Abstract
The results of surgical treatment of epileptic seizures have gradually improved in the past decade, approaching 60% to 90% seizure-free outcome in temporal lobe epilepsy and 45% to 66% in extratemporal lobe epilepsy. Unfortunately some patients continue with seizures after epilepsy surgery and the studies have shown that approximately the 3% to 15% of patients with a previous failed surgical procedure are reoperated. Selected patients may be candidates for further surgery, potentially leading to a significant decrease in the frequency and severity of seizures. In patients with intractable partial epilepsy there are many possible factors, alone or in combination, that could be related to the failure of resection. Some of the factors could be genetic or acquired predisposition to epileptogenicity. In this article we report a case with intractable epilepsy that required three interventions to render seizure free. We analyzed our specific case in the light of previous reports on reoperation and enumerate the potential reasons for reoperation that could apply to all patients with failure of an initial procedure.
Background
The results of surgical treatment of epileptic seizures have improved in the past two decades, approaching 60% to 90% seizure-free outcome in patients with temporal lobe epilepsy and 40% to 60% in extratemporal lobe epilepsy.Citation1 However, there are few alternative treatment options to patients who fail epilepsy surgery such as reoperation, use of electrical stimulation and new medications. Reoperation for recurrent temporal epilepsy was first reported in 1954 by Penfield. Selected patients may be candidates for reoperation, potentially leading to a significant decrease in seizure burden. The frequency of reoperation reported in the literature is variable, ranging from 3% to 14%.Citation2–Citation4
The success after a second surgical procedure is variable and different studies have reported different seizure-free rates. Awad et al reported that 47% of patients were seizure free after a second procedure,Citation2 Germano et al 63%,Citation5 Gonzalez-Martinez 38%,Citation6 and Salanova 57%.Citation7
With recent advances in neuroimaging and more frequent use of noninvasive video-electroencephalography (VEEG) monitoring, a more comprehensive and accurate evaluation of the epileptogenic zone should be accomplished before the first epilepsy surgery. In patients with intractable partial epilepsy there are many possible factors, alone or in combination, that could be related to the failure of resection. Some of the factors could be related to acquired and genetic predisposition to continuous seizures.
Specific case to consider
We present a 27-year-old, right-handed male with no previous history of febrile seizures, head trauma, central nervous system infections or family history of seizures.
Since the age of 5, the patient had complex partial seizures with and without secondary generalization plus occasional grand mal seizures. The seizures were not preceded by an aura and the patient had oral and bimanual automatisms, bipedal automatisms and loss of awareness during the seizures with no postictal confusion. This patient had a high frequency of seizures (10–15 seizures per day) since his epilepsy began. Over the years he failed to the following medications: topiramate, carbamazepine, levetiracetam and valproic acid.
This patient had the first investigation for epilepsy surgery when he was 17 years old. Before surgery he was taking the combination of valproic acid and carbamazepine with adequate doses, and adequate therapeutic levels with no response. In pre-operative investigation, scalp EEG showed his seizures originated over the right frontal area. The patient had intracranial recording with electrodes covering the orbito-frontal area, the frontal convexity and the fronto-polar area, which supported the previous localization.
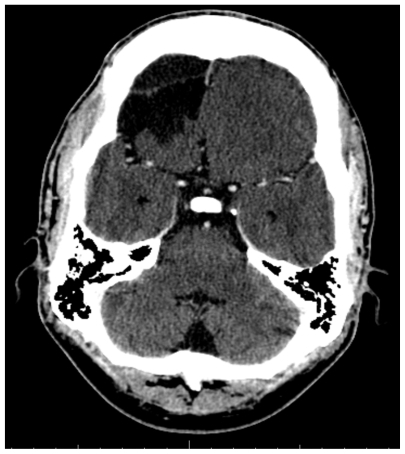
The patient had a small resection of the fronto-polar area (). He was rendered seizure free for 6 months and the medications were stopped. Pathology was consistent with cortical dysplasia.
Figure 1 Axial CT scan showing the first resection in this patient over the superior aspect of the right frontal convexity.

At the end of the first year after surgery the patient’s seizures restarted with the same frequency as before the intervention. The patient was retreated with the same medications used before surgery with no response and in the following years he failed to levetiracetam and topiramate. Also the patient was implanted with a vagal nerve stimulator when he was 20 years old, with no response.
The patient had a second investigation when he was 22 years old. The scalp EEG pointed to the seizure onset being over the right frontal area. Two ictal single photon emission computed tomography (SPECT) scans were taken showing an onset over the right orbito-frontal area. A decision was made to perform a right orbito-frontal resection without the necessity of intracranial recording (). The pathology was consistent with cortical dysplasia. The resection was performed and the patient rendered seizure free for 6 months and then the medications were stopped.
