Abstract
A 35-year-old male who had been receiving conservative treatment for L4 isthmic spondylolisthesis suffered from pyogenic spondylodiscitis in the degenerative L4/L5 intervertebral disc space, which could be identified by comparison with previous images. Symptoms improved with conservative antibiotic treatment. Neovascularization may occur in the annulus fibrosus of a degenerative intervertebral disc, which may increase the risk of hematogenous infection, leading to “discitis” even in adults.
Introduction
In many cases of pyogenic spondylodiscitis, infection occurs primarily in the anterior corner of the vertebral body, and the infected lesion gradually extends to the adjacent vertebra via an intervertebral disc. However, we often encounter cases in which infectious changes are seen only in an intervertebral disc space without bone destruction or spur formation in the anterior corner of the vertebral body. Although an intervertebral disc is avascular in adults, such cases seem to be similar to “discitis” in infants. In these cases, the primary focus of the infection may not be an anterior corner of the vertebral body but in an intervertebral disc itself. Various factors, such as intervertebral disc degeneration, may be involved in the occurrence of hematogenous infection directly to an intervertebral disc in adults. However, the mechanisms are unclear.
We encountered a patient with pyogenic spondylodiscitis in the slipped intervertebral disc space of lumbar isthmic spondylolisthesis. We were able to confirm by comparison with previous images obtained from the patient that lumbar isthmic spondylolisthesis preceded pyogenic spondylodiscitis and that pyogenic spondylodiscitis developed only in the degenerative disc space. The relationship between degeneration of an intervertebral disc and hematogenous infection with focus on neovascularization into the annulus fibrosus of the degenerated disc is discussed.
Case report
A 35-year-old man, an orthopedic surgeon, had experienced low back pain since the age of 17 years. He was diagnosed with L4 lumbar isthmic spondylolisthesis at the age of 28 years and had been receiving conservative treatment with periodic plain x-ray and magnetic resonance imaging (MRI) examinations (). There was no particular past or familial medical history. In January 2006, he felt severe low back pain and took an oral nonsteroidal anti-inflammatory agent of his own accord, but the pain aggravated the following day. He was admitted to our hospital for close examination and treatment.
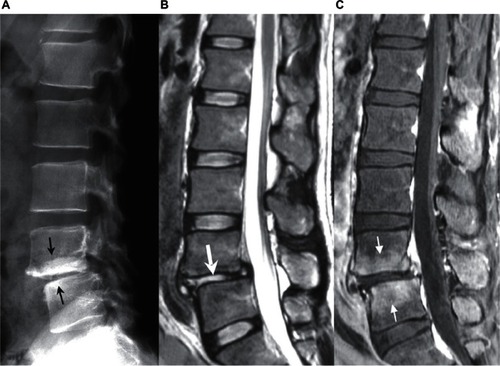
Figure 1 Images 7 months before the onset of pyogenic spondylodiscitis. A) Plain x-ray. Separation of the L4 vertebral arch (small white arrow) and L4/L5 listhesis were noted. B) Plain T2-weighted MRI. The L4/L5 intervertebral disc was degenerated and the height of the intervertebral disc space was decreased (thick white arrow). Separation of ring apophysis of the L4 vertebral body was noted (small black arrow).

His body temperature was 38.5°C and he had severe continuous pain over the entire lumbar region on admission, but no apparent neurologic disturbance was detected. Blood examination showed that his white blood cell (WBC) count and C-reactive protein (CRP) had risen to high levels (8,500/μL and 3.72 mg/dL, respectively). Plain lumbar x-ray and MRI were performed () and the images were compared with those acquired 7 months previously. Although osteosclerosis of the vertebral body adjacent to the L4/L5 intervertebral disc space was noted on x-ray images, height and slip amount of the L4/L5 disc space was not changed, and no apparent bone destruction or spur formation was seen in the anterior corner of the vertebral bodies. An apparent change in the signal intensity of the L4/L5 disc space was noted on T2-weighted MRI, and the vertebrae adjacent to the L4/L5 disc space were enhanced on gadolinium-enhanced fat-suppressed T1-weighted MRI.
