Abstract
Renal involvement, which can rarely occur in echinococcosis, more commonly manifests as hydatid cyst of the kidney. Scattered case reports of nephrotic syndrome secondary to hydatid cyst in the liver or lung have been reported for over two decades. The glomerular picture varied from minimal change lesion to mesangiocapillary glomerulonephritis. We report a case of predominantly tubulointerstitial nephritis with mesangioproliferative glomerulonephritis in a patient with hepatic hydatid cyst which responded to cyst resection alone.
Introduction
Echinococcosis or hydatid disease is caused by larvae of the tapeworm, Echinococcus. Echinococcosis has a worldwide distribution. In cystic echinococcosis, humans are an accidental host and are usually infected after handling an infected dog. The liver and lungs are the most frequently involved organs. Rarely occurrences of primary cysts in kidneys have been reported, with the consequent finding of jellylike hydatid material in the urine.Citation1 Few cases of glomerular lesions that presented with nephrotic syndrome associated with hydatid disease have been described. We report a unique case of a female who presented with nephrotic syndrome due to mesangioproliferative glomerulonephritis with acute or chronic tubulointerstitial nephritis with a large hepatic hydatid cyst. Proteinuria was abolished by surgical cyst removal and restored the patient to sustained good health.
Case report
An 18-year-old female presented with complaints of generalized edema of three months duration in January 2008. She also had loss of appetite, low grade fever, and right-sided upper abdominal pain for the same duration. She did not have any discoloration of urine, joint pain, skin rash, or hair loss. She had no history of allergies, tuberculosis, or hypertension.
On admission to the hospital she had pallor and anasarca with ascites. She was afebrile with normal blood pressure. Her liver was enlarged and extended 4 cm below the costal margin in midcalvicular line. Liver was firm and tender. No other organomegaly was noted.
Urine was positive for protein on dipstick and contained red cells, pus cells, and proteinaceous casts. She was excreting 3.2 g of urinary protein in 24 hours. Renal function was normal. Her hemoglobin was 9.8 g/dL with normochromic, normocytic picture with no evidence of hemolysis. Her complete blood count was normal and autoantibody screen (antinuclear and antineutrophil cytoplasmic) was negative. The complement levels C3 and C4 were normal. The liver function was normal except for that serum albumin level was significantly low with a value of 1.8 g/dL and total protein was 4.3 g/dL. The serum cholesterol level was elevated and was 465 mg/dL.
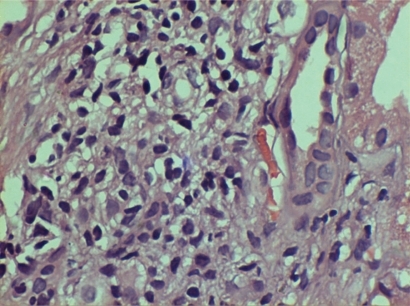
Chest X-ray revealed a raised right hemidiaphragm. Renal ultrasound showed normal kidneys except for slightly increased echogenecity. Liver ultrasound showed fluid filled cavity of 9.3 × 8.1 cm with multiple cysts within it in the left lobe of liver. Ultrasound also revealed mild ascites. Serology for Echinococcus granulosus (IgG/IgM) was positive. Computed tomography (CT) scan of the abdomen showed an 11 × 10 × 6 cm cystic lesion with areas of rim calcification and few small cysts within it in the left lobe of liver which was extending into the lesser sac (). Mild ascites were also noted. The above findings confirmed the diagnosis of hydatid disease of liver. The patient was subjected to renal biopsy as it was a nephrotic presentation. Renal biopsy revealed mesangial proliferation with acute on chronic tubulo-interstitial nephritis (, ). Electron microscopy was not done as there was no in-house facility.
Figure 1 CT abdomen: 11 × 10 × 6 cm cystic lesion with areas of rim calcification and few small cysts within it noted in the left lobe of liver extending into lesser sac. Mild ascites. Suggestive of hydatid disease of liver.