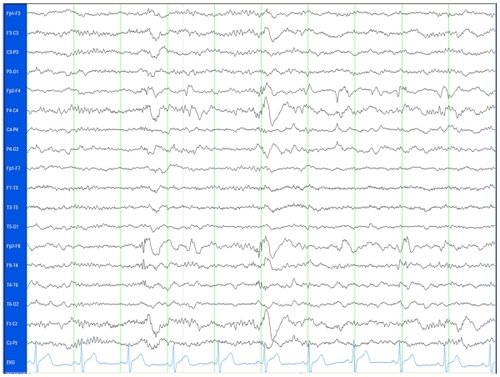
At the end of the first year after surgery, patient’s seizures restarted with the same frequency as prior to surgery. Before the second procedure patient was on the combination of topiramate and levetiracetam. These medications were restarted after the surgery with no success. Over the years more medications were added due to the high frequency of seizures and before being assessed in our center he was on a combination of 4 medications, clobazam 10 mg twice daily, lamotrigine 250 mg twice daily, phenytoin 400 mg per day, and oxcarbazepine 600 mg twice daily. A telemetry investigation was done recording 40 seizures with a potential onset over the right frontal vs temporal area (see ), with very rapid secondary generalization.
Figure 3A The onset of one of the seizures recorded with the scalp EEG. The EEG trace shows a simultaneous onset in the right temporal and frontal regions, involving the electrodes F4, Fp2, F8, T4 and some spread to T6.
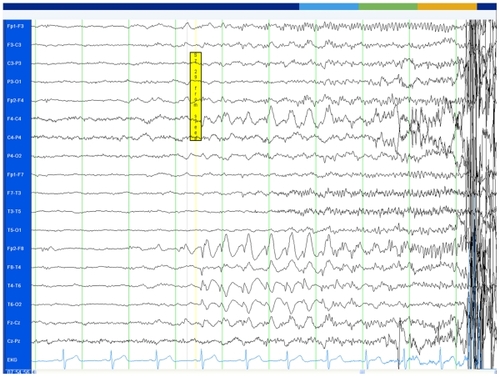
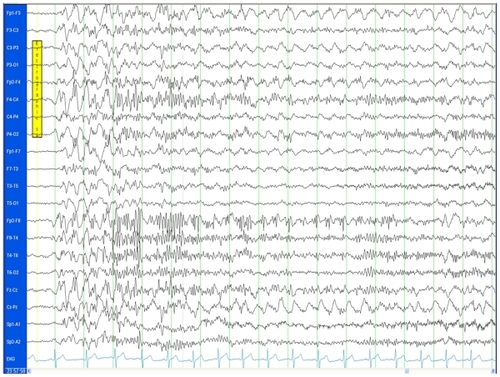
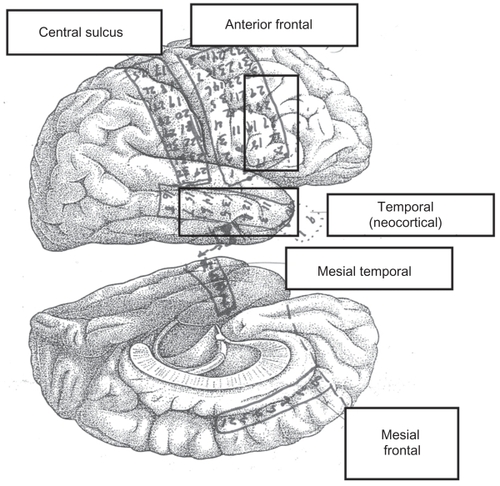
Interictally, the EEG also showed independent right frontal and temporal spikes () and during sleep the EEG showed a generalized polyspike wave (). An intracranial investigation was performed in this patient covering the remaining areas of the right frontal lobe and the temporal area (). The seizures have a simultaneous onset over the right frontal convexity and the neocortical aspect of the temporal area ().
Figure 3D The placement of electrodes in this patient. The seizure onset for the 40 seizures is displayed in the two boxes, corresponding to the right frontal convexity and the neocortical aspect of the temporal area.
A right frontal resection was performed sparing the motor strip and a standard temporal lobectomy was also performed. The patient had some postoperative seizures in the first 2 days characterized by jerks in the face and arm. These disappeared after 1 week and were attributed to inflammation related with the intracranial procedure. These seizures were treated with valproic acid IV, a daily dose of 20 mg per kg for 7 days. The patient did not have any modification in the anti-epileptic drugs and was rendered seizure free after 1 week.
The patient remained seizure free for 2 years with no modifications in the medications. No cognitive testing was done before surgery because of the high frequency of seizures and no significant cognitive decline was seen after surgery. The patient was able to get a driver licence after 1 year and started working as a clerk.
