Abstract
Depression and anxiety occur at high rates among patients suffering an acute coronary syndrome (ACS). Both depressive symptoms and anxiety appear to adversely affect in-hospital and long term cardiac outcomes of post-ACS patients, independent of traditional risk factors. Despite their high prevalence and serious impact, mood and anxiety symptoms go unrecognized and untreated in most ACS patients and such symptoms (rather than being transient reactions to ACS) persist for months and beyond. The mechanisms by which depression and anxiety are linked to these negative medical outcomes are likely a combination of the effects of these conditions on inflammation, catecholamines, heart rate variability, and endothelial function, along with effects on health-promoting behavior. Fortunately, standard treatments for these disorders appear to be safe, well-tolerated and efficacious in this population; indeed, selective serotonin reuptake inhibitors may actually improve cardiac outcomes. Future research goals include gaining a better understanding of the combined effects of depression and anxiety, as well as definitive prospective studies of the impact of treatment on cardiac outcomes. Clinically, protocols that allow for efficient and systematic screening, evaluation, and treatment for depression and anxiety in cardiac patients are critical to help patients avoid the devastating effects of these illnesses on quality of life and cardiac health.
Introduction
Depression and anxiety are common among patients who have an acute coronary syndrome (ACS) or other major cardiovascular event. Despite their frequency, these psychiatric syndromes often go unrecognized and can persist for months to years, substantially impacting quality of life.Citation1–Citation4 Furthermore, both depression and anxiety have been independently associated with negative cardiac outcomes in patients with acute cardiac events and, indeed, across the spectrum of cardiac disease.Citation5–Citation8 Fortunately, safe and effective treatments exist for depression and anxiety disorders in these patients,Citation9–Citation11 and systematic evaluation of cardiac patients for psychiatric symptoms has the potential to substantially improve outcomes.Citation12
In this review, we will examine the phenomenology of ACS and outline the prevalence and medical impact of depression and anxiety in patients with ACS and other forms of cardiovascular illness. We will discuss the mechanisms by which mood and anxiety symptoms may impair cardiac prognosis and will describe treatment considerations in this population. In the literature, depression in cardiac patients has been defined in several different ways, with some studies focusing on the formal syndrome of major depression and others focusing on elevated depressive symptoms on self-report measures. Similarly, though most studies of anxiety in heart disease have used self-report measures, there is increasing study of specific anxiety disorders among patients with cardiac illness. In this article, we will review the literature on both self-reported symptoms of depression and anxiety and the existing data on specific depressive and anxiety disorders.
Acute coronary syndromes: an overview
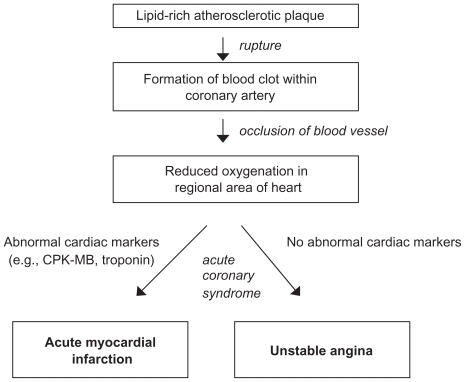
Cardiovascular disease is the number one cause of death in the world.Citation13 Among patients with cardiovascular disease, unstable angina (UA) and myocardial infarction (MI) are severe, life-threatening conditions that represent sudden myocardial ischemia (loss of blood flow to the heart muscle, with loss of oxygen to cardiac cells). Both UA and MI are generally captured under the umbrella term ACS; this term represents a wide clinical spectrum of myocardial ischemia severity, ranging from UA (by definition, ischemia without myocardial injury) to MI, representing ischemia with resultant cell death ().
Figure 1 Pathophysiology of acute coronary syndrome.
