Abstract
Objectives:
To develop and test the effectiveness of an Internet-based self management program by multidisciplinary health care professionals for patients with heart failure (HF).
Methods:
The comprehensive educational material for HF was created and posted on a website. A computer with Internet connection and computer training were provided first. A secure and simple web-based recording system of vital signs and health behaviors and a mechanism for feedback regarding each participant’s record were developed. A randomized controlled trial with a one-year intervention was conducted using a total of 40 patients who were assessed three times in their homes. An intention-to-treat analysis used multivariate statistics.
Results:
The treatment group had a high (85%) adherence to the intervention. Only the treatment group showed a significant improvement in the knowledge level (p < 0.001), amount of exercise (p = 0.001), and quality of life (p = 0.001), and reduction in HF related symptoms (dyspnea, p = 0.001; fatigue, p = 0.003; functional emotion, p < 0.001), blood pressure (systolic, p = 0.002; diastolic, p < 0.001), frequency of emergency room visit, and length of hospital stay (both p = 0.001).
Conclusions:
An effective program to change one’s behaviors in managing HF takes a multidisciplinary approach to create and provide feedback regarding a patient’s daily record, which can be accomplished through Internet use.
Introduction
Heart failure (HF), or congestive heart failure, is a debilitating illness affecting about five million Americans, with 550,000 new cases diagnosed each year.Citation1 Approximately 79% of adults with HF are over 65 years of age, with a 30%–40% annual hospitalization rate.Citation2 This is the most expensive illness among the population 65 years and over due to recurring emergency room visits and hospitalizations. In 2005, in the US alone, HF-related costs rose to $27.9 billion, a $4.7 billion increase in three years.Citation3 This rise is likely to continue due to the rapid growth in the aging population along with a longer life expectancy. HF is a final common pathway of various illnesses and conditions and is usually chronic without a cure. HF, therefore, is a condition that greatly impacts the individual and society as a whole.
One strategy for slowing decline with chronic HF is to improve daily healthy behaviors including reducing and monitoring salt and fat intake, smoking, and alcohol consumption, committing to regular exercise,Citation1 medication adherence, and maintaining a positive attitude. This strategy takes a multidisciplinary approach to develop and individualize. Although effective, the obstacles for this intervention have been identified: the high cost and the large amount of effortCitation4 for providers as well as patients.
In order to overcome these limitations, Internet use has been suggested as a means to change daily health behaviorCitation4 by empowering a large number of patients to take more control of their health.Citation5 An early study with HF patients compared the efficacy of an interactive voice response system and interactive web-based technologies (e-health group) to change health behavior.Citation6 After one year of intervention, exercise and general activities were similar for both groups, but the e-health group had lower health care costs. A study using a meta-analysis concluded that Internet-based health interventions can improve behavioral outcomes such as increased exercise time, knowledge of nutritional status, knowledge of asthma treatment, body shape perception, and was also effective in weight loss maintenance.Citation7
Although Internet access is less common among older adults than younger adults, once they use, their use pattern is similar to that of younger adults.Citation8,Citation9 As rapid growth of Internet use among older adults advances, theoretically, so do both the opportunity and the tools to improve health practices and improve health outcomes while reducing health costs.
