Abstract
Background
Neurologic involvement in Behçet’s disease (BD), also known as neuro-Behcet’s disease (NBD), is one of the most devastating manifestations of the disease. The etiology of BD remains obscure and speculative. NBD usually occurs 1–10 years after the first symptom of BD has occurred, and its incidence is 18% (range of 4%–49%).
Objective
This study was conducted to describe the clinical and prognostic aspects of neurologic involvement in BD among patients attending a multidisciplinary hospital clinic.
Methods
Eighty patients with BD were diagnosed according to the International Study Group Criteria for BD at our hospital. Sixteen patients (20%, including 11 men and five women) had evidence of and fulfilled the diagnostic criteria for NBD. These patients underwent laboratory and imaging investigations, including human leukocyte antigen-typing, lumbar puncture, electroencephalographic studies, and computed tomography scanning.
Results
Fourteen of the 16 patients received high-dose steroids, and four of these 14 patients were treated with a combination of steroids and cytotoxic agents. Relief was observed in 14 of 16 patients (87.5%). The remaining two patients were untreated males who suffered severe brainstem lesions, and later died.
Conclusion
In contrast with previous reports of a poor prognosis with NBD, our study shows that early aggressive intervention with corticosteroids and cytotoxic agents may ameliorate the prognosis in these patients, and can diminish and stabilize the negative effect of neurologic involvement.
Introduction
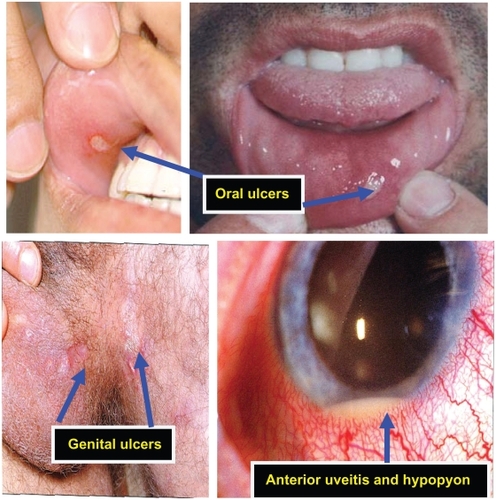
In 1937, Hulusi Behçet, a Turkish dermatologist, described a “triple symptom complex” of aphthous ulceration, genital ulceration, and iridocyclitisCitation1 (). Since Behçet’s original description, many musculoskeletal, gastrointestinal, urogenital, cardiac, cutaneous, and neurologic symptoms have been attributed to Behçet’s disease (BD).Citation2–Citation4
Figure 1 Triple symptom complex commonly observed in Behcet’s disease: Aphthous ulceration, iridocyclitis, and genital ulceration. Aphthous ulceration often appears as the first symptom, ie, a painful, oval or round, shallow or deep, 1–20 mm lesion with central whitish or yellowish necrotic base and red halo. Almost always present during flares, and may precede other features by years. Iridocyclitis and ocular disease is usually more bilateral than unilateral, with anterior uveitis and hypopyon commonly observed. Retinal involvement may also be present, ie, retinal vasculitis/optic neuritis or atrophy and genital ulceration, which are similar in appearance and usually present as large ulcers which are deep and often cause scarring.
Although the cause of BD is unknown, autoimmune, infectious, and genetic causes have been suspected. Environmental factors, such as microbial infections, are also suspected to be factors that contribute to the development of BD. Because BD has a characteristic geographic distribution spanning the Mediterranean basin and Asia, it is also known as “Silk Road” disease,Citation5–Citation6 the Silk Road being a geographic distribution along the historic route of commerce and travel between Europe and Asia. In fact, BD is more common (and often more severe) along the ancient Silk Road, especially from Eastern Asia to the Mediterranean.Citation5 It is most common in Turkey (80–300/100,000),Citation7 while the prevalence ranges from 10–20/100,000 in Japan, Korea, China, Iran, and Saudi Arabia.Citation7–Citation9 The prevalence of BD in Paris, France, in 2003 was reported to be 7.1/100,000, with rates of 2.4/100,000 in those of European ancestry, 34.6 in those of North African ancestry, and 17.5 in those of Asian ancestry.Citation10–Citation11 The prevalence ranges from 1/15,000 to 1/500,000 in Northern American (Olmsted County, MN) and Northern European countries.Citation5
BD is somewhat more common in men in the Eastern Mediterranean area and in women in Northern European countries, and typically affects young adults aged 20–40 years.Citation5 However, the epidemiology of the disease shows geographic variation, coupled with a similar variation in human leukocyte antigen (HLA)-B51 which has been reported to be associated strongly with the disease in high prevalence areas.Citation12–Citation15
Diagnosing BD can take a long time because symptoms may wax and wane, and it may take months or even years to develop all of the symptoms. There is no cure, and treatment focuses on reducing pain and preventing serious complications of the disease.
