Abstract
We used the technology and principles of adult learning to enhance a one-day geroneuropsychology rotation for internal medicine residents in a busy neuropsychology clinic. We created a multimedia Microsoft PowerPoint™ presentation highlighting the role of neuropsychology in the medical care of older adults. We added an active learning experience in which the resident administered a screening tool. Finally, we incorporated a video-recording of the resident’s administration in the feedback session. We evaluated the effectiveness of these innovations by assessing change in performance on an objective test administered at the beginning and end of the rotation day and by analyzing residents’ ratings of the rotation. Objective testing showed significant learning regardless of level of curriculum enrichment. However, residents’ ratings generally rose as we added enhancements. These results suggest that health care professionals without technical training can devise effective setting-specific, computer-delivered educational programs. These techniques show promise for boosting learning in clinical settings without lengthening the rotation or increasing direct supervisor contact.
Introduction
How can a busy clinic provide an effective introduction to geroneuropsychology for internal medicine residents in a single day? Using technology, we transformed a largely passive, unstructured experience into an active outcome-oriented one without lengthening it or requiring more staff time.
Given world-wide population aging, all residents need training in good elder care. One of the ways in which Henry Ford Health System addresses this need is to require all internal medicine residents to complete a one-month geriatrics rotation. This rotation encompasses didactic and clinical experiences related to inpatient and outpatient medical care of older adults and to hospice programs. It also includes a single day in the Neuropsychology Clinic, a busy service to which patients of all ages come from referral sources throughout our large healthcare system and metropolitan community. This short rotation provides staff neuropsychologists with an invaluable opportunity to introduce residents to common psychological and neurological issues that arise in care of older adults in medical settings and to effective ways to address these questions.
Taking advantage of this training opportunity requires neuropsychology staff to overcome several obstacles. Most residents are unfamiliar with neuropsychology. Their backgrounds in psychiatry and neurology vary. Because of limited flexibility in the residents’ schedule, the one-day rotation in neuropsychology cannot be rescheduled when there are last-minute appointment changes in the Neuropsychology Clinic or unexpected clinical demands on neuropsychology staff involved in training.
Prior to this project, each resident watched a 4- to 5-hour clinical neuropsychological assessment of an older adult, met with a neuropsychology fellow or staff neuropsychologist for 15–60 minutes, and received reading material. Quality, length, and content of this one-on-one teaching time varied considerably in response to clinic and resident factors. From the resident’s perspective, the experience consisted chiefly of observation. Cancellations and other demands sometimes precluded observation. The resident’s and neuropsychologist’s informal remarks to the rotation supervisor constituted the only evaluation of the experience.
In contrast, guidelines for medical teaching and adult education emphasize the importance of outcome-oriented, problem-based, and patient-centered learning (CitationACGME 2004). Incorporating these principles ensures exposure to essential content, attitudes, and skills while taking maximal advantage of unexpected teaching opportunities in the clinic.
In this project, we sought to determine the efficacy of computer-assisted delivery of an instructional package. This package was designed to achieve the desired outcomes of our geroneuropsychology rotation despite variable prior resident knowledge and fluctuating clinical resources and demands.
In addition, our pilot study included other innovations suggested by the literature on clinical preceptorship. Neber’s group outlined skills facilitating effective clinical teaching in small time segments (CitationNeber et al 1992). Giving feedback to trainees about patient encounters is one of these core skills. Steinert advised that reviewing video-recordings of the trainee’s patient encounters during feedback further augments the resident’s learning (CitationSteinert 1993). Therefore, we added a curriculum component in which residents administered a screening measure and received feedback on their administration. In the final enhancement, the feedback session incorporated review of a video-record of the screening test administration.
Method
Setting
This research took place within the Neuropsychology Clinic of Henry Ford Behavioral Health, a component of Henry Ford Health System, a large not-for-profit healthcare system serving a very diverse patient base. Patients of all ages undergo individual clinical assessments. Residents viewed the curriculum in a separate room.
