poorer understanding of their treatment and have lower adherence to medical regimens (CitationCentre for Health Care Strategies 2008).
Studies in a less wealthy population suggest that patients with low health literacy skills and chronic diseases such as diabetes, asthma, or hypertension have less knowledge of their disease and its treatment, as well as fewer correct self management skills than literate patients (CitationWilliams et al 1998a). Low health literacy is independently associated with poor understanding of disease (CitationWilliams et al 1998b), worse health status (CitationWeiss BD 1992; CitationSchillinger et al 2002), and higher use of services. (CitationBaker et al 1997, Citation1998).
Low literacy affects all aspects of patients’ lives and 40% have been reported to express feelings of shame with two thirds not telling spouses of their literacy problems and over half never telling their children (CitationParikh et al 1996).
Health literacy in the elderly
Tests of literacy such as the Rapid Estimate of Adult Literacy in Medicine tool (REALM) assess the reading ability of individuals and are a crude measure of health literacy. This has been used to identify likely reduced health literacy skills in several patient groups. Among 127 patients attending a UK hospital clinic with rheumatoid arthritis 15% were found to have functional illiteracy (CitationGordon et al 2002). Among those attending an US asthma clinic 13% read at below 3rd grade (CitationWilliams et al 1998a). In a UK outpatient study of COPD patients 15% of patients were not able to use written information (CitationTaylor et al 2005).
Other studies have shown lower reading skills in older age groups (CitationGazmararian et al 1999). The NALS study showed that in those aged over 65 years, 44% had the lowest reading level compared to 16% in 45 to 54 age group. Further analysis of the data showed that 43.6% of the elderly in this study were taking more than 3 medications per day and 66.5% had at least one of five chronic conditions (COPD, coronary heart disease, heart failure, hypertension, or diabetes) (CitationKirsch et al 1993). CitationPaasche-Orlow et al (2005) showed in a systematic review of 31,129 patients that a low level of health literacy correlated with reduced level of education, ethnicity and older age.
There are many factors which may explain the high incidence of reduced health literacy in elderly populations and conditions such as dementia and cognitive decline will clearly also affect an individual’s health literacy. The incidence of dementia increases dramatically in older people (CitationHatcher 1999). Dementia affects approximately 6% of people at 65 years and approximately 24% of those over 85 years, although these figures are not consistently found (CitationHenderson and Jorm 1998). Depression may also impair concentration and may be a risk factor for cognitive decline (CitationJorm 2000).
Poor reading skills have a very important impact on the elderly due to their high prevalence of chronic disease and their need to understand healthcare information. Patients with chronic conditions such as COPD are an important group to tackle because these patients typically have complex treatment regimens, requiring multiple consultations often with different clinicians.
Adherence with COPD therapy
The nature of the disease, the treatment, patient beliefs and expectations about therapy all combine to influence patient adherence to therapy (CitationHorne and Weinman 1999). In COPD as in asthma, adherence can be low and is a significant risk factor for morbidity and mortality (CitationCochrane 1992). Studies in asthma and COPD have shown that adherence can be less than 50% of prescribed medication (CitationRand 2005). Patients are likely to under-use maintenance therapy and symptom relieving drugs are often over used (CitationHand and Bradley 1996). In a study investigating prescription refill adherence for asthma and COPD, over half of repeat prescriptions for inhaled corticosteroids dispensed to patients over 60 showed an undersupply suggesting that these patients are not using their prescriptions optimally (CitationKrigsman et al 2007).
In addition to a general limitation of their ability to recall information, patients with reduced health literacy may inherently have more difficulty comprehending medical information. Such individuals are thus more likely to be non-compliant due to misunderstandings (CitationRand 2005). Much of what is said in any medical consultation is forgotten soon after it ends (CitationLey 1979), and in elderly COPD patients, cognitive impairment can be an additional barrier to comprehension (CitationAllen and Ragab 2002). Large-scale studies have been performed in patients with hypoxemia and have shown impairments in abstract reasoning, memory and co-ordination of simple motor tasks (CitationPrigatano et al 1983; CitationGrant et al 1982, Citation1987).
