Abstract
Cardiac involvement, as an initial presentation of malignant lymphoma is rare. We report a 42-year-old Taiwanese man with frequent syncope. Routine electrocardiography disclosed complete atrioventricular block. Before permanent pacemaker implantation was undertaken, transthoracic echocardiography revealed a solid mass infiltrating the left atrium and interatrial septum. Transesophageal echocardiography proved cardiac neoplasm with biatrial infiltration. Endomyocardial tissue biopsy was performed under angiography guide. Pathology diagnosis unraveled large B-cell lymphoma. Despite aggressive chemotherapy, the patient’s condition worsened and he died 2 months later.
Introduction
Cardiac lymphoma is a rare disease with a high mortality rate. When this malady is diagnosed prognosis is usually grim due to the advanced stage of myocardial involvement at presentation. It is defined as non-Hodgkin’s lymphoma with heart and/or the pericardium involvement only. Primary cardiac lymphoma accounts for 1.3% of primary cardiac tumors and 0.5% of the extranodal lymphomas.Citation1 However, disseminated cardiac lymphoma is more common, with an incident rate at 15%~30%, of all lymphoma in various post-mortem series.Citation2,Citation3 The prognosis of both primary and disseminated cardiac lymphoma remains grave, largely because of late presentation and substantial delay at the critical point of initial diagnosis. Here, we report a uremic patient presenting with frequent syncope. His intriguing clinical course is delineated below.
Case report
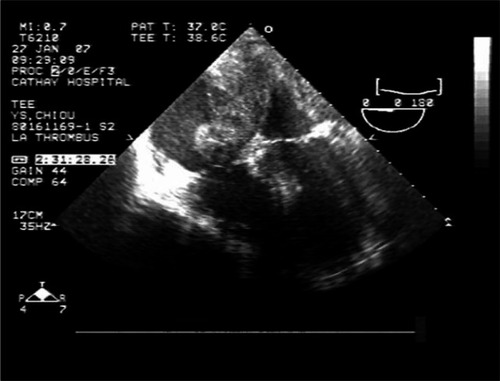
A 42-year-old Taiwanese man with diabetic nephropathy in a uremic stage received regular hemodialysis in our hospital. He presented to our outpatient department with frequent syncope over a period of one month. Electrocardiogram revealed complete atrioventricular block with junctional escape rhythm (). Before a permanent pacemaker was implanted, transthoracic echocardiography revealed a massive infiltrative thickening of the inferior aspect of the left atrial septum and interatrial septum mimic thrombus (). Ensuing transesophageal echocardiography revealed a mass attached to the interatrial septum and protruding into both atrial cavities (). Assayed tumor markers were all within the normal range (carcinoembryonic antigen [CEA], alpha-fetoprotein [AFP], cancer antigen [CA 19-9]). An epicardial permanent pacemaker implantation was performed due to the right atrial mass and fear of tumor embolization. During the procedure of pacemaker implantation a pericardial biopsy was performed.
Figure 1 Electrocardiogram revealing complete atrioventricular block with junctional escape rhythm (arrows).
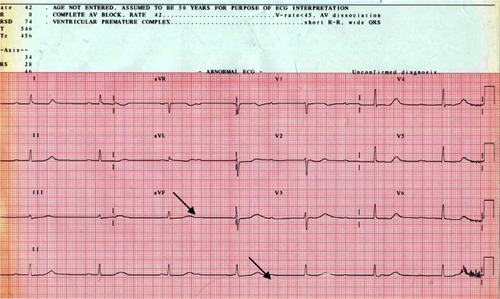
Figure 2 An ultrasonogram showing a massive infiltrative thickening of the posterior aspect of the left atrial septum and interatrial septum.
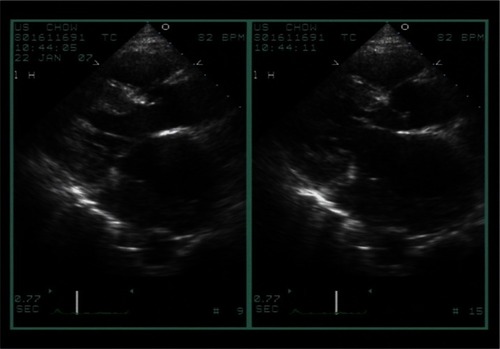
Figure 3 Transesophageal echocardiography showing tumor masses attached to the interatrial septum and protruding into both atrial cavities.
