Abstract
Background
The ability for patients to access and consume sufficient quantities of nutrients to meet recommendations for wound management is vital if decline in nutritional status during hospital admission is to be prevented. This study aims to investigate menu quality, consumption patterns, and changes in nutritional status for inpatients with wounds.
Methods
Wound healing recommendations were compared against the nutrient content of the inpatient menu. Individual intakes were compared to estimated requirements: energy using the Schofield equation; protein using wound healing recommendations; vitamin A, C, and zinc using the recommended daily intake (RDI).
Results
The inpatient menu did not provide sufficient energy or zinc to meet the estimated average requirement while the ordering practices of participants allowed all RDI to be achieved except for zinc. Actual intake fell below recommendations: 62%, 41%, 55%, and 79% of patients not meeting energy, minimum protein requirements, vitamin A or zinc RDI respectively. A nonsignificant trend for weight loss, particularly fat mass, was observed over time.
Conclusion
Inpatients with wounds are at risk of being unable to consume sufficient quantities of nutrients important for healing and prevention of decline in nutritional status. This is despite the menu seemingly providing sufficient nutrients. More attention to education, encouragement, and supplementation are recommended.
Keywords:
Introduction
Poorly healed wounds and pressure ulcers are a major health care problem worldwide, with delayed wound healing and wound failure causing significant financial burden on health care systems (CitationArnold and Barbul 2006). There is limited data on the incidence and prevalence of wounds and pressure ulcers in Australia. CitationThe Australian Wound Management Association (2001) reported that pressure ulcer prevalence in Australia ranged from 5.4% to 15.6%. Some estimates within Australia are as high as 37% (CitationQueensland Government 2004). In the United States, the National Pressure Ulcer Advisory Panel (CitationNPUAP 2001) reported incidence rates of 10%–18%. Another American study found an excess mortality rate of 7.2% within 10 years when patients were matched for age, sex, race and diagnosis-related group (CitationStausberg et al 2005). The costs of lower limb wounds alone are estimated at $450–600 million annually in Australia (CitationDarzins et al 2000). The burden associated with pressure ulcers and lower-limb wounds demonstrates the need for effective preventative and treatment strategies.
Nutrition plays an important role in the progression of wound healing. While pre-existing protein-energy malnutrition has been recognized as a risk factor for development of wounds (CitationHimes 1999), there is also evidence that insufficient protein and energy intake contributes to delayed wound healing (CitationThompson and Fuhrman 2005; CitationWilliams and Barbul 2003) and increases the risk of skin breakdown (CitationPeninsula Health 2007) and wound infection (CitationArnold and Barbul 2006).
There is increasing evidence that other nutrients, specifically zinc, arginine and vitamins A, C, and E play an important role in wound healing. This evidence remains controversial due to the lack of high quality epidemiological studies (CitationClark 2003; CitationScholl and Langkamp-Henken 2001), with most clinical practice guidelines based solely on small pilot studies or expert opinion. There is a body of evidence which investigates the impact of various combinations of nutrients which in this study will be termed as multi-nutrient oral nutritional support (ONS). Whilst there is evidence that ONS reduces the incidence of pressure ulcers and may improve the healing of pressure ulcers (CitationStratton et al 2005), it is difficult to decipher the actual effects of individual nutrients.
Little is known about changes in nutritional status during hospital admission among patients with wounds. There is evidence that ONS reduces incidence of pressure ulcers however there is no evidence regarding hospital menu/patient consumption practices and wound healing. There are also limited data available to describe the changes in nutritional status during the hospital admission, the predictors (eg, poor quality of menu, poor intake) and consequences. Hence this study aims to determine: (1) whether the menu quality of a university affiliated teaching hospital in Southern Adelaide, Australia is consistent with current wound healing recommendations; (2) the nutrient intake and menu ordering practices of patients with lower limb wounds or pressure ulcers and compare this to estimated requirements; and (3) whether there are significant changes in nutritional status throughout admission in patients with lower limb wounds or pressure ulcers.
