Abstract
Exacerbations contribute significantly to the morbidity of COPD, leading to an accelerated decline in lung function, reduced functional status, reduced health status and quality of life, poorer prognosis and increased mortality. Prevention of exacerbations is thus an important goal of COPD management. In patients with COPD, treatment with a combination of the inhaled corticosteroid fluticasone propionate (250 μg) and the long-acting β2-agonist salmeterol (50 μg) in a single inhaler (250/50 μg) is an effective therapy option that has been shown to reduce the frequency of exacerbations, to improve lung function, dyspnea and health status, and to be relatively cost-effective as a COPD maintenance therapy. Importantly, results of various studies suggest that fluticasone propionate and salmeterol have synergistic effects when administered together that improve their efficacy in controlling symptoms and reducing exacerbations. The present non-systematic review summarizes the role of fluticasone propionate/salmeterol combination therapy in the prevention of exacerbations of COPD and its related effects on lung function, survival, health status, and healthcare costs.
Introduction
Exacerbations contribute significantly to the morbidity, mortality and cost burden of COPD, a disease characterized by progressive air flow limitation that is not entirely reversible, airway inflammation and mucociliary dysfunction.Citation1,Citation2 In addition to producing short-term increases in breathlessness and other symptoms, exacerbations have sustained effects, including an accelerated decline in lung function,Citation3,Citation4 reduced health status and quality of life,Citation5–Citation9 and increased risk of death.Citation10–Citation11 Although therapeutic interventions to control the clinical symptoms of COPD and reduce airway inflammation are available, most studies indicate available treatments do not slow the long-term progression of the disease.Citation2 However, newer therapies, including combination therapy with an inhaled corticosteroid (ICS) and long-acting beta-agonist (LABA), are able to prevent episodes of exacerbation, thereby enhancing treatment strategies, particularly for moderate-to-severe COPD.
The present non-systematic review summarizes the role of fluticasone propionate and salmeterol combination therapy (FSC) in the prevention of exacerbations of COPD as well as its related effects on lung function, survival, health status and quality of life, and healthcare costs. This review also discusses prescribing considerations of interest to practicing clinicians. Although the intended focus of this review is FSC, where relevant we have referenced studies of budesonide/formoterol (Symbicort®; AstraZeneca), another currently available ICS/LABA combination therapy; however, the majority of the clinical experience, clinical trial data, and other real-world observational outcomes data available at this time concern FSC (Advair®/Seretide®; GlaxoSmithKline), in part because this formulation has been available for a longer period of time.
Impact of exacerbations in COPD
Although there is no consensus on a definition, an exacerbation of COPD is generally defined as an acute worsening of dyspnea, cough, and/or sputum that is beyond normal day-to-day variation and sufficient to warrant a change in medication.Citation1,Citation2 Exacerbations are associated with airway inflammation that is most often triggered by bacterial or viral infection, air pollution or cold weather; no cause is identified about one-third of the time.Citation2,Citation12 A bacterial etiology, related to either pre-existing lower airway colonization or newly acquired bacterial strains, has been identified in approximately 50% of exacerbations.Citation13,Citation14 Bacterial load has been considered the primary factor; however, a recent prospective, longitudinal study utilizing molecular typing found that the concentration of either pre-existing or newly acquired strains had no or only a small impact on exacerbation incidence, a finding which suggests that more complex host-pathogen interactions are involved in exacerbations of bacterial etiology than simply bacterial load.Citation13,Citation14
The precise mechanisms underlying the amplified inflammatory response remain unclear, but exacerbations have been associated with infiltration of neutrophils and eosinophils, markers of oxidative stress, into airway walls along with tumor necrosis factor-α (TNF-α), leukotriene (LT) B4, interleukin (IL)-8, leukotrienes and other pro-inflammatory cytokines.Citation2,Citation12,Citation15
Exacerbations are common in COPD and are recognized more frequently in patients with more severe disease, some of whom are likely to experience three or more exacerbations per year.Citation12 Donaldson and colleagues reported a median of 2.68 exacerbations per year in those with moderate disease (GOLD stage II) and 3.43 exacerbations per year in those with severe disease (GOLD stage III).Citation16 A history of exacerbation in the prior year is predictive of exacerbations in the current year.Citation8 Exacerbations tend to cluster together in time; Hurst et al found that over a quarter of first exacerbations were followed by a second exacerbation within 8 weeks and about one-third of all exacerbations were recurrent ones.Citation17 In a retrospective cohort study of recently hospitalized patients with COPD exacerbations, 13.2% of patients in the reference group were readmitted within 12 months and 24.3% died within the year following a COPD hospitalization.Citation18 Similarly, a study from Canadian hospitals found that 38% of patients admitted for COPD were readmitted within an average of 5 months.Citation19
Even with appropriate treatment during the acute episode, exacerbations often instigate a downward spiral in which the patient never returns to baseline lung or physical functioning levels. In a study of 109 patients with COPD, those with frequent exacerbations (≥2.92 exacerbations/year) were found to experience additional declines of 8.0 mL/year in FEV1 and 2.22 L/min/year in peak expiratory flow (PEF) compared to patients with fewer exacerbations.Citation3 In a longitudinal cohort study, only 75% of COPD patients experiencing an exacerbation had regained their basal pulmonary function by 5 weeks and 7% had not recovered by 3 months.Citation4 Severe exacerbations requiring hospitalization have even poorer outcomes. Inpatient mortality during COPD admission is as high as 4% to 30%.Citation10 The hospitalization itself is associated with functional decline and psychological disorders, including anxiety and depression, which contribute to readmission.Citation20–Citation22 Quality of life, as assessed by the St George’s Respiratory Questionnaire (SGRQ) and other health/functional status instruments, is also severely impacted by acute exacerbation events, which frequently lead to marked restriction in activities of daily living and poorer mental state.Citation5–Citation9 This deterioration in physical functioning and health status occurs even with no significant deterioration in FEV1, but instead correlates with worsened symptoms, particularly dyspnea, following exacerbation.Citation6–Citation8 Thus, preventing exacerbations is important not only from the short-term clinical perspective, but to help patients to function better and feel better in the longer term.