Multislice computed tomography (MSCT) revealed a bulky infiltrative mass 8.62 cm × 6.45 cm × 9 cm at the posterior-lateral and inferior aspect of the left atrium with invasion to myocardium, the interatrial septum, tricuspid valve, right atrium, pericardium, left hilar region and left pleura (). There are lymph nodes in the paratracheal regions, paraaortic regions and highest mediastinum. To confirm the occult tumor origin and check if there were metastases, we arranged positron electric tomography (PET). After intravenous injection of 10 mCi of FCitation18-labeled 2-deoxyglucose (FDG), upper body and brain studies were performed with a Philips Gemini GXL PET/CT scanner. Images were reconstructed using line of response (LOR) reconstruction with computer tomography (CT) attenuation correlation. FDG-PET scans revealed increased glucose metabolism in the right atrium (RA), interatrial septum and left atrium (LA). The maximal standardized uptake value (SUV) value was 9.24. However, the result showed no abnormal radiotracer uptake in the pleura and lymph nodes ().
Figure 4 A multislice computed tomogram showing a bulky infiltrative mass about 8.62 cm × 6.45 cm × 9 cm at posterior-lateral and inferior aspect of the left atrium with invasion to myocardium, the interatrial septum, tricuspid valve, right atrium, pericardium, left hilar region, and left pleura (arrow).
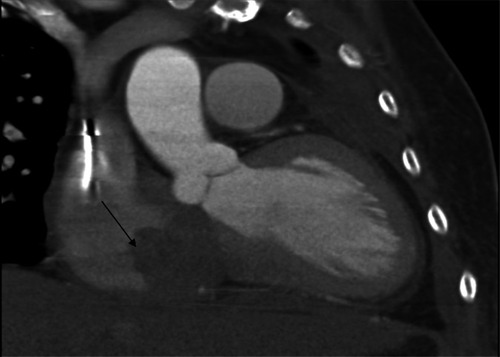
Figure 5 FDG-PET revealed remarkably increased glucose metabolism in the RA, interatrial septum, LA, and in a tumor mass protruding from the posterior aspect of pericardium.
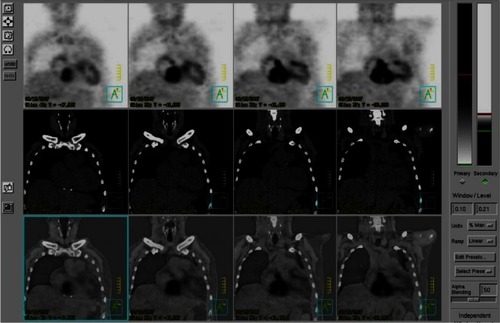
Figure 6 Section showing monotonous proliferation of large centroblast-like lymphoid cells having round to irregular nuclei, with vesicular chromatin and distinct 1 to 3 nucleoli and a moderate amount of cytoplasm (arrow).
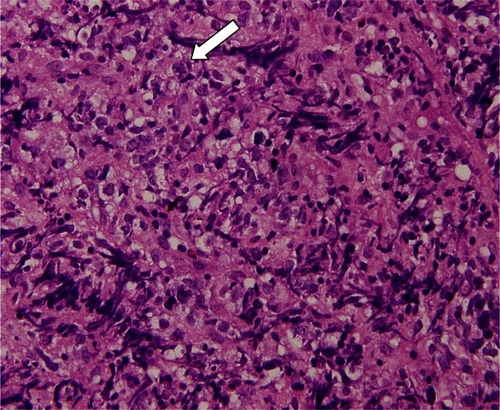
Transvenous endomyocardial biopsy was undertaken, under fluoroscopic guidance, for pathologic diagnosis. The pathology report confirmed the presence of a diffuse large B-cell lymphoma. Immunohistochemically, the large tumor cells are strongly although diffusely positive for CLA (common leukocyte antigen) and CD20 (a marker for B-cells), admixed with small reactive CD3+/CD5+ T cells, but negative for cytokeratin, S-100, chromogranin, CD56, desmin, FLI-1, and CD34 (). The patient was thus referred to a hematologist for chemotherapy with regimens of CHOP (cyclophosphamide, doxorubicin, vincristine, and prednisone) for 3 courses, with rituximab for 2 courses. Before the first course, a bone marrow biopsy was performed and the pathology report showed no evidence of bone marrow involvement. One month after chemotherapy, noncapture of the permanent pacemaker was found during hemodialysis with symptoms of malaise. The permanent pacemaker was thus adjusted by increasing output to maintain capture. Unfortunately, the patient suffered sudden cardiac death 2 months after chemotherapy.