There is also an increased risk of depression in COPD patients, up to 2.5 times greater for severe COPD when compared to patients in the control group (Citationvan Manen et al 2002). Many patients with COPD experience a strong sense of loss and feelings of hopelessness perceiving that they were told that “nothing could be done” or that the condition was “self inflicted” (CitationOliver 2001). The published literature has shown that patients may feel guilty or depressed about their condition and studies recognize that consultations should involve the patient in decision making (CitationBooker 2005; CitationOsman and Hyland 2005). A study of diabetics with poor health literacy showed that physicians very rarely checked patient recall of new concepts or explained them more clearly (CitationSchillinger et al 2003).
However little work has been done to identify the impact of health literacy on compliance in COPD or its effect upon what patients do or do not do in a consultation. We have previously shown how patients do not fully understand the medical letters they receive (CitationRoberts and Partridge 2006) and have tried to provide further information to patients to improve their understanding (CitationBrown et al 2007). However, there is little published evidence regarding the modifying of consultations/guidelines for patients with COPD who might have cognitive problems or limited health literacy.
Improving compliance – interventions and educational programmes
Using asthma as an example, self management strategies have been used to increase medication adherence and may include disease education, self-monitoring, teaching, and checking inhaler technique and reinforcement. Many of these interventions have been shown to work in adults with asthma (CitationBailey et al 1990; CitationOnyirimba et al 2003; CitationPut et al 2003). In COPD CitationBourbeau et al (2003) showed a reduction in hospital utilization in patients with COPD following a complex intervention; they demonstrated a reduction in hospital admission for exacerbations of COPD by 39.8% and ER attendances by 41%. This programme included education, a home exercise programme, support, an action plan including use of antibiotics and steroid tablets, and case management. In 2003 a Cochrane review by CitationMonninkhof et al (2003) concluded that there was too little data to say that self management in COPD works, although of the 8 studies reviewed only 2 involved the patient receiving a written self management action plan. Using an action plan with COPD patients increases recognition of a severe exacerbation and increases use of antibiotics and oral steroids (CitationTurnock et al 2005) and can reduce unscheduled primary care consultations and may reduce mortality (CitationSridhar et al 2008).
These studies have thus shown that by giving patients individualized advice and going through medication with patients along with other interventions such as pulmonary rehabilitation and case management can improve some outcomes. However advice needs to be tailored further to ensure comprehensibility by all and this may involve use of pictorial aids within action plans and use of other formats such as DVDs to reinforce important messages for patients to take home.
Acceptance of interventions such as rehabilitation also needs to be considered and how invitations are made may be critical. In a study of those with chronic obstructive pulmonary disease involving pulmonary rehabilitation, 120 of 297 suitable patients responded that they did not wish to take part in the trial. These patients were subsequently approached in a qualitative study to determine why they declined to take part in the study. The results revealed that several themes influenced patients’ willingness or otherwise to take part in a research project involving pulmonary rehabilitation. Patients often found it difficult to get to the hospital, they did not understand the purpose or benefit of the research, and they had negative experiences of the hospital and also thought that the pulmonary rehabilitation component would be detrimental to their health (CitationTaylor et al 2007). The role of health literacy was not addressed in this study but we need to ensure that information such as invitation letters are user friendly and at an appropriate reading age to ensure recruitment of all suitable patients.
Consultations with patients
Consultations can be stressful events for patients and take place in an environment which is often perceived to be unfamiliar. Most patients are interrupted by the doctor within 18 seconds of their opening statement (CitationBeckman and Frankel 1984), even though another study has shown that the average spontaneous talking time uninterrupted was 92 seconds and more than three quarters of patients had finished talking within 2 minutes (CitationLangewitz et al 2002).
Studies by CitationFalvo and Tippy (1988) and CitationSchillinger et al (2003) have shown that patients recall very little (less than 50%) of what they are told about during their consultations and another study has shown that patients and doctors often have conflicting views regarding the key messages that should be taken away from a consultation (CitationParkin 2003). Even when information is given patients commonly complain that physicians do not provide understandable explanations (CitationZiegler et al 2001). For patients with low levels of functional health literacy this problem will be enhanced and thus may experience problems reading labels of medication, interpreting results, comprehending appointment or reading materials and conceptualizing risk. They will also have difficulty naming and describing their medications (CitationWilliams et al 1995).