From a societal perspective, exacerbations are costly. Hospitalizations for exacerbations account for nearly 70% of the direct healthcare costs of treating COPD.Citation23 In the United States alone, COPD-related hospital inpatient and emergency department (ED) costs were estimated to be $10 billion in 2003,Citation24 with estimated mean costs in 2001 of $571 for an emergency department visit, $5997 for a standard hospital admission, and $36,743 for an admission requiring intensive care and intubation.Citation24,Citation25 Patients with both asthma and COPD have particularly high respiratory-related and all-cause healthcare costs and use significantly more healthcare services than those with asthma or COPD.Citation26–Citation28 Given the significant clinical, quality of life, and economic consequences of exacerbations, their prevention has become a widely accepted and singularly important goal in the management of COPD.Citation1,Citation2
COPD maintenance therapy goals
The primary goals of COPD treatment are to improve symptoms and health status and reduce the frequency of exacerbations.Citation2 While pharmacologic therapy is needed for most patients with COPD, it is just one part of disease management. Other components of care include regular visits to monitor and assess disease progression (including repeat spirometry) and identify COPD-related complications and co-morbidities, and reducing risk factors such as smoking, occupational exposures, and exposure to indoor and outdoor air pollution.Citation1,Citation2 Pulmonary rehabilitation and patient education can improve health status, help patients cope better with symptoms and activities of daily living, and prompt earlier recognition of exacerbations by the patient and thus timely treatment.Citation2 Pulmonary rehabilitation results in improvements in exercise capacity, endurance, walking distance, dyspnea and quality of life, and is beneficial even in older patients.Citation29,Citation30 Smoking cessation education in particular provides a significant opportunity to influence the course of the disease and reduce age-related decline in FEV1.Citation31 Early identification of exacerbations is an important objective of COPD care, as early treatment is associated with faster recovery, reduced risk for hospitalization, and better quality of life.Citation32
Pharmacologic therapy is based primarily on the patient’s symptoms and disease severity, with additional agents added as the disease progresses and symptoms worsen. According to guidelines, pharmacotherapy in mild COPD (FEV1/FVC < 0.70 and FEV1 ≤ 80% of predicted value) focuses on short-acting bronchodilators to relieve symptoms, including short-acting β2-agonists (eg, albuterol) and short-acting anticholinergics (eg, ipratropium bromide, oxitropium); the latter have a longer duration of effect (6 to 9 hours) than short-acting β2-agonists (4 to 6 hours).Citation1,Citation2 When symptoms are persistent, the addition of one or more long-acting bronchodilators is recommended (FEV1/FVC < 0.70, FEV1 < 80% predicted). Recommended agents include LABAs (eg, formoterol, salmeterol), long-acting anticholinergics (eg, tiotropium), and, rarely, methylxanthines (eg, theophylline). Treatment with a combination of bronchodilators with different durations and mechanisms of action is recommended when single-agent therapy is inadequate, as this can achieve improved bronchodilation while reducing the risk of side effects from a higher dose of a single agent.Citation2 To improve health status and reduce the frequency of exacerbations, the Global Initiative for Chronic Obstructive Long Disease (GOLD) guidelines recommend adding ICS for symptomatic patients with GOLD stage III or IV disease, FEV1 < 50% predicted, and repeated exacerbationsCitation2, while the American Thoracic Society (ATS)/European Respiratory Society (ERS) guidelines recommend consideration of ICS for patients with FEV1 < 50% predicted and one or more exacerbations in the last year requiring treatment with oral corticosteroids or antibiotics.Citation1 The 50% FEV1 cut-off level is somewhat arbitrary, and many patients with FEV1 > 50% have multiple exacerbations each year. Clinically, combination therapy is often started for patients who are approaching Stage III COPD and have frequent exacerbations. Thus, within the context of a stepped approach to therapy for COPD, FSC is an important option for maintenance therapy and prevention of exacerbations.
Treatment goals are unlikely to be reached if the patient handles the inhaler device incorrectly and the lungs do not receive adequate doses of medication. Teaching the patient correct inhaler technique upon initiation of a new medication and monitoring the patient’s technique at subsequent visits are crucial but often overlooked tasks.Citation33
Pharmacologic effects
Long-acting β2-adrenoceptor agonists have bronchodilator effects. The LABA salmeterol is highly selective for β2-adrenergic receptors and its binding at these sites stimulates production of cyclic adenosine monophosphate (cAMP), leading to relaxation of bronchial smooth muscle and in turn, improved lung emptying during tidal breathing and a decreased perception of dyspnea.Citation34–Citation35 Salmeterol also has non-bronchodilator effects, including improved mucociliary clearance and ciliary beat activity and inhibition of histamine, leukotrienes and other inflammatory mediators produced by mast cells.Citation35,Citation36 Its effects on lung function are apparent within two hours of administration and last for approximately 12 hours.Citation37 A key benefit of salmeterol is thus the symptomatic control of COPD on a day-to-day basis and a decreased need for rescue medication.Citation34,Citation38
Fluticasone propionate, a synthetic trifluorinated corticosteroid, is a glucocorticoid receptor agonist with a receptor binding affinity in vitro greater than that of the glucocorticoid steroids dexamethasone, beclometasone and budesonide.Citation35 Glucocorticoid receptors contain DNA-binding proteins that alter the transcription rates of responsive genes.Citation39 The anti-inflammatory effects of fluticasone propionate derive from its ability to induce conformational changes in cytoplasmic glucocorticoid receptors that subsequently inhibit the expression of inflammatory genes and increase the transcription of anti-inflammatory genes.Citation35,Citation40 An acute decrease in bronchial blood flow occurs following fluticasone propionate administration, and although less well understood, may be due to effects on kinases and phosphatases associated with glucocorticoid receptors that lead to rapid changes in cell function and vasoconstriction.Citation40 The inflammatory processes in COPD primarily involve CD8+ T-lymphocytes (an increase of which is associated with increased airflow obstruction), CD68+ macrophages, and infiltration of neutrophils into airway and lung parenchyma.Citation41,Citation42 Some research indicates that fluticasone propionate does not reduce the number of CD8 cells in bronchial epithelium, but reduces the CD8:CD4 ratio, suggesting that it prevents a rise in CD4 cells.Citation43 It also has been shown to reduce bronchial mucosal mast cells,Citation43,Citation44 neutrophils,Citation45 and systemic markers of inflammation, including C-reactive protein, RP, IL-6, and other inflammatory cytokines.Citation46
Pharmacologic effects of co-administration of fluticasone propionate and salmeterol
There is evidence that the co-administration of fluticasone propionate and salmeterol has synergistic effects at the molecular level whereby fluticasone propionate enhances the β-agonist effect of salmeterol and salmeterol enhances the anti-inflammatory effects of fluticasone propionate.Citation40,Citation41 Several mechanisms appear to be involved. Glucocorticoids prevent the down-regulation of β2-adrenoceptors and increase β2-adrenoceptor gene transcription; this leads to increased β2-adrenoceptor synthesis, providing additional receptors for β2-agonists to activate and increasing intracellular cAMP levels.Citation40,Citation41,Citation47 Long-acting β2-agonists may improve the anti-inflammatory effects of ICS by facilitating translocation of the glucocorticoid receptor/ligand complex into the nucleus.Citation35 Adding salmeterol to fluticasone propionate leads to a greater reduction in TNF-α and macrophage chemokines following rhinovirus infection than is achieved by ICS therapy alone.Citation48,Citation49 These examples of synergistic molecular effects of salmeterol and fluticasone propionate are consistent with results of in vivo studies and clinical trials that have observed greater clinical efficacy with FSC than with its individual components.Citation36,Citation50–Citation54 In contrast, a bronchial biopsy study of steroid-naïve current and former smokers with moderate to severe COPD found that fluticasone propionate 500 μg reduced CD3+, CD4+, CD8+, mast cells and hyperresponsiveness at 6 months compared to placebo, but adding LABA (50 μg) did not lead to greater anti-inflammatory effects.Citation55 Sample size in this study was small (N = 114), however, and a larger follow-up study is needed.
Clinical efficacy
Compared to monotherapy with fluticasone propionate or salmeterol, FSC has been shown in a number of clinical trials to lead to improvements in one or more of the following parameters: lung function, exacerbation rates, dyspnea, chronic bronchitis symptoms, night awakenings, frequency of rescue medication use and health status.Citation36,Citation42,Citation47,Citation51–Citation54 In reviewing clinical efficacy, we have relied primarily on level I evidence from randomized controlled trials (RCTs).