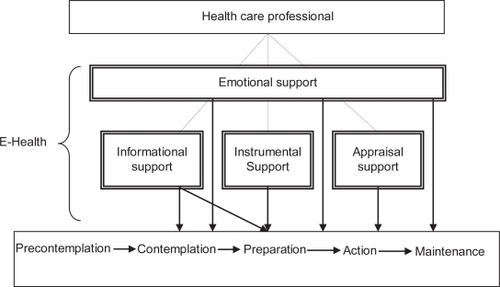
A conceptual framework, Model Toward Optimal Independence through Technological Adoption (M-TOMITA) was formed for this study based on the Trans-theoretical Model (TTM),Citation10 social support theory,Citation11 and a mass communication theory called Uses and Gratifications.Citation12 The M-TOMITA works best when individuals are already aware of their chronic conditions and are contemplating doing something to manage their illness but are not sure what to do (the contemplation stage). If someone has little knowledge of their illness and is not aware that changing health behavior may help them, this model may not be effective. The model is an empowerment process that progresses through stages from contemplation, preparation, and action, to maintenance. Using the Internet method, four types of support by health care professionals can be provided. Informational support or education of chronic illness and suggested health behaviors is especially important in the initial stage but should continue all the stages. Among the recommended health behaviors, patients will choose an activity to focus on. Once the first activity is successfully implemented, additional activities will be added, one by one. After the decision regarding a particular health behavior is made, Instrumental support should be provided via the Internet. Through the online record-keeping system the participant can track their own vital signs and health behaviors so that they can become aware of a cause (life style) and effect (symptom and general health) relationship. The website also provides participants and nurse monitors the record with alerts for critical measures so that health care providers can be notified. This record is shared with their health care providers at office or home visits for the purpose of monitoring as well as appraisal support to reinforce patient motivation. Internet use, especially in the initial stage, boosts older adults’ self-esteem. They realize their ability to learn something new and feel they are up to date with their children and their grandchildren. The Internet is so versatile; it provides not only opportunities for education, but also for frequent communication with families and friends, leisure through playing games to stimulate and challenge the mind, and can improve instrumental activity of daily living (IADL) by participating in online shopping on drugs, books, and even groceries. Mastering Internet technology, therefore, improves the quality of life of older adults. Throughout this process, emotional support from health care professionals is important to keep the participants motivated until the time that their illness prevents them from using the computer. Its application to Internet use is described in the intervention section of this study, and is illustrated in .
The objectives of this study were to develop and test an e-health intervention using a multidisciplinary approach to improve health behavior and outcomes among older adults with HF. Hypotheses in this study are that the treatment group will: (1) adhere to the intervention program at a high rate (>75%)Citation13; (2) improve in knowledge of HF and related healthy behaviors; (3) reduce specific HF symptoms and sick days, and improve blood pressure (BP), (4) improve in perceived quality of life; and (5) reduce frequency of emergency room visits and length of hospital stays. Participants’ subjective evaluation of the program was also sought. It included satisfaction/dissatisfaction, reasons for the rating, benefit, improved or not improved HF, the most liked/disliked part of the method, and suggestions for the program.
Methods
Study design
The study employed a randomized controlled design with a one-year intervention. Three assessments (baseline, and follow-ups at six and 12 months) were conducted in participants’ homes. The control group received usual care. Usual care for home-based patients in the US is a three-month regular check up with their physicians. If they are hospitalized, they may have nurse visits, physical or occupational therapists’ home care, and phone calls from their insurance company to report their weight and blood pressure for three months. None of the partisans were receiving nurse visits due to hospitalization. The treatment group received the e-health intervention in addition to usual care, and process measures were collected daily.
Subjects
Individuals with HF were recruited from three hospitals and two health insurance companies in Western New York using a convenience sampling method. Inclusion criteria were those who: (1) were living at home and 60 years of age or older; (2) had at least one emergency room visit or overnight hospital admission due to HF in the past year; and (3) met the New York Heart Association (NYHA) Classification of Heart Failure for Class II (Slight limitation of activity or dyspnea and fatigue with moderate physical activity) or Class III (Marked limitations of activity or dyspnea with minimal activity).Citation14 Exclusion criteria were individuals who: (1) were scheduled for any kind of heart surgery and/or (2) had cognitive impairment (Mini Mental State Exam [MMSE] < 24).Citation15
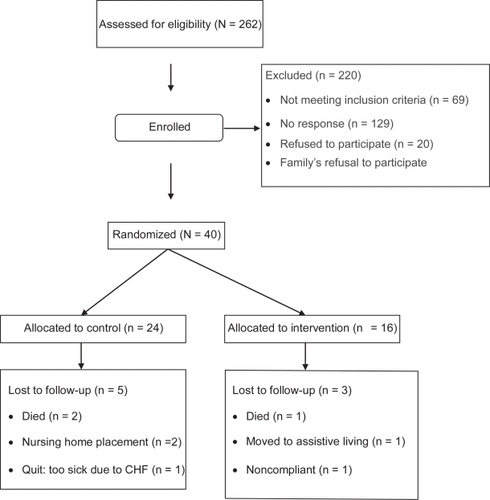
The sample size, determined by a power analysis to achieve 80% of power at α1 = 0.05 with a large effect size (d = 0.90)Citation16 was 15 in each group. Considering a high attrition rate anticipated for the control group, 24 in the control group and 16 in the treatment group were recruited. The sample size flow-chart is included in .