CitationConstantinidou and Baker (2002) showed that older adults learned better from visual presentations of information than by auditory presentations. Use of both written and verbal communication has been shown to be the most effective way of increasing patient understanding and compliance (CitationHouts et al 1998, Citation2001, Citation2006). Consultations may thus be improved in several ways, for example by giving the patient written advice or information such as a leaflet with details of their individual medication (CitationSandler et al 1989). As part of the UK NHS plan (Department of Health 2000) letters being sent from a specialist to the patients’ general practitioner are also offered to the patient. This provision of information can be developed further by dictating these letters in front of the patient both to reduce factual errors before they leave but also to again reinforce information by means of the spoken word (CitationLloyd 1997). However, patients often do not fully understand the medical terms detailed within the letters they receive and the letters to primary care physicians copied to patients have been shown to be quite difficult for patients to read (CitationRoberts and Partridge 2006). We designed a respiratory glossary which can be used as a tool in aiding respiratory patients understanding of the letter being sent to their GP (CitationBrown et al 2007). It is important that the magnitude of low health literacy in the population is recognized and instead of trying to identify these vulnerable patient groups, other methods should be used to reinforce the comprehensibility for all patients especially those with long-term conditions. These may include use of consultation tools such as decision aids, pictograms, leaflets, or videos (CitationPartridge 1986; CitationPlimpton and Root 1994; CitationDelp and Jones 1996; CitationSechrest and Henry 1996; CitationHouts et al 1998; CitationMurphy et al 2000). Pictorial representations have been shown to improve recall of medical instructions in a clinical setting (CitationHouts et al 1998) and pictograms have been shown to be an effective tool, enhancing consultations and aiding understanding (CitationHouts et al 2006). Patients with long term conditions should always be helped to learn how to manage their own condition (CitationPartridge 2005).
Identifying patients with low health literacy
Individuals may have low health literacy skills for a range of reasons such as a lack of educational opportunity, learning difficulties, or cognitive decline which is increased in older adults. Individuals with low health literacy are more likely to be unable to name their medication, frequently miss appointments or say they have forgotten their glasses, and are more likely attend with someone else who takes on the role of “surrogate reader”. In a study of patients seeing resident physicians, only 50% of those with impaired health literacy were correctly identified by the doctor (CitationRogers et al 2006). CitationKelly and Haidet (2007) have shown that doctors overestimated patient literacy for 54% of African Americans, 11% of white non-Hispanics, and 36% of other patients.
Two tools have been widely used with patients to objectively measure health literacy levels. The first is the Rapid Estimate of Adult Literacy in Medicine (REALM) test (CitationDavis et al 1993) which is medical-word recognition and pronunciation test. Patients read 3 lists of words which increase in complexity and patients score from 0 to 66 which translates to American school grade level. The second test is the “TOFHLA” test which is a test of functional health literacy in adults, measuring numeracy and reading comprehension (CitationBaker 1999). These tests can range from taking a few minutes (REALM) to 20 minutes (TOFHLA) to undertake and the appropriateness of the test and time to administer should be considered when selecting a test. Their use would normally be for research purposes alone and they would not usually be administered in a busy clinical situation. These tools need to be used sensitively for they can be distressing to patients who feel they are being tested, and in clinical practice the realization of the size of the problem of functional illiteracy is the vital point so that other methods of communication are used to reinforce advice for all patients.
Improving comprehension within consultations with those with COPD
It is difficult to predict which patients have limited health literacy (CitationKelly and Haidet 2007) and (CitationRogers et al 2006) and screening literacy levels in every new patient is probably impractical as well as potentially distressing to some who may find it an affront to their dignity. We know from published studies that it is likely that a minimum of 15% of patients may have diminished literacy (CitationWilliams et al 1998a; CitationGordon et al 2002). Reports show that those with diminished literacy often conceal it from others, including close family members (CitationParikh et al 1996). When considering how to improve comprehension within the consultation an increased awareness that those with COPD may have diminished literacy is a good a starting place.