Currently, the most widely used diagnostic criteria for BD is the International Study Group’s classificationCitation16 (), which requires recurrent oral ulceration plus two of the following in order to establish a definite diagnosis, ie, recurrent genital ulcerations, skin or eye lesions, or a positive pathology test.Citation17 Although the diagnosis is made on the basis of the combination of typical clinical symptoms, radiologic findings of BD show characteristic features of gastrointestinal, neurologic, cardiovascular, and thoracic organ system involvement.Citation2
Table 1 International Study Group criteria for Behçet’s diseaseCitation16
In the gastrointestinal tract, BD may produce various types of ulcers in the esophagus, stomach, and small and large intestines, as well as deeply penetrating ulcerations in the ileocecal region, frequently accompanied by enteric fistulae. Neurologic involvement includes typical and atypical parenchymal NBD, dural sinus thrombosis, cerebral arterial aneurysm, occlusion, dissection, and meningitis.Citation2
Neurologic involvement in BD was first reported in 1941 by Knapp,Citation17 and the term “neuro-Behçet’s syndrome” was introduced by Cavara and D’Ermo in 1954.Citation18
The reported rate of development of neurologic involvement among BD patients ranges from 4% to 49%.Citation19–Citation23 It has been reported that neurologic involvement develops over a time interval of more than 10 years after the onset of BD,Citation22,Citation24 and is classified as parenchymal or nonparenchymal.Citation22,Citation23
Parenchymal involvement primarily affects the brainstem, spinal cord, and cerebral hemispheres. Nonparenchymal involvement includes intracranial hypertension, aseptic meningitis, cranial neuropathy, and cerebrovascular disorders such as dural sinus thrombosis, arterial dissection, occlusion, and aneurysm. Central nervous system (CNS) involvement is one of the most dangerous manifestations of BD.Citation20
The disease tends to involve the white matter portion of the brain and brainstem, and may lead to headaches, confusion, strokes, personality changes, and (rarely) dementia. BD may also involve the meninges, leading to meningitis. Because the meningitis of BD is not associated with any known infection, it is often referred to as “aseptic” meningitis. Citation25 NBD is commonly a motor–mental disorder, with a predilection for the brainstem and the basal ganglion region, as suggested by earlier neuropathology studies and neuroradiologic data. At the time of a neurologic attack, typical neuroradiologic findings have been defined.Citation26
Polymorphonuclear pleocytosis and/or absence of IgG oligoclonal bands are suggestive of NBD. The presence of worse prognostic factors should be considered when treatment is initiated. The presence of abnormal cerebrospinal fluid (CSF) and parenchymal involvement, especially of the “brainstem +” type, justifies more aggressive treatment.Citation22
Vascular involvement is divided into three subsets, including venous occlusion, arterial occlusion, and arterial aneurysm.Citation3 Cardiac manifestations include intracardiac thrombus, endomyocardial fibrosis, periaortic pseudoaneurysm, and rupture of the sinus of Valsalva.Citation2 Manifestations of BD in the thorax include pulmonary arterial aneurysm, pulmonary arterial thromboembolism, and thrombosis in the superior vena cava, pulmonary infarction, hemorrhage, and vasculitis of the pleura and pericardium.Citation2,Citation27
The various manifestations of BD respond to steroid treatment. Citation28 However, one of the characteristics of BD is a high rate of complications and recurrence after surgery. Familiarity with its various radiologic and clinical characteristics is essential for making an accurate early diagnosis and for prompt treatment of patients with BD. Susceptibility to BD is strongly associated with the presence of the HLA-B51 allele,Citation29–Citation32 or HLA-B5, coupled by a negative lupus band test.
Although the pathogenesis of BD is largely unknown, associations with HLA-B51, genetic mutations including Factor V Leiden, and triggering by microbial antigens have been identified.Citation33 Mutation of Factor V Leiden is recognized as the most common hereditary abnormality causing hyper-coagulability, and is associated with BD.