Each year, more than one million Americans suffer an ACS.Citation14 Risk factors for having cardiac disease, and ultimately an ACS, include gender (men are slightly more likely to have cardiac illness), age (men over 45 years and women over 55 years), family history of cardiovascular disease, and modifiable risk factors.Citation14 ACS is more common in men (eg, 58% of all ACS events occurred in men in 2005), though ACS prevalence in women approaches that of men in older age.Citation14 Modifiable risk factors for an ACS include hypertension, hyperlipidemia, diabetes, sedentary lifestyle, and smoking. In addition to these risk factors, it has become increasingly clear that psychological factors, particularly depression and anxiety, may play an important and independent role in the development and propagation of cardiac disease. Further, some have begun to suggest that depression, in particular, be included among the list of classic cardiac risk factors given the strength of evidence linking this illness to cardiac outcomes.Citation15,Citation16
Pathophysiologically, the most common cause for an ACS is the disruption of a previously nonsevere atherosclerotic plaque. Indeed, it is now recognized that the great majority of coronary atherosclerotic plaques that lead to ACS are typically relatively nonobstructive prior to the ACS, with a predisposition to rupture that is determined more by their intrinsic biology, than degree of protrusion into the coronary lumen.Citation17
The characteristic “vulnerable” atherosclerotic plaque is one that has a rich lipid core (typically filled with necrotic, highly inflammatory debris), a large number of inflammatory cells (such as macrophages), a paucity of fibroblasts, and a relatively thin fibrous cap separating the plaque contents from the blood.Citation17 In the context of a trigger, biological or physiological, the thin fibrous cap may rupture, leading to a cascade of events ranging from an asymptomatic cardiac event to sudden cardiac death.
In the context of plaque rupture, a series of inflammatory and platelet-related events lead to the formation of a thrombus, a blood clot, on the surface of the plaque, which may lead to occlusion of the coronary artery.Citation18 Factors that determine this process include both the size and severity of the plaque rupture, as well as the vigor of the biological response to plaque rupture, including severity of platelet response and coagulation activation.
If the coronary thrombosis is significant enough, blood flow to that area of the heart is either reduced or blocked and myocardial ischemia results. Moreover, a substantial degree of myocardial ischemia in the context of ACS is not only due to occlusion of the epicardial coronary vessel, but also to downstream embolization of platelet-rich debris to the resistance microvasculature.Citation19 In the setting of acute myocardial ischemia, classic signs and symptoms in men that may follow include chest heaviness that may radiate to the jaw or arm, diaphoresis, shortness of breath, and lightheadedness. Such symptoms may be less common in certain important populations, such as women and the elderly.
Diagnostically, patients with suspected ACS are evaluated with 12-lead electrocardiography (ECG). Diagnostic changes on ECG include depression or elevation of the ST-segments; the presence of either of these findings identifies a patient with severe coronary ischemia (ST-depression) or frank myocardial injury (ST-elevation). If the ACS leads to cardiac cell death, typically detected using sensitive tests for myocardial cell death (eg, serum troponin) then, by definition, it is an MI. In addition to being useful for diagnosis of MI, serum troponins also predict the risk for recurrent MI, as well as death.Citation20 Accordingly, troponin elevation in the setting of an ACS identifies a population of patients that are typically managed in a more aggressive fashion clinically.
Typical acute treatments for ACS include oxygen, aspirin, beta-adrenergic blocking agents, high dose lipid-lowering agents, anticoagulants such as heparin, as well as nitroglycerin, and/or morphine sulfate for ongoing symptoms. More aggressive antithrombotic drugs such as clopidogrel (an oral antiplatelet agent) and/or platelet glycoprotein antagonists are widely used in this setting as well.
Goals of acute treatment are to eradicate symptoms, normalize electrocardiogram findings, and prevent complications. In addition to medication treatment, patients (especially those suffering a myocardial infarction with ST-segment elevation seen on the ECG) will undergo reperfusion treatment. Most commonly, the patient will undergo urgent/emergent cardiac catheterization with coronary angiography, to identify areas of stenosis within the coronary artery system. These narrowed areas may then be dilated using balloon angioplasty, most commonly with adjunctive placement of a coronary stent. In the absence of available catheterization facilities, reperfusion can also be achieved using fibrinolytic agents, medications that may dissolve the intracoronary thrombosis, although the success of fibrinolysis is significantly lower than angioplasty and stenting.Citation21
Once the symptoms of ACS have acutely subsided, important medication interventions to reduce risk of future complications and recurrence include the use of a wide array of medications, including beta-blockers, angiotensin-converting enzyme inhibitors, cholesterol-lowering agents, and antiplatelet agents (aspirin, clopidogrel). Lifestyle and risk factor modification is also essential.