Lung function and symptoms
The comparative effects of FSC on lung function and symptoms versus fluticasone propionate or salmeterol monotherapy have been investigated in several RCTs of COPD (). In a 24-week trial of 691 patients, Mahler et al reported a significantly greater increase in pre-bronchodilator FEV1 with FSC (500/50 μg) than with salmeterol (50 μg), resulting in an improvement of 14.5% over baseline, and a greater increase in 2-hour post-bronchodilator FEV1 with FSC than with fluticasone propionate (500 μg).Citation52 Patients receiving FSC also had improved morning PEF and less dyspnea than patients who received fluticasone propionate or salmeterol alone. Evidence of a synergistic effect of combination therapy was seen, as the PEF mean change from baseline was greater than the sum of the changes achieved with fluticasone propionate and salmeterol individually. Similarly, a 12-month trial (N = 1465) observed greater improvements in pre- and post-bronchodilator FEV1, health status, cough, and breathlessness with FSC 500/50 μg compared with either fluticasone propionate 500 μg or salmeterol 50 μg, and night-time awakenings were decreased with either FSC or fluticasone propionate compared to salmeterol.Citation50 In these trials, an FSC dosage of 500/50 μg administered twice daily was used. The effects of a lower dose of FSC on lung function were assessed in a randomized controlled trial of 723 patients.Citation36 Hanania and colleagues reported a greater increase in morning predose FEV1 with FSC 250/50 μg than with either fluticasone propionate 250 μg or salmeterol 50 μg, with effects observable within 24 hours of the first dose and sustained over 24 weeks, and an increased 2-hour postdose FEV1 with FSC compared with salmeterol.
Table 1 Clinical trials of the effect of fluticasone propionate/salmeterol combination therapy on lung function, symptoms and health status
The effect of FSC on the rate of decline in lung function (FEV1) was evaluated as a secondary outcome in the Towards a Revolution in COPD Health (TORCH) trial, a 3-year, randomized, controlled trial of 6112 patients with moderate-to-severe COPD.Citation56 Lung function (FEV1) declined more slowly with FSC 500/50 μg treatment (39 mL/year) compared to placebo (55 ml/year); however, this rate of decline was not significantly different from the rates of decline seen in the fluticasone propionate 500 μg (42 mL/year) and salmeterol 50 μg (42 mL/year) treatment arms. Two recent parallel-group trials of FSC 250/50 μg and salmeterol 50 μg evaluated morning predose FEV1 as a secondary endpoint and observed declines in lung function in both groups over the 52-week treatment period, but FSC treatment preserved lung function better than did salmeterol alone.Citation51,Citation53 Moreover, withdrawal of fluticasone propionate in patients receiving FSC (500/50 μg) has been shown to result in deterioration in lung function and dyspnea and an increase in mild exacerbations.Citation57
Exacerbation prevention
There is little evidence that LABA alone is effective in preventing exacerbations, but clinical trials have shown that ICS alone (fluticasone propionate or budesonide) reduces COPD exacerbations in the range of 10% to 20%.Citation50,Citation58–Citation61 Several RCTs also have shown that combination ICS/LABA therapy is superior to LABA or ICS alone in reducing exacerbations ().Citation42,Citation51,Citation53,Citation54,Citation62 In contrast, a 12-month trial (N = 1465) found no difference in exacerbation rates between FSC 500/50 μg, salmeterol 50 μg or fluticasone propionate 500 μg.Citation50
Table 2 Clinical trials of efficacy of fluticasone propionate/salmeterol combination therapy in the prevention of COPD exacerbations
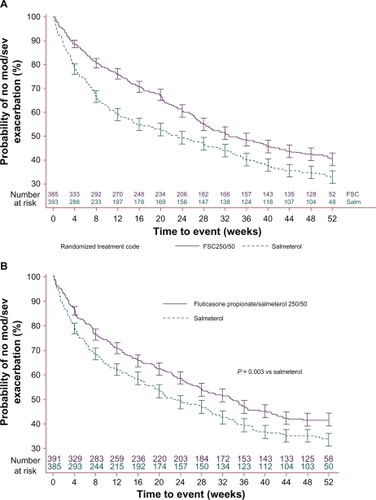
In the 3-year TORCH study, FSC 500/50 μg reduced moderate/severe exacerbations by 12% compared to salmeterol, 9% compared to fluticasone propionate, and 25% compared to placebo.Citation50 A shorter 44-week trial of 994 COPD patients randomized to FSC 500/50 μg or salmeterol 50 μg reported 35% fewer exacerbations in the FSC group.Citation42 Most recently, 2 replicate parallel-group trials evaluated whether the FSC 250/50 μg dose is also associated with reducing annual rates of moderate or severe COPD exacerbations ().Citation51,Citation53 These studies observed reductions in moderate/severe exacerbations of 30.4% and 30.5%, respectively, with FSC compared to active treatment with salmeterol 50 μg.
Figure 1 (A) Reprinted with permission from Anzueto A, Ferguson GT, Feldman G, Chinksy K, et al. Effect of fluticasone propionate/salmeterol (250/50) on COPD exacerbations and impact on patient outcomes. COPD. 2009;6(5):320–329.Citation53 Copyright © 2009 Taylor & Francis. (B) Reprinted with permission from Ferguson GT, Anzueto A, Fei R, Emmett A, Knobil K, Kalberg C. Effect of fluticasone propionate/salmeterol (250/50 μg) or salmeterol (50 μg) on COPD exacerbations. Respir Med. 2008;102(8): 1099–1108.Citation51 Copyright © 2008 Elsevier.
Similar findings have been observed for budesonide/formoterol (160/4.5 μg). In a 12-month trial, this combination therapy led to a 35% lower rate of mild exacerbations compared to budesonide 200 μg alone.Citation62 The same study observed a 23% lower rate of severe exacerbations with budesonide/formoterol compared to formoterol (4.5 μg) but no difference compared to budesonide.
Improvement in exacerbation rates in patients treated with FSC has been most evident in patients with more severe disease; however, a recent analysis of the TORCH trial data based on disease severity found that FSC treatment decreased exacerbations by 31% relative to placebo in patients with GOLD stage II COPD (moderate; FEV1/FVC < 0.70, 50% ≤ FEV1 ≤ 80% predicted).Citation63
Survival
It is not entirely clear whether or not FSC treatment confers a survival benefit, as clinical studies to date have been underpowered to assess mortality. The TORCH study reported a 17.5% lower risk for death (2.6% absolute risk reduction) in the combination therapy group; however, this finding was just short of statistical significance (P = 0.052).Citation54 Statistical and clinical significance are not always the same and the observed absolute reduction in risk identified in the TORCH trial deserves careful clinical consideration. Practitioners of clinical medicine may feel less concern with a small deviation from a statistically significant finding when the absolute size of the effect is relatively large and clinically relevant, as sample size has a large influence on the P-value.Citation64 In a pooled analysis of seven randomized controlled trials, Sin and colleagues observed a decrease in all-cause mortality of approximately 27% with ICS plus LABA compared to placebo (hazard ratio [HR] 0.73, 95% confidence interval [CI], 0.55 to 0.96).Citation65 In several retrospective observational studies, FSC or ICS have been associated with significantly lower mortality,Citation18,Citation66–Citation69 but one other study found no survival benefit associated with ICS.Citation70
Health status and quality of life
Measures of lung function, such as FEV1, do not necessarily reflect the degree of disability experienced by patients with COPD.Citation6,Citation8 While patients may not experience a decline in FEV1 over a particular period of time, they may find nonetheless that it has become harder to walk to the mailbox, a sign of decreased functional capability. One of the hurdles to gleaning associations between clinical measures and patient-reported outcomes is the lack of congruence between accepted lung function measures and measures important to patient well-being and quality of life. Assessment of health status and quality of life improves our understanding of the effects of treatment and the impact of exacerbations.