NBD may present as acute focal or multifocal CNS dysfunction, and the clinical picture of NBD may resemble multiple sclerosis (MS).Citation21,Citation34–Citation39
It has been observed that a substantial number of patients with NBD have a relapsing–remitting course while others may have a secondary progressive course. Some NBD patients have an insidious onset of the disease with primary progressive CNS dysfunction, and others may display symptoms attributable to intracranial hypertension associated with dural venous sinus thrombosis.Citation40–Citation42
Although nonneurologic involvement generally precedes neurologic findings, it may go unrecognized in some cases or may appear late in the course of BD, thus posing diagnostic difficulties.Citation43–Citation45 Peripheral nerve involvement, although reported in NBD, is relatively uncommon.Citation46
The purpose of this investigation was to determine the frequency of the various neurologic symptoms in BD, to describe the clinical patterns of neurologic presentation in BD patients attending a multidisciplinary hospital clinic, and to examine the impact of neurologic disorders on the prognosis of the disease.
Methods
Eighty patients were identified as having been diagnosed with BD at our hospital during the previous 30 years. The diagnosis was based on at least three of four criteria, ie, aphthous stomatitis, genital ulceration, ophthalmic lesions, and skin erythema. Every patient suspected of suffering from neurologic symptoms was examined by a neurologist. The time interval elapsing between onset of the disease and appearance of neurologic symptoms was recorded.
The 80 patients were diagnosed according to the International Study Group’s classification (), which requires recurrent oral ulcerations plus two of the following in order to establish a definite diagnosis, ie, recurrent genital ulcerations, skin or eye lesions, and supported by neutrophil chemotaxis, HLA-B51, or HLA-B5, and coupled with a negative lupus band test. Sixteen patients (20%, including 11 men and five women) had evidence of NBD. Fifteen of these patients were of Middle Eastern or North African origin, and one patient was an Ashkenazi Jew. Age of onset in our series was 18–38 (mean age 25.5) years. Age of onset of neurologic symptoms was 25–41 (mean 31.6) years. The time interval between onset of BD and neurologic manifestations varied widely, up to a maximum of 23 years. The 16 patients who had evidence of NBD underwent laboratory and imaging investigations. HLA-typing and electroencephalographic (EEG) studies were performed on all 16 patients, computed tomographic (CT) scan in 12, and lumbar puncture in 11 ().
Table 2 Results of laboratory investigations, EEG, CT scan, and CSF examination in 16 patients with BD
Results
HLA-B51, which serves as an immunogenetic marker for a subgroup of patients with BD, was present in nine NBD patients, and HLA-B5 was present in two patients. EEG results were normal in nine patients, with three showing diffuse slowing, two showing diffuse slowing and sharp waves, and other two having clinical convulsions. CT scan was normal in nine patients, with one patient showing a low-density lesion in the parietal lobe and in the brainstem, one patient having a low-density lesion in the brainstem, and another patient show sagittal sinus thrombosis. The remaining four patients refused to undergo a CT scan. With regard to CSF results, 11 patients had predominantly lymphocytic pleocytosis and two patients had positive oligoclonal immunoglobulin G bands (). The most frequent neurologic manifestations were mild cognitive impairment (19%), severe headache (12.5%), convulsive disorders (12.5%), dural sinus thrombosis (6%), optic atrophy (19%) and other cranial nerve palsies (19%), hemispheric syndrome (19%), severe brainstem lesions (12.5%), pyramidal signs (19%), cerebellar signs (19%), myelopathy (20%), and peripheral neuropathy (6%, ). Subacute onset and a relapsing-remitting course were the most commonly observed temporal patterns.
Table 3 Neurological manifestations observed among our patients
Treatment
Of 14 patients who received high-dose steroids, 13 were given prednisone 60–80 mg/day orally and one patient was treated with intravenous methylprednisolone 1000 mg/day, with gradual tapering of the dose. Four patients were treated with a combination of steroids and cytotoxic agents, namely azathioprine or chlorambucil. By the end of the treatment period, marked relief was observed in 87.5% of patients, except for two males who suffered severe brainstem lesions, did not receive any treatment, and subsequently died. One of these patients died three years after onset of severe neurologic symptoms, and the other died shortly after a brainstem stroke, having suffered from headache and a convulsive disorder for 30 years.