Depression and anxiety in patients with acute cardiac disease
Among patients with cardiac disease, depression is common, persistent, and under recognized. The syndrome of major depression () is present in approximately 15% of patients with cardiac disease,Citation22 including those suffering ACS.Citation23,Citation24 Such a rate is substantially higher than that seen in the general population (4% to 5%)Citation25 or primary care patients (8% to 10%).Citation26 Though some cardiac illnesses may have associated impairments of appetite, concentration, sleep, and energy, true depression (with persistent depressed mood or anhedonia) is not a normal consequence of cardiac disease.
Table 1 Criteria for a major depressive episode
Rather than being a transient reaction to having cardiac disease, depression in cardiac patients is often both chronic and recurrent.Citation27,Citation28 For example, the large Sertraline Antidepressant Heart Attack Randomized Trial (SADHART) trialCitation27 found that, among ACS patients who entered the hospital with major depression, 94% of such patients had been depressed for over one month, 61% had been depressed for over six months and more than half had a prior major depressive episode. Furthermore, depressive symptoms are not transient after myocardial infarction, but instead persist if untreated. Two studies have found that depressive symptoms are essentially stable over the year following MI, with little reduction of symptoms over this period in untreated patients.Citation3,Citation29 Despite the frequency and persistence of depression in this cohort, it often goes unrecognized and untreated in the vast majority of patients suffering ACS. A pair of studies on acute cardiac units found that front-line clinicians were unable to identify depression in their post-MI patients,Citation2,Citation4 and rates of depression treatment in this setting have been less than 15%.Citation30,Citation31
Anxiety is also common among patients with acute cardiovascular disease. Elevated levels of self-reported anxiety are present in 20% to 50% of patients following acute MI,Citation1,Citation32–Citation34 with up to one quarter experiencing symptoms of anxiety at least as intense as the average inpatient on a psychiatric unit.Citation35 Anxiety often persists after such cardiac events and, among patients with anxiety shortly after ACS, many have clinically significant anxiety up to 2 years later.Citation1,Citation36,Citation37 The finding that patients with stable coronary heart disease have higher levels of anxiety than the general population, with prevalence rates ranging from 16% to 42%, is further evidence of the pervasive nature of anxiety in coronary heart disease patients.Citation6,Citation38–Citation40
In addition to elevated levels of overall anxiety as measured on anxiety scales, formal anxiety disorders are more common in cardiac patients than in the general population. One cross-sectional study utilizing semi-structured diagnostic interviews found that 36% of patients met criteria for an anxiety disorder at the time of evaluation and 45% had a lifetime history of an anxiety disorder.Citation41 Generalized anxiety disorder is present in up to 24% of patients with cardiac disease,Citation6,Citation41,Citation42 and panic disorder also occurs at substantially elevated rates among patients with cardiovascular disease, with 5% to 50% of cardiac patients having active panic disorder.Citation41,Citation43–Citation45
As with depression, clinically significant anxiety in post-ACS patients often goes unrecognized and untreated by front-line clinicians on cardiac inpatient units.Citation2 Follow-up of patients with these symptoms is equally limited; in one study, roughly one third of patients who had elevated anxiety following an ACS were questioned about these symptoms by their medical clinicians over the next year.Citation1
Links between depression, anxiety, and negative cardiac outcomes among patients suffering acute ischemic events
There is substantial evidence to suggest that depression is independently associated with negative cardiac outcomes across the spectrum of cardiac disease. Depression in healthy persons without cardiac disease has been associated with the development of coronary artery disease. The Johns Hopkins Precursor study followed male medical students for 40 years and found depression to independently predict the subsequent development of cardiac disease and MI.Citation46 Since that time, there have been numerous studies of healthy men and women linking depression to the onset of cardiac illness; a meta-analysis of this population found that depression was associated with a 60% increase in cardiac disease.Citation47
Among patients with existing cardiac disease, depression has been associated with progression of the illness. Patients found to have depression when diagnosed with coronary artery disease at cardiac catheterization are more likely to have acute cardiovascular/ischemic events than nondepressed patientsCitation48 and hypertensive patients with depression more likely to die of their cardiac disease.Citation49
Finally, and most strikingly, patients with depression in the setting of acute myocardial ischemia (ACS) have substantially impaired medical/cardiac outcomes compared to those without depression. Specifically, post-MI depression is associated with poor health-related quality of life, recurrent cardiac events, and mortality, independent of other medical and demographic characteristics.Citation24,Citation50,Citation51 These links appear to exist either when depression is measured by self-report or by a structured clinical interview.Citation5 A 2004 meta-analysis of 22 studies that included over 6000 patients found that the uncorrected relative risks of recurrent cardiac events and cardiac mortality in the year following MI were 2.0 and 2.6 in patients with depression in the post-MI period compared to those without depression.Citation24
Depressive symptoms in the post-ACS period can have far reaching consequences. A recent longitudinal study of post-ACS depression found that baseline depression severity a few weeks after ACS was a strong and independent risk factor for cardiac mortality approximately 7 years after the index event.Citation52 Findings from this study and others indicate that ACS patients whose depression is resistant to standard treatments appear to be at highest risk of suffering adverse cardiac outcomes.Citation52–Citation54 It is unclear whether this is because the depression persists or whether this is a separate subtype of depression.
