Abstract
Diagnosis of complex partial epilepsy is based on the clinical history, and laboratory tests, including EEG and neuroimaging studies, corroborate the diagnosis. The goal of epilepsy management is to make the patient completely seizure-free without drug-induced side effects, even in the patient with refractory complex partial seizures. Frequently this can be accomplished by choice of the optimal antiepileptic drug (AED) or a combination of drugs, the use of strategies to maximize the effectiveness of drug treatment, or by surgical removal of the seizure focus. Currently there are five “classical” first-line AEDs and 11 new AEDs available in the US and in many other countries for the treatment of localization-related epilepsy. The current state of the evidence is that no AED is clearly superior to other AEDs in the management of refractory complex partial seizures. Therefore the choice of which drug to use in an individual patient has to be based on other considerations, including the potential adverse reactions that may occur in that patient. There are a number of strategies for optimal use of AEDs in the management of refractory complex partial seizures. These include verification of the diagnosis of epilepsy and classification of specific seizure types, use of monotherapy if possible but polytherapy if necessary, starting with a low dose and raising it slowly but, until complete seizure control is achieved, pushing to the maximum tolerated dose, changing timing of dosing to reduce toxicity, using pharmacokinetic principles to fine-tune AED doses, adjusting dose for drug–drug interactions, and never giving up in the pursuit of better seizure control. Resection of the seizure focus can be curative in the majority of patients with seizures localized to one mesial temporal lobe. Success rates for resection of extratemporal seizure foci are lower. Vagus nerve stimulation (VNS) devices result in a significant reduction of seizure frequency in many patients, but patients rarely become completely seizure-free as a result of VNS device implantation. Management of refractory complex partial seizures continues to improve with the identification of new drugs and the development of new approaches to their control and cure.
Introduction
Epilepsy is the second most common neurologic disorder after headache. At least 50 million people in the world suffer from recurrent nonprovoked seizures,Citation1 with age-adjusted prevalence rates of 0.2% to 4.1%, depending on the population studied.Citation2 Fundamentally, there are two types of epilepsy, primary (or idiopathic) generalized epilepsy and localization-related epilepsy. Primary generalized epilepsy is considered to be genetic in etiology, whereas most localization-related epilepsy is presumed to be the result of a cerebral insult, even though the insult cannot be determined in about half of all epileptic patients, regardless of age.Citation3–Citation8 However, recent developments in imaging technology have reduced this figure in children and young adults with refractory epilepsy, where malformations of cortical development have been implicated in about 25% of such cases.Citation9–Citation13
Localization-related epilepsy is manifested as one or more of three types of seizures: simple partial, complex partial, and partial onset with secondary generalization. The specific seizure type exhibited by a person with localization-related epilepsy is determined by many factors, including choice and dose of antiepileptic drugs, and may vary in the same individual as a result of changes in both the internal and external environment. Localization-related epilepsy accounts for about 60%–75% of all epilepsy, and more than half of such patients experience complex partial seizures.Citation14,Citation15 Only about half of patients with complex partial seizures have epilepsy that can be fully controlled with medication; the other half have seizures while on antiepileptic drugs, or experience significant side effects in order to gain complete seizure control. From these statements, it should be apparent that there are more than 7.5 million people in the world with refractory complex partial seizures. This article will discuss recent advances and strategies in the management of refractory complex partial seizures. Seizures are generally considered refractory when two are more antiepileptic drugs have failed to control the seizures. For research purposes, full control has been defined as complete cessation of seizures for at least one year.Citation16,Citation17
Epidemiology
The incidence of epilepsy overall is highest in infancy and early childhood, and in the elderly.Citation3,Citation8 However, this U-shaped distribution is not true in localization-related epilepsy, where the incidence is around 20/100,000/year from birth to 60 years of age, after which the incidence rises dramatically.Citation8 In a UK study, the incidence of epilepsy (almost all of which was localization-related) increased from 76/100,000 in people 60–69 years of age to 159/100,000 in those 80 years and older.Citation18 This dramatic rise in new onset epilepsy in the elderly is largely attributable to cerebrovascular disease and degenerative disorders, such as Alzheimer’s disease.Citation19,Citation20 These numbers may represent an underestimate of the true incidence, because in a number of epidemiologic studies of epilepsy it is likely that many secondarily generalized tonic-clonic seizures have been labeled as generalized, rather than partial onset. Furthermore, the incidence of epilepsy is clearly higher in developing countries than in industrialized countries.Citation21 Nonetheless, it is worthwhile to review further what is known about the epidemiology of localization-related epilepsy in general and, to the extent possible, of intractable complex partial seizures.
Four studies have reviewed the epidemiology of localization-related epilepsy.Citation3,Citation14,Citation22–Citation24 Over a 50-year period from 1934 to 1984, 880 people were diagnosed with epilepsy in Rochester, Minnesota (a predominantly Caucasian middle-class community). Fifty-seven percent had localization-related epilepsy and, of these, two-thirds had complex partial seizures. The age-adjusted incidence of individuals with complex partial seizures was 16/100,000/year.Citation3 In Southwest France the overall incidence of symptomatic localization-related epilepsy was 17.1/100,000 but 33.2/100,000 in those aged 60 or older.Citation23,Citation24 In a Danish study of 1508 consecutive adults, 73.5% had localization-related epilepsy, and individuals with complex partial seizures accounted for 38.2% of all cases.Citation14 Patients with complex partial seizures accounted for 21.4% of the cases in a recent Icelandic study but nearly half of the cases were listed as generalized, not otherwise specified.Citation8
The etiology of localization-related epilepsy is highly dependent on the age of onset. In all age groups, the etiology cannot be determined in more than half (55%–89%) of all individuals with epilepsy.Citation15 When etiology can be determined, congenital anomaly is the largest etiologic category in children. In young adults the etiology is unknown in more than 75% of patients, but head trauma is the largest single etiologic category. In adults aged 35–64 years, head trauma, vascular insults, and tumors are all important etiologies, whereas cerebrovascular disease and degenerative disorders account for most of the identifiable etiologies in localization-related epilepsy in individuals 65 years of age or older.Citation19 Advances in neuroimaging techniques have improved understanding of the etiology of localization-related epilepsy. Imaging has allowed the identification of the cause of epilepsy in many patients, especially children previously considered to have cryptogenic epilepsy. For instance, Kuzniecky et alCitation10 reported that 25% of children undergoing surgery for medically intractable partial seizures had magnetic resonance imaging (MRI) and pathologic findings of cerebral developmental anomalies.