Exacerbations produce a short-term deterioration in COPD-specific health status and dyspnea, with significant improvement generally following within 10 days.Citation71 Seemungal followed patients for 1 year and showed that those with more exacerbations had significantly worse health-related quality of life (HRQOL) as measured by the SGRQ.Citation8 In addition, dyspnea was not related to exacerbation frequency but was strongly related to HRQOL, indicating the very real effect of symptoms on health status independent of measurable changes in lung function. In a 2-year study of patients with moderate COPD (GOLD stage II), those with 3 or more exacerbations had SGRQ scores that were approximately 2 points higher (indicating worse quality of life) per year than patients with fewer exacerbations, and the biggest changes were associated with the symptom subscale.Citation6 Hospital admissions were also associated with a higher SGRQ score, and it was noted that patients with frequent exacerbations during follow-up had significantly lower HRQOL at baseline, suggesting that these patients were already at increased risk for exacerbation.
Treatment with FSC has resulted in clinically important improvements in health status (). In a 24-week study of 691 patients, the FSC group had a significant increase (improvement) from baseline in mean Chronic Respiratory Disease Questionnaire (CRDQ) score compared to the fluticasone propionate and placebo groups (a change of 10.0 points from baseline for FSC versus 4.8 for fluticasone propionate and 5.0 for placebo).Citation52 In 2 parallel 12-month clinical trials, nighttime awakenings were decreased by approximately 1 awakening per week in the FSC groups, while awakenings increased slightly in the salmeterol groups.Citation51,Citation53 Symptoms and health status in COPD patients generally worsen over time, but the FSC groups in both trials had better dyspnea and SGRQ scores compared to baseline than the salmeterol groups, although the changes in SGRQ scores did not reach the threshold of 4 units considered clinically meaningful. Other trials also have shown improvements in symptoms (generally dyspnea or cough) and HRQOL in patients treated with FSC.Citation36,Citation42,Citation47,Citation50,Citation54,Citation72
Pharmacoeconomic evidence
While randomized clinical trials are important for their strong internal validity in interventional research, they are expensive to conduct and lack generalizability due to restrictive patient inclusion criteria. Observational, real-world studies using administrative claims data are an additional way to answer research questions. These have greater external validity and can be designed so as to reduce selection bias in the absence of randomization. In this section, we describe studies that have examined clinical and economic outcomes using observational, retrospective designs.
The direct costs of medical care for COPD patients are approximately double those for patients without COPD, and reducing exacerbations could significantly lower the economic burden of the disease.Citation73 Retrospective analyses of healthcare claims data suggest that sizable cost savings might be achieved with FSC therapy, primarily through prevention of exacerbation-related hospitalizations.
A study using data from the UK General Practice Database found patients prescribed ICS and LABA had a 38% lower risk for a combined endpoint of hospitalization or death than patients prescribed ICS plus a short-acting beta-agonist (HR 0.62; 95% CI, 0.43 to 0.87).Citation74 Similarly Soriano and colleagues reported that patients discharged with ICS and LABA had a 41% lower risk for rehospitalization or death in the following year compared to patients discharged with a short-acting beta-agonist.Citation18 In the TORCH trial, however, annual hospital admission rates for exacerbations were similar in the FSC and salmeterol groups, but were 17% and 18% lower, respectively, than in the placebo group.Citation54
Cost analyses comparing FSC to ipratropium (alone or in combination with albuterol) show cost benefits as well. Among managed care enrollees, those prescribed ICS plus LABA had a 47% lower risk for a COPD hospitalization (HR 0.533, 95% CI, 0.328 to 0.865) and a 36% lower risk for any respiratory admission compared to ipratropium therapy (HR 0.643; 95% CI, 0.512 to 0.808).Citation75 Newly diagnosed COPD patients receiving initial maintenance therapy with FSC had a 32% lower risk for hospitalization/ED visit during the first 6 months of therapy compared with patients receiving ipratropium therapy (HR 0.685, 95% CI, 0.620 to 0.757), and a lower risk than patients receiving either fluticasone propionate or salmeterol.Citation76 Two US studies, one in a Texas Medicaid population and one in a cohort of Medicare-eligible health plan members, reported 27% and 45% reductions in risk, respectively, for a COPD-related hospitalization or ED visit with FSC compared to ipratropium.Citation73,Citation77 In addition, these analyses found lower overall medical costs for FSC therapy even though FSC was associated with higher pharmacy costs than was ipratropium. A third study, however, found no difference in COPD-related costs between FSC and ipratropium.Citation78
Prescribing considerations
In the United States, 250/50 μg FSC is approved for twice-daily maintenance therapy in COPD to improve lung function and reduce exacerbations.Citation79 In Europe, the approved dose is 500/50 μg and its use in patients with milder COPD (FEV1 ≤ 60% of predicted pre-bronchodilator value and a history of exacerbations) has been approved based primarily on the TORCH study, which found that FSC is associated with a reduced rate of exacerbations, improved lung function and HRQOL, and possibly improved survival.Citation34,Citation54,Citation56
Current evidence-based guidelines recommend the addition of inhaled corticosteroid (ICS) for symptomatic patients with moderate-to-severe disease (FEV1 < 50% predicted) and repeated exacerbations.Citation1,Citation2 It is suggested that a dose sufficient in strength to establish control be chosen, followed by a dose reduction, when appropriate, to a level that maintains control and minimizes deleterious effects. Although 3 exacerbations in 3 years is suggested as a threshold for considering more aggressive therapy, as with other illnesses, good judgment must be exercised in the clinical setting. How is one to treat a patient with FEV1 > 50% predicted and 2 exacerbations in the past year, or 1 very severe exacerbation? Another issue clinicians must consider is the prevention of repeat exacerbations. Should one start patients on FSC sooner, given the clinical evidence for its efficacy and safety in COPD? Or add FSC to other long-acting bronchodilators to slow, if not prevent, the inevitable progression of COPD? A weighing of the risks and benefits, including consideration of the patient’s symptoms and functional status, is especially necessary in treating patients with mild or moderate COPD.