In addition to the long term effects of post-ACS depression, it appears that depression may also have immediate detrimental effects among those admitted to the hospital with acute myocardial ischemia. In this regard, at least two studies have found that MI patients who enter the hospital with an ongoing major depressive episode are more likely to have an in-hospital cardiac complication.Citation31,Citation55 Though most studies of ACS patients have primarily evaluated depression after MI, depression in the setting of UA has also been specifically associated with cardiac morbidity and mortality.Citation23
Anxiety also appears to be linked to negative cardiac outcomes across the spectrum of cardiac disease. Persons with elevated anxiety have higher rates of subsequent development of coronary heart disease than nonanxious persons, independent of other risk factors. Indeed, anxiety may be more strongly associated with the onset of cardiac disease than depression.Citation8 In particular, worry is a component of anxiety that appears to be especially associated with cardiac disease.Citation56,Citation57 Among patients with acute cardiovascular disease, the population of patients most vulnerable to catastrophic cardiac events and complications, several studies have found that elevated anxiety after MI has been independently associated with in-hospital cardiac complications. Citation58–Citation60 Furthermore, though prior studies found no such association,Citation34,Citation61 multiple recent studies have also found that anxiety following MI is associated with longer-term cardiac complications and mortality. Citation1,Citation6,Citation62 These studies include a recent well-designed study by Frasure-Smith and colleaguesCitation6 finding that generalized anxiety disorder (GAD) in the setting of coronary artery disease was associated with 2 year major adverse cardiac events, independent of other patient characteristics and a study by Strik and coworkersCitation62 finding that post-MI anxiety symptoms, independent of depression and medical characteristics, predicted recurrent cardiac events.
Do depression and anxiety have additive effects on cardiovascular outcomes among patients with myocardial ischemic events? There has been a relative paucity of studies in this area and thus far the results have been mixed. A recent analysis of data from the Women’s Ischemia Syndrome Evaluation (WISE) study found that depressed women with higher levels of anxiety were more likely to have adverse cardiovascular events than depressed women with low anxiety.Citation63 In contrast, the previously mentioned study by Frasure-Smith and colleaguesCitation6 found that both major depression and generalized anxiety disorder were associated with cardiac events, but that patients with both disorders were not at further elevated risk.
In sum, depression and anxiety appear to be independently associated with adverse cardiovascular outcomes among patients with ischemic heart disease; depression, in particular, appears to be clearly associated with cardiac events in both the short and long term.
Potential mechanisms linking depression/anxiety and myocardial ischemia
Given the substantial literature linking depression and anxiety with adverse cardiac events, there has been an increasing focus on determining the mechanisms by which these links may occur (). Overall, there are two mechanistic categories that likely contribute to these associations: physiologic effects and behavioral effects. We will first discuss physiologic effects.
Figure 2 Putative mechanisms linking depression/anxiety and cardiac outcomes in acute coronary syndrome (ACS) patients.