Discussion
This patient had 3 surgical interventions before he became seizure free. This is a very illustrative case of refractory epilepsy and shows many aspects common to all patients requiring reoperation after epilepsy surgery.
Potential reasons for surgery failure are as follows:
Extent of the first resection. Some centers have reported that the extent of the resection is an important factor for seizure recurrence. Holmes et al described 21 patients who had previous epilepsy surgery with recurrence of seizures, most of whom required extension of previous resections.Citation8 Currently the tendency in all epilepsy centers is to perform more selective resections or less aggressive procedures in order to spare other mental functions in patients. This patient finished with a very aggressive resection in order to control the seizures without a significant cognitive decline, supporting the possibility to perform aggressive procedures in selected patients.
Incorrect mapping or erroneous identification of the epileptogenic area. The second aspect that could be discussed in this patient is the possibility that the epileptogenic area was not correctly mapped in the first intracranial investigation. One of the disadvantages of intracranial recording includes limited cortical sampling with consequent sampling error.Citation9 This aspect is important in our case because the first investigation only covered the frontal area. The third investigation was more extensive, also covering the temporal area that showed a simultaneous onset with the frontal area.
Normal MRI before surgery. In his series of reoperations, Hennessy et al pointed out that some patients with reoperations had initial normal MRI and then in a second evaluation some abnormalities were identified.Citation10 The non-lesional status is a well recognized factor that predisposes to recurrence of seizures after epilepsy surgery.Citation11 Our patient had several MRIs over the years with no findings. This fact was probably an independent risk factor for reoperation.
Interpretation of test. Another aspect in this patient is the ictal SPECT. This case showed that decisions based only on one test such as the SPECT probably are not adequate. Currently the evidence does not support the use of PET and SPECT in isolation to make surgical decisions. It has been shown that ictal SPECT is most useful in patients with extratemporal focal epilepsy to guide the placement of intracranial electrodes at the possible ictal onset zones.Citation12,Citation13 The PET scan is more of a lateralizing value, especially in temporal lobe epilepsy compared to extratemporal epilepsy.Citation14
Pathological diagnosis. The pathological diagnosis in this patient was consistent with cortical dysplasia. This is an important consideration because it could explain in part the reoperations. Gonzalez-Martinez reported 57 patients who had temporal and extratemporal resections, and showed that patients with confirmed cortical dysplasia or mesial temporal sclerosis in temporal cases had worse outcome after reoperation.Citation6
Duration of epilepsy. Siegel et al described in a series of 64 patients with reoperations.Citation15 In this study patients with duration of epilepsy greater than 5 years had more possibilities of reoperation. This risk factor was present in our study, because our patient began to experience seizures at the age of 5 years and had a history of epilepsy of 22 years.
Multifocal seizure onset and candidacy for surgery. In a series of reoperated patients, a common reason of failure and reoperation is a previously demonstrated multifocal seizure onset.Citation6 In the majority of these cases the surgery is used for palliative reasons. Salanova et al described some cases of reoperations where the resection was initially frontal and then the second resection involved temporal structures, suggesting that multifocal seizure onset is an important reason for reoperation.Citation16
Development of new epileptogenic foci. Awad et al described some patients with new distant epileptogenic areas, suggesting the development of new epileptogenic foci after the first resection.Citation2 In our case the involvement of the temporal area could be a new epileptogenic area but could possibly be an epileptogenic area that was not discovered initially.
Coexistence of generalized epilepsy. Hennessy et al described the neurophysiological findings of a group of patients with reoperations. Few patients had generalized epileptiform discharges.Citation10 The possibility that some patients with reoperations can have coexistence of primary generalized epilepsy in addition to focal epilepsy is an important consideration. The fact that our patient had both types of epilepsy could be an additional risk factor for reoperation.
History of encephalitis or head injury. Recent series have described that previous head injury or encephalitis could be a strong predictor of epilepsy surgery failure.Citation7,Citation17 The potential consequence of these types of events in life is a more widespread involvement in the brain with the possibility of multiple epileptogenic foci. Our patient did not have any of these risk factors that could explain the recurrence.
Incomplete resections. The most common reported situation in reoperated cases is the presence of residual mesial structures after temporal resections. Germano et al reported 40 patients with temporal epilepsy that had a second resection. Citation5 The imaging studies after surgery show that mesial structures were remaining in these 40 patients. The prognosis of patients after reoperation in this study was favorable, with 60% of patients rendered seizure free after surgery.
Lack of febrile seizures. Salanova et al compared 41 patients with seizure recurrence with 170 patients that were rendered seizure free after temporal resections. Citation7 They found that the lack of febrile seizures was an indicator for reoperation. Therefore, lack of previous febrile seizures in our patient could be an indicator for reoperation.