Methods
Participants
This study was designed as a prospective longitudinal study. All participants were recruited from the Vascular Unit of the Repatriation General Hospital (RGH), Adelaide, South Australia. Patients admitted to the RGH Vascular Unit with a lower limb wound or pressure ulcers and whom were available to participate within 48 h of wound identification or admission, were screened for inclusion into the study from August 2007 until November 2007. The exclusion criteria were: (1) palliative care patients receiving comfort care, (2) Intensive Care Unit (ICU) patients, as their condition may inhibit active participation in the study, (3) patients whom were unable to fulfill the requirements of the study due to impaired cognitive function, and (4) patients receiving nutrition via enteral feeding or total parenteral nutrition (TPN).
The study was approved by the RGH Research and Ethics Committee and registered with the Australian and New Zealand Clinical Trials Registry [Protocol: ACTRN12607000308493]. All participants provided written informed consent prior to commencement of data collection.
Measurements and procedures
All patients taking part in the study were visited in hospital by a trained researcher whom assessed their nutritional status using a range of parameters: weight, knee height, fat-free mass, fat mass, appetite questionnaire, and a 24-h food recall within 48 h of their admission or identification of the wound. The measurements were repeated at 5–6 day intervals to a maximum of three visits or until patients were discharged (which ever occurred first) to assess changes in nutritional status during hospital admission. Baseline demographic information including age, gender, living accommodation, and type of wound was obtained from medical records.
Weight
Weight was measured using calibrated scales (±0.1 kg) (Wedderburn TI BWB-800C, Australia) to evaluate changes in nutritional status over time and to determine individual energy and protein requirements. All participants were weighed in the morning, in light clothing and without shoes. For patients with an amputation, post-amputation weight was used and the weight of the removed limb was estimated according to standard equations (CitationOsterkamp 1995) and added to obtain estimated weight.
Knee height
Knee height was measured as an estimate for height as the majority of patients were unable to stand in the correct position for accurate measurement of height due to lower limb wounds. Knee height (± 0.1 cm) was measured using a caliper with a fixed foot plate and an adjustable, sliding end plate with the lower right leg positioned at an angle of 90° (Ross Laboratories, OH, USA). Standard equations for age and gender were used to estimate height (CitationChumlea 1992).
Body mass index (kg/m2)
Weight and estimated height was used to calculate estimated body mass index (BMI: kg/m2). The definitions for BMI used for participants aged below 65 years were ‘desirable’ or 20–25 kg/m2, ‘overweight’ or 25–30 kg/m2 and ‘obese’ or >30 kg/m2 (CitationWHO 1998). The definitions for BMI used for participants aged above 65 years were ‘desirable’ or 22–27 kg/m2, ‘overweight’ or >27–32 kg/m2 and ‘obese’ or >32 kg/m2 (CitationLipski 1996).
Fat and fat-free mass
Bioimpedance spectroscopy (BIS) was used to determine body composition. BIS is a valid, portable and relatively inexpensive method of estimating fat-free mass (FFM) (± 0.1 kg) and fat mass (FM) (± 0.1 kg) (CitationKyle et al 2001; CitationLupoli et al 2004). Impedance was measured in the morning with an empty bladder (after at least 8 h fasting) between the wrist and ankle using a tetrapolar electrode method as recommended by the manufacturer (ImpediMed SFB7 Multi-Frequency Analysis Version 5.2.4.0, Eight Mile Plains, Qld, Australia). The participants were dressed in light clothing, without shoes, socks, and jewellery and were instructed to lay supine with arms separated from the body and legs not touching each other. All measurements were taken on the right side unless a wound prevented this, in which case the left side was used. FFM and FM were not measured in participants if lower limb dressings were in situ or in patients with severe edema as edema interferes with measurement accuracy. Measurements were taken on the nonaffected limb in patients with an amputation (CitationKyle et al 2004). Recommended reference ranges for FM for men and women aged 15–98-years-old in the normal BMI range of 20–25 kg/m2 are 13.4% to 21.7% and 24.6% to 33.2%, respectively (CitationKyle et al 2003).