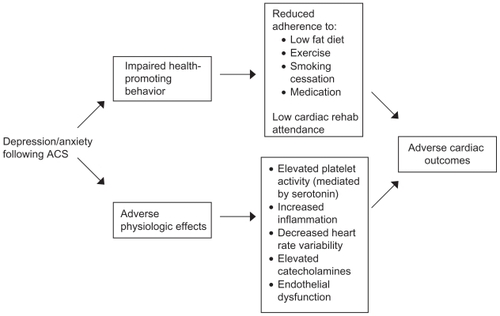
Platelet activity and aggregation
Platelet activity and aggregation are key components of acute myocardial ischemia and evidence of increased platelet activity and aggregation has been found in patients with depression.Citation64–Citation66 The connection between depression and platelet hyper-reactivity (and subsequent aggregation) may be mediated by serotonin. Serotonin is found both in the whole blood and in platelets and plays an essential role in platelet activation. When serotonin binds to 5-hydroxytryptamine-2 (5HT-2) receptors on platelets, it causes the release of procoagulant factors stored in the platelets and enhances platelet aggregation, leading to clot formation. In normal coronary arteries, thrombus formation and ischemia are prevented by serotonin’s stimulation of the endothelium to release nitric oxide, which results in vasodilation in the area surrounding the clot. In atherosclerotic arteries, however, damage to the endothelium prevents the release of nitric oxide with the result that serotonin leads to vasoconstriction.Citation67 Given this, it is not surprising that elevated serotonin blood levels have been associated with coronary artery disease and cardiac events.Citation68
The serotonergic system has also been implicated in the pathogenesis of major depression. Although evidence is not conclusive, several researchers have found that patients with depression (with and without heart disease) have abnormalities in whole blood and platelet serotonin levels,Citation69,Citation70 increased platelet serotonin receptor concentrations,Citation71,Citation72 and abnormally low platelet serotonin transporter levels,Citation73 all of which could lead to serotonin-linked platelet dysfunction and could provide a explanation for how depression could lead to adverse cardiovascular outcomes.
Less is known about the effects of anxiety on platelet aggregation and activity, but the available evidence suggests that serotonin may also mediate changes in platelets in anxious patients. Abnormalities in the serotonergic system have been implicated in the pathogenesis of anxiety disorders and patients with phobic anxiety have been found to have abnormalities in the coagulation and fibrinolytic system leading to a hypercoagulable state.Citation74 Furthermore, abnormalities in serotonin blood levels,Citation75 platelet serotonin transporters,Citation76 and platelet intracellular calcium levels in response to stimulationCitation77 (increasing sensitivity to procoagulant factors) have been reported in patients with specific anxiety disorders. In addition to these mechanisms, acute stress has also been associated with platelet hyperactivity, increased blood viscosity, and hemoconcentration, Citation78,Citation79 potentially increasing the risk for thrombosis and other cardiovascular complications mediated through platelet hyperactivity and increased blood viscosity.
Inflammation
Inflammation appears to play a key role in the pathogenesis of acute ischemic events. Inflammatory cytokines such as tumor necrosis factor-alpha (TNF-α) and interleukin-1 (IL-1) are actively involved in the pathogenesis of atherosclerosis, Citation80,Citation81 and elevations of inflammatory markers, especially C-reactive protein (CRP), are independently associated with mortality following ACS.Citation80,Citation82 Depression is similarly associated with elevations of other inflammatory markers (eg, IL-1, IL-6, and TNF-α),Citation83 and this proinflammatory state in depression may lead to development or propagation of myocardial ischemic events.
As with platelet activation, there is less data on the links between anxiety and inflammation, but levels of circulating inflammatory markers are abnormal in persons with elevated anxiety. A large study of healthy adults found elevated levels of anxiety to be independently associated with abnormalities of multiple inflammatory markers, even after adjustment for multiple other factors.Citation84 With regard to specific anxiety disorders, post-traumatic stress disorder (PTSD) has been associated with abnormal levels of inflammatory markers (eg, IL-1, IL-6, TNF-α, and CRP) in both noncardiac and post-MI patients.Citation85,Citation86 In addition, women with diabetes who have phobic anxiety have higher levels of inflammatory cytokines,Citation87 and generalized anxiety disorder is associated with elevated levels of CRP among patients with cardiac disease.Citation88
Heart rate variability
Heart rate variability (HRV), a measure of the beat-to-beat variability of the heart, involves a complex interplay between the sympathetic and parasympathetic nervous systems and their impact on the cardiac pacemaker. Decreased HRV in post-MI patients has been consistently associated with mortality,Citation89 thought to be due in part to elevated risk of arrhythmia.Citation90 Several studies have found clinical depression to be associated with diminished HRV,Citation91 including studies of depressed cardiac patients,Citation92,Citation93 and given the relative risk of arrhythmic events among post-MI patients, depression may substantially increase risk of cardiac arrhythmic events in this vulnerable population. Likewise, anxiety has been associated with decreased HRVCitation94 and both depression and anxiety in patients with implantable defibrillators has been linked to low HRV.Citation95
Elevated catecholamines
Hyperactivity of the sympathetic nervous system leads to increased release of catecholamines in the periphery. This in turn leads to vasoconstriction, blood pressure elevation, platelet activation, and arrhythmia, all of which can have detrimental effects on cardiovascular stability. Depression is associated with sympathetic nervous system dysregulation, Citation96,Citation97 and, similarly, acute anxiety and chronic worry lead to sympathetic nervous system hyperactivity and autonomic dysregulation, Citation98–Citation100 providing another potential causative link between these disorders and adverse cardiac events.