Scarring after surgery. Schwartz et al described some patients who had reoperations where the potential reason was secondary scarring after epilepsy surgery, in the vicinity of the previous resected epileptogenic area.Citation4 In our patient this factor could have been relevant. The first two surgeries may have triggered secondary scarring in the frontal area, increasing the risk of recurrence.
Genetic predisposition. We do not have enough information for a definite conclusion, but potentially a genetic predisposition could contribute to the risk of reoperations. The genetic predisposition to have seizures occurs more frequently in patients with generalized epilepsy, although some studies have suggested an increased genetic predisposition in some patients with partial epilepsy, potentially explaining the coexistence of generalized and focal epilepsy in the same patient, resulting in intractable epilepsy and potentially reoperations.Citation18
Conclusions
Resective epilepsy surgery is the most effective treatment for patients with pharmacoresistant, localization-related epilepsy, and surgery is the intervention that is most likely to render patients free from seizures.
The frequency of reoperation reported in the literature is variable, ranging from 3% to 14%.
When surgery fails, the correct understanding of why seizures occur, identifying patients who are at risk, and how to manage adverse outcomes when they do occur, is one of the most important endeavors facing epileptologists today.
Multiple factors are related to reoperations. Some of these are acquired characteristics of the patients, others are related to pitfalls in the investigation of patients, genetic predisposition, imaging or pathologic findings, and development of new epileptogenic foci.
Reoperation may be an appropriate alternative form of treatment for selected patients with intractable partial epilepsy who fail to respond to initial surgery.
Disclosure
Dr Téllez-Zenteno receives grants from the Royal University Hospital Foundation in Saskatoon and the University of Saskatchewan.
References
- Téllez-ZentenoJFDharRWiebeSLong-term seizure outcomes following epilepsy surgery: a systematic review and meta-analysisBrain20051281188119815758038
- AwadIANayelMHLudersHSecond operation after the failure of previous resection for epilepsyNeurosurgery1991285105182034344
- AwadIAReoperation for intractable seizuresClin Neurosurg1992391251391458738
- SchwartzTHSpencerDDStrategies for reoperation after comprehensive epilepsy surgeryJ Neurosurg20019561562311596956
- GermanoIMPoulinNOlivierAReoperation for recurrent temporal lobe epilepsyJ Neurosurg19948131368207525
- Gonzalez-MartinezJASrikijvilaikulTNairDBingamanWELong-term seizure outcome in reoperation after failure of epilepsy surgeryNeurosurgery20076087388017460523
- SalanovaVMarkandOWorthRTemporal lobe epilepsy: analysis of failures and the role of reoperationActa Neurol Scand200511112613315644073
- HolmesMDWilenskyAJOjemannLMOjemannGAPredicting outcome following reoperation for medically intractable epilepsySeizure1999810310610222302
- DubeauFMcLachlanRSInvasive electrographic recording techniques in temporal lobe epilepsyCan J Neurol Sci200027Suppl 1S29S3410830324
- HennessyMJElwesRDBinnieCDPolkeyCEFailed surgery for epilepsy. A study of persistence and recurrence of seizures following temporal resectionBrain2000123Pt 122445246611099447
- BerkovicSFMcIntoshAMKalninsRMPreoperative MRI predicts outcome of temporal lobectomy: an actuarial analysisNeurology199545135813637617198
- O’BrienTJSoELMullanBPSubtraction peri-ictal SPECT is predictive of extratemporal epilepsy surgery outcomeNeurology2000551668167711113221
- O’BrienTJSoELCascinoGDSubtraction SPECT coregistered to MRI in focal malformations of cortical development: localization of the epileptogenic zone in epilepsy surgery candidatesEpilepsia20044536737615030499
- LeeSKLeeSYKimKKHongKSLeeDSChungCKSurgical outcome and prognostic factors of cryptogenic neocortical epilepsyAnn Neurol20055852553216037972
- SiegelAMCascinoGDMeyerFBResective reoperation for failed epilepsy surgery: seizure outcome in 64 patientsNeurology2004632298230215623690
- SalanovaVQuesneyLFRasmussenTAndermannFOlivierAReevaluation of surgical failures and the role of reoperation in 39 patients with frontal lobe epilepsyEpilepsia19943570808112260
- RamosEBenbadisSValeFLFailure of temporal lobe resection for epilepsy in patients with mesial temporal sclerosis: results and treatment optionsJ Neurosurg20091101127113419249930
- bou-KhalilBKreiLLazenbyBHarrisPAHainesJLHederaPFamilial genetic predisposition, epilepsy localization and antecedent febrile seizuresEpilepsy Res20077310411017046202