Curriculum
Technical equipment
Crucial equipment included a Dell DimensionTM 8250 PC with a 120 GB 7200 rpm hard drive (Dell Computer Corporation, Austin, TX, USA). This PC was equipped with hardware and software for capturing and editing video, including the RoxioTM Videowave Movie Creator. The operating system was Microsoft Windows® XP Professional. Microsoft OfficeTM (including PowerPointTM) was installed.
We used a PanasonicTM PV DV Camcorder 702 (Dynamic Computer Corporation, Livonia, MI, USA) to record snippets of simulated assessments. We downloaded video recordings to the PC via an IEEE Firewire, also known as an I-linkTM. We recorded resident administration of a screening tool with the same device. To provide timely feedback to residents, we used TVs in the Clinic for direct playback of recordings from the camcorder.
Computer-administered instructional package
The PowerPoint presentation subtopics were physician use of screening tools for cognitive impairment in older adults; the content, process, and purpose of clinical neuropsychological assessment; and problems of normal and abnormal aging. The presentation included narration, internet links, and video clips made with the digital camcorder. One video clip detailed administration of the MacNeill Lichtenberg Decision Tree (MLDT) (CitationMacNeill and Lichtenberg 2000; CitationBank et al 2002). Developed and validated by neuropsychologists, the MLDT helps physicians prioritize referrals of older adults to psychiatry and neuropsychology services.
Active learning experience
After viewing the MLDT video clip, the resident administered the MLDT to a patient or staff member with subsequent feedback from the observing staff.
Video-record review
A video-recording of this administration was reviewed during feedback.
Research participants
Forty-four of 47 trainees were internal medicine residents; 3 were psychiatry residents. The Henry Ford Health System Institutional Review Board reviewed the proposal for this study and determined that ethical requirements were met.
Study design
Residents received the most enriched curriculum available at the time of their rotation. The study ran about a year. For purposes of statistical analysis, we divided the residents’ rotation experiences into Baseline, Intermediate, Full, and Full plus Video categories. Each successive category subsumes earlier ones.
Baseline
Eighteen residents observed an interview and neuropsychological testing, received reading material, and met with a neuropsychology staff member for 15–60 minutes. One resident also saw an onscreen PowerPoint presentation identical to a handout included in the reading material.
Intermediate
Nine trainees completed a curriculum with some but not all of the components in the Full condition. Seven saw the original PowerPoint presentation enhanced with the MLDT video only. These trainees also administered the MLDT to a staff neuropsychologist or neuropsychology fellow and received verbal feedback. The remaining 2 trainees viewed the final narrated PowerPoint presentation with video clips of testing and the MLDT administration, but they did not administer the MLDT.
Full
Eleven trainees viewed the final narrated PowerPoint presentation with video clips, administered the MLDT, and received feedback on their administration.
Full plus video
For 9 residents, the recorded MLDT administration was played back during feedback.
Evaluation
Pre-test and post-test
A 25-item, anonymously completed, multiple-choice test included 3 subsections corresponding to the subtopics of the PowerPoint presentation.
Twenty-nine trainees had valid pre-test and post-test scores. Thirteen trainees in the baseline condition went through the rotation before test development; 5 trainees’ scores were dropped because of 2 or more omitted responses on either test.
Rating form
At the end, residents anonymously gave an “overall rating” and 5 specific ratings from 1 to 5 on a training rotation form developed by the psychiatry faculty for department-wide use (Frank C 2004 June 21, pers comm). Residents also had the opportunity to write in comments.
Three trainees omitted the ratings but took the pre-test and post-test.
Results
Pretest and post-test
We observed significant improvement from pre-test to post-test in the resident group as a whole (t [28] = −6.16, p < 0.001). Average pre-test and post-test scores were 15.5 and 17.6, respectively. Analyses also showed gains in test subsections.
To determine whether greater curriculum enhancement was associated with greater gains on the objective test, we calculated learning by subtracting the pre-test from the post-test score. We performed a 1-way analysis of variance on learning scores with 3 levels of curriculum enhancement (Baseline/Intermediate, Full, and Full Plus Video). Results were insignificant (F [2.26] = 0.46).