Discussion
Since the f irst description of BD in 1937,Citation17 and the subsequent first report of neurologic involvement in BD in 1941,Citation47 a plethora of studies of NBD have been reported. In addition to the triad of symptoms commonly observed in BD, ie, aphthous ulceration, iridocyclitis, and genital ulceration, other multisystem disorders of unknown etiology have been reported, and almost all organ systems can be involved.Citation2–Citation4 Clinical involvement of the CNS is in the range 4%–49%.Citation4,Citation19–Citation23,Citation48
NBD can be mistaken for other CNS diseases with multifocal presentations, such as multiple sclerosis (MS) and systemic lupus erythematosus (SLE), especially in the absence of systemic manifestations of BD.Citation22 In the acute phase of NBD, large confluent lesions in the brainstem- thalamic-basal ganglia region are highly suggestive of the disease, and can help to differentiate it from MS and SLE.Citation26 In SLE, the lesions predominantly involve the subcortical white matter of the cerebral hemispheres and less frequently involve the basal ganglia or brainstem.Citation26 In MS, the lesions are predominantly periventricular, with infrequent involvement of the basal ganglia and internal capsule.Citation49 Moreover, brain stem lesions in MS are usually small, even in the acute stage, and seen along the floor of the fourth ventricle or anteriorly in the pons. This distribution contrasts with involvement of the central part of the pons in NBD.Citation50 Spinal cord involvement in NBD tends to be extensive, whereas it rarely extends over more than two vertebral segments in MS.Citation4
Neurologic involvement in BD is classified into parenchymal and nonparenchymal.Citation22,Citation23 Parenchymal NBD is more common, and presents with attacks of hemiparesis, cognitive changes, and sphincter disturbance.Citation20 This form of involvement has a predilection for the brainstem, thalamic, and basal ganglia regions. The junction of the midbrain and thalamus (mesodiencephalic junction) is characteristically involved and it is the most common neural parenchymal structure involved. The pontobulbar region is the next most commonly affected area.Citation51–Citation54
The disease involves the basal ganglia and internal capsule region in one-third of the cases. The globus pallidus and posterior limb of the internal capsule are characteristically involved, and lesions in the basal ganglia may extend along the corticospinal tracts to the cervical cord. It should be noted that several factors influence the course and prognosis of NBD; parenchymal involvement, especially of the brainstem, and high CSF cellular and/or protein content, are significantly associated with a worse prognosis.Citation51–Citation54
Sixteen patients (11 males and 5 females) in this series had evidence of NBD ( and ). Two deaths occurred in patients who had suffered from severe brainstem lesions for a long time and had received no treatment during their illness. In the other 14 patients, brainstem lesions were absent, and other neurologic manifestations, including cognitive impairment, sphincter disturbance, and pyramidocerebellar involvement were relatively mild. In fact, mild cognitive impairment was observed in 3/16 patients (Mini- Mental state score 27, 28, and 29, possible total score 30).
Fourteen of the patients in this study improved or stabilized after aggressive steroid treatment, and a number had two or more episodes of neurologic involvement, with improvement on steroid therapy (87.5%). In our view, their favorable prognosis was influenced by their stable clinical course and reduced disability. Certainly, early diagnosis and immediate administration of high-dose corticosteroid and cytotoxic therapy increased survival and decreased the disability and mortality in this patient series.
Conclusion
As described here, the clinical course of NBD may manifest in several ways, including a remittent form with a progressive trend, called the “remittent type”, a remittent form that later becomes progressive, called the “remittent-progressive type”, and the “progressive or monophasic type”.
The clinical course in our patients, except for the two deaths, was more benign, with two distinct patterns identified, ie, a monophasic or biphasic form with almost complete neurologic remission and a remittent or polyphasic form with no significant neurologic deficit between relapses.
Early administration of steroids, or combined steroid and cytotoxic therapy, may have beneficially influenced our findings. In contrast with previous reports of a poor prognosis in NBD, our study shows that immediate and aggressive treatment with corticosteroids and cytotoxic agents may ameliorate the prognosis in patients with mild to moderate NBD, and can diminish and stabilize the negative effect of neurologic involvement in the disease.
Disclosures
The authors report no conflict of interest in this work.