A positive relationship between patient and health worker is essential particularly as this group of patients commonly exhibit low self esteem, depression and guilt regarding a condition which may be perceived as self afflicted. Building patient empathy and pre-empting potential obstacles in communication can aid effective knowledge transfer and improve adherence to therapy regimens and self management plans (CitationKorsch and Negrete 1972). The development of self management plans for COPD patients should be carried out in a partnership between the patient and the doctor or nurse specialist. Providing patients with individualized advice and explaining how to take and how to alter medication, along with other interventions such as pulmonary rehabilitation and regular follow-up can improve outcomes (CitationBailey et al 1990; CitationMonninkhof et al 2003). Advice could be tailored further to ensure that it is suitable for all including those with low literacy by using pictorial aids such as pictorial action plans and using other formats such as DVDs to reinforce important messages for patients to take home.
Information materials which have a predominately written component should be tested for level of readability with tools such as the Flesch reading age and Kincaid Scale available on modern Microsoft word packages. In addition to readability testing, simple thought to ensuring text or pictures are of adequate size is important (CitationWallace et al 2006). Kessler et al have shown that COPD patients’ understanding of the word “exacerbation” was poor, a term which you would expect most COPD patients to recognize. 59.2% of patients had never heard of the term or did not know what it meant, and only 2 (1.6%) could explain its meaning correctly (CitationKessler et al 2006). Patients used alternative words such as shortness of breath, breathlessness, crisis or attack. Speaking plainly, using simple language and identifying the key take home messages you need to convey can be useful: better communication and education are fundamental to allowing patients with COPD to better understand and develop strategies to cope with their disease. In a recent editorial reviewing a COPD rehabilitation programme, it was reported that prior to entry into the programme many patients reported a lack of basic understanding about COPD and management of their condition. Some patients reported not knowing what their condition was called and primary care was criticized as a poor source of expertise, information and support (CitationJones 2007).
Designing the consultation to contain more open ended questions and asking patients to repeat and confirm medication instructions before leaving the consultation can help check that instructions have been understood (CitationSchillinger et al 2003). Rather than instructing someone to take their medicine at 9 AM or 9 PM use the words morning or evening; 24-hour clock time scales can be confusing. In addition awareness of cultural differences that may affect communication ought to be noted. Nodding may mean ‘no’ in some cultures and in those in whom English language is limited, providing a translator or family member who can translate can be helpful. Drawing a simple diagram to explain an investigation or medication taking behaviors can be helpful.
Thought might be given to the use of literature and material pre and post consultation as well as during the consultation (CitationPartridge 1999; CitationBrown et al 2007). Using questionnaires either pre-consultation in the waiting room or posting out to patients at home can have some use in aiding the consultation. Although health professionals should be aware that patients with reduced health literacy may struggle to fill in the simplest questionnaire, such tools may enable the patient to seek clarification from a partner or confidant such that they enter the consultation better prepared. We have shown, for example, that among those with suspected sleep apnea syndrome the Epworth Sleepiness Scale (ESS), a worded tool that is designed to be self completed, was not easily understood by all (CitationGhiassi et al 2007a). Respondents were required to mark the likelihood of falling asleep with an answer ranging from 0 to 3, yet 33.8% of new users and 15.7% of those who had used the scale previously made errors when completing the form and needed additional one to one assistance from staff. Common errors ranged from giving answers between scores, leaving questions blank, or ticking or marking answers with a cross. 5% of patients were upfront and reported problems with health literacy and 2.5% asked a family member or friend to fill in the form. Some who struggled to complete the form reported that they had left their spectacles at home, an excuse often used by those with impaired health literacy skills.
Pictorial aids – their use and evaluation
To help deliver key health messages, clinicians have a range of resources available to them ranging from the written word to pictorial aids and videos. Consultation aids such as those given in are useful in reinforcing health information (CitationPartridge 1999; CitationHouts et al 1998, Citation2001, Citation2006). In particular for those with diminished health literacy it may be important to present information in a variety of ways. Confucius (and sometimes Napoleon) is attributed with saying ‘A picture is worth a thousand words’. Advertisers have been coupling pictures and words for decades to aid the successful transfer of information. Pictures in medicine similarly have been shown to be a successful adjunct to both verbal and written medical information (CitationKatz et al 2006).