Rating form
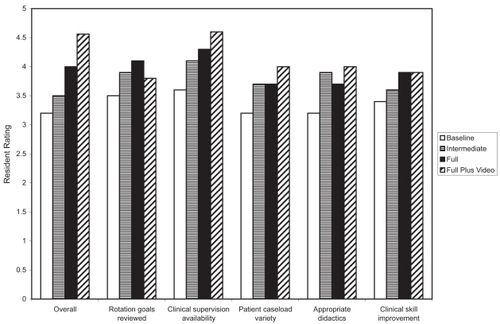
We calculated an asymmetric Somers’ d statistic based on the assumption that curriculum enrichment was the independent variable and the rating was the dependent. This ordinal-level statistic was significant for the overall rating and for 3 of 5 specific ratings, as shown in .
Figure 1 Mean resident rating as a function of level of curriculum enhancement. Ratings increased significantly with level of enrichment for resident judgments of the “Overall Rotation” (Somers’ d = 0.398, p < 0.001), “Available Clinical Supervision” (d = 0.325, p < 0.01), “Variety of Patient Caseload” (d = 0.26, p < 0.05), and “Appropriate Use of Didactic Teaching” (d = 0.248, p < 0.05), but not for “Improvement of Clinical Skills as Result of Rotation” or “Goals of Rotation Reviewed.” Rating points 1–5 were labeled “unacceptable,” “needs improvement,” “meets expectations,” “exceeds expectations,” and “superior.”
Discussion
In this pilot project, we developed and tested a self-paced, multimedia, geroneuropsychology curriculum designed to achieve specific outcomes. Administration of the MLDT, a cognitive screening measure, added an active learning component to the curriculum. In a further enhancement, residents received feedback on their administration of this measure. In the final enhancement, the supervisor reviewed a video-record of the residents’ MLDT administration during feedback. We designed and implemented our curriculum without specialized technical training. Costs were limited to the purchase of a research-dedicated personal computer capable of video-editing, a digital camcorder, microphone, tripod, and storage media. Running the enhanced curriculum did not lengthen the rotation or place additional time demands on staff.
The degree of curriculum enrichment correlated with residents’ self-reported learning, although objective learning was not associated with the level of enhancement. We are encouraged by these early results, which reflect our first attempts at creation of a self-paced, multimedia instructional package. We expect our program to become more effective as our experience in recording and editing video clips grows.
We recommend application of these techniques to other medical settings. Further studies may identify what mix of educational experiences best promotes learning and excellent patient care. Through technology, health-care professionals can make and update multimedia curricula inexpensively without special training and rise to the challenge of concurrent patient care and resident training.
Acknowledgments
We wish to acknowledge the support and guidance of Tom Palmer, Cathy Frank, and Kenneth Podell, as well as the inspiration and faculty development program provided by Marla Rowe and Francine Hekelman. June Blackwell, Brian Yochim, and Ann Marie McCullen helped us create the video clips.
At the time of the study, all authors were affiliated with the Neuropsychology Division of the Psychiatry Department of Henry Ford Health System. During most of the project, Anne Baird’s primary affiliation was with the Psychology Department at the University of Windsor. A Henry Ford Health System Educational Small Grant to the first three authors funded this study.
References
- [ACGME] Accreditation Council for Graduate Medical EducationGeneral competencies2004ACGME Outcome Project: Enhancing residency education through outcomes assessment [online] Accessed 23 June 2004 URL: http://www.acgme.org/outcome/comp/compFull.asp
- BankALMacNeillSEHallEM2002More than meets the eye: How examiner training affects the reliability of the MacNeill-Lichtenberg Decision Tree in geriatric rehabilitation patientsArch Phys Med Rehabil834051111887123
- MacNeillSELichtenbergPA2000The MacNeill-Lichtenberg Decision Tree: A unique method of triaging mental health problems in older medical rehabilitation patientsArch Phys Med Rehabil816182210807102
- NeberJOGordonKCMeyerB1992A five-step “microskills” model of clinical teachingJ Am Board Fam Pract5419241496899
- SteinertY1993Twelve tips for using videotape reviews for feedback on clinical performanceMed Teach1513198246709