Safety
Treatment with ICS/LABA is generally well tolerated. In most clinical trials, there has been good medication adherence and a lower withdrawal rate due to adverse events in the FSC group compared to the placebo and/or salmeterol groups.Citation42,Citation50–Citation53,Citation56 Oral candidiasis is the most frequent adverse event associated with ICS use. In a recent post hoc safety analysis of TORCH trial data, no significant differences in bone density were seen between the groups receiving study drugs and the placebo group.Citation80 An increased risk of pneumonia has been associated with FSC use. In the largest and longest study to date, the three-year TORCH trial, a higher incidence of pneumonia was seen in the FSC (19.6%) and fluticasone propionate (18.3%) groups than in the salmeterol (13.3%) and placebo (12.3%) groups (all P < 0.001).Citation54 However, there was not a corollary increase in pneumonia-related hospitalizations or deaths in the FSC group. The decrease in the exacerbation rate (−0.28 events/100 patients/year) was greater than the increase in pneumonia (+0.03 events/100 patients/year). A more recent post-hoc analysis of TORCH data reported 88 pneumonia events per 1000 treatment-years for FSC and 84 events per 1000 treatment-years for fluticasone propionate, compared with 52 events per 1000 treatment-years with salmeterol or placebo.Citation81 Factors associated with increased risk for pneumonia included age ≥55 years, FEV1 < 50% predicted, COPD exacerbation in the prior year, a worse dyspnea score and body mass index <25 kg/m2. In addition, a 44-week trial comparing FSC to salmeterol reported that a greater incidence of pneumonia was associated with FSC use (4.5% vs 1.8%).Citation42 The INSPIRE study, a trial of the effects of FSC versus tiotropium on exacerbation rates, found equivalent exacerbation outcomes, but a higher incidence of pneumonia in the FSC group (8% vs 4%; P < 0.01); however, overall mortality was significantly lower in the FSC group.Citation82 The pneumonia data from some trials have been difficult to interpret because pneumonia events were not anticipated when the studies began and so the study protocols did not require that diagnosis be confirmed by chest X-ray. Interestingly, a recent meta-analysis of seven large clinical trials found no differences in pneumonia between patients receiving the ICS budesonide (with or without formoterol) and patients receiving other therapy; pneumonia occurred in 3% of patients in each group.Citation83 Nevertheless, the possibility of a slightly increased risk of pneumonia with ICS or FSC therapy, especially in patients at increased risk for respiratory infection, warrants vigilance.
Multiple morbidities
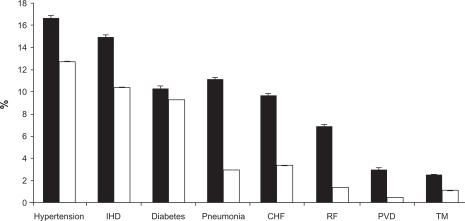
Patients seldom present only with COPD. Many patients have multiple morbidities including asthma, cardiovascular disease, hypercholesterolemia, hypertension, depression, cataracts, osteoporosis and diabetes ().Citation84 Many of these conditions are linked by common risk factors, most notably smoking, and COPD and cardiovascular disease are particularly closely related. Comorbid conditions may account for some of the deterioration in lung health seen in COPD and should be assessed and treated.Citation85 Many patients with COPD are nutritionally depleted, and malnutrition is associated with poor prognosis; dietary counseling and nutritional support have been shown to improve airflow and quality of life.Citation86,Citation87 In the presence of multiple morbidities and comorbid conditions, treatment decisions must be based on the various risks and benefits relative to all of the patient’s health problems.Citation80,Citation85,Citation88 Therapy for one condition, however, may be contraindicated in the presence of a second morbidity, complicating treatment decisions.
Figure 2 Estimated prevalence of hospital discharges with selected comorbidities in patients with and without COPD.
Abbreviations: IHD, ischemic heart disease; CHF, congestive heart failure; RF, respiratory failure; PVD, pulmonary vascular disease; TM, thoracic malignancy. Reprinted with permission from Holguin F, Folch E, Redd SC, Mannino DM. Comorbidity and mortality in COPD-related hospitalizations in the United States, 1979 to 2001. Chest. 2005;128(4):2005–2011.Citation84 Copyright © 2005 American College of Chest Physicians.
Given the high prevalence of osteoporosis in patients with COPD, concern has been raised about the long-term effects of ICS on bone density. A recent analysis of data from the TORCH trial found that 18% of men and 30% of women had osteoporosis and 42% of men and 41% of women had low bone density at baseline.Citation80 However, no significant changes in bone mineral density were observed in any of the treatment arms (FSC, fluticasone propionate, salmeterol, placebo) during 3 years of follow-up. Rates of fractures across treatment groups were also low, with no differences detected between groups. Smoking, lack of calcium and vitamin D, and a sedentary lifestyle contribute significantly to low bone density, and these areas present opportunities for lowering osteoporosis risk in patients with COPD. Therapy for COPD with ICS should not necessarily be ruled out in the case of a patient with low bone density, as more aggressive therapy might improve functional status enough to permit a patient to be more active, not only reducing osteoporosis risk but impacting favorably on the course of COPD and other morbidities, such as hypertension and cardiovascular disease. With appropriate pharmacotherapy, a patient might also be better able to participate in pulmonary rehabilitation, an intervention that may not only improve physical functioning and symptom management, but reduce depression, a common problem in patients with COPD.Citation89–Citation91
There has also been concern that ICS therapy in COPD patients with diabetes may make glycemic control more difficult. However, a small study (N = 12) of the effect of ICS on glucose control in patients with COPD and diabetes found no significant change in hemoglobin A1c over 6 weeks of therapy.Citation92 It appears prudent to carefully monitor patients for changes in glycemic control following ICS or FSC therapy.
Adherence issues
Finally, in making therapy decisions, treatment acceptance and adherence to treatment must be considered, since no medication regimen is effective if the medication is not taken. Increased adherence to COPD inhaled therapy is associated with improved mortality and reduced hospitalization.Citation93 Patient adherence to treatment regimens in COPD is not optimal and treatment persistence is generally low for inhaled medications.Citation94,Citation95 Poor adherence can be related to overuse, underuse, or improper use of a medicine, and any of these problems may be sporadic or systematic, intentional or unintentional.Citation94 Unintentional non-adherence is particularly an issue with inhaled medication; one study reported that only 43% of patients used a metered-dose inhaler (MDI) correctly, 55% used an MDI plus spacer correctly, and 59% used a dry powder inhaler correctly.Citation96 Patients make mistakes even directly following face-to-face instruction, underscoring the importance of physician’s attentiveness to patients’ inhaler technique.Citation95 As a routine part of office visits, adherence needs to be assessed in a neutral manner and addressed collaboratively to improve therapeutic outcomes.
The feasibility of using combination ICS/LABA therapy has improved with the availability of single inhaler devices that contain both medications, and this may also improve patient adherence, in part because salmeterol provides symptom relief, making it more likely that patients will comply with scheduled dosing regimens.Citation97 In a 12-month period, patients with COPD who were prescribed FSC obtained more refills than patients prescribed salmeterol or ICSCitation76 and in a second study of pharmacy claims, medication compliance was 12% higher with FSC than with ipratropium.Citation78 Thus, when both ICS and LABA are needed, FSC delivered via a single inhaler may result in better treatment adherence.Citation94,Citation97
Just as important as optimizing patient adherence to pharmacotherapy is the need to bridge the existing gap between optimal management of COPD and actual practice. An existing hurdle to overcome is the frequent failure to recognize that smoker’s cough and bronchitis are in reality COPD and exacerbations of COPD.Citation98 Simply put, if clinicians do not correctly identify the patient’s condition as COPD, there is little chance the disease will be treated according to existing guidelines for care. Use of a simple questionnaire may be beneficial for screening for COPD in primary care patients.Citation98,Citation99 In addition, increased awareness that the course of COPD and patient’s quality of life can be significantly improved by newer maintenance therapies and patient self-management education is needed. Undertreatment of COPD is common and being recognized.Citation88 A study of Canadian patients with COPD found that 33% had never received a written action plan and 67% had not been told how to prevent an exacerbation.Citation100 Several concerns about potential side effects with ICS have been allayed by new research, and there is a need to educate physicians about the benefits and risks of COPD maintenance therapies, including treatment with FSC, as well as the need for vigilance regarding untoward effects. Other barriers to optimal care, such as formulary decisions that limit the clinician’s ability to do what is best for the patient, will require health policy changes.
