Abstract
Background
Inflammation increases during exacerbations of COPD, but only a few studies systematically assessed these changes. Better identification of these changes will increase our knowledge and potentially guide therapy, for instance by helping with quicker distinction of bacterially induced exacerbations from other causes.
Aim
To identify which inflammatory parameters increase during COPD exacerbations compared to stable disease, and to compare bacterial and non-bacterial exacerbations.
Methods
In 45 COPD patients (37 male/8 female, 21 current smokers, mean age 65, FEV1 52% predicted, pack years 38) sputum was collected during a stable phase and subsequently during an exacerbation.
Results
Sputum total cell counts (9.0 versus 7.9 × 106/mL), eosinophils (0.3 versus 0.2 × 106/mL), neutrophils (6.1 versus 5.8 × 106/mL), and lymphocytes (0.07 versus 0.02 × 106/mL) increased significantly during an exacerbation compared to stable disease. A bacterial infection was demonstrated by culture in 8 sputum samples obtained during an exacerbation. These exacerbations had significantly increased sputum total cell and neutrophil counts, leukotriene-B4, myeloperoxidase, interleukin-8 and interleukin-6, and tumor necrosis factor-α (TNF-α) levels, and were also associated with more systemic inflammation compared to exacerbations without a bacterial infection. Sputum TNF-α level during an exacerbation had the best test characteristics to predict a bacterial infection.
Conclusion
Sputum eosinophil, neutrophil, and lymphocyte counts increase during COPD exacerbations. The increase in systemic inflammation during exacerbations seems to be limited to exacerbations caused by bacterial infections of the lower airways. Sputum TNF-α is a candidate marker for predicting airway bacterial infection.
Introduction
The frequent occurrence of exacerbations is an important feature of chronic obstructive pulmonary disease (COPD). The impact of exacerbations on a patient’s health is large since they are remarkably closely linked to quality of life, accelerated lung function loss, and to mortality.Citation1,Citation2 There is also a huge impact on society since the direct costs to the health care system associated with the management of acute exacerbations of COPD are enormous.Citation3 Notwithstanding this, there is still no universally accepted defini-tion of a COPD exacerbation though several have been proposed.Citation4–Citation7 All definitions of exacerbation focus on symptoms, sometimes in combination with infectious etiology and/or airway obstruction, but remarkably, none of the definitions make any reference to changes or increases in inflammation. This is especially relevant since inflammation is part of the definition of COPD,Citation6 and most clinicians hold the general perception that exacerbations are associated with changes in airway inflammation.
There is limited understanding of the causes of exacerbations, and, linked to this of the optimal treatment in relation to the cause. This has resulted in large international differences in the prescription levels of most notably antibiotics, given the lack of sufficient guidance to prescribe antibiotics or none. This is partially due to the fact that results of sputum cultures have quite a delay before test results are known. Thus a quicker detection of bacterial infections during COPD exacerbations should also lead to improvements in clinical care by aiding in the decision whether to start antibiotics. A few markers have been proposed, such as C-reactive protein (CRP), and procalcitonin,Citation8,Citation9 but none have good test characteristics or have gained wide acceptance so far.
The aim of the current study is to identify which inflammatory parameters are increased in induced sputum and in blood during COPD exacerbations compared to a stable phase of the disease, and specifically to assess which parameters change during a bacterial exacerbation. Some of the present results have been described in the form of an abstract.Citation10
Methods
Patients with a diagnosis of COPD were included if age >40 years, post-bronchodilator forced expiratory flow in the first second (FEV1) <85% predicted and >0.7 L, postbronchodilator FEV1/slow inspiratory vital capacity (IVC) <predicted normal (<88% predicted in men and <89% predicted in women),Citation11 and were current or ex smokers. Patients were not allowed to use oral corticosteroids, long-acting anticholinergics, beta-blockers, or long term oxygen therapy, have a history of asthma, or a significant other disease that could interfere with results of the study. The local medical ethics committee approved the study. A written informed consent was obtained from all patients prior to the study.