Traumatic brain injury is an important cause of localization-related epilepsy, especially in military personnel. Traumatic brain injury has become known as the signature injury in the Iraq and Afghanistan conflicts because the use of body armor and the frequency of blast injuries have allowed many soldiers to sustain but survive head injuries. As many as 50% of individuals with severe head injuries, especially penetrating head injuries, may develop localization-related epilepsy, most often within the first two years.Citation25
Clinical features
Localization-related epilepsy is manifested as simple partial seizures, complex partial seizures, and partial onset seizures that become secondarily generalized. All start from a cortical seizure focus. Simple partial seizures remain sufficiently localized that there is no impairment of consciousness, and the clinical features of the seizure are a reflection of the location of the seizure focus. Complex partial seizures spread sufficiently to engage portions of the opposite hemisphere, and thus result in at least some impairment of consciousness, ie, decreased contact with the environment. Secondarily generalized seizures start from a cortical focus, but spread to the diencephalon and the opposite hemisphere to produce complete impairment of consciousness and generalized tonic-clonic convulsions.
The clinical semiology of complex partial seizures depends on the location of the cortical seizure focus. The temporal lobe is the most common site of origin of complex partial seizures.Citation26,Citation27 About 80% of patients with localization-related epilepsy have temporal lobe seizures.Citation28 Complex partial seizures of mesial temporal origin are frequently associated with mesial temporal sclerosis on MRI studies and often begin with an aura. Most common are viscerosensory sensations such as a rising sensation from the abdomen, or a sense of fear. Déjà vu and olfactory sensations are less common. Oro-alimentary automatisms (lip smacking, chewing) are common. Head turning to the ipsilateral side, manual automatisms on the ipsilateral side, or dystonic posturing of the contralateral upper extremity may help lateralize the seizure focus.Citation29 Postictal confusion usually lasts at least several minutes, after which there is gradual recovery. Typically, the patient is amnestic for events during the complex partial seizure. However, many patients insist that they are able to perceive their environment during complex partial seizures. This likely is because they remember the simple partial portion of the seizure, which they perceive as the complete seizure. Complex partial seizures of lateral or other neocortical temporal origin probably constitute less than 10% of temporal onset seizures.Citation27 It has been suggested that neocortical temporal lobe seizures most commonly begin with sensory illusions or auditory hallucinations, rapid loss of contact with the environment, early contralateral dystonic posturing without oro-alimentary automatisms, shorter seizure duration, and frequent secondary generalization.Citation27 Maillard et alCitation30 have described three electrophysiologic subtypes of temporal lobe epilepsy.
Frontal lobe onset complex partial seizures are most commonly nocturnal. Typically they are abrupt in onset, short in duration, and have little or no postictal confusion. Behavior can be explosive and bizarre.Citation31 Because of the bizarre behavior and frequent difficulty recording unequivocal ictal discharges on the EEG (because of large areas of frontal cortex inaccessible to surface electrodes), such seizures may at times be considered psychogenic nonepileptic seizures. However, the stereotyped nature of such seizures in a given patient, regardless of how bizarre the behavior is, should alert the physician to the likelihood of frontal lobe seizures. Characteristics of frontal lobe seizures may vary considerably, depending on location of the seizure focus within the frontal lobe. Characteristics of seven different types of frontal lobe seizures have been detailed in the International Classification of Epilepsies and Epileptic Syndromes.Citation31
Occipital lobe origin complex partial seizures are much less common that those of temporal or frontal origin, and are characterized by elementary or complex visual hallucinations or illusions. Forced blinking or eyelid flutter at the beginning of occipital origin seizures has also been described. The clinical features of occipital lobe complex partial epilepsies have recently been reviewed.Citation27
Parietal lobe epilepsy is the least common of the localization-related epilepsies. Partial onset seizures of parietal origin consist of sensory alterations, visuospatial disorientation, or apraxias. Seizures arising from or spreading to the parietal eye field may result in ipsilateral movement of the eyes, in contrast with seizures engaging the frontal eye field, which drive the eyes contralateral to the seizure focus.Citation32
Diagnosis of complex partial seizures is based on the clinical history, as is true when dealing with all types of epilepsy. Fundamentally epilepsy is a clinical diagnosis. Laboratory tests, including EEG and imaging studies, corroborate the clinical diagnosis. presents characteristic features of epileptic seizures, which by history taking enable their differentiation from syncopal spells or psychogenic events. presents a series of questions useful in making the diagnosis of an epileptic seizure by history. Deacon et alCitation33 studied the accuracy of clinical histories taken by epileptologists in the identification of seizures in 88 patients with suspected refractory complex partial seizures. They reported sensitivity for seizure identification of 96%, but specificity of only 50%. Accuracy for complex partial seizures and generalized seizures was higher than for simple partial seizures. Misidentification occurred only with simple partial seizures and nonepileptic events.
Table 1 Characteristics of epileptic seizures
Table 2 Historical information helpful for diagnosis of epilepsy
The history is also critical in the search for the etiology of the patient’s epilepsy. It is essential to review the patient’s medical history in sufficient detail to identify possible risk factors for epilepsy. This is especially important if the etiology is one that itself requires treatment and, ideally, can be corrected.