Appetite survey
Appetite was determined using the Simplified Nutritional Appetite Questionnaire (SNAQ) (CitationWilson et al 2005) a validated, four-item questionnaire addressing level of appetite, satiety, taste, and number of meals consumed per day. Patients scoring below than or equal to 14 were considered to be at significant risk of losing at least 5% of their body weight within six months.
Meal quality of RGH menu
The menu at RGH includes breakfast, lunch, and dinner. For breakfast, participants are given choices of either porridge or cereal with a hot dish (eg, eggs, baked beans), toast, milk, orange juice, and a hot beverage. Lunch and dinner includes a soup, a hot meal or sandwiches, three types of vegetables, bread, dessert or fruit, and a hot beverage. An analysis of the two-week default menu cycle at RGH was performed using the dietary analysis program Foodworks Version 4 (2005, Xyris Software, Qld, Australia). The default menu is a standardized 2 week cycle which is provided to patients who have been unable to self-select from the menu (eg, if a patient has not completed a menu due to being absent when menus are distributed).The average daily nutrient content of the menu (food and fluid items) was compared to current wound healing recommendations (CitationClark 2003; CitationPeninsula Health 2007) and estimated average requirements (EAR) (CitationNHMRC 2005). EAR was used as a suitable target as it is designed to meet the needs of at least 50% of the population (CitationNHMRC 2005).
Assessment of ordering practices and dietary intake
RGH utilizes the ‘Buckeye’ (Buckeye Food Management Solutions, Melbourne, Vic, Australia) food service system to manage the menu services for all inpatients. Participants typically receive and complete menus one day in advance to order their main meals. Following completion, the menus are scanned by a computer to produce tray tickets and ordering summaries. This enabled the researcher to determine the menu choices of the study participants and subsequently compare the groups ordering practices to average individual estimated energy requirements (CitationSchofield 1985), wound healing recommendations for protein (CitationClark 2003; CitationPeninsula Health 2007) and the recommended dietary intake (RDI) (CitationNHMRC 2005) for micronutrients.
The researcher conducted 24-h food recalls during each of the patient visits utilizing the data collected on ordered food items as a prompt to determine what proportion of meals were consumed. Food intake was evaluated using a 25% increasing consumption scale (ingestion of 0%, 25%, 50%, 75%, or 100% of the meal). Detailed information on all foods and beverages consumed beyond the menu were taken into account by interviewing the participants on food brought from outside (purchased or brought in by family/friends). Analysis of the 24-h recall was performed using Foodworks Version 4 (Xyris Software) to determine the nutrient intake of individual participants. Intake was compared to individual estimated energy requirements (CitationSchofield 1985), wound healing recommendations for protein (CitationClark 2003; CitationPeninsula Health 2007), and the RDI for micronutrients (CitationNHMRC 2005).
Total energy expenditure (TEE) was estimated using the Schofield equations (CitationSchofield 1985) with an activity factor of 1.2 as all participants were bed bound or of limited mobility. For participants who were not in the ‘desirable’ BMI range, the upper or lower end of the healthy weight range (whichever was closest to the participants’ BMI) was used to determine TEE. Protein requirements were calculated based on international recommendations of 1.0–1.5 g/kg body weight for patients with pressure ulcers (CitationClark 2003; CitationPeninsula Health 2007). Vitamin A, C, and zinc requirements were based on the RDI (CitationNHMRC 2005). At individual levels, RDI is recommended to assess the probability of adequacy (CitationNHMRC 2005).
Energy and nutrients ordered and consumed were compared to individual requirements and then expressed as a percentage of target requirements.
Statistical analysis
All data were analysed using the SPSS statistical package (SPSS for Windows Graduate Student Version 15.0.0 2006; SPSS Inc., Chicago, IL, USA). Data are reported as median (Interquartile range) or mean (95% confidence interval) and n (%). To determine if any differences existed between groups (eg, eligible versus noneligible), Mann-Whitney U test for nonparametric continuous data (eg, age) and chi-square test of association or Fisher’s exact test for categorical data (eg, type of wounds, accommodation, gender) were performed. Maximum likelihood mixed effects modeling was used to analyze changes in weight, FFM, FM, appetite, and nutrient intake over time. This model takes into consideration missing data and difference across three time points. Significance was considered at the level of p < 0.05.