Study design
In case inhaled corticosteroids (ICS) were being used at inclusion, they were discontinued. Thereafter subjects had to be stable for 2 months. At the second visit, 2 months later, spirometry was performed followed by sputum induction; these measures were used as baseline, stable phase values in the study. From the second visit until the end of the randomized treatment period, all long-acting beta2-sympaticomimetics were also withdrawn. Patients were asked to contact the research doctor, who was available around the clock, to report any deterioration in symptoms for which they would normally contact their primary care physician or pulmonologist. An exacerbation was defined as a history of increased breathlessness and at least two of the following symptoms for 24 hours or more: increased cough frequency or severity, sputum volume or purulence, and wheeze. When presenting with an exacerbation, patients were randomized provided postbronchodilator FEV1 was <70% of predicted and PaO2 > 8.0 kPa. After this, a randomized controlled trial followed (data not shown).
Measurements
At each visit, sputum induction, blood sampling, and lung function measurements were performed. FEV1 and IVC were measured according to the guidelines of the European Respiratory Society.Citation12
Health status was measured by the Clinical COPD Questionnaire.Citation13
Sputum induction and processing
Sputum was induced by standard methods with modifications according to Pizzichini.Citation14 Whole sputum samples were processed within 120 minutes as described previously.Citation15 Cytospins were prepared and cell-free supernatant was collected and stored in aliquots at −80 °C pending analyses of soluble mediators.
Differential cell counts were counted on May Grünwald Giemsa stained cytospins in a blinded fashion.Citation16 Cell counts were expressed as percentage of non-squamous cells. A sputum sample was considered inadequate when the percentage squamous cells was >80%.
The following soluble mediators were measured in sputum supernatant by ELISA: leukotriene-B4 (LTB4, Amersham Biosciences, UK), eosinophilic cationic protein (ECP, Pharmacia, Uppsala, Sweden), myeloperoxidase (MPO, homemadeCitation17). Albumin in sputum and blood was measured by nephelometry (Dade Behring, Leusden, the Netherlands). Sputum interleukin-6 (IL-6), IL-8, tumor necrosis factor-α (TNF-α), monocyte chemoattractant protein-1 (MCP-1), and both serum IL-6 and TNF-α were measured by xMAP technology (Luminex B.V., Oosterhout, the Netherlands), using multiplex immunoassay kits obtained from Linco, St Charles, USA.
Bacterial culturing
Spontaneous sputum samples were cultured. A bacterial cause of exacerbation was defined by the following features: the cultured micro-organisms are potentially pathogenic, the growth density in the culture is high (semi quantitative), the number of squameous epithelial cells is <25, and the number of the leukocytes in the Gram-stained preparation of the sputum sample is >15 per high power field (100 × 10), which corresponds with Geckler group 4–6).Citation18
Sputum cytokine mRNA expression
Messenger ribonucleic acid (mRNA) was harvested from 1 million viable non-squamous sputum cells. RNA was isolated using a Qiagen RNeasy mini kit (Venlo, The Netherlands) and cDNA was synthesized as described.Citation19 Expression of cytokine mRNA was analyzed by quantitative real-time PCR, using the ABI 7900 HT system (Applied Biosystems, Nieuwekerk a/d IJssel, The Netherlands). The gene expression assays for hemoxygenase-1 (HO-1), TNF-α, chemotactic cytokine ligand5 (CCL5), IL-5, IL-10, IL-12, IL-13, transforming growth factor-β (TGF-β), interferon-γ (IFN-γ), and β-2-microglobulin, were obtained from Applied Biosystems (Nieuwekerk a/d IJssel, Netherlands). Cytokine gene expression was normalized to the expression of β-2-microglobulin. The mRNA quantification is expressed in threshold cycle values (Ct-values), which is the number of amplification cycles to reach a detectable mRNA amount. Thus lower Ct-values correspond with higher mRNA expression.