Lessons for the future
In appropriate patients, FSC is an effective therapy option that has been shown to reduce the frequency of exacerbations in patients with COPD, modestly improve lung function, and improve dyspnea, health status and quality of life. A range of studies suggests that fluticasone propionate and salmeterol have synergistic effects when administered together that improve their efficacy in controlling symptoms and reducing exacerbations. While clinical trials have clearly shown a benefit of FSC in preventing exacerbations in Stage III and IV COPD, there is also some evidence of benefit in patients with moderate COPD, and this topic warrants further research. Investigations of the optimal doses of FSC and comparative studies of the clinical and pharmacoeconomic benefits of FSC relative to other medications for COPD maintenance therapy are also needed. In particular, additional studies to clarify the potential value of triple therapy with FSC and tiotropium would be beneficial, and research in this area is underway.
For both the clinician and patient, the optimal scenario would be to have available a range of therapeutic options that meet the needs of patients with differing symptoms, lung function profiles, and comorbidities, that improve quality of life, and that minimize adherence issues and deleterious effects. Treatment with FSC within the context of COPD maintenance therapy is a useful, effective option in the clinician’s armamentarium, which based on evidence to date appears to have benefits for disease management, cost, adherence, and quality of life.
Disclosures
BPY has received research funding for COPD studies from GSK, Novartis and NIH. IR and AAD are employees of GlaxoSmithKline (GSK); AAD owns GSK company stock. JSH has received financial compensation from GSK for medical writing services and research funding for COPD studies from Boehringer Ingelheim, GSK, Pfizer Global Pharmaceuticals, and SmithKlineBeecham Pharmaceuticals.
References
- CelliBRMacNeeWATS/ERS Task ForceStandards for the diagnosis and treatment of patients with COPD: a summary of the ATS/ERS position paperEur Respir J200423693294615219010
- Global Initiative for Chronic Obstructive Lung Disease (GOLD)Global Strategy for Diagnosis, Management and Prevention of COPD. Updated 2009Gig Harbor, WAMedical Communications Resources, Inc2009http://www.goldcopd.com
- DonaldsonGCSeemungalTABhowmikAWedzichaJARelationship between exacerbation frequency and lung function decline in chronic obstructive pulmonary diseaseThorax2002571084785212324669
- SeemungalTADonaldsonGCBhowmikAJeffriesDJWedzichaJATime course and recovery of exacerbations in patients with chronic obstructive pulmonary diseaseAm J Respir Crit Care Med200016151608161310806163
- BourbeauJFordGZackonHPinskyNLeeJRubertoGImpact on patients’ health status following early identification of a COPD exacerbationEur Respir J200730590791317715163
- MiravitllesMFerrerMPontAEffect of exacerbations on quality of life in patients with chronic obstructive pulmonary disease: a 2 year follow up studyThorax200459538739515115864
- NishimuraKSatoSTsukinoMEffect of exacerbations on health status in subjects with chronic obstructive pulmonary diseaseHealth Qual Life Outcomes200976919624834
- SeemungalTADonaldsonGCPaulEABestallJCJeffriesDJWedzichaJAEffect of exacerbation on quality of life in patients with chronic obstructive pulmonary diseaseAm J Respir Crit Care Med19981575 Pt 1141814229603117
- SpencerSCalverleyPMBurgePSJonesPWImpact of preventing exacerbations on health status in chronic obstructive pulmonary diseaseEur Respir J200423569870215176682
- DonaldsonGCWedzichaJACOPD exacerbations: 1: epidemiologyThorax200661216416816443707
- Soler-CatalunaJJMartinez-GarciaMARoman-SanchezPRSalcedoENavarroMOchandoRSevere acute exacerbations and mortality in patients with chronic obstructive pulmonary diseaseThorax2005601192593116055622
- BurgeSWedzichaJACOPD exacerbations: definitions and classificationsEur Respir J200321Suppl 4146s53s
- SethiSEvansNGrantBJMurphyTFNew strains of bacteria and exacerbations in chronic obstructive pulmonary diseaseN Engl J Med2002347746547112181400
- SethiSSethiREschbergerKAirway bacterial concentrations and exacerbations of chronic obstructive pulmonary diseaseAm J Crit Clin Care Med20071764356361
- BaathornEKerstjensHPostmaDTimensWMacNeeWAirways inflammation and treatment during acute exacerbations of COPDInt J Chron Obstruct Pulmon Dis20083221722918686731
- DonaldsonGCSeemungalTAPatelISLongitudinal changes in nature, severity and frequency of COPD exacerbationsEur Respir J200322693193614680081
- HurstJRDonaldsonGCQuintTKBoldringJJBaghai-RavaryRWedzichaJATemporal clustering of exacerbations in chronic obstructive pulmonary diseaseAm J Respir Crit Care Med2009179536937419074596
- SorianoJBKiriVAPrideNBVestboJInhaled corticosteroids with/without long-acting beta-agonists reduce the risk of rehospitalization and death in COPD patientsAm J Respir Med200321677414720023
- BahadoriKFitzGeraldJMLevyRDFeraTSwistonJRisk factors and outcomes associated with chronic obstructive pulmonary disease exacerbations requiring hospitalizationsCan Respir J2008164e43e4919707601
- LeffBBurtonLMaderSLHospital at home: feasibility and outcomes of a program to provide hospital-level care at home for acutely ill older patientsAnn Int Med20051431179880816330791
- ColeCSWilliamsEBWilliamsRDAssessment and discharge planning for hospitalized older adults with deliriumMedsurg Nurs2006152717616700244
- Gruffydd-JonesKA national strategy for the management of chronic obstructive pulmonary disease in England: aiming to improve the quality of care for patientsPrim Care Respir J200817Suppl 1S1S819137200
- StrasselsSASmithDHSullivanSDMahajanPSThe costs of treating COPD in the United StatesChest2001119234435211171708
- NiewoehnerDEThe impact of severe exacerbations on quality of life and the clinical course of chronic obstructive pulmonary diseaseAm J Med200611910 Suppl 1384516996898
- StanfordRHShenYMcLaughlinTCost of chronic obstructive pulmonary disease in the emergency department and hospitalTreat Respir Med20065534334916928147
- BlanchetteCMBroderMOryCChangeEAkazawaMDalalAACost and utilization of COPD and asthma among insured adults in the USCurr Med Res Opin2009251385139219419342
- ShayaFTDongyiDAkazawaMOBurden of concomitant asthma and COPD in a Medicaid populationChest20081341141918339789
- Simoni-WastiliLBlanchetteCMQianJBurden of chronic obstructive pulmonary disease in Medicare beneficiaries residing in long-term care facilitiesAm J Ger Pharmacother200975262270
- ReisALBauldoffGSCasaburiRMahlerDARochesterCLHerreriasCPulmonary rehabilitation. Joint ACCP/AACVR evidence-based clinical practice guidelinesChest200713154S42S17494825
- SundararajanLBalamiJPackhamSEffectiveness of outpatient pulmonary rehabilitation in elderly patients with chronic obstructive pulmonary diseaseJ Cardiopulm Rehabil Prev20091125, doi: 101097/HCR0b013e3181be7c56 [epub ahead of print].