Intervention
Technology
Participants in the treatment group were provided a standard PC with Internet access as well as basic computer training. Publicly accessible and secured websites were created by a multidisciplinary health care team of a health behaviorist, a geriatric physician, a geriatric nurse, an occupational therapist, a physical therapist, and an exercise physiologist. We used the web creation guidelines published by the National Institute on Aging and the National Library of Medicine.Citation17 Four types of support (informational, instrumental, appraisal, and emotional) at suitable stages of behavioral changes were provided in this e-health intervention.
Informational support included online information on: HF, drugs used to treat HF, effects of alcohol and smoking, depression, prescribed home exercise, nutrition, weight management, and exercise in general using the Flesch–Kincaid Reading Grade level of eight on average. An exercise instruction program (walking, breathing, stretching, range of motion, upper and lower extremity strength training, and stationary biking) was developed and delivered via streaming video. This support was provided in the beginning of the intervention period.
Instrumental support included availability of a secure, simple, and short online recording system using Lotus Notes Web Server 6.5. This support was provided after participants became comfortable with the use of a computer and Internet. Participants were asked to access the website daily to record their vital signs and health behaviors. The site asks questions about blood pressure, pulse, weight, medication use, type and amount of exercise, levels of fatigue, intake of salt, sugar, alcohol, and tobacco, health changes, and HF-specific questions regarding swelling, fatigue, and dyspnea. Additionally, a webpage containing their past records with an automatic alerting function for sudden weight gain was available. Any overnight gain of 3 lbs or more resulted in a red dot display in the record that signaled participants to contact their physician.
Appraisal support was provided via email every month from appropriate health care professionals in dealing with subjects for the purpose of feedback for patients’ records. This support was provided to encourage participant’s ongoing actions for changing their health behaviors toward a maintenance stage (beyond six months).
Emotional support was provided on an as needed basis via email. Since no participants were depressed (>15 Center of Epidemiological Study- DiseaseCitation18) at the time of initial assessment, an online discussion group was not formed.
Dependent variables
A knowledge questionnaire was developed for this study consisting of 20 questions with a possible total score ranging from 0 to 60 (all correct responses). Frequency of exercise was captured on a nominal scale (every day, 2–3 times/week, less than once/week, rarely and none) for breathing exercise, stretching, walking, and mild exercise including stationary biking, swimming, and golfing.
HF-specific symptoms (dyspnea during daily activities, fatigue, and emotional function) were measured using the Congestive Heart Failure Questionnaire (CHFQ).Citation19 Higher scores are indicators of better conditions. The psychometric of CHFQ has been tested. It has good reproducibility for the total score and the three subcategories and responsiveness for change.Citation20 The responsiveness was found to be similar to the Minnesota Living with Heart FailureCitation21 and better then SF 12.Citation22,Citation23
Perceived quality of life (QOL) was assessed using a 50-item age relevant questionnaire on diet, health care, safety, social, communication, psychological health, activities, and perceived aging, with a higher score indicating a higher level of wellness.
Statistical methods
An intention-to-treat analysis was conducted using mostly a multivariate linear model. To explain the observed variability in the data and test for differences within and between groups, the model was fit to numeric endpoints via restricted maximum likelihood methods, adjusting to the difference for the severity of illness. To analyze health care use, actual data of those whose data were available at follow-up 2, due to nonnormal distributions, Friedman’s Tests for correlated samples were used. A significance level of 0.05 was set for each hypothesis test. SAS version 9.1.3 statistics software (SAS Inc., Cary, NC) was used for all analyses.