Blood analyses
Blood differential counts were analyzed by flow cytometry (Coulter-STKS, Beckman Coulter, Miami, USA). Serum C-Reactive Protein (CRP) and albumin were measured by nephelometry (Dade Behring, Leusden, the Netherlands).
Statistical analysis
Data are expressed as medians and inter quartile ranges (IQR). Non-normally distributed parameters were normalized by log10 transformation. Stable phase levels of inflammatory parameters were compared to exacerbation levels using paired sample t-tests, or Wilcoxon log rank tests. Exacerbations with and without a bacterial infection were compared with respect to both the cross-sectional values at exacerbation and the differences in the percentage change of biomarkers from baseline to exacerbation (t-tests or Mann-Witney U-test). Using Receiver Operating Curves, cut-off points for the biomarkers were adjusted until the highest area under the curve was reached. Data were analyzed using SPSS version 12.0.2.
Results
We included 114 patients in this study. Some patients did not sustain corticosteroid withdrawal, or did not remain stable in the run in period (n = 9), other patients did not report an exacerbation (n = 26), or were excluded due to an adverse event (n = 4), or due to various other reasons (n = 30). The remaining 45 patients reporting an exacerbation within the study period were analyzed. The baseline characteristics of these patients are presented in . During the exacerbation, patients had a significantly and clinically relevant poorer health status as measured by higher CCQ scores compared to the stable phase (median value 2.5 versus 1.7 respectively, p < 0.01). The minimal clinically important difference of the CCQ is 0.4.Citation20
Table 1 Patient characteristics of the patients who had an exacerbation during the trial (n = 45), and of the total study population (n = 114)
Inflammatory indices
Sputum samples were adequate in both the stable phase, after ICS withdrawal, and during exacerbation in 41 out of 45 patients. The cellular differences between the stable phase (2 months after ICS withdrawal) and during the exacerbation are presented in . Sputum total cell, eosinophil, neutrophil, and lymphocyte counts were significantly increased at exacerbation versus stable disease.
Table 2 Cellular inflammatory parameters
Analyses of mRNA levels in sputum showed a lower IL-12a expression at exacerbation compared to stable state values (median ct-values 41.5 versus 37.7 respectively; p = 0.051). No differences were found in sputum mRNA levels of HO-1, TNF-α, IL-5, CCL5, IL-10, IL-12b, IL-13, TGF-β, and INF-γ (data not shown). The sputum protein levels of ECP, MCP-1, and LTB-4, were significantly increased at exacerbation compared to stable state and levels of MPO and IL-8 tended to be increased ().
Table 3 Inflammatory biomarkers
Systemic inflammation during COPD exacerbations was increased compared to the stable phase, ie, blood leukocyte and neutrophil counts were significantly increased (), as were serum protein levels of IL-6 (). There was a trend towards an increase in CRP (p = 0.07).
Bacterial cultures
Eight sputum samples for bacterial culture during exacerbation of COPD were missing: 5 patients produced too small a volume of spontaneous sputum, and 3 samples were missing due to logistical problems. Eight of the remaining 37 sputum samples were indicative of a bacterial infection: 5 with Haemophilus influenzae, 2 with Moraxella catarrhalis, and 1 with Streptococcus pneumoniae. These patients had a negative culture in stable phase. In stable phase, 10 patients produced too small a volume of spontaneous sputum and 1 was missing due to logistical problems. Two of the remaining 34 samples were indicative of a bacterial infection (H. influenzae and combination of H. influenzae and M. catarrhalis). These 2 patients had a negative culture during exacerbation.
Differences between bacterial and non-bacterial exacerbations
shows the differences between bacterial and non-bacterial exacerbations both cross-sectionally at the exacerbation visit, and as a change from baseline with stable disease to the exacerbation in order to correct for stable phase values.