Figure 2 Images on admission. A) Plain x-ray. Although osteosclerosis of the L4 and L5 vertebral bodies was noted (small black arrow), no apparent bone destruction or spur formation was seen in the anterior corner of the vertebral bodies. B) Plain T2-weighted MRI. Signal intensity of the L4/L5 intervertebral disc had apparently changed in comparison with that shown in (thick white arrow). C) Gadolinium-enhanced fat-suppressed T1-weighted MRI. The L4 and L5 vertebral bodies adjacent to the L4/L5 intervertebral disc space were enhanced with gadolinium (small white arrow).
Based on these findings, L4/L5 intervertebral pyogenic spondylodiscitis was diagnosed, and conservative treatment with antibiotics by drip infusion was initiated. Cefazolin sodium was administered intravenously for 40 days (4 g/day for 7 days and 2 g/day for 33 days), followed by oral cefaclor at 750 mg/day for about 3 months. A venous blood culture test performed on the night of admission was negative. WBC count, neutrophil rate, CRP, and erythrocyte sedimentation rate reached maximum levels on the fourth, sixth, and ninth days of treatment, and then gradually decreased (see ). The low back pain gradually improved, and the patient was discharged after 2 months and was able to walk with a semirigid corset attachment.
Table 1 Time courses of WBC count, neutrophil count, CRP, and ESR
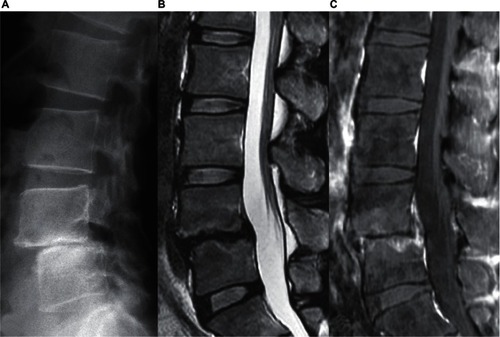
On plain lumbar x-ray taken 6 months after treatment, the L4/L5 disc space was lost and instability present before the occurrence of pyogenic spondylodiscitis was resolved. The marked signal intensity of the L4/L5 intervertebral disc space on MRI had disappeared, but enhancement of the adjacent vertebral bodies remained (). There has been no recurrence of low back pain as of about 4 years after treatment and the patient has returned to work as an orthopedic surgeon.
Figure 3 Images 6 months after treatment. A) Plain x-ray. The L4/L5 intervertebral space was lost. B) Plain T2-weighted MRI. The high signal intensity of the L4/L5 intervertebral disc was resolved. C) Gadolinium-enhanced fat-suppressed T1-weighted MRI. Enhancement in the adjacent vertebral bodies remained.
Discussion
To our knowledge, there have been only 4 reports of lumbar isthmic spondylolisthesis and pyogenic spondylodiscitis occurrence in the same intervertebral region,Citation1–Citation4 although the actual frequency of occurrence is unclear. The reasons for infection of the listhetic intervertebral space were not discussed in those reports because all cases were primarily examined at the onset of pyogenic spondylodiscitis and, therefore, no images preceding pyogenic spondylodiscitis were available. In contrast, our case provided evidence based on comparison with previous images that lumbar isthmic spondylolisthesis and intervertebral disc degeneration preceded pyogenic spondylodiscitis and that pyogenic spondylodiscitis occurred in the degenerative disc space.
The patient was young and had no apparent risk of infection. Furthermore, infection occurred only in the degenerative intervertebral disc space. These facts suggest that degeneration of an intervertebral disc might be related to susceptibility to microbial infection.