Results
Recruitment
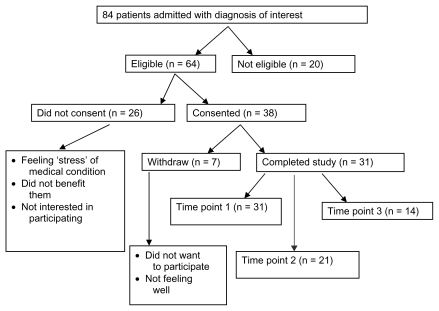
Recruitment of subjects is described in . Eighty-four patients were screened for eligibility with 38 providing written consent (59% of total eligible). Reasons for declining to participate included feeling stressed, not interested in participating and felt the study would not be of individual benefit. Fourteen participants completed the study (data available for all three time points). There was no significant difference in age, type of wounds, gender, or accommodation between those identified as eligible and those who were not eligible. Similarly, there was no significant difference between those identified as eligible who agreed or refused to consent. FM and FFM was not recorded for eight participants due to severe edema or due to both lower limbs being bandaged. Two participants did not have intake data at baseline as they were unwell or undergoing a procedure at the scheduled time of interview.
Baseline characteristics
presents the baseline characteristics of participants. Participants were mostly elderly with the majority being male. The majority lived independently in the community prior to admission. Median length of stay was 14 days (interquartile range, 6–23 days). The most common wounds were nonsurgical wounds and most common comorbidities were diabetes and cardiovascular conditions. In terms of nutritional health, the majority of the group were overweight or obese with a high percentage fat mass. According to the SNAQ questionnaire, 9 (31%) participants were at significant risk of losing at least 5% of their body weight within six months.
Table 1 Baseline characteristics of study participants (n = 31)
Menu quality
The menu was mostly found to be consistent with guidelines with the exception of energy, where the menu only provided 80%–93% of the recommendations. The menu provided sufficient zinc for female participants but not for males. In addition, protein was found to be borderline at risk ().
Table 2 Comparison between the menu provided at RGH with wound healing recommendations
Ordering practices and consumption of wound patients
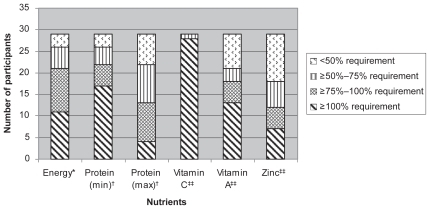
On average, ordering practices of wound patients demonstrated that at all three time-points, most estimated requirements would be able to be achieved expect for zinc. Ordering practices of wound patients provide an average of 8070 kJ (95% CI 7505, 8635), 97 g protein (95% CI 89, 104), 260 mg vitamin C (95% CI 236, 285), 1485 mg vitamin A (95% CI 1149, 1821) and 11 mg zinc (95% CI 9.8, 12.2) at baseline. The participants had a mean intake of 6566 kJ (95% CI 5907, 7325), 76 g protein (95% CI 66, 87), 196 mg vitamin C (95% CI 164, 227), 1082 mg vitamin A (95% CI 761, 1404) and 8.3 mg zinc (95% CI 6.8, 9.7). illustrates the number of participants able to meet varying proportions of estimated requirements for each nutrient of interest. At baseline, only 11/29 participants met their estimated total energy requirements and 17/29 participants met their minimum protein requirements. The majority of participants (28/29) met their vitamin C requirements, however the requirements for vitamin A and zinc were not as easily attained, with only 13/29 and 7/29 participants meeting the RDI, respectively.
Figure 2 Proportion of nutritional requirements met by wound patients who participated in the trial evaluating nutritional changes overtime at RGH (n = 31).
Supplements
Six (19%) participants were receiving oral nutrition supplements and additional snacks. At baseline, supplements provided 14%–31% and 20%–35% of individual energy and protein requirements, respectively. Using maximum likelihood mixed effects modeling, no significant change was found in the nutritional intake of patients over time for patients receiving supplements and/or snacks. Those consuming supplements achieved a higher intake of energy (p = 0.048), protein (p = 0.049), vitamin A (p < 0.001), and zinc (p = 0.002) compared to those on hospital meals only. However, no significant difference was observed in weight change between the supplemented and nonsupplemented groups over time.