Table 4a Differences between bacterial and non-bacterial exacerbations (sputum parameters)
Table 4b Differences between bacterial and non-bacterial exacerbations (blood parameters)
Bacterial exacerbations were accompanied by higher values for sputum total cell and neutrophil counts, LTB4, MPO, IL-8, and TNF-α level than non bacterial exacerbations. In serum, bacterial exacerbations were associated with higher total leukocytes and neutrophil counts. Additionally, when analyzed as the percentage change from baseline to exacerbation, serum CRP and IL-6 levels showed a significantly larger increase when a bacterial exacerbation occurred compared to exacerbations without a bacterial infection.
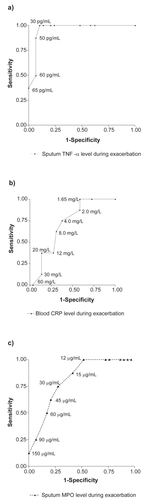
The predictive values of the level of blood CRP, sputum TNF-α and sputum MPO for a bacterial cause of the exacerbation are presented in Receiver Operating Curves (). Sputum TNF-α had the best test characteristics.
Figure 1 Receiver operating characteristic curves for distinguishing a bacterial cause of exacerbations with inflammatory markers. On the curve, several biomarker concentration levels are presented, which provides an indication for optimal cut-off points and their corresponding predictive values. a) sputum tumor necrosis factor-α (TNF-α), b) blood C-reactive protein (CRP), c) sputum myeloperoxidase (MPO).
Discussion
The present study assessed the change in inflammation from a stable phase of COPD to an out-patient COPD exacerbation. Eight patients had a sputum sample indicative of a bacterial infection. None of these patients had a positive culture in stable phase. Sputum neutrophil, lymphocyte, and eosinophil numbers increased during an exacerbation. Furthermore, systemic inflammation increased during exacerbations as assessed by blood total leukocyte and neutrophil counts, and serum CRP and IL-6. These biomarkers were particularly increased in case of bacterial exacerbations. The level of sputum TNF-α during an exacerbation was the best predictor of a bacterial airway infection.
Airway inflammation during COPD exacerbations has been the focus of a few studies but their results have been inconsistent.Citation21–Citation26 This inconsistency can be explained by several factors. Firstly, it is difficult to gain information regarding airway inflammation during COPD exacerbations. Sputum induction by inhaled saline can cause additional broncho-constriction and analysis of spontaneously produced sputum samples yields less cell viability,Citation27 whereas more invasive techniques such as bronchoscopy are even more difficult to perform during exacerbations. Secondly, the causes of COPD exacerbations are heterogeneous. It is possible that well known inducing factors such as viruses, bacteria, and air pollution lead to different inflammatory patterns.Citation6 Additionally, the specific focus of a study may well bias the selection of patients, for instance in the case of studies assessing the efficacy of antibiotics. Thirdly, the use of medication by patients with COPD can influence the inflammatory pattern, as is known with inhaled corticosteroids.Citation28
This study was part of a randomized controlled trial studying the anti-inflammatory treatment effects of budesonide/formoterol therapy versus prednisolone during COPD exacerbations.Citation29 To study these effects without biasing effects of maintenance therapy, inhaled corticosteroids were withdrawn if used. This study design also allowed us to study the change in inflammation from stable disease prospectively, non-modulated by inhaled corticosteroid therapy. The results should therefore be extrapolated only to similar patients, ie, not on steroids. Whether the same findings hold true for patients on inhaled corticosteroids remains to be established.
As expected, there was an increase in sputum neutrophils during COPD exacerbations.Citation23,Citation26,Citation30 The increase in sputum neutrophil numbers was accompanied by an increase in sputum levels of LTB4 and IL-8, both attractants of neutrophils, and the neutrophil degranulation product MPO. These changes confirm an earlier study of Gompertz et alCitation31 reporting a decrease in airway inflammation from the start of a COPD exacerbation to its resolution. These authors also reported a change in microvascular leakage as determined by the sputum/serum albumin ratio, which we confirm in our prospective study.
