Abstract
Osteoporotic vertebral fractures are associated with considerable reduction of quality of life, morbidity, and mortality. The management of patients with vertebral fractures should include treatment for osteoporosis and measures to reduce pain and improve mobility. This article provides information for management and rehabilitation of vertebral fractures based on clinical experience and literature.
Introduction
Health consequences from osteoporotic fractures in women include disability and increased mortality. As a result vertebral fractures have a negative impact on the quality of life and their presence is linked with cardiopulmonary morbidities, depression and death.Citation1–Citation6
The most important target is to prevent these fractures, but if a fracture exists the focus shifts to rehabilitation and prevention of the next fracture. Lindsay et al confirmed that women who develop a vertebral fracture are at substantial risk for additional fracture within the next year.Citation7
Musculoskeletal pain, common in patients with osteoporotic vertebral fractures, is one of the most frequent symptoms for which medical assistance is sought. Osteoporosis represents one of the main causes of back pain in postmenopausal women.Citation8 Although, in the same population, nonosteoporotic vertebral deformities are seen as often as osteoporotic ones, and they are also a main cause of back pain. In women up to 60 years back pain was found to be mostly due to degenerative disorders of the spine.Citation9
Clinical or subclinical vertebral fractures are a common cause of back pain. Vertebral fractures cause acute pain in the back in the acute phase of the fracture and chronic pain resulting from the associated skeletal deformity, joint incongruity, and tension on muscles and tendons,Citation10 leading to disability. It is surprising that most of these patients do not receive an antiosteoporotic treatment.Citation11
Targeted osteoporotic drug treatment
Pharmacologic treatment should be prescribed for those who have sustained vertebral fractures.Citation11 In fact in a retrospective study only 15% of medical records indicated that fracture patients had been prescribed antiosteoporotic medications within one year after discharge from hospital.Citation12,Citation13
The therapeutic effect of bisphosphonates on back pain has rarely been reported on in patients with vertebral fractures.Citation14 Nevitt et al have reported the efficacy of long-term treatment with alendronate in elderly osteoporotic patients for reducing the burden of activity limitation and bed disability caused by back pain.Citation14,Citation15 A valuable drug in the rehabilitation process of elderly patients suffering from back pain due to osteoporotic vertebral collapse seems to be intravenous pamidronate.Citation14,Citation16
Armingeat et al in their controlled trial of intravenous pamidronate comparing placebo for pain relief in recent osteoporotic vertebral compression fractures found a rapid, marked, and sustained analgesic effect of pamidronate for reducing acute back pain due to recent osteoporotic vertebral fracture, without any significant safety concerns.Citation17
In a review article Ulivieri stated that treating patients with antiresorptive and anabolic agents reduces the risk of new or worsening back pain, particularly with teriparatide therapy.Citation18 In line with this paper Nevitt et al in a meta-analysis, concluded that teriparatide had a reduced risk of new or worsening back pain compared to patients randomized to placebo, hormone replacement therapy, or alendronate.Citation19 In a retrospective analysis, Lindsay et al reported that the presence of one or more vertebral fractures resulted in a five-fold increase in risk for sustaining a subsequent vertebral fracture.Citation20 Therapeutic options can reduce the number of new vertebral compression fractures by 40%–60% within the first year in individuals with a fracture.Citation21
Calcium, vitamin D, and vitamin D analoguesCitation21
Pooled data comparing vitamin D alone with placebo or no treatment showed no statistically significant effect on vertebral fracture or deformity.Citation22 Vitamin D (including 25-hydroxy vitamin D) with calcium was no more effective than calcium alone on vertebral fracture. Evidence has shown that vitamin D alone was less effective than calcium for the prevention of vertebral fracture or deformity. There was no evidence of a statistically significant preventive effect on clinical vertebral fractures from the administration of vitamin D and calcium and vitamin D plus calcium versus placebo or no treatment. In participants with osteoporosis no statistically significant effect of alfacalcidol (1-alpha-hydroxy vitamin D3) compared with vitamin D and calcium on people with new vertebral deformities was found. Calcitriol (1,25 dihydroxy vitamin D3), and additional supplementation with calcitriol in people with osteoporosis who were already taking calcium had no statistically significant effect on new vertebral deformity. No statistically significant effect on the number of people developing new vertebral deformities receiving calcitriol plus vitamin D and calcium versus vitamin D and calcium was found. Overall, there was no statistically significant effect on the incidence of vertebral deformities with calcitriol versus calcium. When calcitriol was compared with vitamin D in people with pre-existing osteoporosis no statistically significant effect was seen for vertebral deformities.