Discussion
Cardiac tumors can be divided into primary cardiac tumors from heart and secondary cardiac tumors metastasized to heart. The documented incidence of primary cardiac tumors ranged from 0.17% to 0.19% in unselected autopsy series. Approximately 75% of primary cardiac tumors are benign, with the residual 25% being malignant. Fifty percent of benign tumors are myxomas. Among cardiac malignant tumors: angiosarcomas; rhabdomyosarcomas; malignant mesotheliomas; and fibrosarcomas are among most common. Lymphomas may arise from the heart, although the occurrence is rare. Primary cardiac lymphoma accounts for just 1.3% of primary cardiac tumors and 0.5% of the extranodal lymphomas.Citation14
Cardiac involvement at first presentation of malignant lymphoma is rare. When compared with cardiac lymphoma, disseminated cardiac lymphoma occurs more frequently. Cardiac lymphoma invades primarily the right atrium, followed by the right ventricle, the left ventricle, and finally the atrial septum.Citation5,Citation6 Primary cardiac lymphomas originating in left atrium, as found in this case are rare. This makes the differential diagnosis of myxomas or atrial thrombus important. Myxomas often involve the left atrium and might protrude into the left ventricle.Citation7 Atrial thrombus is often found in the left atrial appendage under the condition of rheumatic mitral stenosis or atrial fibrillation. Our patient presented with syncope and complete atrioventricular block. The reported age of patients with this condition, at presentation, is usually in the mid-60s although range is from 13- to 90-year-olds.Citation1 There is no pathognomonic clinical picture suggestive of primary cardiac lymphoma. All clinical presentations are related to the site of primary cardiac lymphoma involvement. Clinical presentations varies range from: congestive heart failure; dyspnea;Citation8 fainting; syncope; atrial or ventricular arrhythmia;Citation9–Citation11 neoplastic pulmonary embolism;Citation12 pericardial effusion;Citation13 pleural effusion; myocardial infarction; stroke;Citation14 and sudden cardiac death. Elevation of the erythrocyte sedimentation rate, lactate dehydrogenase and inerleukin-2 receptor concentration are the main laboratory indicative features.Citation15 Electrocardiography findings include: atrial flutter; fibrillation; bundle branch block and low voltage.Citation9–Citation11 Transthoracic echocardiography is a basic tool to identify pericardial effusion, pleural effusion and lesion of tumor. However, it does yield lower sensitivity. Additionally, transesophageal echocardiography provides better visualization of any suspicious cardiac mass and cardiac structure than transthoracic echocardiography.Citation16
Computer tomography and magnetic resonance imaging (MRI) provide more precise assessment of tumor morphology: composition, number and extent than echocardiography. They are also superior in the detection of pericardium and paracardiac structures such as in the mediastinum, great vessels and lungs.Citation17 Cardiac lymphoma with pericardium or pleura involvement could be diagnosed by cytology of associated pericardial or pleural effusion. If cytological diagnosis from serous fluid is inclusive, invasive biopsy should then be performed immediately.Citation1 The prognosis of primary cardiac lymphoma could be improved with early diagnosis and early chemotherapy. Biopsy procedures such as: transesophageal echocardiography-guided biopsy,Citation18 transvenous angiography-guided biopsy,Citation1,Citation7 mediastinoscopic biopsy or thoracoscopic biopsy are less invasive. Although direct thoracotomy biopsy is more invasive it yields a more accurate diagnosis rate. In pathology, the majority of primary cardiac lymphoma are large B-cell type, B-cell neoplasms. In immunophenotypic studies, cardiac lymphomas can be distinguished from other cardiac neoplasms on the basis of their reactivity for common leukocyte antigen and pan B-cell markers (CD 20) or pan T-cell makers (CD 3). Diffuse B-cell lymphoma accounts for about 80% of primary cardiac lymphomas in immunocompetent patients. In immunodeficiency patients, small noncleaved or immunoblastic lymphomas are more frequent.Citation19 Increased glucose metabolism in the myocardium and/or pericardium, without abnormal exracardiac radiotracer uptake found by FDG-PET, would confirm the lymphoma being confined to the heart. Treatment includes chemotherapy, radiotherapy and surgery. Some researchers recommend a therapeutic strategy which includes CHOP chemotherapy. however, CHOP chemotherapy with rituximab is more effective than CHOP chemotherapy on its own Other strategies include chemotherapy with radiotherapy, which appear to prolong the survival period.Citation1
In summary, primary cardiac lymphoma is a rare and often fatal malignancy with varied clinical presentation depending upon the site of tumor involvements. Early diagnosis and early treatment promises better prognoses. Transthoracic echocardiogram is traditionally used as a screening tool for any cardiac mass although it lacks the precise diagnostic rate of other techniques. Transesophageal echocardiogram, an invasive and operator dependent technique, provides better visualization of suspicious cardiac masses and cardiac structure, especially in though involving the atria. CT or MRI yields more detailed views of the mass location and extent of the tumor as compared to echocardiography. Biopsy for pathology diagnosis and therapy should be done as soon as possible after first presentation as the tumor growth rate is rapid and the diminishing prognosis is grave.