References
- BehçetHUber rezidivierende Aphthose durch ein Virus-veursachtr Geschwur am Mund, am Auge und an den GenitalienDermatol Monatsschr19373611521157
- ChaeEJKyung-HyunDSeoJBRadiologic and clinical findings of Behçet disease: Comprehensive review of multisystemic involvementRadiographics200828e3118603663
- KalkoYBasaranMAydinUKafaUBasaranogluGYasarTThe surgical treatment of arterial aneurysms in Behçet disease: A report of 16 patientsJ Vasc Surg20054267367716242553
- KocerNIslakCSivaACNS involvement in neuro-Behcet syndrome: An MR studyAm J Neuroradiol1999201015102410445437
- SakaneTTakenoMSuzukiNInabaGBehcet’s diseaseN Engl J Med1999341128410528040
- JamesDGSilk route diseasePostgrad Med J1986621511533714598
- YaziciHYurdakulSHamuryudanVKlippelJHDieppePABehcet’s syndromeRheumatology2nd edLondon, UKMosby International1998
- ShimuzuTEhrlichGEInabaGHayashiKBehcet disease (Behcet syndrome)Semin Arthritis Rheum19798223260382361
- Al-DalaanAAl-BallaSAl-SukaitMBahabriSMousaMBigariTThe prevalence of Behcet’s disease in Al Qassim region of Saudi ArabiaVIIth International Conference on Behcet’s diseaseRevue du RhumatismeEnglish ed199663539 Abstr C09
- MahrABelarbiLWechslerBPopulation-based prevalence study of Behcet‘s disease: differences by ethnic origin and low variation by age at immigrationArthritis Rheum200858395119035493
- YaziciHSeyahiEYurdakulSBehcet’s syndrome is not so rare: Why do we need to know?Arthritis Rheum200858364019035470
- YaziciHAkhanGYalçinBMüftüoluAThe high prevalence of HLA-B5 in Behçet’s diseaseClin Exp Immunol197730259261606446
- YurdakulSGünaydinITüzünHThe prevalence of Behçet’s syndrome in a rural area in northern TurkeyJ Rheumatol1988158208223172095
- OhnoSOhguchiMHiroseSMatsudaHWakisakaAAizavaMClose association of HLA-BW51 with Behçet’s diseaseArch Opthalmol198210014551458
- MizukiNInokoHOhnoSMolecular genetics (HLA) of Behçet’s diseaseYonsei Med J1997384234279509912
- The International Study Group for Behçet’s DiseaseEvaluation of diagnostic (“classification”) criteria in Behçet’s disease: Towards internationally agreed criteriaBr J Rheumatol1992312993081581771
- KnappPBeitrag zur Symptomatologie und Therapie der rezidiverenden Hypopyoniritis und der begleitenden apthösen SchleimhauterkrankungenShweiz Med Wochenschr19417112881290
- CavaraVD’ErmoEA case of neuro-Behçet’s syndromeActa XVII Concili Ophtalmologici195431489
- SerdarogluPBehçet’s disease and the nervous systemJ Neurol19982451972059591220
- FarahSAl-ShubailiAMontaserABehçet’s syndrome: A report of 41 patients with emphasis on neurological manifestationsJ Neurol Neurosurg Psychiatry1998643823849527155
- SivaASaipSKantarciONeuro-Behçet syndrome (NBS): Clinical and imaging correlatesJ Neurol1997244Suppl 3545
- Akman-DemirGSerdarogluPTasciBClinical patterns of neurological involvement in Behçet’s disease: Evaluation of 200 patients. The Neuro- Behçet Study GroupBrain19991222171218210545401
- KiddDSteuerADenmanAMRudgePNeurological complications in Behçet’s syndromeBrain19991222183219410545402
- MatsuoKYamadaKNakajimaKNakagawaMNeuro-Behçet disease mimicking brain tumorAm J Neuroradiol20052665065315760881
- KaraBSomerAPişkinSAydınlıNSalmanNYalçınINeuro- Behçet syndrome presenting as acute meningeal syndromeJ Infect200652e120e12316197999
- ÇobanOBaharSAkman-DemirGMasked assessment of MRI findings: Is it possible to differentiate neuro-Behçet’s disease from other central nervous system diseasesNeuroradiology19994125526010344509
- ErkanaFGülbATasaliaEPulmonary manifestations of Behçet’s diseaseThorax20015657257811413359
- Al-FahadSAl-ArajiANeuro-Behçet’s disease in Iraq: A study of 40 patientsJ Neurol Sci199917010511110561525
