Abstract
A 28-year-old female presented with a huge intra-abdominal mass. Initially a mesenteric mass was diagnosed, but her tumor was found to be a gastrointestinal stromal tumor (GIST). Laparotomy was performed. The mass was resected en bloc with clear surgical margins in January 2007. It was found to be 20 × 18 × 16 cm. In order to remove the tumor, the left half of transverse colon with its mesocolon, spleen, body and tail of pancreas, and a part of the small intestine had to be removed. The mass was tightly attached to these viscera. The tumor was surgically removed three years ago. The pathology report of the case presented places the tumor in the high-risk category. The tumor had a relatively high mitotic index. It was positive for CD117 and CD34 stains and also positive for smooth muscle actin. Although the patient did not receive adjuvant chemotherapy, no signs of local recurrence or distant metastasis could be recognized on follow up. Surgery remains the standard initial management for all localized GISTs. The tumor should be removed en bloc, with clear surgical margin. The case presented indicates no association of tumor size with early local recurrence of the tumor or early distant metastasis.
Introduction
Gastrointestinal stromal tumors (GISTs) are rare in the Egyptian population. GISTs are the most common nonepithelial tumors of the gastrointestinal tract.Citation1 Surgery is the primary therapy of choice and for a long time has been the only effective therapy for GIST with an overall five-years survival rate of 45%–55%.Citation2 Uncertainty remains whether an individual tumor is benign or has the potential for metastatic spread.Citation3
Case presentation
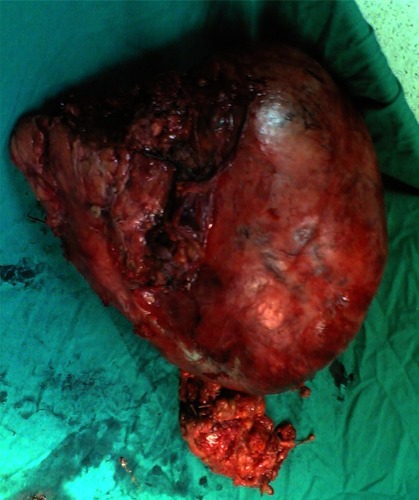
A 28-year-old Egyptian female presented with abdominal pain and distension. Written informed consent was obtained from the patient for publication of this case report and accompanying images. There was no family history of malignant tumors. Clinical examination revealed a large abdominal mass in the upper left quadrant of the abdomen. An abdominal computerized tomography (CT) imaging demonstrated an intra-abdominal mass related to the upper border of pancreas and mesentery of transverse mesocolon, without invasion of adjacent viscera. CT examination did not detect any abdominal distant metastasis. Provisional diagnosis was a huge mesenteric mass. Laparotomy was performed. The mass was resected en bloc with clear surgical margins in January 2007. It was found to be 20 × 18 × 16 cm. In order to remove the tumor, the left half of transverse colon with its mesocolon, spleen, body and tail of pancreas, and a part of the small intestine had to be removed ( and ). The mass was tightly attached to these viscera. The spleen was also removed because the splenic vein was ligated as it was traversing the tumor mass.
Figure 1 The anterior aspect of a GIST presenting as a huge abdominal mass attached to the left half of transverse colon with its mesocolon, body and tail of pancreas, and a part of the small intestine removed from a 28-year-old female.
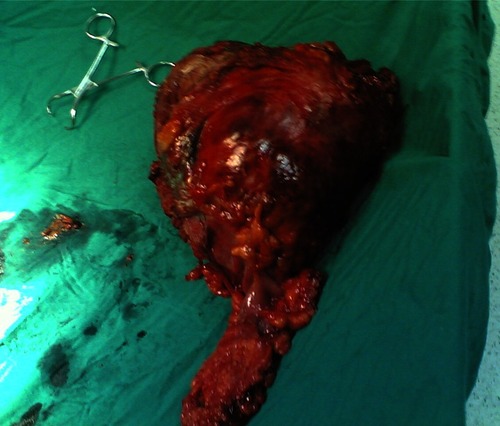
Figure 2 The posterior aspect of a GIST presenting as a huge abdominal mass attached to the left half of transverse colon with its mesocolon, body and tail of pancreas, and a part of the small intestine removed from a 28-year-old female.