The purpose of the neurologic examination in evaluating the patient with possible epileptic seizures is two-fold. First, the presence of even subtle abnormalities on the neurologic examination adds support to the likelihood that the patient’s “spells” are epileptic seizures. Second, identification of lateralizing abnormalities on the neurologic examination allows prediction, to some extent, of the location of the epileptic focus. This is also done by including specific questions regarding seizure semiology when taking the history from patients and observers, and looking for such signs on video recordings of the seizures either from home videos or on an epilepsy monitoring unit (EMU).
Most lateralizing signs are contralateral to the seizure focus and include unilateral clonic activity, tonic activity in frontal origin seizures (but not temporal origin seizures), dystonic posturing, and version (forced deviation of head and eyes). Asymmetric tonic posturing producing a “figure-of-four” sign consists of flexion of the ipsilateral arm and rigid extension of the contralateral arm. The last clonic jerk is almost always on the side ipsilateral to the seizure focus, and unilateral postictal paralysis is always contralateral.Citation29 Unfortunately, none of these signs is 100% infallible, so such signs need to be used together to build a confident picture of lateralization, and need to be considered only as suggestive of the likely lateralization of seizure origin. Chung et alCitation34 recently described a highly reliable sign with which to differentiate between epileptic seizures and psychogenic nonepileptic events. Almost all (94%) patients with epileptic seizures keep their eyes open during the seizure, whereas almost all (99%) patients with nonepileptic events close their eyes during the seizure.
The electroencephalogram (EEG) is an essential element in the evaluation of patients with possible epilepsy, but finding epileptiform discharges on the EEG is not essential for the diagnosis. Even in adults with established epilepsy, only 29% to 55% have interictal spikes on their first EEG, although 80% to 90% will eventually show interictal spikes on repeated EEG examinations.Citation35 In localization-related epilepsy, finding an interictal spike focus, especially in the anterior or midtemporal regions, indicates cortical irritability or hyperexcitability, and strongly suggests the presence of a seizure focus in that location. Focal slowing, indicative of underlying structural damage, may also localize a seizure focus, but is much less specific than a spike or sharp wave focus. The likelihood of observing interictal spikes or sharp waves can be increased significantly by recording 30 minutes of sleep; other EEG activation procedures do not often reveal spikes or sharp waves not present during the routine recording.
Ictal discharges on the EEG are usually observed on an EMU, except on infrequent occasions when a seizure is captured on a routine EEG. Seizures recorded on EMU have the advantage that behavior recorded on video (seizure semiology, as described above) can be correlated with EEG changes. Almost all patients with localization-related epilepsy who are evaluated on an EMU have medically refractory seizures, so studies have not differentiated between ictal EEG findings in patients with medically responsive and medically refractory seizures. Ictal discharges recorded from scalp electrodes can vary in appearance, beginning with low-voltage fast activity or rhythmic slowing, or sometimes flattening of the EEG. There may be a heralding spike at onset, and interictal spikes may increase or decrease in frequency before a partial onset seizure. Onset can be quite focal in onset, begin simultaneously over most of one hemisphere, or begin diffusely over most electrodes. Characteristically, there is an evolution of the EEG changes, often with an increase in amplitude and decrease in frequency as the seizure progresses and, if the seizure has begun focally, spread to engage other cortical areas. As a generalization, seizures that impair consciousness exhibit associated EEG changes in scalp recordings, although frontal lobe origin complex partial seizures may not. Seizures that do not impair consciousness (simple partial seizures) may not exhibit EEG changes. Only 21%–61% exhibit a scalp EEG correlate.Citation36–Citation38 This is because the neuronal hypersynchronous discharges of the simple partial seizure may remain sufficiently localized that EEG changes are attenuated between cortex and scalp. The minimal size of a hypersynchronous cortical discharge that can be detected as a spike by scalp electrodes is 6 cm2,Citation39 but a 10 cm2 area of activation is much more likely to be detected on the surface as a spike or ictal rhythm, and synchronous activation of 10–20 cm2 of gyral cortex is common.Citation40,Citation41
Neuroimaging has become of increasing importance in the evaluation of refractory complex partial seizures with the development of high resolution MRI, new imaging protocols, and nuclear medicine procedures, such as positron emission tomography scanning, and ictal and interictal single positron emission computerized tomography (SPECT). More recently, subtraction ictal single-photon emission tomography coregistered to magnetic resonance imaging (SISCOM) has enhanced the power of SPECT. These new techniques have led to significant improvement in the ability to identify the ictal onset zone. For instance, it has been suggested that SISCOM can reveal areas of hyperperfusion or hypoperfusion in up to 80% of patients with intractable seizures and may also predict operative outcome.Citation42,Citation43
MRI continues to be the most sensitive and specific imaging technique for localization-related epilepsy. Detection of abnormalities (atrophy, increase in signal) can be enhanced by use of specific “seizure” protocols, which orient the image in the oblique coronal plane to best visualize the amygdalar and hippocampal structures. The introduction of increasingly powerful magnets has improved resolution as well. Hippocampal atrophy can best be seen using T1- weighted imaging, whereas increased signal brightness can best be appreciated with T2-weighted imaging or fluid-attenuated inversion recovery (FLAIR) sequences. Quantitative volumetric studies can be helpful for the detection of hippocampal atrophy, but are labor intensive and only available in a few centers.
Medical treatment
The goal of epilepsy management is to make the patient completely seizure-free. This is the goal of management of refractory complex partial seizures as well, and not infrequently can be achieved by the choice of the optimal AED or a combination of drugs, the use of strategies to maximize the effectiveness of drug treatment, or by surgical removal of the seizure focus.