Other interventions
Back pain in the majority of these patients is treated with prolonged bed-rest, local and systemic analgesia, and bracing.Citation23 Thereby, the incidence of a vertebral fracture should be followed by a limited period of bed rest, to avoid the hazards of deconditioning, accelerated bone loss, deep venous thrombosis, pneumonia, decubitus ulcers, disorientation, and depression.Citation24,Citation25
The extension of bed-rest in these patients results in increase of bone loss (identified by increase of hydroxyproline excretion) and muscle weakness and joint stiffness. Another interesting aspect is that most osteoporotic vertebral fractures happen in high bone turnover patients, and in these patients postfracture immobilization is an additional risk factor of increased bone loss.Citation26 Nasal salmon calcitonin in a daily dose of 200 IU has an equivalent analgesic effect to 100 IU of injectable salmon calcitonin.Citation21,Citation27,Citation28 The analgesic efficacy of nasal calcitonin was tested in 32 men and 68 postmenopausal women with a mean age of 76 and 71 years respectively, who, within the previous 5 days, had sustained a nontraumatic vertebral fracture which had been confirmed radiographically and clinically.Citation13 The patients were hospitalized for a period of 28 days and were randomly assigned to receive either 200 IU of nasal salmon calcitonin or a matching nasal placebo spray. In addition patients were permitted to take paracetamol as a rescue analgesic up to 6 tablets of 500 mg daily. Treatment was initiated after baseline measurements on day 0. Pain evaluation was performed daily using a 10-degree visual analog scale (VAS) (0 = no pain, 10 = agonizing pain). Pain was tested during different locomotor functions eg, bed rest, sitting, standing, and walking. In our experience if a patient records a pain above 7 (in the VAS scale) he is not capable of attempting the recommended locomotor function. In turn, a rating of pain less than 7 suggests that the patient does not require nursing and bed rest and that he is able to begin physiotherapy. After the completion of 28 days of follow-up it was found that pain was reduced dramatically in the group receiving calcitonin (P < 0.001). The analgesic effect of nasal calcitonin was negatively associated with the number of paracetamol tablets consumed. The VAS pain rating showed that most patients gradually gained full mobility after the first week of calcitonin treatment. The number of patients who remained bedridden was significantly higher in the placebo group at all time points than in the calcitonin group.Citation13
Spinal compression fracture and pain can produce an imbalance between the use of back extensors (the major trunk supportive muscles) and flexors. To decrease painful contractions of the erector spinae muscles, one needs to decrease the load over the anterior aspect of the spinal column and vertebral bodies.
Bracing is used in acute nonsurgical management, whereas spinal orthoses relieve the pain and promote the healing process by stabilizing the spine. It should be noted that the latter reduces the load applied on the anterior column and vertebral body by restraining any attempt of forward flexion. Even though there is a lack of specific studies comparing various types of orthoses, it is widely accepted that all spine orthoses, whether made of cloth, metal, or plastic, and whether rigid or flexible, use a three-point pressure system.Citation24,Citation25
The most broadly used types of spinal orthoses in GreeceCitation24 are: a) the TLSO type that provides support to the thoracolumbosacral spine by making it adopt an anatomically correct position (Knight-Taylor, Jewett, CASH, or Cruciform Anterior Sternal, Boston, MA), b) the posture training support (PTS) type, which is a device that has shoulder straps joining above the waist at the back, where a pouch holds small weights,Citation29 c) Spinomed®, the new ‘bracing’ philosophy, based on biofeedback theoryCitation30 and d) Osteomed®, which is based upon the gate control theory of pain.Citation31,Citation32
Kaplan et al pointed out that orthotic devices impose a risk of reduction in muscular strength. Their controlled pilot study with a 4-week observation period demonstrated that the strength of the back extensors was reduced to below the initial value in 40% of female patients wearing a stable orthotic device.Citation33 On the contrary we published recently preliminary results of women with established osteoporosis and/or an angle of kyphosis more than 55 degrees wearing Spinomed orthosis for at least 2 hours/day for 6 months showing that Spinomed significantly decreased back pain (P = 0.001) (evaluation was performed using visual analog scale at the beginning and 6 months follow-up of the examination) and increased personal isometric trunk muscle strength, ( and ).Citation34
Figure 1 Schematic presentation of values in personal isometric force in Newton (N): Force (F)/Weight (W) in abdominals and extensor muscles (F/W abdominals and F/W ext, respectively), after 6 months wearing Spinomed orthosis (F: force in Newton, W: weight in Kg).