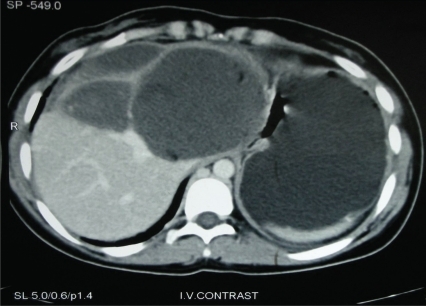
Figure 2 Glomeruli showed moderate mesangial matrix accentuation with hypercellularity. Capillary lumina were open with thickened, wrinkled membranes. Bowman’s capillary segmentally thickened and occasionally ruptured. Tubules had moderate degenerative changes. Mild interstitial edema with diffuse mixed leucocytic infiltration noted.
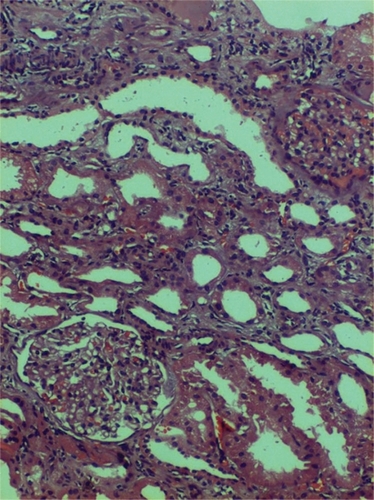
Figure 3 Acute on chronic tubulo-interstitial nephritis with mesangioproliferative glomerulonephritis.
Treatment was started with diuretics, albumin infusion, and high protein diet. The patient was also initiated with albendazole 400 mg twice a day. After three weeks of preparation, hepatic cyst resection was done. The laparotomy was uneventful and histopathological evaluation of the resected specimen confirmed the diagnosis of hydatid cyst.
Two weeks after surgery, the serum albumin had only marginal improvement to 2.2 g/dL and 24-hour urine protein excretion was 2.5 g. One month after surgery, the 24-hour urine protein excretion decreased to less than 1 g. Two months after surgery, the serum albumin level became 3.6 g/dL and 24-hour urine protein excretion became less than 300 mg. Follow-up urine examination and ultrasound was normal for one year after surgery, which confirmed good renal recovery and absence of residual hepatic Echinococcus disease. Albendazole was given for a total of twelve weeks. The patient was never treated with steroids or any other immunosuppressant.
Discussion
Parasitic infections (ie, Protozoa or helminths) may be responsible for acute or chronic diseases which may result in a variety of renal complications.Citation2 These can be a direct consequence of the parasite’s life cycle or more often caused by either the host’s immune response to infection. Echinococcosis or hydatid disease is caused by larvae of the tapeworm, Echinococcus. The usual life-cycle is between dogs and sheep, with humans infrequently accidental hosts.Citation3 The embryos escape from the eggs, penetrate the intestinal mucosa of the human host, and enter the portal circulation. Although most larvae are filtered out by the liver and lungs, some escape to the general circulation to involve other sites such as the kidneys (2%). The larvae that are not destroyed develop into hydatid cysts.Citation4
Different types of kidney involvement were reported with hydatid cyst disease. Most reports of hydatid disease and renal involvement concern development of renal cysts.Citation4 A few cases of glomerular lesions that presented with nephrotic syndrome associated with hydatid disease have been described. The histological changes reported have been minimal change lesion and disease, membranous nephropathy, and mesangiocapillary glomerulonephritis.Citation3,Citation5–Citation7
Miatello and colleaguesCitation8 were the first to describe a patient in whom nephrotic syndrome disappeared following the excision of a pulmonary hydatid cyst. Subsequently in 1981, Vialtel and colleaguesCitation5 and Sánchez Ibarrola and colleaguesCitation6 reported a case each of membranous nephropathy secondary to hydatid cyst. Both the cases had resolved by surgical resection of the cyst. In 1996, Covic and colleaguesCitation3 reported a 67-year-old patient who had developed mesangiocapillary glomerulonephritis secondary to hepatic hydatid disease who responded to the removal of the echinococcal cysts. Gelman and colleaguesCitation7 also described a 63-year-old man with minimal change glomerulonephritis. Oner and colleaguesCitation9 reported a case of post-infectious glomerulonephritis associated with hepatic hydatid disease. des Grottes and colleaguesCitation10 reported a case with secondary immunoglobulin A (IgA) glomerulonephritis. Kaaroud and colleaguesCitation11 reported a case where renal amylodosis had a recovery after cyst resection and colichicine treatment.