Currently there are five “classical” first-line AEDs and 11 new AEDs available in the US and in many other countries (). Unfortunately, few direct comparisons provide data with which to determine the relative effectiveness of these drugs. Two US Veterans Administration Cooperative studies compared the classical AEDs in the treatment of new onset partial onset seizures in adults, using a randomized double-blind design. The principal outcome measure was retention on the drug (ie, the drug was sufficiently effective and sufficiently free of side effects that the patient and investigator agreed to continue that drug). In the first study, phenytoin (PHT) and carbamazepine (CBZ) were superior to phenobarbital (PB) and primidone (PRIM) in patients with mostly simple and/or complex partial seizures.Citation44 In the second study there was no difference in retention, but CBZ was superior to divalproex sodium in the treatment of complex partial seizures in four of five secondary measures.Citation45 A large, unblinded, randomized, pragmatic trial in hospital-based outpatients in the United Kingdom identified 1721 patients for whom CBZ was considered standard treatment (ie, those with partial onset seizures) and randomized them to treatment with one of five AEDs: CBZ, gabapentin (GBP), lamotrigine (LTG), oxcarbazepine (OXC), or topiramate (TPM). Two primary outcome measures were used, ie, time to treatment failure and time to 12-month remission. LTG was significantly better than CBZ, GBP, and TPM and had a nonsignificant advantage over OXC in the time to treatment failure measure, but CBZ was significantly better than GBP and had a nonsignificant advantage over LTG, TPM, and OXC in time to 12-month remission.Citation46 About 50% of patients reported side effects at some point in the study, but differences among AEDs were not large. Tiredness, headache, and fatigue were common symptoms for all drugs. Depression, disturbance of memory, and various psychiatric symptoms were also common, particularly with TPM. Rash was most common with CBZ and OXC, and least common with LTG. No multiple drug comparison trials have been done in patients with refractory complex partial seizures. A joint committee of the American Academy of Neurology and the American Epilepsy Society reviewed seven new AEDs (GBP, LTG, TPM, tiagabine [TGB], OXC, levetiracetam [LEV], and zonisamide [ZNS]) and considered all to be appropriate for adjunctive treatment of refractory partial seizures in adults.Citation47 Multiple individual drug comparisons have failed to show consistent superiority of the new AEDs over the classical AEDs or of one new AED over another in the treatment of either new onset or refractory partial onset seizures. Wilby et al conducted a systematic review of 212 studies of newer drugs for epilepsy (GBP, LTG, LEV, OXC, TGB, TPM, and vigabatrin). They concluded that there is “… little good-quality evidence from clinical trials to support the use of newer monotherapy or adjunctive therapy AEDs over older drugs, or to support the use of one newer AED in preference to another. In general, data relating to clinical effectiveness, safety and tolerability [have] failed to demonstrate consistent and statistically significant differences between the drugs”.Citation48
Table 3 AEDs available for partial onset seizures
The current state of the evidence, therefore, is that none of the presently available AEDs is clearly superior to other AEDs in the management of refractory complex partial seizures. Therefore, the choice of which drug to use in an individual patient has to be based on other considerations, including previous success or failure of a given drug, cost, and side effect profile of the drug matched to individual patient characteristics (). For instance, drugs associated with significant weight gain potential, valproate (VPA) and pregabalin in particular, might best be avoided in already overweight individuals. Drugs with significant potential for cognitive impairment (eg, TPM) should be used with caution in individuals with intellectually demanding occupations. AEDs that can be taken once daily (eg, PHT, ZNS, TPM, and extended-release forms of CBZ, LTG, and LEV) have a clear advantage in patients for whom denial of their epilepsy can frequently lead to poor compliance. In women of child-bearing potential, AEDs with a significant risk of teratogenicity (eg, VPA) should be avoided.
Table 4 Factors to consider when choosing an AED for a specific patient
There are a number of strategies for the optimal use of AEDs in the management of refractory complex partial seizures (). Diagnosis and classification of the seizure type and choice of AEDs have been discussed above. In the medically refractory patient, a review of previously tried AEDs is essential. Was the drug tried at maximal tolerated doses and given for long enough to achieve pharmacokinetic and pharmacodynamic steady states and to allow resolution of early treatment side effects, such as sedation and gastrointestinal upset? All too often potentially effective AEDs are abandoned because initial doses are so high or the rate of titration so fast that early side effects develop which could have been avoided had the drug been started more slowly. In the medically refractory patient, rapid titration of a new-to-the-patient AED is rarely necessary; the patient has had refractory seizures for a long time and a few days or even weeks spent slowly increasing the dose can often make the difference between success and failure.
Table 5 Strategies for optimizing management of refractory complex partial seizures
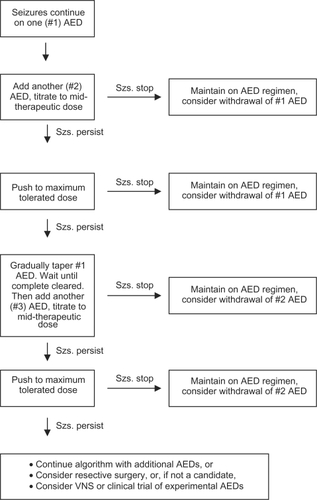
If possible, seizure control with a single agent is preferable. This avoids the potential for drug–drug interactions, is generally less expensive, and may result in better seizure control.Citation49 Therefore, ideally, each of the first-line AEDs available for management of partial onset seizures (ie, all current first-line drugs except ethosuximide) which are appropriate for the specific patient, should be tried before considering polytherapy. Although one drug may fail as monotherapy, another may succeed, even when the two drugs have similar profiles in animal models and share the same mechanism of action.Citation50 For example, when PHT and CBZ (both stabilizers of the sodium channel) were compared in three crossover trials in the treatment of complex partial seizures, some patients responded much better to one drug than to the other, even though there were no differences in the overall efficacy of the two drugs.Citation51–Citation53 However, sequential trials of AEDs as monotherapy must not leave the patient without drug treatment. A useful approach () is to increase the dose of a single AED to that which is maximally tolerated. If seizure control is not achieved, a second AED should be added and the dose should be raised gradually to mid-therapeutic range. Transient dose-related side effects are far less dangerous to the patient than an increase in seizure frequency or severity that could occur if the dose of the first drug is lowered before the dose of the second drug is increased. If there is at least some therapeutic response to the second drug, the dose can be escalated further until either seizure control is achieved or unacceptable side effects appear. If seizure control is achieved, the dose of the first drug then may be gradually tapered to determine if seizure control can be maintained with monotherapy. If there is no response, the procedure can be repeated with yet another AED. In this way a series of AEDs used as monotherapy and as dual therapy can be screened to identify the optimal drug or combination of drugs for a particular patient.Citation50 Although combination therapy has little additional benefit in most patients with new onset epilepsy,Citation17 it may have significant benefit in patients with refractory complex partial seizures. At least one-third of patients with new onset epilepsy and more than half with complex partial seizures will require more than one drug to achieve seizure control.