Results
Demographic and health information at baseline for 40 participants is summarized in . The two groups were equivalent for all characteristics. An overall mean age was 76.2 years, 32.5% were males, 2.5% were Asian, 12.5% were African American/Black, and 85.0% were Caucasian. Fifty-eight percent had 12 years of education or less, 36.7% had between 13 and 16 years, and 5.4% had 17 years or more. Mean MMSE score was 29 of 30. The mean number of comorbidity was 10 and medication taken was 8. The control group was comprised of 79.2% of patients with NYNA Level II and 20.8% of Level III while the treatment group had 75% and 25%, respectively. Although statistically not significant, this difference was adjusted in the multivariate linear approach. The control group had 5.1 years of HF while the treatment group, 3.6 years.
Table 1 Baseline demographic and health characteristics (N = 40)
Adherence to the program (Hypothesis 1)
All participants in the treatment group visited the publicly available website with a mean frequency of 3.5 times a month and recorded daily vital signs and health activities a mean of 85% of the days in one year which is considered high.
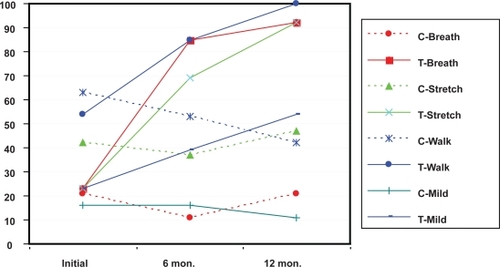
The number of exercisers was analyzed using a nominal binary scale: exercisers (exercising 2–3 times/week or more) and nonexercisers (exercising 1 time/week or less). The change in percentage of exercisers for three time points for various exercises is summarized in . For any exercises, there were no significant changes for the control group during the study while the treatment group showed significant increases in all exercises after one year. At 12 months the percentage of exercisers increased to 92% for both breathing and stretching, 54% for mild exercise, and 100% for walking. At 12 months, significant differences were found between the two groups for all exercises.
Knowledge of HF and related health behaviors (Hypothesis 2)
At baseline, the control group had higher knowledge scores than the treatment group, but at six months, the treatment group increased their knowledge level surpassing the control group, and maintained the trend at 12 months. At both six and 12 months, the treatment group was significantly higher than the control group (both p < 0.05). Descriptive statistics, change scores, and p-values for within-group change and between group differences for Hypotheses 2 through 5 are presented in .
Table 2 Change over one year in heart failure-related symptoms, blood pressure, and weight
HF-specific symptoms and general health indicators (Hypothesis 3)
For dyspnea, the control group, which initially scored better (23.5) than the treatment group (18.5) worsened gradually. The treatment group showed improvement with significance at six and 12 months (both p = 0.001). For fatigue, the control group showed significantly lower levels of fatigue at six months, then showed a significant increase at 12 months (p = 0.011). The treatment group recorded greater fatigue at six months but felt less tired at 12 months as compared to the baseline (p = 0.002). These changes were both significant.
For emotional function, the control group showed significant gradual decrease over one year (p = 0.001), while the treatment group exhibited significant gradual improvement (p < 0.001).
Elevated BP was observed in both groups during the year. The control group’s systolic BP decreased significantly initially, but rebounded to significantly higher levels at 12 months relative to baseline readings (p = 0.003). While initially much higher than the control group, the treatment group’s systolic BP significantly decreased by six months and remained lower at 12 months (p = 0.010). Regarding diastolic BP, both groups decreased significantly.
For the treatment group, the number of people who were sick less than one week in the past six months was significantly increased at six months and 12 months.
QOL (Hypothesis 4)
Although both groups increased the QOL scores significantly for the first six months and maintained for another six months, the treatment group had greater gains at both follow-ups, resulting in significant between groups differences (p < 0.05).
Health care utilization (Hypothesis 5)
For the control group, health care use did not change. For the treatment group, the number of visits to an emergency room and the length of hospital stay decreased significantly at six months; this was maintained at 12 months.