Changes in nutrient intake
Data for the 14 participants that completed the study (all three time points) is displayed in . When nutrient intake was evaluated over time (), a nonsignificant trend for an improvement in energy and zinc intake was observed but this was not true for the other nutrients measured.
Table 3 Comparison of nutritional changes of patients who completed the trial in evaluating nutritional changes overtime in wound patients at RGH. Participants represent 14 unless otherwise stated. Values represent median (IQR) unless otherwise stated.
Changes in nutritional status
When looking at changes in nutritional status over time, there was a nonsignificant trend for weight loss, particularly FM in the patients (n = 14) that completed the study ().
Discussion
Findings from this study indicated that: (1) the default menu at RGH was able to provide sufficient nutrients with the exception of energy and zinc to meet wound healing recommendations, (2) wound patients were able to meet estimated requirements expect for zinc via the items they ordered from the menu, (3) wound patients were consuming insufficient quantities of nutrients important for wound healing, and (4) there is no statistically significant change in the nutritional status of patients with wounds during hospital admission, however there was a trend in the direction of decline.
While protein-energy malnutrition was not prevalent in our study participants, they do remain at risk of suboptimal nutritional health. With the exception of energy and zinc, the default menu at RGH is able provide sufficient nutrients to meet recommendations, however a considerable proportion were not consuming sufficient nutrients to meet estimated requirements. At baseline only 11 (38%) participants met their energy requirements via a combination of hospital meals, supplements, and items brought from outside of the hospital. While this was found to improve over time, even at time point 3, 7 participants (50%) still consumed less than their estimated requirements for energy. This finding is consistent with much of the literature. Low energy intake in wound patients has been reported by CitationRaffoul and colleagues (2006), where only 22% of patients were able to meet more than 90% of energy requirements via hospital meals only and 55% of patients met their energy requirements when their diet was supplemented with oral nutrition support. In a trial that evaluated the intake of patients with and without pressure ulcers, a lower energy intake was found in patients with pressure ulcers (CitationGreen et al 1999). A study that investigated meal patterns and meal quality in relation to nutritional status in patients with leg ulcers had similar findings (CitationWissing et al 2000).
Interestingly, and in keeping with findings suggesting patients with wounds do not meet energy requirements, the present study found a nonsignificant trend for weight loss of 1.4 kg (at d 10–11) for patients that completed the study. These findings were similar to the study conducted by CitationRaffoul and colleagues (2006) where weight loss of 1–4 kg occurred during hospital stay (median length of stay 9 days). There was also a nonsignificant trend observed for a reduction in FM. The results of our study were inconsistent with findings reported by CitationSchneider and colleagues (2002) that elderly are more likely to experience a larger proportion of FFM loss rather than FM loss when intake does not meet requirements.
While the majority of the participants in our study were in the overweight or obese category (median 28 kg/m2 (IQR 18.9–43.1 kg/m2), the weight loss observed is concerning as evidence suggests that the prognosis for patients who lose weight is poorer than those who maintain their weight, regardless of their baseline BMI status (CitationBannerman et al 2002). This is particularly the case in older adults where studies suggest that overweight elderly should maintain their weight to reduce the risk of impaired function and mobility (CitationBannerman et al 2002). More work is required in this area as despite increasing energy intake over time, a trend for weight loss was observed and questions are therefore justified about the accuracy of the determination of energy requirements in this patient group. For the present study, the Schofield equations with a 1.2 factor for physical activity were used. The appropriateness of these equations in obese individuals remains controversial (CitationThomas 2004) and no stress factor was applied despite evidence that patients with wounds undergo a period of catabolism which would warrant the application of a stress factor (CitationLong et al 1979; CitationWeekes 2007).