Furthermore, we found an increase of sputum lymphocytes during exacerbations. Lymphocytes play an important role in the pathogenesis of COPD. They are related to its development and progression. Lams et al found that smokers who develop COPD have increased CD8+ T-cells in large airways compared to asymptomatic smokers.Citation32 Furthermore, there is an increase in CD4+ cells in patients with COPD, particularly as the disease progresses.Citation33 This increase in lymphocytes has been suggested to be caused by chronic immune stimulation due to infectious pathogens.Citation34 Not only T-cells, but also B-cells are increased in stable COPD.Citation35–Citation37 Although in this study we did not succeed in identifying viruses in induced sputum samples for an unknown but presumably technical reason, we still believe that viral airway infections may contribute in this respect.Citation38,Citation39 An autoimmune origin has also been suggested.Citation35,Citation40,Citation41 Whether part of the increase in lymphocytes in our study is of B-cell origin was not evaluated.
This is at least the forth report documenting an increase in eosinophil counts during exacerbations.Citation25,Citation30,Citation42 Next to the increase in eosinophils, we also found increased sputum ECP. ECP has been associated with tissue damage and tissue remodelling in in vitro studies.Citation43 This might thus contribute to the observed association between exacerbation frequency and excess decline in lung function.Citation1 However, not all prior studies have found increases in eosinophils during COPD exacerbations.Citation22 This difference between our and others’ observation of an increase in eosinophils may be simply explained by a suppressive effect of the used steroids on sputum eosinophils in these studies.Citation28
Neutrophil, and eosinophil sputum cell counts, were significantly increased, but not their percentages. This shows that absolute cell counts provide different information about inflammation than cell percentages. Absolute cell counts reflect the concentration of these cells and therefore the total load, whereas the percentage reflects an inflammatory pattern. Our data point out that there can be an increase in inflammation, without a significant change in the inflammatory pattern.
Next to increased sputum inflammation as proxy of airways inflammation, we also found increased systemic inflammation as demonstrated by increased number of blood total leukocytes, neutrophils, IL-6, and a trend in CRP during exacerbations. This confirms an earlier report of increased systemic inflammation (increased serum IL-6 and CRP) during COPD exacerbations.Citation44,Citation45 In 22% of our sputum samples the exacerbation was associated with a bacterial infection. These exacerbations showed a higher increase of total cell and neutrophil counts, IL-6, TNF-α levels in sputum, and leukocyte and neutrophil counts, CRP, and IL-6 levels in blood. This relationship of higher sputum and systemic inflammation in the presence of a bacterial pathogen in sputum has been reported in earlier studies,Citation26,Citation44 though not all studies have found this relationship.Citation21 However, these studies did not investigate whether these high levels were already present in stable state,Citation26,Citation44 or, as we now show, indeed reflected an increase that occurs with a bacterial infection. Our data show that some of the biomarkers that are increased in an exacerbation actually only change if the specific exacerbation is induced by a bacterial infection.
Serum CRP has been investigated as a marker to identify exacerbations in one study.Citation8 The predictive value of serum CRP alone was limited in that study, and use of the combination of the CRP level with a symptom of exacerbation was proposed to improve the predictive value of CRP. Our study shows that CRP is much more increased in bacterial exacerbations. We believe this underlines the limitations of CRP as a general biomarker of COPD exacerbations.
It would be of clinical use if clinicians would have bio-markers with cut-off points to differentiate which patient has a bacterial airway infection. If one would know from a rapidly available biomarker whether there is a high chance of a bacterial infection, this would improve the efficiency of use of antibiotic treatment. Our study population had mild to moderate COPD and is not large enough to provide firm data on such cut-off points, and we investigated exacerbations that did not require hospitalization. Nevertheless, we do present the receiver operating charateristic curves to offer reference and directions for future assessment of firm cut-off points. From our preliminary analyses, sputum TNF-α seems to be a good candidate biomarker in future studies. Sputum TNF-α levels were only increased in patients with a bacterial exacerbation, and not in patients with a non-bacterial exacerbation. Since the majority of patients did not have a bacterial exacerbation, the change in sputum TNF-α levels for the total group from stable to exacerbation was not significant (). This finding is supported by a study by Sethi et al which reports significantly increased sputum TNF-α levels in exacerbations with new bacterial strains.Citation46 We do not have data on changes in strains: all patients with an bacterial exacerbation had negative cultures in stable phase.