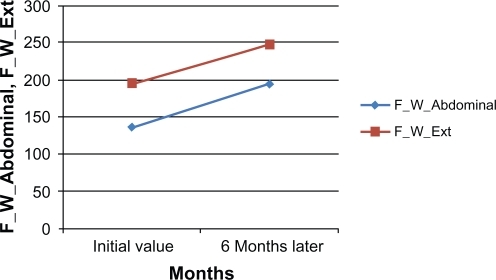
Table 1 Differences in values of visual analog scale (VAS) and personal isometric force: force (F)/weight (W) in abdominals and extensors muscles (F/W abdominals and F/W extensors, respectively), after 6 months wearing Spinomed orthosis. (F: force in Newton, W: weight in Kg) measured with ISO-RACK device (Digimax, MechaTronic, Germany)
Pfeifer et al also reported the effectiveness of Spinomed for stabilizing osteoporotic vertebral fractures. In their study the use of Spinomed was associated with a significant increase in trunk muscle strength, most likely because of increased muscular activity while wearing the orthosis.Citation30
A program of physical therapy is necessary and helps prevent deformity by strengthening antigravity muscles and promoting postural retraining. Breathing exercises promote thoracic expansion and improve the heavily degraded pulmonary function found in patients with spinal osteoporotic fractures.Citation35 Instruction on the proper method of lifting things, as well as how to use a walker or a cane properly, could be beneficial and thus is strongly recommended.Citation24,Citation35 Patients with fractures could subject themselves to low-intensity exercise and gentle strengthening programs (eg, Tai Chi and hydrotherapy) and are strongly recommended to avoid high impact exercise or movements, so that they avoid suffering new vertebral fractures.Citation29 Forward bending of the spine or flexion exercises, especially in combination with twisting, should be avoided.Citation24,Citation29 According to Bassey, this includes several old favorite exercises which are now considered outdated, namely straight-leg toe touches and sit ups (or crunches) for strengthening the abdominal muscles.Citation36 Sinaki and Mikkelsen reported that the latter are associated with a dramatically increased rate of vertebral fracture in osteoporotic women (89% compared to 16% of those who did extension exercises).Citation37 As the acute fracture pain subsides, a walking program can begin with gentle strengthening exercises focusing on spinal extensor muscles.Citation38 A carefully supervised rehabilitation program should be started after 3 to 4 months, to strengthen the spinal extensor and abdominal muscles more aggressively.Citation24,Citation39
Vertebroplasty and kyphoplasty
These procedures are different in several aspects. Vertebroplasty mainly involves the application of polymethylmethacrylate (PMMA) to the fracture. This procedure is considered to be very successful in the stabilization of fractured osteoporotic vertebral body and in pain relief.Citation40 A possible alternative is to inject calcium phosphate cement into a vertebral fracture, while in kyphoplasty a balloon is inserted to create space in the fractured vertebra, to restore its height and shape, before the balloch it is removed and the cement is delivered to the resulting space. Percutaneous vertebroplasty obtains early pain relief and improves the integrity of the osteoporotic vertebral body.Citation41 On the other hand the mini-surgical intervention may cause serious complications to patients with recent fractures, such as paraplegia,Citation42 and the occurrence of a new vertebral body fracture, and possible cardiopulmonary events.Citation43 Two studies in 2009 concerning the efficacy of vertebroplasty may signal a different approach for this procedure.Citation44,Citation45 In the first studyCitation44 78 patients with one or two painful osteoporotic vertebral fractures were randomized in a multicenter, double-blind, placebo-controlled trial (vertebroplasty vs a sham procedure). The authors found no significant advantage for vertebroplasty at any time point during follow-up between groups with respect to pain at night and at rest, physical functioning, quality of life, and perceived improvement. Another study in 131 patients, with one to three painful osteoporotic vertebral fractures, randomized either in vertebroplasty or a sham procedure found similar results.Citation45 The authors noted a trend toward a higher rate of clinically meaningful improvement in pain in the vertebroplasty group but improved disability and pain scores were noted immediately following both procedures.