- AnthonisenNRConnettJEKileyJPEffects of smoking intervention and the use of an inhaled anticholinergic bronchodilator on the rate of decline of FEV1. The Lung Health StudyJAMA199427219149715057966841
- WilkinsonTMADonaldsonGCHurstJRSeemungalTARWedzichaJAEarly therapy improves outcomes of exacerbations of chronic obstructive pulmonary diseaseAm J Respir Crit Care Med2004169121298130314990395
- BroedersMSanchisJLevyMLCromptonGKDekhuijzenPNfor the ADMIT Working GroupThe ADMIT series – issues in inhalation therapy. 2) improving technique and clinical effectivenessPrim Care Respir J2009182768219475324
- HananiaNAThe impact of inhaled corticosteroid and long-acting B-agonist combination therapy on outcomes in COPDPulm Pharmacol Ther200821354055018280761
- KeatingGMMcCormackPLSalmeterol/fluticasone propionate. A review of its use in the treatment of chronic obstructive pulmonary diseaseDrugs200767162383240517983257
- HananiaNADarkenPHorstmanDThe efficacy and safety of fluticasone propionate (250 microg)/salmeterol (50 microg) combined in the Diskus Inhaler for the treatment of COPDChest2003124383484312970006
- Di MarcoFMilic-EmiliJBoveriBEffect of inhaled broncho-dilators on inspiratory capacity and dyspnoea at rest in COPDEur Respir J2003211869412570114
- CalverleyPMAReducing the frequency and severity of exacerbations of chronic obstructive pulmonary diseaseProc Am Thorac Soc20041212112416113424
- OakleyRHCidlowskiJAHomologous down regulation of the glucocorticoid receptor: the molecular machineryCrit Rev Eukaryot Gene Expr19933263888324294
- ChungKFCaramoriGAdcockIMInhaled corticosteroids as combination therapy with β-adrenergic agonists in airways disease: present and futureEur J Clin Pharmacol200965985386119557399
- BarnesNCQiuY-SPavordIDAnti-inflammatory effects of salmeterol/fluticasone propionate in chronic obstructive pulmonary diseaseAm J Respir Crit Care Med2006173773674316424444
- KardosPWenchkerMGlaabTVogelmeierCImpact of salmeterol/fluticasone propionate versus salmeterol on exacerbations in severe chronic obstructive pulmonary diseaseAm J Respir Crit Care Med2007175214414917053207
- HattotuwaKLGizyckiMJAnsariTWJefferyPKBarnesNCThe effects of inhaled fluticasone on airway inflammation in chronic obstructive pulmonary diseaseAm J Resp Crit Care Med2002165121592159612070058
- GizyckiMJHattotuwaKLBarnesNJefferyPKEffects of fluticasone propionate on inflammatory cells in COPD: an ultrastructural examination of endobronchial biopsy tissueThorax200257979980312200525
- ConfalonieriMMainardiEDella PortaRInhaled corticosteroids reduce neutrophilic inflammation in patients with chronic obstructive pulmonary diseaseThorax19985375835859797758
- SinDDLacyPYorkPManSFPEffects of fluticasone on systemic markers of inflammationAm J Respir Crit Care Med20041707160165
- Dal NegroRWPomariCTognellaSMichelettoCSalmeterol and fluticasone 50 μg/250 μg bid in combination provides a better long-term control than salmeterol 50 μg bid alone and placebo in COPD patients already treated with theophyllinePulm Pharmacol Ther200316424124612850128
- EdwardsMJohnsonMJohnsonSSynergistic effects of salmeterol and fluticasone in human rhinovirus induced pro-inflammatory cytokine production [abstract]Am J Respir Crit Care Med2003167A399
- SeetoLJBurgessJKJohnsonPRBlackJLRothMLimSEffect of fluticasone and salmeterol on human alveolar macrophage cytokine production in patients with chronic obstructive pulmonary disease (COPD) [abstract]Am J Respir Crit Care Med2003167A318
- CalverleyPPauwelsRVestboJCombined salmeterol and fluticasone in the treatment of chronic obstructive pulmonary disease: a randomized clinical trial [Erratum in: Lancet. 2003;351(9369);1660]Lancet2003361935644945612583942
- FergusonGTAnzuetoAFeiREmmettAKnobilKKalbergCEffect of fluticasone propionate/salmeterol (250/50 μg) or salmeterol (50 μg) on COPD exacerbationsRespir Med200810281099110818614347
- MahlerDAWirePHorstmanDEffectiveness of fluticasone propionate and salmeterol combination delivered via the Diskus device in the treatment of chronic obstructive pulmonary diseaseAm J Respir Crit Care Med200216681084109112379552
- AnzuetoAFergusonGTFeldmanGEffect of fluticasone propionate/salmeterol (250/50) on COPD exacerbations and impact on patient outcomesCOPD20096532032919863361
- CalverleyPMAndersonJACelliBSalmeterol and fluticasone propionate and survival in chronic obstructive pulmonary diseaseN Engl J Med2007356877578917314337
- LapperreTSSnoeck-StrobandJBGosmanMMEthe GLU-COLD (Groningen Leiden Universities Corticosteroids in Obstructive Lung Disease) Study GroupEffect of fluticasone with and without salmeterol on pulmonary outcomes in chronic obstructive pulmonary diseaseAnn Int Med2009151851752719841453
- CelliBRThomasNEAndersonJAEffect of pharmacotherapy on rate of decline of lung function in COPD: results from the TORCH StudyAm J Respir Crit Care Med2008178432232318676961
- WoutersEFPostmaDSFokkensBfor the COSMIC (COPD and Seretide: a Multi-Center Intervention and Characterization) Study GroupWithdrawal of fluticasone propionate from combined salmeterol/fluticasone treatment in patients with COPD causes immediate and sustained disease deterioration: a randomised controlled trialThorax200560648048715923248
- AlsaeediASinDDMcAlisterFAThe effects of inhaled corticosteroids in chronic obstructive pulmonary disease: a systematic review of randomized placebo-controlled trialsAm J Med20021131596512106623
- BurgePSCalverleyPMJonesPWSpencerSAndersonJAMaslenTKRandomised, double blind, placebo controlled study of fluticasone propionate in patients with moderate to severe chronic obstructive pulmonary disease: the ISOLDE trialBMJ200032072451297130310807619
- Lung Health Study Research GroupEffect of inhaled triamcinolone on the decline in pulmonary function in chronic obstructive pulmonary diseaseN Engl J Med343261902190911136260
- PaggiaroPLDahleRBakranIFrithLHollingsworthKEfthimiouJMulticenter randomized placebo-controlled trial of inhaled fluticasone propionate in patients with chronic obstructive pulmonary disease. [Erratum in: Lancet. 1998;351(9120):1968]Lancet199835191057737809519948
- SzafranskiWCukierARamirezAEfficacy and safety of budesonide/formoterol in the management of chronic obstructive pulmonary diseaseEur Resp J20032157481
- JenkinsCRJonesPWCalverleyPMEfficacy of salmeterol/fluticasone propionate by GOLD stage of chronic obstructive pulmonary disease: analysis from the randomized, placebo-controlled TORCH studyResp Res20091059