In summary, this study showed an increase in neutrophilic, eosinophilic, and lymphocytic airway inflammation from a stable phase of disease to an exacerbation in out-patient COPD patients withdrawn from inhaled corticosteroids. In addition, systemic airway inflammation increased during exacerbations and of interest, this was limited to exacerbations with bacterial infections. Some of the bio-markers, specifically sputum LTB4, MPO, IL-6, TNF-α, and serum CRP and IL-6, which are commonly associated with exacerbations, are increased during bacterial exacerbations, but little or not increased at all during non-bacterial exacerbations. Though our group of patients was too small to draw firm conclusions, the data lend support to further investigation of whether these inflammatory parameters, and specifically TNF-α, provide a useful tool for identification of a bacterial infection in COPD.
Abbreviations
| CCL-5 | = | chemotactic cytokine ligand-5 |
| CCQ | = | clinical COPD questionnaire |
| COPD | = | chronic obstructive pulmonary disease |
| CRP | = | C-reactive protein |
| Ct | = | cycle threshold |
| ECP | = | eosinophilic cationic protein |
| FEV1 | = | forced expiratory flow in one second |
| FVC | = | forced vital capacity |
| HO-1 | = | heme oxygenase-1 |
| IFN-γ | = | interferon-γ |
| IL | = | interleukin |
| IQR | = | interquartile range |
| LTB4 | = | leukotriene-B4 |
| MCP-1 | = | monocyte chemoattractant protein-1 |
| MPO | = | myeloperoxidase |
| mRNA | = | messenger ribonucleic acid |
| TGF-β | = | transforming growth factor-β |
| TNF-α | = | tumor necrosis factor-α |
| VC | = | slow inspiratory vital capacity |
Acknowledgments
The authors thank Ibolya Sloots, Brigitte Dijkhuizen, Koos van de Belt, and Janneke Heimweg for the sputum measurements, the lung function department for the many lung function measurements, and Dr N.E.L. Meessen for his help with the interpretation of sputum culture results.
Disclosures
This study was supported by a research grant from AstraZeneca, the Netherlands.
Erik Bathoorn’s and Jeroen Liesker’s salaries were paid by AstraZeneca.
Huib Kerstjens and Dirkje Postma receive funds for research from AstraZeneca and have competing arrangements with the competitors GlaxoSmithKline and Altana.
Gerard Koëter, Marco van der Toorn, Sicco van der Heide, and Antoon J.M. van Oosterhout have no conflicts of interests to declare.
References
- DonaldsonGCSeemungalTABhowmikAWedzichaJARelationship between exacerbation frequency and lung function decline in chronic obstructive pulmonary diseaseThorax2002571084785212324669
- SchmierJKHalpernMTHigashiMKBakstAThe quality of life impact of acute exacerbations of chronic bronchitis (AECB): a literature reviewQual Life Res200514232934715892423
- McGuireAIrwinDEFennPThe excess cost of acute exacerbations of chronic bronchitis in patients aged 45 and older in England and WalesValue Health20014537037511705127
- Rodriguez-RoisinRToward a consensus definition for COPD exacerbationsChest20001175 Suppl 2398S401S10843984
- MadisonJMIrwinRSChronic obstructive pulmonary diseaseLancet199835291264674739708769
- Global Strategy for the Diagnosis, management and prevention of Chronic Obstructive Pulmonary Disease; updated 2006. available from http://www.goldcopd.com. 2006.