Table 1 Tools that reinforce advice and information given during the consultation
A study by Dowse and Ehlers assessed understanding of “text only” or “text plus pictogram” labels on prescribed antibiotics in a female low literacy population. Adherence to therapy and understanding of medication instructions were improved in the group that received “text and pictograms” in contrast to “text only” labels (CitationDowse and Ehlers 2005). Indeed even amongst those with normal literacy levels, pictograms have been shown to enhance the recall and transfer of medical information (CitationHouts et al 1998, Citation2001). Research indicates that humans have a cognitive preference for picture based rather than text based information and the ‘picture superiority effect’ describes this phenomenon (CitationKatz et al 2006). Much of the research with pictograms and symbols used in medicine has been done with pharmaceutical agencies producing standardized pictorial symbols which depict medication-taking behaviors that help patients to comprehend medical information (CitationDowse and Ehlers 2001; CitationKatz et al 2006).
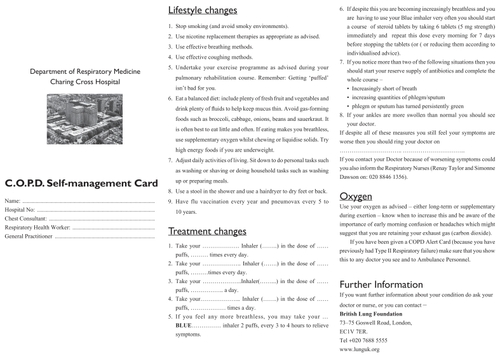
Producing generic pictograms that are comprehensible to all is not easy and there is evidence that comprehensibility of some pictograms may be disease specific. In the development of a pictorial sleepiness and screening tool for obstructive sleep apnoea syndrome (OSAS), the image of ‘witnessed apnoea’ was better understood by those diagnosed with OSAS in contrast to those without the disease (CitationGhiassi et al 2007b). The use of pictograms requires care and it is not adequate to develop a representation without first testing the understanding and comprehensibility of the desired images in the appropriate population. Before images can be used with a population it is preferable to validate and test the images to ensure that both the patients and the healthcare professionals perceive the pictograms in a similar way. One validated method of testing pictograms is using Guessability and Transclucency questionnaires (CitationBloomberg 1990; CitationYovetich and Young 1988). The guessability questionnaire prompts subjects to look at each image and they are asked to record what they think it represents (). With translucency testing, the image and word are shown together and respondents are required to rate the relationship between image and word from a score ranging from 1 to 7, with 1 representing a poor relationship and 7 the strongest relationship (). The two questionnaires can be used to modify and develop pictorial tools. Pictograms can be repeatedly tested and modified according to their comprehensibility by patients in whom they are likely to be used, ensuring the best representations are used for the desired tool. Using such techniques we have previously developed both a paper and an electronic version of an asthma self management plan and are currently testing a pictorial COPD self management plan ().
Figure 1 An example of an image used in guessability and translucency testing. The guessability questionnaire asks subjects to give a short meaning to the image for each image being tested. The translucency questionnaire allows subjects to review the image and the meaning and asks subject to rate the relationship between the two. The score ranges from one (no relationship) to seven (very strong relationship). Subjects are normally asked to complete the guessability questionnaire before the translucency questionnaire.
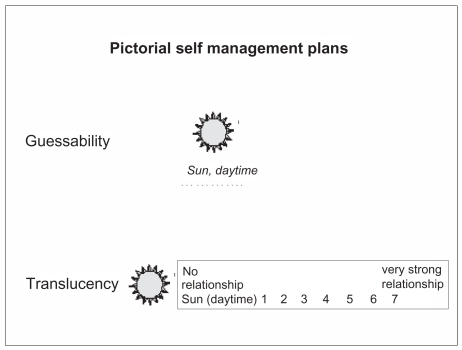
Figure 2 Example of a written COPD self management plan; Pictorial versions of this plan are currently being tested with COPD patients.
Overall, it is important that information given to patients is not “dumbed down”; it should be pitched and tailored carefully to each patient, patients with higher literacy skills should have access to more detailed information should they require it.