Endothelial dysfunction
The endothelium is the critical, active layer of tissue between circulating blood and the vasculature and is a key regulator of vascular homeostasis. Endothelial dysfunction has a substantial impact on cardiovascular health. Indeed, endothelial dysfunction in patients with cardiovascular illness has been independently associated with increased rates of cardiac mortality.Citation101–Citation103 It is increasingly understood that depression is associated with abnormal function of the endothelium, with depressed patients having more abnormalities on specialized testing of the endothelium than patients who are nondepressed, independent of other factors.Citation104,Citation105 Endothelial dysfunction also has been reported in patients with elevated levels of anxiety, particularly in the elderly.Citation106–Citation108 Abnormal vascular function in the setting of depression or anxiety certainly could lead to adverse cardiovascular physiology and outcomes.
Behavioral effects
In addition to these physiologic effects, depression is associated with poor secondary prevention among patients who have had an acute ischemic event. Patients with post-MI depression, compared to MI patients who are not depressed, are less likely to follow a low fat diet, reduce their cholesterol, exercise, quit smoking, or reduce stress in their lives, all of which increase their risk for a recurrent cardiac event.Citation109,Citation110 In fact, in the large Heart and Soul studyCitation111 of patients with depression and coronary artery disease, an association between depressive symptoms and adverse cardiovascular events was largely explained by behavioral factors, especially physical inactivity. Patients suffering from anxiety or emotional distress following MI also have been found to have difficulty adhering to risk-reducing behaviors such as easing stress, increasing socialization, improving diet, and ceasing to smoke.Citation61,Citation112 Finally, patients with depression or anxiety may be less likely to attendCitation113,Citation114 or completeCitation115,Citation116 cardiac rehabilitation programs where both their secondary prevention behaviors and their psychiatric symptoms could be addressed.
In sum, depression and anxiety have myriad effects on cardiovascular physiology via a variety of mechanisms and these effects likely play a role in the increased incidence of ischemic events in patients with these symptoms. Furthermore, the effects of depression and anxiety on health-promoting behavior clearly play a role in these patients’ poor cardiac outcomes.
Treatments for depression and anxiety in cardiac patients
Antidepressants
Antidepressants can be used to treat patients with depression and patients with formal anxiety disorders, such as generalized anxiety disorder, panic disorder, or post-traumatic stress disorder. In general, the older tricyclic antidepressants (eg, amitriptyline, nortriptyline) should be avoided in patients with cardiac illness. First, these agents have adverse cardiovascular side effects in this population including orthostatic hypotension as well as tachycardia due to anticholinergic effects. Furthermore, these agents can lengthen cardiac intervals (eg, QRS and QTc) and can be proarrhythmic in a subset of the population. Citation117 In epidemiologic studies, prescription of tricyclic antidepressants has been associated with increased rates of subsequent MI compared to patients receiving selective serotonin reuptake inhibitors (SSRIs) or no treatment.Citation118
In contrast, SSRIs appear to be safe and effective in cardiac populations. These agents can be used to treat depression and formal anxiety disorders (eg, generalized anxiety disorder, panic disorder) in cardiac patients. Though SSRIs can be associated with increased anxiety, insomnia, or restlessness during the first several days of treatment in some patients, these effects are generally mild. They do not commonly cause orthostasis, tachycardia, or other adverse cardiovascular effects, and are well-tolerated in this population. Small trials of SSRIs and other antidepressants have found these agents to be safe and to significantly reduce symptoms of depression in patients with ischemic heart disease.Citation119,Citation120
A larger study, the Canadian Cardiac Randomized Evaluation of Antidepressant and Psychotherapy Efficacy (CREATE) placebo-controlled trial of 284 depressed outpatients with coronary artery disease, found that citalopram was significantly more efficacious than placebo. Citation28 Citalopram was well-tolerated in this study and was not associated with serious adverse events. Further, the multicenter SADHART randomized controlled trial of 369 post-ACS patients with major depressive disorder (MDD) found sertraline to be safe, well-tolerated, and efficacious in patients who began treatment approximately 1 month post-ACS.Citation10 Furthermore, a post hoc analysis of the Enhancing Recovery in Coronary Heart Disease Patients (ENRICHD) trial (a trial of cognitive behavioral therapy (CBT) for post-MI depression that had some patients taking antidepressants in both the experimental and control groups) found that patients receiving SSRIs had an over 40% reduction in the risk of cardiac mortality and reinfarction over a mean 29 month follow-up, compared to those not taking SSRIs.Citation121 One potential mechanism by which SSRIs may reduce cardiac events may involve reduction of platelet activity, as treatment of depressed patients with SSRIs leads to decreased markers of platelet hyperactivity.Citation65,Citation122,Citation123