- AnthonisenNRManfredaJWarrenCPHershfieldESHardingGKNelsonNAAntibiotic therapy in exacerbations of chronic obstructive pulmonary diseaseAnn Intern Med198710621962043492164
- HurstJRDonaldsonGCPereaWRUtility of plasma biomarkers at exacerbation of chronic obstructive pulmonary diseaseAm J Respir Crit Care Med2006174886787416799074
- Christ-CrainMJaccard-StolzDBingisserREffect of procalcitonin-guided treatment on antibiotic use and outcome in lower respiratory tract infections: cluster-randomised, single-blinded intervention trialLancet2004363940960060714987884
- BathoornDChange in inflammation during COPD exacerbationsEur Respir J200526Suppl 4915s
- SiafakasNMVermeirePPrideNBOptimal assessment and management of chronic obstructive pulmonary disease (COPD). The European Respiratory Society Task ForceEur Respir J199588139814207489808
- QuanjerPHTammelingGJCotesJEPedersenOFPeslinRYernaultJCLung volumes and forced ventilatory flows. Report Working Party Standardization of Lung Function Tests, European Community for Steel and Coal. Official Statement of the European Respiratory SocietyEur Respir J Suppl1993165408499054
- van der MolenTWillemseBWSchokkerSten HackenNHPostmaDSJuniperEFDevelopment, validity and responsiveness of the Clinical COPD QuestionnaireHealth Qual Life Outcomes2003281(1)1312773199
- PizzichiniMMPizzichiniEClellandLSputum in severe exacerbations of asthma: kinetics of inflammatory indices after prednisone treatmentAm J Respir Crit Care Med19971555150115089154849
- RutgersSRTimensWKaufmannHFvan der MarkTWKoeterGHPostmaDSComparison of induced sputum with bronchial wash, bronchoalveolar lavage and bronchial biopsies in COPDEur Respir J200015110911510678630
- MeijerRJKerstjensHAArendsLRKauffmanHFKoeterGHPostmaDSEffects of inhaled fluticasone and oral prednisolone on clinical and inflammatory parameters in patients with asthmaThorax1999541089489910491451
- RenkemaTEPostmaDSNoordhoekJASluiterHJKauffmanHFIn vitro release of neutrophil elastase, myeloperoxidase and beta-glucuronidase in patients with emphysema and healthy subjectsEur Respir J1991410123712441666565
- GecklerRWGremillionDHMcAllisterCKEllenbogenCMicroscopic and bacteriological comparison of paired sputa and transtracheal aspiratesJ Clin Microbiol197764396399334796
- BorgerPVellengaEGringhuisSIProstaglandin E2 differentially modulates IL-5 gene expression in activated human T lymphocytes depending on the costimulatory signalJ Allergy Clin Immunol19981012 Pt 12312409500757
- KocksJWTuinengaMGUilSMvan den BergJWStahlEvan der MolenTHealth status measurement in COPD: the minimal clinically important difference of the clinical COPD questionnaireRespir Res200676216603063
- AaronSDAngelJBLunauMGranulocyte inflammatory markers and airway infection during acute exacerbation of chronic obstructive pulmonary diseaseAm J Respir Crit Care Med2001163234935511179105
- BhowmikASeemungalTASapsfordRJWedzichaJARelation of sputum inflammatory markers to symptoms and lung function changes in COPD exacerbationsThorax200055211412010639527
- FujimotoKYasuoMUrushibataKHanaokaMKoizumiTKuboKAirway inflammation during stable and acutely exacerbated chronic obstructive pulmonary diseaseEur Respir J200525464064615802337
- QiuYZhuJBandiVBiopsy neutrophilia, neutrophil chemokine and receptor gene expression in severe exacerbations of chronic obstructive pulmonary diseaseAm J Respir Crit Care Med2003168896897512857718
- SaettaMDi StefanoAMaestrelliPAirway eosinophilia in chronic bronchitis during exacerbationsAm J Respir Crit Care Med19941506 Pt 1164616527952628