Since there is circulation in the annulus fibrosus of the intervertebral disc in infants,Citation5–Citation7 the initial stage of disc space infection in infants is considered to be “discitis”.Citation8–Citation10 In adults, in contrast, the intervertebral artery terminates in the cancellous bone proximal to the vertebral end plate and thus the intervertebral discs are avascular in nature. Thus, the initial stage of disc space infection in adults is considered to be “spondylitis” or “vertebral osteomyelitis”.Citation5,Citation10–Citation12 However, in some studies, high expression levels of vascularization-related growth factors were noted in the annulus fibrosus of degenerative discs with progression of vascularization.Citation13–Citation15 These observations suggest that the annulus fibrosus may occasionally be the primary site of hematogenous infection,Citation16 and that the risk of hematogenous infection increases with progression of disc degeneration. Thus, not only “spondylitis” or “vertebral osteomyelitis”, but also “discitis”, may occur in an adult who has disc space degeneration. Although results of some retrospective clinical studiesCitation17,Citation18 suggesting a correlation between disc degeneration and infection might support these hypotheses, many aspects still remain unclear and further investigation is necessary.
The patient was an orthopedic surgeon, and therefore the subjective symptoms and the clinical progress described above were considered to be objective and accurate. The patient was informed that data and photographs from the case would be submitted for publication, and his consent was given.
Disclosure
The authors report no conflict of interest in this work.
References
- SmorgickYFlomanYAneksteinYShitritRCopeliovitchLMirovskyYDiscitis and isthmic spondylolisthesis: A case reportJ Pediatr Orthop B200817394118043376
- GuglielminoASorbelloMMurabitoPA case of lumbar sciatica in a patient with spondylolysis and spondylolysthesis and underlying misdiagnosed brucellar discitisMinerva Anestesiol20077330731217529921
- NagashimaHMorioYNishiTHaginoHTeshimaRSpontaneous fusion of isthmic spondylolisthesis after discitis: A case reportClin Orthop Relat Res200240310410712360015
- WynneATSouthgateGWDiscitis causing spondylolisthesis. A case reportSpine1986119709723824075
- RudertMTillmannBLymph and blood supply of the human intervertebral disc. Cadaver study of correlations to discitisActa Orthop Scand19936437408451943
- WhalenJLParkeWWMazurJMStaufferESThe intrinsic vasculature of developing vertebral end plates and its nutritive significance to the intervertebral discsJ Pediatr Orthop198554034104019751
- RobertsSEvansHTrivediJMenageJHistology and pathology of the human intervertebral discJ Bone Joint Surg Am200688Suppl 2101416595436
- ScolesPVQuinnTPIntervertebral discitis in children and adolescentsClin Orthop Relat Res198216231367067229
- SongKSOgdenJAGaneyTGuideraKJContiguous discitis and osteomyelitis in childrenJ Pediatr Orthop1997174704779364386
- WileyAMTruetaJThe vascular anatomy of the spine and its relationship to pyogenic vertebral osteomyelitisJ Bone Joint Surg Br195941B79680913855377
- RatcliffeJFAnatomic basis for the pathogenesis and radiologic features of vertebral osteomyelitis and its differentiation from childhood discitis. A microarteriographic investigationActa Radiol Diagn (Stockh)1985261371433993417
- RatcliffeJFThe arterial anatomy of the adult human lumbar vertebral body: A microarteriographic studyJ Anat198013157797440404
- AliRMaitreCLRichardsonSMHoylandJAFreemontAJConnective tissue growth factor expression in human intervertebral disc: Implications for angiogenesis in intervertebral disc degenerationBiotech Histochem20088323924519016368
- BoosNWeissbachSRohrbachHWeilerCSprattKFNerlichAGClassification of age-related changes in lumbar intervertebral discsSpine2002272631264412461389
- KauppilaLIIngrowth of blood vessels in disc degeneration. Angiographic and histological studies of cadaveric spinesJ Bone Joint Surg Am19957726317822352
- KempHBJacksonJWJeremiahJDHallAJPyogenic infections occurring primarily in intervertebral discsJ Bone Joint Surg Br1973556987144766176
- TanigawaNAkagiSKatoYSasaiKSaitoTIidaHVertebral osteomyelitis of the cervical spineSeikei-Saigai Geka. (Orthopaedic Surgery and Traumatology)200346767774 Japanese
- SaigaMKawaiSTreatment from the viewpoint of clinical features of cervical purulent spondylitisMon Book Orthop199693741 Japanese