- YoungJUnderstanding statistical analysis in the surgical literature: some key conceptsANZJ Surg2009795398403
- SinDDWuLAndersonJAInhaled corticosteroids and mortality in chronic obstructive pulmonary diseaseThorax2005601299299716227327
- MapelDWHurleyJSRoblinDSurvival of COPD patients using inhaled corticosteroids and long-acting beta agonistsRespir Med2006100459560916199151
- MapelDWNelsonLSLydickESorianoJYoodMUDavisKJSurvival among COPD patients using fluticasone/salmeterol in combination versus other inhaled steroids and bronchodilators aloneCOPD20074212713417530506
- SinDDTuJVInhaled corticosteroids and the risk of mortality and readmission in elderly patients with chronic obstructive pulmonary diseaseAm J Respir Crit Care Med2001164458058411520719
- SorianoJBVestboJPrideNBKiriVMadenCMaierWCSurvival in COPD patients after regular use of fluticasone propionate and salmeterol in general practiceEur Respir J200220481982512412670
- FanVSBrysonCLCurtisJRInhaled corticosteroids in chronic obstructive pulmonary disease and risk of death and hospitalization: time-dependent analysisAm J Respir Crit Care Med2003168121488149414525798
- AaronSDVandemheenKLClinchJJMeasurement of short-term changes in dyspnea and disease-specific quality of life following an acute COPD exacerbationChest2002121368869611888946
- ZhengJPYangLWuYMThe efficacy and safety of combination salmeterol (50 μg)/fluticasone propionate (500 μg) inhalation twice daily via Accuhaler in Chinese patients with COPDChest200713261756176317951625
- RascatiKLAkazawaMJohnsrudMStanfordRHBlanchetteCMComparison of hospitalizations, emergency department visits, and the associated costs in a historical cohort of Texas Medicaid patients with chronic obstructive pulmonary disease, by initial medication regimenClin Ther20072961203121317692734
- KiriVABettoncelliGTestiRViegiGInhaled corticosteroids are more effective in COPD patients when used with LABA than with SABARespir Med20059991115112415921904
- AnzuetoAMcLaughlinTStanfordRHInitial treatment regimen and risk of hospitalization in patients with chronic obstructive pulmonary diseaseCOPD20041220521417136988
- AkazawaMHayflingerDCStanfordRHBlanchetteCMEconomic assessment of initial maintenance therapy for chronic obstructive pulmonary disease from a managed care perspectiveAm J Managed Care20081472132
- BlanchetteCMAkazawaMDalalASimoni-WastilaLRisk of hopitalizations/emergency department visits and treatment costs associated with initial maintenance therapy using fluticasone propionate 500 microg/salmeterol 50 microg compared with ipratropium for chronic obstructive pulmonary disease in older adultsAm J Geriatr Pharmacother20086313814618775388
- DeleaTEHagiwaraMDalalAAStanfordRHBlanchetteCMHealthcare use and costs in patients with chronic bronchitis initiating maintenance therapy with fluticasone/salmeterol vs other inhaled maintenance therapiesCurr Med Res Opin200935111319210134
- Advair DISKUS [package insert]Research Triangle Park, NCGlaxo-SmithKline42009
- FergusonGTCalverleyPMAndersonJAPrevalence and progression of osteoporosis in patients with COPD. Results from TORCHChest200913661456146519581353
- CrimCCalverleyPMAndersonJAPneumonia risk in COPD patients receiving inhaled corticosteroids alone or in combination. TORCH study resultsEur Resp J2009343641647
- WedzichaJACalverleyPMSeemungalTAHaganGAnsariZStockleyRAfor the INSPIRE InvestigatorsThe prevention of chronic obstructive pulmonary disease exacerbations by salmeterol/fluticasone propionate or tiotropium bromideAm J Respir Crit Care Med20081771192617916806
- SinDDTashkinDZhangXBudesonide and the risk of pneumonia: a meta-analysis of individual patient dataLancet2009374969171271919716963
- HolguinFFolchEReddSCManninoDMComorbidity and mortality in COPD-related hospitalizations in the United States, 1979 to 2001Chest200512842005201116236848
- TanSLWoodAMChronic obstructive pulmonary disease and comorbidity: a review and consideration of pathophysiologyPanminerva Med2009512819319776710
- WeekesCEEmeryPWEliaMDietary counselling and food fortification in stable COPD: a randomised trialThorax200964432633119074931
- PlanasMAlvarezJGarcia-PerisPANutritional support and quality of life in stable chronic obstructive pulmonary disease (COPD) patientsClin Nutr200524343344115896431
- BarrRGCelliBRManninoDMComorbidities, patient knowledge, and disease management in a national sample of patients with COPDAm J Med2009122434835519332230
- CoventryPADoes pulmonary rehabilitation reduce anxiety and depression in chronic obstructive pulmonary disease?Curr Opin Pulm Med200915214314919532030
- OmachiTAKatzPPYelinEHDepression and health-related quality of life in chronic obstructive pulmonary diseaseAm J Med20091228778.e9e1519635280
- SchneiderCJickSSBothnerUMeierCRChronic obstructive pulmonary disease and the risk of depressionChest2009103;doi: 101378/chest09-0614 [Epub ahead of print].
- FaulJLWilsonSRChuJWCanfieldJKuschnerWGThe effects of an inhaled corticosteroid on glucose control in type 2 diabetesClin Med Res200971–2142019251584
- VestboJAndersonJACalverleyPAdherence to inhaled therapy, mortality, and hospital admission in COPDThorax2009641193994319703830
- CramerJABradley-KennedyCScaleraATreatment persistence and compliance with medications for chronic obstructive pulmonary diseaseCan Respir J2007141252917315055
- RestrepoRDAlvarezMTWittnebelLDMedication adherence issues in patients treated for COPDInt J Chron Obstruct Pulm Dis200833371384
- BrocklebankDRamFComparison of the effectiveness of inhaler devices in asthma and chronic obstructive airways disease: a systematic review of the literatureHealth Tech Assess20015261149
- CazzolaMHananiaNAThe role of combination therapy with corticosteroids and long-acting beta-2-agonists in the prevention of exacerbations in COPDInt J Chron Obstruct Pulmon Dis20061434535418044091
- YawnBPKeenanJMCOPD – the primary care perspective: addressing epidemiology, pathology, diagnosis, treatment of smoking’s multiple morbidities and the patient’s perspectiveCOPD200741678317364679
- PriceDBTinkelmanDGNordykeRJIsonakaSHalbertRJCOPD Questionnaire Study GroupScoring system and clinical application of COPD diagnostic questionnairesChest200612961531153916778271
- HernandezPBalterMBourbeauJHodderRLiving with chronic obstructive pulmonary disease: a survey of patients’ knowledge and attitudesRespir Med200910371004101219269150