In summary, there are several tools or strategies available for improving the consultation to make it optimal for those with a range of literacy skills (). After the consultation, written and pictorial advice should be given to patients to reinforce advice and improve patients’ ability to recall information ultimately increasing patient adherence to therapies and patient satisfaction.
Summary points
Reduced health literacy is associated with reduced compliance and poor health outcomes
Literacy skills in patients are difficult to assess
Tools to assess literacy such as REALM can highlight reduced literacy but can be an embarrassing procedure for patients
You can improve recall and compliance in all patients if you:
Give patients some information before their appointment to inform them of what will take place
Use less jargon in your consultations
Ask your patients questions about details you have changed during their current consultation, ie, medication “Can you tell me how often you are going to take your new inhaler (show picture to patient) when you get home?”
Draw diagrams or give patients some key written messages to take home
Use leaflets or pictures to reinforce any key messages you want patients to remember
Send your patients a copy of the letter you send to their physician, but do so with a glossary of terms it may contain
Disclosures
The authors report no conflicts of interest.
References
- AllenSCRagabS2002Ability to learn inhaler technique in relation to cognitive scores and tests of praxis in old agePostgrad Med J7837911796871
- BaileyWCRichardsJMJrBrooksCM1990A randomized trial to improve self-management practices of adults with asthmaArch Intern Med150166482200380
- BakerDW1999Development of a brief test to measure functional health literacyPatient Education and Counseling38334214528569
- BakerDWParkerRMWilliamsMV1998Health literacy and the risk of hospital admissionJ Gen Intern Med1379189844076
- BakerDParkerRMWilliamsMV1997The relationship of patient reading ability to self-reported health and use of health servicesAm J Public Health871027309224190
- BeckmanHBFrankelRM1984The effect of physician behaviour on the collection of dataAnn Intern Med10169266486600
- BloombergK1990The comparative translucency of initial lexical items represented in five graphic symbol systems and setsJ Speech Hearing Res33717252148789
- BookerR2005Effective communication with the patientEur Respir Rev14936
- BourbeauJJulienMMaltaisF2003Reduction of hospital utilization in patients with chronic obstructive pulmonary disease: a disease-specific self-management interventionArch Intern Med1635859112622605
- BrownCERobertsNJPartridgeMR2007Does the use of a glossary aid patient understanding of the letters sent to their general practitioner?Clin Med74576017990712
- Centre for Health Care Strategies2008Centre for Health Care Strategies Health Literacy Factsheets [online]Accessed 11 January URL: http://www.chcs.org/resource/hl.html
- CochraneGM1992Therapeutic compliance in asthma; its magnitude and implicationsEur Respir J512241577134
- ConstantinidouFBakerS2002Stimulus modality and verbal learning performance in normal agingBrain Lang8229631112160526
- DavisTCLongSWJacksonRH1993Rapid Estimate of Adult Literacy in Medicine: a shortened screen instrumentFam Med2539158349060
- DavisTCWolfMSBassPF2006Literacy and misunderstanding prescription drug labelsAnn Intern Med1458879417135578
- DelpCJonesJ1996Communicating information to patients: the use of cartoon illustrations to improve comprehension of instructionsAcad Emerg Med3264708673784
- DowseREhlersMS2001The evaluation of pharmaceutical pictograms in a low-literate South African populationPatient Education and Counselling458799
- DowseREhlersM2005Medicine labels incorporating pictograms: do they influence understanding and adherence?Patient Educ Couns58637015950838
- FalvoDTippyP1988Communicating information to patients. Patient satisfaction and adherence as associated with resident skillJ Fam Pract2664373379367
- GazmararianJABakerDWWilliamsMV1999Health literacy among Medicare enrollees in a managed care organizationJAMA2815455110022111
- GhiassiRCumminASlingsbyL2007aCan patients self-adminster the epworth sleepiness scale?Thorax62A110