Disclosures
The authors report no conflicts of interest relevant to this study.
References
- CeresoliGLFerreriAJBucciERipaCPonzoniMVillaEPrimary cardiac lymphoma in immunocompetent patients: diagnostic and therapeutic managementCancer1997808149715069338475
- MukaiKShinkaiTTominagaKShimosatoYThe incidence of secondary tumors of the heart and pericardium: a 10-year studyJpn J Clin Oncol19881831952013411785
- McDonnellPJMannRBBulkleyBHInvolvement of the heart by malignant lymphoma: a clinicopathologic studyCancer19824959449517037154
- McAllisterHAMcAllisterJJFTumors of the cardiovascular systemAtlas of Tumor PathologyWashington DCArmed Forces Institute of Pathology1978
- GrebencMLRosado de ChristensonMLBurkeAPGreenCEGalvinJRPrimary cardiac and pericardial neoplasms: radiologic-pathologic correlationRadiographics20002041073110310903697
- SaotomeMYoshitomiYKojimaSKuramochiMPrimary cardiac lymphoma-a case reportAngiology200253223924111952118
- NguyenDTMeierCRSchneiderDPrimary cardiac lymphoma mimicking left atrial myxoma in an immunocompetent patientJ Clin Oncol200826115015218165648
- RobertsCSGottdienerJSRobertsWCClinically undetected cardiac lymphoma causing fatal congestive heart failureAm Heart J19901205123912422239684
- HayesDLilesDKSorrellVLAn unusual cause of new-onset atrial flutter: primary cardiac lymphomaSouth Med J200396879980214515922
- ZahariaLGillPSPrimary cardiac lymphomaAm J Clin Oncol19911421421452028920
- TaiCJWangWSChungMTComplete atrio-ventricular block as a major clinical presentation of the primary cardiac lymphoma: a case reportJpn J Clin Oncol200131521722011450997
- BestettiRBSoaresFASoaresEGOliveiraJSPrimary lymphoma of the right atrium with fatal neoplastic pulmonary embolismAm Heart J19921244108810901529888
- RoseAGGrobbelaarJCommerfordPJPericardial effusion and heart block caused by lymphoma. A case reportS Afr Med J19887452402423413616
- BinderJPflegerSSchwarzSImages in cardiovascular medicine. Right atrial primary cardiac lymphoma presenting with strokeCirculation200411017e451e45215505107
- MakishimaHIsobeMImamuraHA case of primary cardiac lymphoma: utility of serum soluble interleukin-2 receptor for noninvasive diagnosisInt J Cardiol19986532912939740487
- MüggeADanielWGHaverichALichtlenPRDiagnosis of non-infective cardiac mass lesions by two-dimensional echocardiography. Comparison of the transthoracic and transesophageal approachesCirculation199183170781984900
- DorsayTAHoVBRoviraMJArmstrongMABrissetteMDPrimary cardiac lymphoma: CT and MR findingsJ Comput Assist Tomogr19931769789818227590
- BurlingFDevlinGHealdSPrimary cardiac lymphoma diagnosed with transesophageal echocardiography-guided endomyocardial biopsyCirculation200010117E179E18110790358
- DuongMDuboisCBuissonMNon-Hodgkin’s lymphoma of the heart in patients infected with human immunodeficiency virusClin Cardiol19972054975029134285