Regarding other antidepressant agents, mirtazapine was studied in the randomized controlled Myocardial INfarction and Depression – Intervention Trial (MIND-IT) for patients with post-MI depression. The authors found that mirtazapine was safe, well-tolerated, and more efficacious than placebo over the 24 week trial.Citation124 However, treatment with mirtazapine did not appear to impact cardiovascular outcomes,Citation125 and some side effects of this agent (eg, weight gain, increased lipids) may relegate it to second-line status on patients with a history of myocardial ischemia. Finally, there is less evidence for the use of mirtazapine for anxiety disorders compared to the SSRIs.
Bupropion, while relatively unstudied for depression in patients with cardiac illness, has been studied in post-MI patients as an aid to smoking cessation. These studies found this agent to be safe and well-tolerated in this subset of patients (though it can cause anxiety, restlessness, or insomnia) and it has not been associated with increased rates of serious cardiovascular side effects.Citation126 Therefore bupropion may be indicated in depressed cardiac patients who wish to quit smoking. Other antidepressants, such as venlafaxine and duloxetine, have not been well-studied in cardiac populations, though venlafaxine is known to have dose-dependent increases in blood pressure associated with its use.Citation127
In sum, the SSRIs are well-studied agents for depression in patients with cardiac disease, are safe and efficacious in this population, can also be used for patients with anxiety disorders, and may be associated with decreased rates of adverse cardiac outcomes. Other antidepressants can be used under specific circumstances, though tricyclic antidepressants are generally not recommended.
Benzodiazepines
Benzodiazepines are effective in the reduction of acute anxiety and are effective in the treatment of some anxiety disorders (eg, panic disorder). These agents are rapidly effective and are well-used in patients with ongoing or recent myocardial ischemia for whom anxiety is leading to elevated heart rate, blood pressure, or other physiologic difficulties. These agents have several beneficial physiologic effects including acutely lowering catecholamine levels and decreasing coronary vascular resistance.Citation11,Citation128,Citation129 However, there are several caveats with the use of these agents: they can be associated with increased risk of falls, sedation, respiratory depression, and physiologic dependence,Citation130 and they do not treat comorbid depressive symptoms. Despite these caveats, these rapidly-acting anxiolytics can be substantially effective among patients with ischemic heart disease and ongoing anxiety, Citation131 though for patients with depression or formal anxiety disorders, antidepressants are often the treatment of choice.
Psychotherapy
Psychotherapeutic interventions are appealing for cardiac patients because of their lack of somatic side effects. In addition, these interventions can be individualized to focus on a given patient’s specific difficulties. Specific forms of psychotherapy have been studied in cardiac patients. The largest trial of psychotherapy in post-MI patients, the previously mentioned ENRICHD trial of 2481 patients,Citation9 found that treatment with CBT significantly reduced depressive symptoms and improved quality of life among post-MI patients, though it did not (in contrast to antidepressants) improve cardiac outcomes. The CREATE trial, in addition to studying citalopram, also utilized an evidence-based treatment called interpersonal psychotherapy (IPT), but found it did not improve depressive symptoms compared to an active control.Citation28 To our knowledge, there has not been a psychotherapeutic intervention for anxiety in cardiac patients, though CBT has been used to treat a wide variety of anxiety disorders in other populations.Citation132 Finally, a variety of other supportive and psychotherapeutic interventions have been used in patients with cardiovascular disease for a variety of conditions and though the studies of many of these interventions have been less rigorous than those listed above, they appear to improve outcomes.Citation133
Overall, psychotherapy can be effective for cardiac patients with depression or anxiety, though it may have less efficacy or impact on medical outcomes than treatment with antidepressants. A further pragmatic difficulty with psychotherapy is that such therapy, particularly evidence-based forms of treatment, can be difficult to source, especially in areas without nearby academic centers.