- GhiassiRCumminAMurphyK2007bThe development of a pictorial screening tool to assess sleepiness and obstructive sleep apnoea syndromeAm J Respir Crit Care Med175A698
- GordonMHampsonRCapellH2002Illteracy in rheumatoid arthritis patients as determined by the Rapid Estimate of Adult Literacy in Medicine (REALM) scoreRheumatology41750412096223
- GrantIHeatonRKMcSweenyAJ1982Neuropsychologic findings in hypoxemic chronic obstructive pulmonary diseaseArch Intern Med142147067103628
- GrantIPrigatanoGPHeatonRK1987Progressive neuropsychologic impairment and hypoxemia. Relationship in chronic obstructive pulmonary diseaseArch Gen Psychiatry4499910063675139
- HandCBradleyC1996Health beliefs of adults with asthma: toward an understanding of the difference between symptomatic and preventive use of inhaler treatmentJ Asthma3333188827940
- HatcherS1999Review: incidence of dementia and Alzheimer’s disease increases with increasing ageEvid Based Ment Health260
- HendersonASJormAF1998Dementia in AustraliaCanberra (ACT): Department of Health and Family Services; Aged and Community Care Service Development and Evaluation Report No 35
- HorneRWeinmanJ1999Patients’ beliefs about prescribed medicines and their role in adherence to treatment in chronic physical illnessJ Psychosom Res475556710661603
- HoutsPBachrachRWitmerJ1998Using pictographs to enhance recall of spoken medical instructionsPatient Educ Couns3583810026551
- HoutsPDoakCLoscalzoM2006The role of pictures in improving health communication: A review of research on attention, comprehension, recall, and adherencePatient Educ Couns611739016122896
- HoutsPWitmerJEgethH2001Using pictographs to enhance recall of spoken medical instructions IIPatient Educ Couns432314211384821
- JonesD2007Too little, too late the patients’ perspective on education for COPDChron Respir Dis41899018029430
- JormAF2000Is depression a risk factor for dementia or cognitive decline?Gerontology462192710859462
- KatzMGKripalaniSWeissBD2006Use of pictorial aids in medication instructions: a review of the literatureAm J Health Syst Pharm632391717106013
- KellyPAHaidetP2007Physician overestimation of patient literacy: a potential source of health care disparitiesPatient Educ Couns661192217140758
- KesslerRStahlEVogelmeierC2006Patient understanding, detection, and experience of COPD exacerbations: an observational, interview-based studyChest1301334216840393
- KirschISJungeblutAJenkinsL1993Adult literacy in America: a first look at the results of the National Adult Literacy SurveyWashington, DCNational Center for Education Statistics, United States Department of Education
- KorschBMNegreteVF1972Doctor-patient communicationSci Am22766745044413
- KrigsmanKMoenJNilssonJL2007Refill adherence by the elderly for asthma/chronic obstructive pulmonary disease drugs dispensed over a 10-year periodJ Clin Pharm Ther326031118021338
- KutnerMGreenbergEJinY2006The health literacy of America’s adults: results from the 2003 National Assessment of Adult Literacy (NCES 2006–483)Washington (DC)US Department of Education, National Center for Education Statistics
- LangewitzWDenzMKellerA2002Spontaneous talking time at start of consultation in outpatient clinic: cohort studyBMJ325682312351359
- LeyP1979Memory for medical informationBr J Soc Clin Psychol1824555454984
- LloydB1997A randomised controlled trial of dictating the clinic letter in front of the patientBMJ314707734789040328
- MonninkhofEvan der ValkPvan der PalenJ2003Self-management education for patients with chronic obstructive pulmonary disease: a systematic reviewThorax58394812728158
- MurphyPWChessonALWalkerL2000Comparing the effectiveness of video and written material for improving knowledge among sleep disorders clinic patients with limited literacy skillsSouth Med J9329730410728518
- OliverSM2001Living with failing lungs: the doctor-patient relationshipFam Pract18430911477052
- OnyirimbaFApterAReisineS2003Direct clinician-to-patient feedback discussion of inhaled steroid use: its effect on adherenceAnn Allergy Asthma Immunol90411512722963
- OsmanLMHylandME2005Patient needs and medication styles in COPDEur Respir Rev148992
- Paasche-OrlowMKParkerRM2005The Prevalence of Limited Health LiteracyJ Gen Intern Med201758415836552