Figure 1 Algorithm for successive monotherapy trials in a patient with uncontrolled seizures. This approach allows testing the efficacy and tolerability of AEDs as monotherapy without subjecting the patient to the risk of increased seizures that could occur if an existing drug is tapered simultaneously with the uptitration of an additional drug. Dose-related side effects are in general much less dangerous than the risk of additional seizures and can be treated by lowering the dose of the offending drug.
The use of more than one AED in a patient creates the potential for pharmacokinetic drug–drug interactions, as does the use of AEDs in patients taking drugs for other indications. Most of the “classical” AEDs have the potential for either induction or inhibition of cytochrome P450 isozymes; fortunately many of the newer drugs do not. provides a list of currently available AEDs and their potential for drug–drug interactions. provides a list of drugs other than AEDs which may interact with AEDs. These potential interactions have to be considered whenever a patient is taking more than one drug, and may necessitate adjusting the dose of one AED if others are also being prescribed, or if the patient is taking other drugs as well as AEDs. Grapefruit inhibits CYP3A4, a P450 isozyme important in the metabolism of some of the benzodiazepines, CBZ, TGB, and ZNS.Citation54
Table 6 Potential drug–drug interactions of AEDs caused by microsomal P450 induction or inhibition
Table 7 Potential effects of some nonantiepileptic drugs on AED elimination via microsomal P450 enzyme
It is essential in the management of the patient with refractory complex partial seizures to push the dose(s) of the AED or combination of drugs as high as necessary to achieve seizure control without producing unacceptable side effects. Animal and human studies show that seizure control is correlated with AED concentrations.Citation50 The therapeutic range for all currently available AEDs is no more than an empirically-derived probability statement, with the low end being the serum concentration at which efficacy is seen in most but not all patients and the high end being the concentration at which toxicity is seen in most but not all patients. These therapeutic ranges have been determined empirically in a nonsystematic fashion. There has never been a formal prospective determination of the median effective dose or median toxic dose of any AED in human patients. Therefore, the effective dose and the toxic dose of an AED must be determined empirically for individual patients. The therapeutic range should only serve as a rough guide to dosing, but should never inhibit upward titration of the dose of an AED if the patient is tolerating the drug well and continues to have seizures.
The pharmacokinetic characteristics of the drug must be considered when increasing the dose of an AED. Most AEDs exhibit first-order kinetics within the therapeutic range, so that there is a linear relationship between dose and serum concentration (). However, three current AEDs (CBZ, VPA, GBP) exhibit a curvilinear relationship between dose and concentration such that there is a decrease in the concentration response as the dose is increased. On the other hand PHT exhibits Michaelis-Menten (saturation) elimination kinetics within the therapeutic range, and thus there is an increase in the concentration response as the dose is increased. Small increases in dose result in large increases in concentration. Because PHT is still used by many physicians (including non-neurologists) it is important to understand how to make adjustments of the dose to achieve maximum seizure control whilst avoiding toxic side effects. At the high end of the therapeutic range PHT doses should be adjusted by 10 mg increments to avoid excessive increases in serum concentration and consequent toxic side effects.Citation50 provides predicted increases in PHT serum concentration following 10 mg increases in the daily dose for low, mid, and high serum concentrations. 10 mg increments in the oral dose can be achieved for any dose of 180 mg and above by using a combination of the available 100 mg and 30 mg capsules.
Figure 2 Effect of dose on elimination kinetics of AEDs.
For most AEDs the relationship between AED dose and concentration is linear. However, valproate (because of saturation of serum protein-binding sites), gabapentin (because of saturation of L-amino acid transport enzymes in the intestine) and carbamazepine (because of autoinduction of its own metabolizing p450 isozymes) exhibit a nonlinear relationship between dose and serum concentration. The higher the dose, the less increase in concentration per unit dose is achieved. Phenytoin exhibits Michaelis-Menten (saturation) kinetics. Because of the saturation of the microsomal p450 isozymes responsible for phenytoin metabolism, the higher the dose the greater the increase in serum concentration per unit dose. Figure modified and updated from Kriel and Cloyd.Citation66
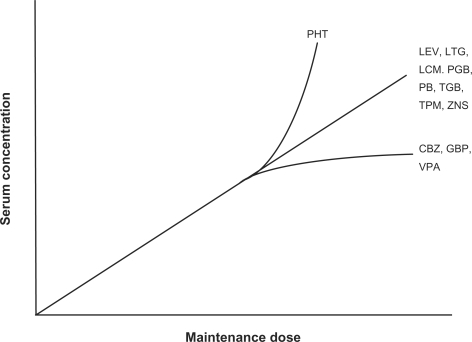
Table 8 Predicted increase in serum phenytoin concentration following a 10 mg increase in daily doseCitation50
Therapeutic drug monitoring can be useful in the management of refractory complex partial seizures. It is particulary useful in helping to determine which drug is causing adverse effects if a patient is taking two or more AEDs. It may also be useful in some circumstances to verify compliance. Finally, serum concentrations are very useful for fine-tuning PHT dosing, especially in the intensive care setting where a patient may be receiving a multitude of drugs, but also in the outpatient setting, as described above. Peak concentrations are most useful in assessing toxicity; trough levels are most helpful in assessing compliance. Serum concentrations are readily and rapidly available for most of the classical AEDs (PB, PHT, CBZ, VPA) but not as easily obtainable for most of the newer AEDs. Furthermore, therapeutic ranges are not nearly as well established for the newer AEDs, so therapeutic monitoring is less useful in the management of these drugs.