On the other hand a randomized controlled trial (Fracture Reduction Evaluation [FREE] trial) which took place at 21 sites in eight countries and included 149 patients assigned to balloon kyphoplasty showed that in patients with acute, painful, vertebral fractures, balloon kyphoplasty improved quality of life, function, mobility, and pain more rapidly than did nonsurgical management, with significant differences in improvement between the groups at 1 month.Citation46
Disclosure
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
References
- PapaioannouAWattsNBKendlerDLYuenCKAdachiJDFerkoNDiagnosis and management of vertebral fractures in elderly adultsAm J Med200211322022812208381
- YamaguchiTSugimotoTYamauchiMMatsumoriYTsutsumiMChiharaKMultiple vertebral fractures are associated with refractory reflux esophagitis in postmenopausal womenJ Bone Miner Metab200523364015616892
- TosiLLBouxseinMLJohnellOCommentary on the AAOS position statement: recommendations for enhancing the care for patients with fragility fracturesTech Orthop200419121125
- CooperCAtkinsonEJJacobsenSJO’FallonWMMeltonLJIIIPopulation based study of survival after osteoporotic fracturesAm J Epidemiol1993137100110058317445
- IsmailAACockerillWCooperCPrevalent vertebral deformity predicts incident hip though not distal forearm fracture: results from the European Prospective Osteoporosis StudyOsteoporos Int200112859011303719
- GoldDTOsteoporosis and quality of life: psychosocial outcomes and interventions for individual patientsClin Geriatr Med20031927128012916286
- LindsayRSilvermanSLCooperCRisk of new vertebral fracture in the year following a fractureJAMA200128532032311176842
- GehlbachSHBigelowCHeimisdottirMMaySWalkerMKirkwoodJRRecognition of vertebral fracture in a clinical settingOsteoporos Int20001157758211069191
- MolsbergerAJensenKUMullerUWinkelmannWWehlingPChronic pain syndromes in orthopedics. Typical types, follow-up and patient characteristicsZ Orthop Ihre Grenzgeb19891276957002618151
- FrancisRMAsprayTJHideGSutcliffeAMWilkinsonPBack pain in osteoporotic vertebral fracturesOsteoporos Int20081989590318071648
- BouxseinMLKaufmanJTosiLCummingsSLaneJJohnellORecommendations for optimal care of the fragility fracture patient to reduce the risk of future fractureJ Am Acad Orthop Surg20041238539515615504
- PannemanMJLipsPSenSSHeringsRMUndertreatment with antiosteoporotic drugs after hospitalization for fractureOsteoporos Int20041512012414618302
- LyritisGPTrovasGAnalgesic effects of calcitoninBone200230Suppl 571S74S12008162
- IwamotoJTakedaTIchimuraSUzawaMComparative effects of treatment with etidronate and alendronate on bone resorption, back pain, and activities of daily living in elderly women with vertebral fracturesKeio J Med20035223023514748475
- NevittMCThompsonDEBlackDMEffect of alendronate on limited activity days and bed-disability days caused by back pain in postmenopausal women with existing vertebral fractures. Fracture Intervention Trial Research GroupArch Intern Med2000160778510632308
- GangjiVAppelboomTAnalgesic effect of intravenous pamidronate on chronic back pain due to osteoporotic vertebral fracturesClin Rheumatol19991826626711206358
- ArmingeatTBrondinoRPhamTLegréVLafforguePIntravenous pamidronate for pain relief in recent osteoporotic vertebral compression fracture: a randomized double-blind controlled studyOsteoporos Int2006171659166516896508
- UlivieriFMBack pain treatment in post-menopausal osteoporosis with vertebral fracturesAging Clin Exp Res200719Suppl 3212318180603
- NevittMCChenPDoreRKReduced risk of back pain following teriparatide treatment: a meta-analysisOsteoporos Int20061727328016142502
- LindsayRSilvermanSLCooperCRisk of new vertebral fracture in the year following a fractureJAMA200128532032311176842
- LyritisGPTsakalakosNMagiasisBKarachaliosTYiatzidesATsekouraMAnalgesic effect of salmon calcitonin in osteoporotic vertebral fractures: a double-blind placebo-controlled clinical studyCalcif Tissue Int1991493693721818759