- ParikhNSParkerRMNurssJR1996Shame and health literacy: the unspoken connectionPatient Educ Couns273398788747
- ParkinT2003Discrepancies between patient and professionals recall and perception of an outpatient consultationDiabet Med209091414632716
- PartridgeMR1986Asthma education: more reading or more viewing?J R Soc Med7932683723532
- PartridgeMR2005The asthma consultation: what is important?Curr Med Res Opin2111815881471
- PartridgeM1999Making effective use of limited consultation timeAsthma Journal46873
- PlimptonSRootJ1994Materials and strategies that work in low literacy health communicationPublic Health Rep10986928303020
- PrigatanoGPParsonsOWrightE1983Neuropsychological test performance in mildly hypoxemic patients with chronic obstructive pulmonary diseaseJ Consult Clin Psychol51108166826857
- PutCvan den BerghOLemaigreV2003Evaluation of an individual asthma programme directed at behavioural changeEur Respir J211091512570118
- RandCS2005Patient adherence with COPD therapyEur Respir Rev1497101
- RobertsNJPartridgeMR2006How useful are post consultation letters to patients?BMC Med4216426444
- RogersESWallaceLSWeissBD2006Misperceptions of medical understanding in low-literacy patients: implications for cancer preventionCancer Control13225916885919
- SandlerDAHeatonCGarnerST1989Patients’ and general practitioners’ satisfaction with information given on discharge from hospital: audit of a new information cardBMJ299151132514868
- SchillingerDGrumbachKPietteJ2002Association of Health Literacy With Diabetes OutcomesJAMA2884758212132978
- SchillingerDPietteJGrumbachK2003Closing the loop: physician communication with diabetic patients who have low health literacyArch Intern Med163839012523921
- SechrestRCHenryDJ1996Computer-based patient education: observations on effective communication in the clinical settingJ Biocommun238128723546
- SridharMTaylorRDawsonS2008A Nurse-Led intermediate care package in patients who have been hospitalised with an acute exacerbation of chronic obstructive pulmonary diseaseThorax6319420017901162
- TaylorJDawsonSSridharM2005Functional illiteracy amongst those with chronic obstructive pulmonary disease (COPD)Eur Respir J2657s
- TaylorRDawsonSRobertsN2007Why do patients decline to take part in a research project involving pulmonary rehabilitation?Respir Med1011942617540553
- The Skills for Life Survey2003A national needs and impact survey of literacy, numeracy and ICT skillsResearch Brief RB 490 DfES Publication
- TurnockAWaltersEWaltersJ2005Action plans for chronic obstructive pulmonary diseaseThe Cochrane Database of Systematic Reviews4Art. No: CD00507410.1002/14651858.CD005074.pub2
- US Department of Health and Human Services2000Healthy People 2010: Understanding and Improving Health with understanding and improving health and objectives for improving health2Washington, DCUS Government Printing Office
- van ManenJGBindelsPJEDekkerFW2002Risk of depression in patients with chronic obstructive pulmonary disease and its determinantsThorax57412611978917
- WallaceLSRoskosSEWeissBD2006Readability characteristics of consumer medication information for asthma inhalation devicesJ Asthma43375816801142
- WeissBDHartGMcGeeDL1992Health status of illiterate adults: relation between literacy and health status among persons with low literacy skillsJ Am Board Fam Pract5257641580173
- WilliamsMVBakerDWHonigEG1998aInadequate literacy is a barrier to asthma knowledge and self-careChest1141008159792569
- WilliamsMVBakerDWParkerRM1998bRelationship of Functional Health Literacy to Patients’ Knowledge of Their Chronic Disease: A Study of Patients With Hypertension and DiabetesArch Intern Med158166729448555
- WilliamsMVParkerRMBakerDW1995Inadequate functional health literacy among patients at two public hospitalsJAMA2741677827474271
- WolfMSGazmararianJABakerDW2005Health Literacy and Functional Health Status Among Older AdultsArch Intern Med16519465216186463
- YovetichWYoungTA1988The effects of representativeness and concreteness on the “Guessability” of blissymbolsAugment Altern Comm359
- ZieglerDKMosierMCBuenaverM2001How much information about adverse effects of medication do patients want from physicians?Arch Intern Med1617061311231703