Most cases of glomerular lesions associated with hydatid disease are reported to be reversible by treating the infection.Citation3,Citation5 Moreover, Viatel and colleaguesCitation5 eluted echinococcal antigens and antibodies to these antigens from renal tissue of their patient; supporting an immune-complex-mediated pathogenesis. The naturally existing model of E. granulosus-associated membranoproliferative glomerulonephritis in sheep might help to unravel the mechanisms involved in this disease,Citation12 but follow-up of these studies has not been reported. Edelweiss and colleaguesCitation12,Citation13 had been successful in showing echinococcal antigen and corresponding antibody in the glomeruli by immunoperoxidase studies. Continual antigen presentation as an E. granulosus antigen may cause long-lasting antibody response that causes antigen-antibody deposition in the glomerular basement membrane.Citation14 Although we were unable to demonstrate the E. granulosus antigens in the basement membrane of our patient, the aforementioned clinical course favors an association between this infectious agent and the nephrotic syndrome of this patient.
Disclosure
The authors report no conflicts of interest in this work.
References
- MusacchioEMitchellNPrimary renal echinococcosis: a case reportAm J Trop Med Hyg1966672880883
- ThuraisinghamRAduDRenal disease in the tropicsCookGManson’s Tropical DiseasesLondonWB Saunders1996174192
- CovicAMititiucICaruntuLGoldsmithDJA Reversible neprotic syndrome due to mesangiocapillary glomerulonephritis secondary to hepatic hydatid diseaseNephrol Dial Transplant199611207420768918727
- van VelthuysenMLFlorquinSGlomerulopathy associated with parasitic infectionsClin Microbiol Rev2000131556610627491
- VialtelPChenaisFDesgeorgesPCoudercPMicouinCCordonnierDMembranous nephropathy associated with hydatid diseaseN Engl J Med1981304106106117453732
- Sánchez IbarrolaASobriniBGuisantesJMembranous glomerulonephritis secondary to hydatic diseaseAm J Med19817023113157468614
- GelmanRBrookGGreenJBen-ItzhakONakhoulFMinimal change glomerulonephritis associated with hydatid diseaseClin Nephrol200053215215510711418
- MiatelloVRZanettiNL[Disappearance of a nephrotic syndrome following the excision of a pulmonary hydatic cyst]Medicina (B Aires)19743455325384437390
- OnerADemercinGAkhanOOnerKRenal hydatid cyst detected in a child during the course of acute poststreptococcal glomerulonephritisNephron19956921931947723915
- des GrottesJMOana-CahoolessurMNevePVanhaeverbeekM[Mediastinal and pulmonary hydatidosis, bronchocentric granulomatosis and IgA glomerulonephritis]Acta Clin Belg19934853383438291343
- KaaroudHBen MoussaFBéjiSKhederABen MaïzH[Renal amyloidosis secondary to hydatid cyst of the liver. Clinical remission after surgical excision]Nephrologie200223521321712227254
- Albano EdelweissMILizardo-DaudtHMNaturally existing model of glomerulonephritis mediated by immune complexes associated with hydatidosis in sheepNephron19915722532541826941
- EdelweissMIDaudtHMGoldsteinHFGarciaC[Hepatic hydatidosis with glomerular involvement: report of a case]Rev Assoc Med Bras199238131321307057
- WardleENMinimal change nephrosis and allergyNephron19967424224238893168