Sometimes seizure control can be achieved by changing the timing of AED dosing. As a generalization, an AED should not be given less often than at least once a half-life to avoid excessive fluctuations in peak and trough concentrations. For rapidly absorbed drugs (those without extended-release formulations) the peak concentration (Tmax) occurs about 1.0 to 1.5 hours after oral administration. If the patient experiences post-dose toxicity, this can be reduced by using smaller doses more frequently throughout the day. However, if the drug has a long-half life, it may be possible to give the entire dose immediately before bedtime, so that the peak concentration occurs when the patient is in slow-wave sleep. Drugs that cause insomnia (felbamate and sometimes LTG), however, are best taken early in the day. It is clear that compliance is improved by once or twice a day dosing, and is reduced if AED dosing is more frequent,Citation55 and this must also be considered in any dosing strategy.
Surgical strategies for the management of refractory complex partial seizures will be discussed below. However, if surgery is not an option, it is important to continue to try to achieve seizure control with AEDs. Do not give up. There are now 16 AEDs available in the US for treatment of refractory complex partial seizures. This means there are 120 potential two-drug combinations and many more three drug combinations. Perseverance alone can sometimes lead to successful control of refractory complex partial seizures. Luciano and ShorvonCitation56 recently reported the result of 265 drug additions in 155 adult patients with chronic pharmacoresistant epilepsy. Twenty-eight percent eventually became seizure-free, but only 17% stopped having seizures after the addition of only one AED. The other 11% required trials of two, three, or more additional AEDs to achieve seizure freedom. Similar results have been reported by Callaghan et al.Citation57
Surgical strategies
Surgical intervention has to be a consideration in the management of refractory complex partial seizures. Currently available interventions include resection of the seizure focus, multiple subpial transection when the seizure focus is in eloquent cortex, destruction of the seizure focus by gamma knife, and implantation of a VNS. Deep brain stimulation and stimulation of the seizure focus are under study, but these are not yet approved interventions.
Patients should be considered for resective surgery when the seizure focus appears to be well localized and has a solo focus. This is best predicted by the seizure semiology at onset, as discussed above. The ideal candidate for resective surgery is the patient with refractory complex partial seizures whose semiology suggests mesial temporal onset, who has failed an adequate trial of at least two or three AEDs, and who exhibits mesial temporal sclerosis on MRI. In such patients, success rates of 70%–90% for selective amygdalo-hippocampectomy or temporal lobectomy can be expected in the hands of an experienced surgeon. Téllez-Zentano et alCitation58 recently reviewed the long-term outcome of surgical procedures for epilepsy. Overall the median proportion of long-term seizure-free patients was 66% for temporal lobe resections, 46% for occipital and parietal resections, and 27% for frontal lobe resections. Multiple subpial transections only resulted in long-term seizure freedom in 16%. Successful destruction of the seizure focus with gamma radiation in patients with mesial temporal epilepsy has been reported in several recent series, with long-term success rates comparable with those for resective surgery. However, the mean time to seizure control has been 12 months, in contrast with immediate seizure freedom following open surgery.Citation59–Citation61
When medical treatment options have been exhausted and resective surgery is not possible (usually because of bilateral mesial temporal-independent seizure foci), implantation of a VNS should be considered in the patient with medically refractory complex partial seizures. Overall response rates of 35% to 45% have been reported,Citation62–Citation64 but few patients become completely seizure-free, and almost all remain on AEDs. Nonetheless, a VNS can be of great benefit to some patients with refractory complex partial seizures. High stimulation parameters are more effective than low stimulation parameters, but result in more adverse reactions.Citation65
Conclusion
Epilepsy is the third most common neurologic disorder in incidence, but the second most common neurologic disorder in prevalence. Because it affects all ages and because of the social stigma attached to epilepsy in many cultures, it has a disproportionately high impact on the quality of life of the patients it affects. Refractory complex partial seizures affect at least 7.5 million up to perhaps as many as 10 million people worldwide. Many advances have been made in the management of complex partial seizures, but one-third of afflicted patients continue to have uncontrolled seizures. Fortunately, there are a number of strategies that can improve control of such seizures, as discussed above, and a number of new approaches to management that are likely to come to fruition over the next several decades and result in significant improvement in the management of complex partial seizures.
Disclosures
Dr Treiman has, at various times, received research support from, served as a consultant for, and/or served on a speakers’ bureau for Abbott, Astra, Athena, Carter-Wallace, Cyberonics, Dainippon, Eisai, Élan, GlaxoSmithKline, Ikano, Janssen, Johnson and Johnson, Lundbeck, Merrell Dow, Novartis, Organon, Ovation, Ortho-McNeil, Parke Davis, Pfizer, Roche, Sanofi, Syntex, UCB, Valeant, and Wyeth. The author is not aware of any conflicts of interest in this work.