The ‘optimum’ dietary protein intake in wound and pressure ulcer patients is also controversial. Requirements for these patients are likely to be higher than normal adult recommendations of 0.8 g/kg (CitationThomas 2004). The literature in the area shows three studies (CitationChernoff et al 1990; CitationBreslow et al 1993; CitationLee et al 2006) that investigated protein supplementation (37–150 g) reported a positive effect on wound healing over a period of eight weeks. Based on a 70 kg man, this protein intake would range from 0.5–2.0 g/kg. In a clinical setting, the current recommendations for elderly stressed (burns, pressure ulcers, infections) patients range between 1.2–1.5 g/kg (CitationThomas 2004). National agencies have recommended a protein intake of 1.0–1.5 g/kg for patients with pressure ulcers to promote positive nitrogen balance (CitationClark 2003; CitationPeninsula Health 2007). Therefore in our study, the range of protein requirements (1.0–1.5 g/kg) used would cover the needs of the majority of wound and pressure ulcer patients. This may be the reason why patients did not lose lean body mass if their intake was adequate.
Zinc was the other nutrient of interest in this study. We found that the menu was unable to provide sufficient zinc to meet recommendations. This was highlighted particularly for the males where 22 of 23 male participants were unable to meet the RDI. With prolonged inadequate zinc intake, there is an increased risk of low serum zinc levels in these patients, which may delay wound healing and may warrant zinc supplementation. Studies in this area have reported inconsistent findings (CitationClayton 1972; CitationHallbook and Lanner 1972; CitationHaeger and Lanner 1974; CitationPhillips et al 1977). One possible reason for this inconsistency is the varied classifications used for defining normal serum zinc concentration (85–127.5 μg/100 ml). Although there is no strong evidence for zinc and wound healing, there is stronger evidence that supports recommendations for zinc supplementation for those whom are deficient (CitationPeninsula Health 2007; CitationThompson and Fuhrman 2005). True serum zinc deficiency is difficult to determine (CitationScholl and Langkamp-Henken 2001), low dose supplementation of 15–25 mg of elemental zinc might be advocated in clinical practice to prevent deficiency and/or for patients with nonhealing wounds (CitationPeninsula Health 2007).
Achievement of nutrient RDI’s for some participants (n = 6) was aided through the intake of oral nutritional supplements. The present study found a significant difference in the intake of all nutrients expect vitamin C between those taking oral nutrition supplements compared to those who were not. Similar findings were observed by CitationRaffoul and colleagues (2006). They found that energy from supplements provided more than 40% of energy requirements in the majority of the participants. In a review conducted by CitationStratton and colleagues (2005) oral nutrition supplements showed a trend of improving healing of pressure ulcers compared to routine nutritional care (without supplements). The study also concluded that although enteral nutritional support (ONS and enteral tube feeding) may improve healing of pressure ulcers, more research is needed in the area to confirm this finding. Findings from our study suggest that the intake of our patients was poor and therefore the use of oral supplements for this group of patients may be needed to maximize the nutritional intake of key nutrients for wound healing.
It is important to place the findings of the present study in context by acknowledging the strengths and limitations. Strengths of the study presented are numerous. To our knowledge, this is the first study conducted in Australia involving this patient group that investigates the changes in nutritional status over time and the nutrient intake and menu ordering practices of wound patients. The sample recruited was from a heterogeneous population group which increases the generalizability of the results and participants were recruited very early during admission. In addition, all measures were conducted by a single trained researcher hence minimizing the likelihood of measurement error. The use of the 24-h recall with prompts and printed menus minimized respondent burden and increased the validity of the recall. The study also incorporates the use of the new Nutrient Reference Values (NRV) for Australia and New Zealand. Furthermore, valid and reliable equipment was used in this study. Limitations of this study include the small sample size, the short duration of the study and the BIS technique. The small sample size may be responsible for the inability of this study to detect statistically significant differences. With increased study duration, more participants would have been able to be recruited thus providing a larger sample size and minimizing the risk of Type II error. A small number of patients (n = 2) declined interviews due to ‘feeling unwell’ or fatigue from procedures, therefore other methods of collecting intake data such as food charts may have been beneficial however this method relies on diligent and trained nursing staff. Patients who consented to participate but declined interviews and those who declined to participate in this study are likely to be at greater nutritional risk and hence the concerns uncovered in this study are likely to be greater in the true population. Although the BIS technique has been validated in the elderly population (CitationKyle et al 2001; CitationLupoli et al 2004), it may be affected by various factors especially hydration status, which causes variability of the FFM value (CitationBussolotto et al 1999; CitationKushner et al 1996), hence results of the present study need to be interpreted with caution, as there is no indicator of hydration status for the participants of this study.