- PapiABellettatoCMBraccioniFInfections and airway inflammation in chronic obstructive pulmonary disease severe exacerbationsAm J Respir Crit Care Med2006173101114112116484677
- PizzichiniMMPopovTAEfthimiadisASpontaneous and induced sputum to measure indices of airway inflammation in asthmaAm J Respir Crit Care Med19961544 Pt 18668698887576
- BarnesNCQiuYSPavordIDAntiinflammatory effects of salmeterol/fluticasone propionate in chronic obstructive lung diseaseAm J Respir Crit Care Med2006173773674316424444
- BathoornELieskerJJPostmaDSAnti-inflammatory effects of combined budesonide/formoterol in COPD exacerbationsCOPD20085528229018972276
- MercerPFShuteJKBhowmikADonaldsonGCWedzichaJAWarnerJAMMP-9, TIMP-1 and inflammatory cells in sputum from COPD patients during exacerbationRespir Res2005615116372907
- GompertzSO’BrienCBayleyDLHillSLStockleyRAChanges in bronchial inflammation during acute exacerbations of chronic bronchitisEur Respir J20011761112111911491152
- RolandMBhowmikASapsfordRJSputum and plasma endothelin-1 levels in exacerbations of chronic obstructive pulmonary diseaseThorax2001561303511120901
- MajoriMCorradiMCaminatiACaccianiGBertaccoSPesciAPredominant TH1 cytokine pattern in peripheral blood from subjects with chronic obstructive pulmonary diseaseJ Allergy Clin Immunol19991033 Pt 145846210069880
- RetamalesIElliottWMMeshiBAmplification of inflammation in emphysema and its association with latent adenoviral infectionAm J Respir Crit Care Med2001164346947311500352
- van der StrateBWPostmaDSBrandsmaCACigarette Smoke-induced Emphysema: A Role for the B Cell?Am J Respir Crit Care Med2006173775175816399994
- GosmanMMWillemseBWJansenDFIncreased number of B-cells in bronchial biopsies in COPDEur Respir J2006271606416387936
- HoggJCChuFUtokaparchSThe nature of small-airway obstruction in chronic obstructive pulmonary diseaseN Engl J Med2004350262645265315215480
- GerhardWMozdzanowskaKFurchnerMWashkoGMaieseKRole of the B-cell response in recovery of mice from primary influenza virus infectionImmunol Rev1997159951039416505
- CoroESChangWLBaumgarthNType I IFN receptor signals directly stimulate local B cells early following influenza virus infectionJ Immunol200617674343435116547272
- MajoJGhezzoHCosioMGLymphocyte population and apoptosis in the lungs of smokers and their relation to emphysemaEur Respir J200117594695311488331
- AgustiAMacNeeWDonaldsonKCosioMHypothesis: does COPD have an autoimmune component?Thorax2003581083283414514931
- FujimotoKYasuoMUrushibataKHanaokaMKoizumiTKuboKAirway inflammation during stable and acutely exacerbated chronic obstructive pulmonary diseaseEur Respir J200525464064615802337
- ZagaiUSkoldCMTrulsonAVengePLundahlJThe effect of eosinophils on collagen gel contraction and implications for tissue remodellingClin Exp Immunol2004135342743315008974
- HurstJRPereraWRWilkinsonTMDonaldsonGCWedzichaJASystemic and upper and lower airway inflammation at exacerbation of chronic obstructive pulmonary diseaseAm J Respir Crit Care Med20061731716718
- SeemungalTHarper-OwenRBhowmikARespiratory viruses, symptoms, and inflammatory markers in acute exacerbations and stable chronic obstructive pulmonary diseaseAm J Respir Crit Care Med200116491618162311719299
- SethiSWronaCEschbergerKLobbinsPCaiXMurphyTFInflammatory profile of new bacterial strain exacerbations of chronic obstructive pulmonary diseaseAm J Respir Crit Care Med2008177549149718079493