Table 3 Health care utilization
Participants’ evaluation of the e-health program
At the end of the study period, 100% of the treatment group reported that they were confident in dealing with HF due to the e-health program and said that they would recommend the program to other people who have similar conditions. Furthermore, 84.6% said that they were very satisfied with the system, 15.4% were satisfied, and 92.3% thought that their HF was better than one year before. The most often cited reason for satisfaction was “Monitoring myself for increased awareness.” The second and third reasons were “Better health” and “Support from health care providers.” Two participants reported that the most disliked part of the program was “Feel guilty when I have to record that I did not exercise, so I had to do exercise.” Two suggestions were “Expand the program to diabetes” and “Create a way to find out how other study participants are doing, so that I know my relative status.”
Discussion
This randomized controlled study tested a e-health method of self-management of HF for one year in home-based older adults. Four types of support were delivered via Internet by a team of multidisciplinary health care professionals. Although this e-health method may not be effective for all HF patients, it was beneficial for HF patients with NYHA Class II or III with respect to increasing knowledge of HF and related health behaviors, exercise time, emotional function, and quality of life, and reducing levels of dyspnea, fatigue, blood pressure, and sick days. The result of exercise was parallel to the finding of the meta analysis by Wantland and colleagues.Citation7 It was also effective in decreasing the number of emergency room visits and length of hospital stays. Limitation of the study was that it did not calculate cost effectiveness of the e-health method, which is necessary for its practical application. Also many between-group comparisons were not statistically significant mainly due to the small sample size. On the other hand, with this small sample size, most of within-group comparisons were significant, which is a strong indicator that the intervention was effective. With a larger sample size, it is expected that many between-group comparisons would be statistically significant. Vigorous studies with geographical and ethnical diversity are also needed in the future. Nevertheless, this study provided evidence that the effective e-health method in changing health behaviors and improving health outcomes takes an interdisciplinary approach since changing one’s health behaviors covers various health care disciplines.
Major e-health strategies that lead to successful health behavior change identified in this study are that: (1) relevant information should be provided using easy-to-understand language in an easy-to-see format; (2) a simple recording system for vital signs and health behaviors should be available to allow patients to be aware of their behaviors; (3) patients should be aware that their health activities are monitored by a health professional; and (4) feedback should be provided for continued health behavior change. The strategy was supported by a conceptual framework, M-TOMITA, which applied a concept of human social support to the Internet use by strategically placing the types of support in the stages of health behavioral change. In this model, a multi disciplinary team is necessary at the initial stage but once the program is in place, a nurse may be able to run the program with input from the team for appraisal. In this study we convened a regular distance team meeting every month for appraisal support, but this frequency should be further investigated for its validity. For a comprehensive self-management program, it is strongly recommended to include a pharmacist to check interactions of multiple medication intake and a nutritionist for better diet.
In this study, emotional support was not independent of appraisal and instrumental support, but was not provided in a specific manner, such as forming a discussion/chat group. For patients who are not depressed or believe that they have control over their illness, the level of emotional support provided in this study may be sufficient. However, especially for patients who are depressed, the Internet-based method has been utilized and its effectiveness has been reported.Citation24,Citation25 Subjective evaluation of this program found that some participants wished to know their health behaviors in relation to other participants’. Providing an average of aggregated data of all study participants can be easily done via the Internet. TTM describes a process of behavioral change called social liberalization as the person’s realization of changes of social norms. E-health may be able to create a social norm among study participants and allow them to see how it is changing.
Finally, evidenced by a very high adherence to the program, 85% of 355 days (Internet was not available for 10 days), an e-health approach utilizing a multidisciplinary health care team can be accepted as a tool for self-management of HF and other chronic diseases in the near future when technology is more advanced, computer costs are reduced, and older adults become more computer literate.
Disclosure
This study was funded by the National Institute on Aging, USA.
Reference
- American Heart AssociationHeart Failure. Heart and stroke Statistical Update [updated 2007] Cited on Oct 31, 2008. Available from: http://www.americanheart.org/presenter.jhtml?identifier=1486.