- Nabil SaklyNBoumizaRZrour-HassenSHLA-B27 and HLA-B51 determination in Tunisian healthy subjects and patients with suspected ankylosing spondylitis and Behçet’s diseaseAnn N Y Acad Sci2009117356456919758200
- de MenthonMLaValleyMPMaldiniCGuillevinLMahrAHLA-B51/B5 and the risk of Behçet’s disease: A systematic review and meta-analysis of case-control genetic association studiesArthritis Rheum2009611287129619790126
- ChangHKKimJUCheonKSHLA-B51 and its allelic types in association with Behçet’s disease and recurrent aphthous stomatitis in KoreaClin Exp Rheumatol2001195 Suppl 24S31S3511760395
- MizukiNOtaMKatsuyamaYSequencing-based typing of HLA-B*51 alleles and the significant association of HLA-B*5101 and -B*5108 with Behçet’s disease in Greek patientsTissue Antigens20025911812112028538
- VerityDHWallaceGRVaughanRWStanfordMRBehçet’s disease: From Hippocrates to the third millenniumBr J Ophthalmol2003871175118312928293
- MorriseySPMillerDHHermaszewskiRMagnetic resonance imaging of the central nervous system in Behçet’s diseaseEur Neurol1993332872938348915
- O’DuffyJDGoldsteinNPNeurologic involvement in seven patients with Behçet’s diseaseAm J Med197661170178952291
- MotomuraSTabiraTKoroiwaYA clinical comparative study of multiple sclerosis and neuro-Behçet’s syndromeJ Neurol Neurosurg Psychiatry1980432102137373318
- HerskovitsSLiptonRLantosGNeuro-Behçet’s disease: CT and clinical correlatesNeurology198838171417203185906
- MillerDHOrmerodIECGibsonADuBoulayEPGHRudgePMcDonaldWIMRI brain scanning in patients with vasculitis: Differentiation from multiple sclerosisNeuroradiology1987292262312886954
- SivaASaipSKantarciONeuro-Behçet syndrome (NBS): Clinical and imaging featuresNeurology199748Suppl 1 Abstr 362
- WechslerBVidailhetNPietteJCCerebral venous thrombosis in Behçet’s disease: Clinical study and long-term follow-up of 25 casesNeurology1992426146181549224
- SaipSSivaABasibüyükNNeuro-Behçet syndrome (NBS): Clinical and MRI featuresNeurology199242Suppl 3 Abstr 339
- HarperCMO’NeillBPO’DuffyJDForbesGSIntracranial hypertension in Behçet’s disease: Demonstration of sinus occlusion with use of digital subtraction angiographyMayo Clin Proc1985604194223889512
- DevlinTGrayLAllenNBFriedmanAHTienRMorgenlanderJCNeuro-Behçet‘s disease: Factors hampering proper diagnosisNeurology199545175417577675240
- KozinFHaughtonVBernhardGCNeuro-Behçet disease: Two cases and neuroradiologic findingsNeurology19772711481152563014
- IraguiVJMaraviEBehçet syndrome presenting as cerebrovascular diseaseJ Neurol Neurosurg Psychiatry1986498388403746317
- BasoPKaraIEkerEDilsenNKoniçeMOvulCClinical, electrophysiological, immunological and electron microscopic investigation of Behçet‘s diseaseBehçet’s DiseaseAmsterdam The NetharlandsExcerpta Medica International Congress Series1979
- BerlinCBehçet’s syndrome with involvement of central nervous systemArch Dermatol Syph194449227233
- GumaAAguileraCAcebesJArrugaJPonsLMeningeal involvement in Behcet’s disease: MRINeuroradiology1998405125159763339
- SimonJHNeuro-imaging of multiple sclerosisNeuroimaging Clin N Am19933229246
- WechslerBDell’IsolaBVidailhetMMRI in 31 patients with Behcet‘s disease and neurological involvement: Prospective study with clinical correlationJ Neurol Neurosurg Psychiatry1993567937988331356
- Al-ArajiAKiddDPNeuro-Behçet’s disease: Epidemiology, clinical characteristics, and managementLancet Neurol2009819220419161910
- SivaAKantarciOHSaipSBehçet’s disease: Diagnostic and prognostic aspects of neurological involvementJ Neurol20012489510311284141
- HaghighiABPourmandRNiksereshtARNeuro-Behçet disease: A reviewNeurologist200511808915733330
- HoCLDeruytterMJManifestations of neuro-Behçet’s disease: Report of two cases and review of the literatureClin Neurol Neurosurg200510731031415885390