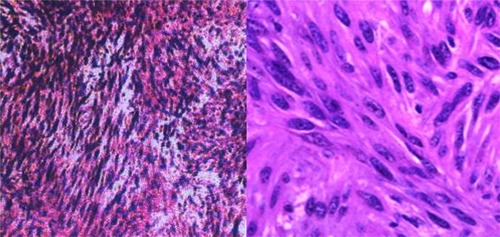
Pathology results demonstrated a malignant noncapsulated gastrointestinal stromal tumor. Tumor showed an advancing pushing border. The tumor was attached to the removed adjacent viscera without invasion. The tumor proved to be GIST. Histopathology examination revealed that local excision was complete with clear margins. The tumor consisted of spindle-shaped cells with twisted nuclei. There was a marked myxoid change. Numerous mast cells were demonstrated. Mature fat cells were demonstrated in clusters within the tumor tissue (). The tumor cells were positive for CD117 and CD34 stains and were also focally positive for smooth muscle actin. They were found to be negative for desmin and S100 protein immunochemical stains. The tumor had 7 mitoses per 50 high-power fields (HPFs).
Figure 3 The pathological examination of a GIST presenting as a huge abdominal mass removed from a 28-year-old female.
The postoperative period passed smoothly except for a mild wound infection. No chemotherapy was given to the patient. The patient was followed-up for three years with an abdominal CT examination every six months and no signs of local recurrence was found. Investigations also revealed no distant metastasis.
Follow-up of the case for the next five years is planned to detect tumor recurrence or distant metastasis.
Discussion
Gastrointestinal stromal tumors (GISTs), although relatively rare, comprising only 0.1% to 3% of all gastrointestinal neoplasms, are the most common mesenchymal tumors of the gastrointestinal tract.Citation4 The vast majority of patients with GIST did not inherit mutations that cause GIST from their parents. Instead the initiating mutation developed in one or more cells sometime during their life. Acquired mutations in the KIT proto-oncogene have been found to be involved in the pathogenesis of GISTs,Citation5 and germline KIT mutations have been identified in rare cases with multiple occurrences of GIST among blood relatives.Citation6 This mutation starts a chain of events that eventually develops into GIST. Despite recent advances in chemotherapeutic regimens, such as introduction of targeted therapy with inhibitors of tyrosine kinase receptors,Citation7 surgical resection is still considered the treatment of choice for GIST.Citation8 The efficacy of chemotherapy is low, with response rates less than 10%.Citation9 GIST does not involve the bowel wall concentrically. As a result bowel obstruction is rare, despite the large size of the GIST.Citation10 Despite apparently complete resection with clear margins, the recurrence rate is high; hepatic or mesenteric recurrence occurs in 40%–90% of patients undergoing apparently curative surgery.Citation11 This may be partly due to tumor rupture leading to mesenteric implants; hence, the risk of recurrence emphasizes the importance of meticulous surgery.Citation12 For this reason, percutaneous biopsy is best avoided.Citation13 Eighty percent of GISTs recurrences occur within two years of excision.Citation14 Tumor size, mitotic index, and site of the tumor are three key prognostic features used to assess risk of GIST recurrence. DeMatteo and colleagues reported that tumor size greater than 10 cm was a significant risk factor for recurrence.Citation15 Machado-Aranda and colleagues described the prevalence and characteristics of patients with confirmed GIST in a community hospital over a six-year period. In surgically resected tumors, a 42% recurrence rate was found with a median average time of recurrence of 22 months. Pathologic grading and type of surgery were not predictors of rate and timing of recurrence.Citation16 The pathology report of the case presented places the tumor in the high-risk category. The tumor had a relatively high mitotic index. It was positive for CD117 and CD34 stains and also positive for smooth muscle actin. Neither early recurrence nor distant metastasis was identified after three years of follow up. The case presented indicates no association of tumor size with early local recurrence of the tumor or early distant metastasis. The combination of large tumor size, high mitotic index and KIT-positivity was not also associated with early tumor recurrence. It is obvious that this does not exclude future recurrence or metastasis. The patient case should be monitored thoroughly in the next seven years to identify any signs of local or distant recurrence.