- AvenellAGillespieWJGillespieLDO’ConnellDVitamin D and vitamin D analogues for preventing fractures associated with involutional and post-menopausal osteoporosisCochrane Database of Syst Rev2009CD00022719370554
- LukertBPVertebral compression fractures: how to manage pain, avoiding disabilityGeriatrics19944922268307385
- DionyssiotisYDontasIAEconomopoulosDLyritisGPRehabilitation after falls and fracturesJ Musculoskelet Neuronal Interact2008824425018799857
- MazanecDJPodichettyVKMompointAPotnisAVertebral compression fractures: manage aggressively to prevent sequelaeCleve Clin J Med20037014715612636346
- LyritisGPMayasisBTsakalakosNThe natural history of the osteoporotic vertebral fractureClin Rheumatol19898Suppl 266692758779
- LyritisGPPaspatiIKarachaliosTIoakimidisDSkarantavosGLyritisPGPain relief from nasal salmon calcitonin in osteoporotic vertebral fractures. A double blind, placebo controlled clinical studyActa Orthop Scand1997275Suppl112114
- LyritisGPIoannidisGVKarachaliosTAnalgesic effect of salmon calcitonin suppositories in patients with acute pain due to recent osteoporotic vertebral crush fractures: a prospective double-blind, randomised, placebo-controlled clinical studyClin J Pain19991528428910617256
- SinakiMLynnSGReducing the risk of falls through proprioceptive dynamic posture training in osteoporotic women with kyphotic posturing: a randomized pilot studyAm J Phys Med Rehabil20028124124611953540
- PfeiferMBegerowBMinneHWEffects of a new spinal orthosis on posture, trunk strength, and quality of life in women with postmenopausal osteoporosis: a randomized trialAm J Phys Med Rehabil20048317718615043351
- HildebrandtHDVogtLDer “Osteoporosebody” – eine multifunktionale OrtheseOrthopädie-Technik2002539096
- VogtLHübscherMBrettmannKBanzerWFinkMPostural correction by osteoporosis orthosis (Osteo-med): a randomized, placebo-controlled trialProsthet Orthot Int20083210311018330809
- KaplanRSSinakiMHameisterMDEffect of back supports on back strength in patients with osteoporosis: a pilot studyMayo Clin Proc1996712352418594280
- DionyssiotisYMichasGGalanosAThomaSLyritisGPA perspective study of spinal orthosis in postmenopausal womenOsteoporos Int200920Suppl 1S23S176
- BonnerFJJrSinakiMGraboisMHealth professional‘s guide to rehabilitation of the patient with osteoporosisOsteoporos Int200314Suppl 2S1S2212759719
- BasseyEJExercise for prevention of osteoporotic fractureAge Ageing200130Suppl 4293111769785
- SinakiMMikkelsenBAPostmenopausal spinal osteoporosis: flexion versus extension exercisesArch Phys Med Rehabil1984655935966487063
- RapadoAGeneral management of vertebral fracturesBone199618S191S196
- SinakiMMusculoskeletal rehabilitationRiggsBLMeltonLJOsteoporosis: Etiology, Diagnosis, and Management2nd edPhiladelphiaLippincott-Raven1995435473
- AhnDKLeeSChoiDJMechanical properties of blood-mixed polymethylmetacrylate in percutaneous vertebroplastyAsian Spine J20093455220404947
- NakamoMHiranoNMatsuuraKPercutaneous transpedicular vertebroplasty with calcium phosphate cement in the treatment of osteoporotic vertebral compression and burst fracturesJ Neurosurg200397Suppl 3287293
- LeeBJLeeSRYooTYParaplegia as a complication of percutaneous vertebroplasty with polymethylmethacrylate: a case reportSpine200227E419E42212394938
- UppinAAHirschJACenteneraLVPfieferBAPazianosAGChoiISOccurrence of new vertebral body fracture after perculaneous vertebroplasty in patients with osteoporosisJ Radiology2003226119124
- KallmesDFComstockBAHeagertyPJA randomized trial of vertebroplasty for osteoporotic spinal fracturesN Engl J Med200936156957919657122
- BuchbinderROsborneRHEbelingPRA randomized trial of vertebroplasty for painful osteoporotic vertebral fracturesN Engl J Med200936155756819657121
- WardlawDCummingsSRVan MeirhaegheJEfficacy and safety of balloon kyphoplasty compared with non-surgical care for vertebral compression fracture (FREE): a randomised controlled trialLancet20093731016102419246088