References
- World Health OrganizationEpilepsy: Aetiology, epidemiology and prognosis Available at: www.who.int/mediacentre/factsheets/fs165/en/.2001
- BanerjeePNFilippiDAllenHWThe descriptive epidemiology of epilepsy – a reviewEpilepsy Res200985314519369037
- HauserWAAnnegersJFKurlandLTIncidence of epilepsy and unprovoked seizures in Rochester, Minnesota: 1935–1984Epilepsia1993344534688504780
- SidenvallRForsgrenLHeijbelJPrevalence and characteristics of epilepsy in children in northern SwedenSeizure199651391468795130
- ForsgrenLBuchtGErikssonSBergmarkLIncidence and clinical characterization of unprovoked seizures in adults: A prospective population-based studyEpilepsia1996372242298598179
- JallonPGoumazMHaenggeliCMorabiaAIncidence of first epileptic seizures in the canton of Geneva, SwitzerlandEpilepsia1997385475529184600
- OlafssonEHauserWALudvigssonPGudmundssonGIncidence of epilepsy in rural Iceland: a population-based studyEpilepsia1996379519558822693
- OlafssonELudvigssonPGudmundssonGHesdorfferDKjartanssonOHauserWAIncidence of unprovoked seizures and epilepsy in Iceland and assessment of the epilepsy syndrome classification: A prospective studyLancet Neurol2005462763416168931
- FarrellMADeRosaMJCurranJGNeuropathologic findings in cortical resections (including hemispherectomies) performed for the treatment of intractable childhood epilepsyActa Neuropathol1992832462591557956
- KuznieckyRMurroAKingDMagnetic resonance imaging in childhood intractable partial epilepsies: Pathologic correlationsNeurology1993436816878469322
- WyllieEComairYGKotagalPBulacioJBingamanWRuggieriPSeizure outcome after epilepsy surgery in children and adolescentsAnn Neurol1998447407489818929
- FraterJLPraysonRAMorrisHHIIIBingamanWESurgical pathologic findings of extratemporal-based intractable epilepsy: A study of 133 consecutive resectionsArch Pathol Lab Med200012454554910747311
- PasquierBPeoc’hMFabre-BocquentinBSurgical pathology of drug-resistant partial epilepsy. A 10-year-experience with a series of 327 consecutive resectionsEpileptic Disord200249911912105073
- AlvingJClassification of the epilepsies. An investigation of 1,508 consecutive adult patientsActa Neurol Scan197858205212
- BanerjeePNHauserWAIncidence and prevalenceEngelJJrPedleyTAEpilepsy: A Comprehensive Textbook2nd edPhiladelphia,PAWolters Kluwer Lippincott Williams Wilkins20084556
- BergATShinnarSThe risk of seizure recurrence following a first unprovoked seizure: A quantitative reviewNeurology1991419659722067659
- KwanPBrodieMJEarly identification of refractory epilepsyN Engl J Med200034231431910660394
- TallisRHallGCraigIDeanAHow common are epileptic seizures in old ageAge Ageing1991204424481776595
- HauserWASeizure disorders: The changes with ageEpilepsia199233Suppl 4S6S141425495
- HopkinsAShorvonSDefinitions and epidemiology of epilepsyHopkinsAShorvonSCascinoGEpilepsy2nd edLondonChapman & Hall Medical2005124
- CarpioAHauserWAEpilepsy in the developing worldCurr Neurol Neurosci Rep2009931932619515285
- SanderJWHartYMJohnsonALShorvonSDNational General Practice Study of Epilepsy: Newly diagnosed epileptic seizures in a general populationLancet1990336126712711978113
- LoiseauJLoiseauPGuyotMDucheBDartiguesJFAubletBSurvey of seizure disorders in the French southwest. I. Incidence of epileptic syndromesEpilepsia1990313913962369875
- LoiseauJLoiseauPDucheBGuyotMDartiguesJFAubletBA survey of epileptic disorders in southwest France: seizures in elderly patientsAnn Neurol1990272322372327734
- SalazarAMJabbariBVanceSCGrafmanJAminDDillonJDEpilepsy after penetrating head injury. I. Clinical correlates: A report of the Vietnam Head Injury StudyNeurology198535140614143929158
- JallonPLoiseauPLoiseauJNewly diagnosed unprovoked epileptic seizures: Presentation at diagnosis in CAROLE study. Coordination Active du Reseau Observatoire Longitudinal de l’ EpilepsieEpilepsia20014246447511440341
- WilliamsonPDEngelJJrAnatomic classification of focal epilepsiesEngelJJrPedleyTAEpilepsy: A Comprehensive Textbook2nd edPhiladelphia, PAWolters Kluwer Lippincott Williams & Wilkins200824652477
- HauserWAHesdorfferDCEpilepsy Frequency, Causes and Consequences1st edNew York, NYDemos1990
- LoddenkemperTKotagalPLateralizing signs during seizures in focal epilepsyEpilepsy Behav2005711715975856
- MaillardLVignalJPGavaretMSemiologic and electrophysiologic correlations in temporal lobe seizure subtypesEpilepsia2004451590159915571517
- Commission on Classification and Terminology of the International League Against EpilepsyProposal for revised classification of epilepsies and epileptic syndromesEpilepsia1989303893992502382
- RafalRDOculomotor functions of the parietal lobe: Effects of chronic lesions in humansCortex20064273073916909633
- DeaconCWiebeSBlumeWTMcLachlanRSYoungGBMatijevicSSeizure identification by clinical description in temporal lobe epilepsy: How accurate are weNeurology2003611686168914694030
- ChungSSGerberPKirlinKAIctal eye closure is a reliable indicator for psychogenic nonepileptic seizuresNeurology2006661730173116769949
- SalinskyMKanterRDasheiffRMEffectiveness of multiple EEGs in supporting the diagnosis of epilepsy: An operational curveEpilepsia1987283313343622408