Conclusion
GIST is a new classification for a group of mesenchymal tumors. These tumors are different in presentation and behavior. Surgery remains the standard initial management for all localized GISTs. The tumor should be removed en bloc, with clear surgical margin. The case presented indicates no association of tumor size with early metastasis of the tumor.
Disclosures
The authors report no conflicts of interest in this work.
References
- MiettinenMLasotaJGastrointestinal stromal tumors – definition, clinical, histological, immunohistochemical, and molecular genetic features and differential diagnosisVirchows Arch2001438111211213830
- DeMatteoRPLewisJJLeungDTwo hundred gastrointestinal stromal tumors: recurrence patterns and prognostic factors for survivalAnn Surg20002311515810636102
- FletcherCDMBermanJJCorlessCLDiagnosis of gastrointestinal stromal tumors: a consensus approachHum Pathol200233545946512094370
- SakuraiSFukasawaTChongJMC-kit gene abnormalities in gastrointestinal stromal tumors (tumors of interstitial cells of Cajal)Jpn J Cancer Res199990121321132810665649
- RubinBPSingerSTsaoCKIT activation is a ubiquitous feature of gastrointestinal stromal tumorsCancer Res200161118118812111719439
- MaeyamaHHidakaEOtaHFamilial gastrointestinal stromal tumor with hyperpigmentation: Association with a germline mutation of the c-kit geneGastroenterology2001120121021511208730
- ShawerLKSlamonDUllrichASmart drugs: tyrosine kinase inhibitors in cancer therapyCancer Cell20021311712312086869
- PierieJPChoudryUMuzikanskyAYeapBYSoubaWWOttMJThe effect of surgery and grade on outcome of gastrointestinal stromal tumorsArch Surg2001136438338911296107
- DematteoRPHeinrichMCEl-RifaiWMDemetriGClinical management of Gastrointestinal stromal tumors: before and after STI-571Hum Pathol200233546647712094371
- SandrasegaranKRajeshARydbergJRushingDAAkisikFMHenleyJDGastrointestinal stromal tumors: Clinical, radiologic, and pathologic featuresAJR Am J Roentgenol2005184380381115728601
- DematteoRPLewisJJLeungDMudanSSWoodruffJMBrennanMFTwo hundred Gastrointestinal stromal tumors: recurrence patterns and prognostic factors for survivalAnn Surg20002311515810636102
- DematteoRPThe GIST of targeted cancer therapy: a tumor (gastrointestinal stromal tumor), a mutated gene (c-kit), and a molecular inhibitor (STI571)Ann Surg Oncol20029983183912417503
- PidoreckyICheneyRTKraybillWGGibbsJFGastrointestinal stromal tumors: current diagnosis, biologic behavior, and managementAnn Surg Oncol20007970571211034250
- SamiianLWeaverMVelanovichVEvaluation of gastrointestinal stromal tumors for recurrence rates and patterns of long-term follow-upAm Surg2004703187191 discussion19119215055839
- DeMatteoRPGoldJSSaranLTumor mitotic rate, size, and location independently predict recurrence after resection of primary gastrointestinal stromal tumor (GIST)Cancer2008112360861518076015
- Machado-ArandaDMalametMChangYJPrevalence and management of gastrointestinal stromal tumorsAm Surg2009751556019213398