Conclusion
This study has shown that it is neither the menu nor the choices made by the patients that influence the decline in nutritional status in this sample. Rather the patients were unable to consume sufficient quantities to meet requirements. The study also highlights that nutritional status may decline in patients with wounds throughout their hospital admission. Following discharge, the trend of weight loss may continue over time, increasing the risk of malnutrition. Therefore more education and encouragement is required to ensure patients consume sufficient quantities of energy and protein to preserve body weight in addition to nutrients known to improve wound healing. It is also important to recognize the need for nutritional intervention for this patient group (eg, dietitian referral, use of nutrient dense meals and oral supplements) to maximize nutritional intake of key nutrients. Routine serum nutrient levels may not be warranted at this stage, however, it is recommended that health-care professionals should consider clinical signs and serum levels to identify deficiencies. Further research measuring micronutrient levels of individuals would provide clearer recommendations in this area. Additional research with a larger sample size is needed to evaluate the trends observed in the changes of nutritional status further.
Acknowledgments
We wish to acknowledge the patients who volunteered to participate and their valuable contribution towards the study. We also acknowledge the assistance of all staff especially the nurses in the vascular wards of Repatriation General Hospital, South Australia and the Flinders University Statistician Kylie Lange for her statistical advice. JT, MM, PP designed and planned the study. LL conducted the recruitment and data collection. LL, JT, and MM analyzed and interpreted the data. LL, JT, MM, and PP critically appraised the manuscript. The authors report no conflicts of interest.
References
- ArnoldMBarbulA2006Nutrition and wound healingAm Soc Plas Surg1177S42S58S
- Australian Wound Management Association2001Clinical practice guidelines for the prediction and prevention of pressure ulcersWestern AustraliaAustralian Wound Management Association
- BannermanEMillerMDanielsL2002Anthropometric indices predict physical function and mobility in older Australians: the Australian Longitudinal Study of AgeingPublic Health Nutr56556212372159
- BreslowARHallfrischJGuyDG1993The importance of dietary protein in healing pressure ulcersJ Am Geriatr Soc41357628463519
- BussolottoMCecconASergiG1999Assessment of body composition in elderly: accuracy of bioelectrical impedance analysisGerontol453943
- ChernoffSMiltonKYLipschitzDA1990The effect of a high protein formula (Replete) on decubitus ulcer healing in long term tube fed institutionalised ptientsJ Am Diet Assoc90A130
- ChumleaWCGuoS1992Equations for predicting stature in white and black elderly individualsJ Gerontol47M1972031430854
- ClarkM2003Nutritional guidelines for pressure ulcer prevention and treatmentEuropean Pressure Ulcer Advisory Panel
- ClaytonR1972Double-blind trial of oral zinc sulphate in patients with leg ulcersBr J Clin Prac2636870
- DarzinsPKhalilZRimazR2000Evaluation of transcutaneous electrical nerve stimulation for the treatment of leg wounds in older people [online]Accessed October 24, 2007 URL: http://www.nari.unimelb.edu.au
- GreenSWinterbergHFranksP1999Nutritional intake in community patients with pressure ulcersJ Wound Care83253010776221
- HaegerKLannerE1974Oral zinc sulphate and ischaemic leg ulcersVasa377814460452
- HallbookTLannerE1972Serum-zinc and healing of venous leg ulcersLancet1478024116227
- HimesD1999Protein-calorie malnutrition and involuntary weight loss: The role of aggressive nutritional intervention in wound healingOstomy Wound Manage45465510347519