- DevinskyOKelleyKPorterRJTheodoreWHClinical and electroencephalographic features of simple partial seizuresNeurology198838134713523137487
- BareMABurnstineTHFisherRSLesserRPElectroencephalographic changes during simple partial seizuresEpilepsia1994357157208082613
- SirvenJISperlingMRFrenchJAO’ConnorMJSignificance of simple partial seizures in temporal lobe epilepsyEpilepsia1996374504548617173
- CooperRWinterALCrowHJWalterWGComparison of subcortical, cortical and scalp activity using chronic indwelling electrodes in manElectroencephalogr Clin Neurophysiol19651821722814255050
- TaoJXRayAHawes-EbersoleSEbersoleJSIntracranial EEG substrates of scalp EEG interictal spikesEpilepsia20054666967615857432
- TaoJXBaldwinMHawes-EbersoleSEbersoleJSCortical substrates of scalp EEG epileptiform dischargesJ Clin Neurophysiol2007249610017414965
- O’BrienTJSoELMullanBPSubtraction SPECT co-registered to MRI improves postictal SPECT localization of seizure fociNeurology1999521371469921861
- O’BrienTJSoELMullanBPSubtraction peri-ictal SPECT is predictive of extratemporal epilepsy surgery outcomeNeurology2000551668167711113221
- MattsonRHCramerJACollinsJFComparison of carbamazepine, phenobarbital, phenytoin, and primidone in partial and secondarily generalized tonic-clonic seizuresN Engl J Med19853131451513925335
- MattsonRHCramerJACollinsJFA comparison of valproate with carbamazepine for the treatment of complex partial seizures and secondarily generalized tonic-clonic seizures in adults. The Department of Veterans Affairs Epilepsy Cooperative Study No. 264 GroupN Engl J Med199210;327117657711298221
- MarsonAGAl-KharusiAMAlwaidhMThe SANAD study of effectiveness of carbamazepine, gabapentin, lamotrigine, oxcarbazepine, or topiramate for treatment of partial epilepsy: An unblinded randomised controlled trialLancet20073691000101517382827
- FrenchJAKannerAMBautistaJEfficacy and tolerability of the new antiepileptic drugs II: Treatment of refractory epilepsy: Report of the Therapeutics and Technology Assessment Subcommittee and Quality Standards Subcommittee of the American Academy of Neurology and the American Epilepsy SocietyNeurology2004621261127315111660
- WilbyJKainthAHawkinsNClinical effectiveness, tolerability and cost-effectiveness of newer drugs for epilepsy in adults: A systematic review and economic evaluationHealth Technol Assess200591157iiiiv15842952
- SchmidtDReduction of two-drug therapy in intractable epilepsyEpilepsia1983243683766406214
- TreimanDMTreatment strategiesWillmoreLJGeneralized tonic-clonic seizures: Identification, classification, and treatmentDeerfield, ILDiscovery International19955469
- SimonsenNZander-OlsenPKühlVLundMWendelboeJA comparative controlled study between carbamazepine and diphenylhydantoin in psychomotor epilepsyEpilepsia197617169176780103
- TroupinAOjemannLMHalpernLCarbamazepine – a double-blind comparison with phenytoinNeurology197727511519405624
- KosteljanetzMChristiansenJMouritzenACarbamazepine vs phenytoin. A controlled clinical trial in focal motor and generalized epilepsyArch Neurol1979362224105689
- LevyRHMatherGGMetabolic enzymes and antiepileptic drug interactionsAdv Neurol19987649559408463
- CramerJVachonLDesforgesCSussmanNMDose frequency and dose interval compliance with multiple antiepileptic medications during a controlled clinical trialEpilepsia199536111111177588455
- LucianoALShorvonSDResults of treatment changes in patients with apparently drug-resistant chronic epilepsyAnn Neurol20076237538117253624
- CallaghanBCAnandKHesdorfferDHauserWAFrenchJALikelihood of seizure remission in an adult population with refractory epilepsyAnn Neurol20076238238917880009
- Tellez-ZentenoJFDharRWiebeSLong-term seizure outcomes following epilepsy surgery: A systematic review and meta-analysisBrain20051281188119815758038
- RegisJReyMBartolomeiFGamma knife surgery in mesial temporal lobe epilepsy: A prospective multicenter studyEpilepsia20044550451515101832
- BartolomeiFHayashiMTamuraMLong-term efficacy of gamma knife radiosurgery in mesial temporal lobe epilepsyNeurology2008701658166318401026
- BarbaroNMQuiggMBroshekDKA multicenter, prospective pilot study of gamma knife radiosurgery for mesial temporal lobe epilepsy: Seizure response, adverse events, and verbal memoryAnn Neurol20096516717519243009
- Ben-MenachemEManon-EspaillatRRistanovicRVagus nerve stimulation for treatment of partial seizures: 1. A controlled study of effect on seizuresEpilepsia1994356166268026408
- HandforthADeGiorgioCMSchachterSCVagus nerve stimulation therapy for partial-onset seizures: A randomized active-control trialNeurology19985148559674777
- DeGiorgioCMSchachterSCHandforthAProspective long-term study of vagus nerve stimulation for the treatment of refractory seizuresEpilepsia2000411195120010999559
- PriviteraMDWeltyTEFickerDMWelgeJVagus nerve stimulation for partial seizuresCochrane Database Syst Rev2002CD00289611869641
- KrielRLCloydJCAntiepilepsy drug therapy in children: Pharma-cokinetcs, adverse effects, and monitoringSwaimanKFPediatric Neurology: Principles and PracticeSt. Louis, MOMosby1994583609
- RambeckBBoenigkHEDunlopAMullenPWWadsworthJRichensAPredicting phenytoin dose – A revised nomogramTher Drug Monit19791325333555577