- Centers for Education and Research on TherapeuticsBetter Treatment for Heart Failure [updated 2003] Cited on Oct 31, 2008. Available from: http://www.certs.hhs.gov/about_certs/annual_reports/year2/centers/duke.html.
- The Joint CommissionThe Joint Commission’s Annual Report on QualityHeart Failure. Improving American’s Hospitals [updated 2007] Cited on Oct 31, 2008. Available from: http://www.jointcommissionreport.org/conditions/heartfilure.aspx.
- GlasgowREEmmonsKMHow can we increase translation of research to practice? Types of evidence neededAnnu Rev Public Health20072841343317150029
- eHealth InstituteeHealth Institute Mission [updated 2004]. Cited on Oct 31, 2008. Available from: http://www.ehealthinstitute.org?Index.aspx.
- RuggerioCMinassianPBarrEDisease management and e-health can be successfully mergedProceedings of the 2000 Healthcare Information and Management System Society2000219
- WantlandDJPortilloCJHolzemerWLThe effectiveness of web-based vs non-web-based interventions: A meta-analysis of behavioral change outcomesJ Med Internet Res20046e4015631964
- FoxSOlder Americans and the Internet2004 Cited on Oct 31, 2008. Available from: http://www.pewinternet.org/PPF/r/117/report_display.asp.
- BeckerSAWeb accessibility for older adults2003 Cited on Oct 31, 2008. Available from: http://cob.fit.edu/facultysites/abecker/Accessibility/OlderAdutlsStats/OlderAdultsSats.html.
- ProchaskaJOReddingCAEversKEThe trenstehrotical model and stages of changeGlanzKRimerBLewisFMHealth Behavior and Health Education3rd edSan Francisco, CAJossey-Bass2002
- HouseJSKahnRMeasures and concepts of social supportCohenSSymeSSocial Support and HealthOrlando, FLAcademic Press198583108
- RossiEUses and gratifications/dependency theory2002 Cited on Oct 31, 2008. Available from: http://zimmer.csufresno.edu/~johnca/spch100/7-4-uses.htm.
- CastroCMKingACTelephone-assisted counselling for physical activityExerc Sport Sci Rev200230646811991539
- Heart Failure Society of AmericaThe strategy of heart failure [updated 2006 Sept 26] Cited on Oct 31, 2008. Available from: http://www.abouthf.org/questions_stages.htm.
- FolsteinMFolsteinSEMcHughPRMini-mental state: a practical method for grading the cognitive state of patients for the clinicianJ Psychiatr Res1988121891981202204
- StewartSMarleyJEHorowitzJDEffects of a multidisciplinary, home-based intervention on unplanned readmissions and survival among patients with chronic congestive heart failure: a randomised controlled studyJ Lancet1999 25;35410771083
- The National Institute on Aging and the National Library of MedicineMaking your site senior-friendly2002 Cited on Oct 31, 2008. Available from: http://www.nlm.nih.gov/pubs/checklist.pdf.
- RadloffLSThe CES-D scale: A self report depression scale for research in the general populationAppl Psycholl Measure19771385401
- GuyattGHNogradiSHalcrowSDevelopment and testing of a new measure of health status for clinical trials in heart failureJ Gen Intern Med198941011072709167
- O’KeeffeSLyeMDonnellanCReproducibility and responsiveness of quality of life assessment and six minute walk test in elderly heart failure patientsHeart1998803773829875117
- RectorTSCohnJNAssessment of patient outcome with the Minnesota Living with Heart failure Questionnaire: Reliability and validity during a randomized, double-blind, placebo-controlled trial of pimobendanAm Heart J1992124101710251529875
- WareJEJrKosinskiMKellerSDA 12-Item Short-Form Health Survey: Construction of scales and preliminary tests of reliability and validityMed Care1996342202338628042
- BennettSJOldridgeNBEckertGJComparison of quality of life measures in heart failureNurs Res20035220721612867777
- GerhardAInternet-based self-help for depression: randomised controlled trialBr J Psychiatry200518745646116260822
- ChristensenHGriffithsKMJormAFDelivering interventions for depression by using the internet: randomised controlled trialBMJ200432826514742346