- KushnerRGudivakaRSchoellerD1996Clinical characteristics influencing bioelectrical impedance analysis measurementsAm J Clin Nur64423S7S
- KyleUBosaeusIDe LorenzoA2004Bioelectrical impedance analysis – part II: Utilization in clinical practiceClin Nutr2314305315556267
- KyleUGentonLKarsegardL2001Single prediction equation for bioelectrical impedance analysis in adults aged 20–94 yearsNutr1724853
- KyleUSchutzYDupertuisY2003Body composition interpretation: Contributions of the fat-free mass index and the body mass indexNutr19597604
- LeeKPosthauerMEDornerB2006Pressure ulcer healing with a concentrated, fortified, collagen protein hydrolysate supplement: A randomised controlled trialAdv Skin Wound Care19946
- LipskiP1996Australian nutrition screening initiativeAust J Aging151417
- LongCSchaffelNGeigerJ1979Metabolic response to injury and illness: estimation of energy and protein needs from indirect calorimetry and nitrogenJPEN J Parenter Enteral Nutr34526575168
- LupoliLSergiGCoinA2004Body Composition in underweight elderly subjects: reliability of bioelectrical impedance analysisClin Nutr2313718015556259
- [NHMRC] National Health and Medical Research Council2005Nutrient reference values for Australia and New Zealand: including recommended dietary intakesNational Health and Medical Research CouncilCanberra
- [NPUAP] National Pressure Ulcer Advisory Panel Board of DirectorsCuddiganJBerlowitzDRAyelloEA2001Pressure ulcers in America: Prevalence, incidence, and implications for the future. An executive summary of the National Pressure Ulcer Advisory Panel MonographAdv Skin Wound Care1420815
- OsterkampL1995Current perspective on assessment of human body proportions of relevance to amputeesJ Am Diet Assoc95215177852688
- Peninsula Health2007Nutrition Guidelines for Wounds and Pressures Ulcers for DietitiansFrankston, VicNutrition and Dietetics Department, Peninsula Health
- PhillipsADavidsonMGreavesM1977Venous leg ulceration: evaluation of zinc treatment, serum zinc and rate of healingClin Exp Dermatol23959342149
- Queensland Government, QH2004Pressure Ulcers Prevention and Management Resource Guidelines, QueenslandBrisbane, QldQueensland Government
- RaffoulWShahinMCayeuxM2006Nutritional status and food intake in nine patients with chronic low-limb ulcers and pressure ulcers: importance of oral supplementsNutr22828
- SchneiderSAl-JaouniRPivotX2002Lack of adaptation to severe malnutrition in elderly patientsClin Nutr2149950412468370
- SchofieldWN1985Predicting basal metabolic rate, new standards and review of previous workHum Nutr Clin Nutr395414044297
- SchollDLangkamp-HenkenB2001Nutrient recommendations for wound healingJ Intraven Nurs241243211836837
- StausbergJKrogerKMaierI2005Interdisciplinary Decubitus Project. Pressure ulcers in secondary care: incidence, prevalence, and relevanceAdv Skin Wound Care18140515840982
- StrattonRJEkACEngferM2005Enteral nutritional support in prevention and treatment of pressure ulcers: A systematic review and meta-analysisAgeing Res Rev44225016081325
- ThomasD2004The relationship of nutrition and pressure ulcersHandbook of Clinical Nutrition and AgingTotowa, NJHumana Press
- ThompsonCFuhrmanM2005Nutrients and wound healing: still searching for the magic bulletNutr Clin Prac2033147
- WeekesEC2007Controversies in the determination of energy requirementsProc Nutr Soc66 3677717637089
- WilliamsJBarbulA2003Nutrition and wound healingSurg Clin Nth Am8357196
- WilsonMThomasDRubensteinL2005Appetite assessment: simple appetite questionnaire predicts weight loss in community-dwelling adults and nursing home residentsAm J Clin Nutr8210748116280441
- WissingULennernasMUnossonM2000Meal patterns and meal quality in patients with leg ulcersJ Hum Nutr Dietet13312
- [WHO] World Health Organisation1998Obesity, Preventing and Managing the Global EpidemicGenevaWorld Health Organisation