Exercise and cardiac rehabilitation
Exercise is an effective antidepressant,Citation134 is associated with reduced anxiety,Citation135 and has substantial cardiovascular benefit. A pair of trials of exercise (30 minutes of continuous walking/jogging to reach a target heart rate, three times per week for 16 weeks) in depressed patients found that regular exercise was as effective as sertraline in the treatment of depression. Citation134,Citation136 Follow-up results from the first trial, six months after the end of the study, found depression improvements among patients in the exercise group to be sustained longer than in those receiving antidepressants.Citation137 In addition, cardiac rehabilitation programs can provide many services that are helpful to cardiac patients with depression, from ongoing depression evaluation, to social support, to specific interventions for cardiovascular health. Therefore, both of these interventions can be tremendously helpful for cardiac patients with psychological distress.
However, cardiac patients with depression are less likely to exercise than their nondepressed counterpartsCitation110 and, as noted, are less likely to attend and complete cardiac rehabilitation programs.Citation114,Citation116 Anxiety also appears to reduce participation in these programs.Citation115 Clinically, we often find that improving patients’ depression, anxiety, and distress initially with medication or psychotherapy is necessary before they are willing and able to participate in exercise or cardiac rehabilitation.
Impact of cardiovascular medications on mood and anxiety symptoms
Patients with cardiac disease, especially those with a history of ischemic events, may be prescribed multiple medications. In general, many commonly prescribed agents, including aspirin, clopidogrel, warfarin, angiotensin-converting enzyme inhibitors, and nitrates are not associated with substantial psychiatric effects.Citation138 Though low cholesterol has been associated with increased rates of depression, aggression, and suicidality in some trials,Citation139–Citation142 this link has also been refuted in several studies. Furthermore, lowering serum cholesterol does not appear to increase the risk of depression or suicidal behaviorCitation143 and studies of lipid-lowering agents such as HMG-CoA reductase inhibitors (‘statins’) have not found any association between these agents and mood symptoms, aggression, or changes in cognition.Citation144,Citation145
Finally, the association between beta-blockers and depression has long been controversial. A number of case reports and several small studies (that sometimes did not control for some important covariables) found associations between propranolol and the onset of depression, Citation146,Citation147 however, a larger prospective controlled study and comprehensive review of the literature on propranolol found no association between this agent and depression.Citation148,Citation149 When expanded to include other beta-blockers, the majority of studies and reviews, including a large 2002 meta-analysis,Citation150 found no association with depression, though there is some association between beta-blockers and fatigue. On the other hand, beta-blockers, specifically propranolol, have been found to be effective in the treatment of anxiety and aggression. Citation151,Citation152 In sum, the relationship between propranolol and depression is equivocal. There is probably no association between beta-blockers and depression for the other agents in this class, though idiosyncratic reactions are always possible. In contrast, propranolol can be used as a therapeutic agent for cardiac patients with anxiety or aggression.
Conclusion
Depression and anxiety among patients with acute myocardial ischemia are highly prevalent and independently associated with adverse cardiovascular outcomes, including mortality. At this point, there is little doubt that addressing these conditions is critical in cardiac patients, but there remain a number of research and clinical steps to bridge the gap between this knowledge and patients receiving optimal care.
With respect to future research, it will be important to learn more about the combined effects of depression and anxiety on cardiac outcomes. Another important goal is the identification of subsets of cardiac patients for whom early and aggressive treatment of depression and anxiety is particularly critical. In addition, a better understanding of the mechanisms by which these psychiatric symptoms impair cardiovascular health may allow the development of mechanism-specific treatments. Finally, large prospective studies, if feasible, of existing treatments of depression and anxiety (eg, SSRIs) to determine whether cardiac outcomes improve as a result of their use would provide highly valuable information about the medical impact of these treatments.
Clinically, it is vital to find ways to help front-line practitioners to systematically identify depression and anxiety among their patients with cardiovascular disease. Likewise, it is necessary to develop infrastructure such that identified patients receive basic, but critical, treatments for these disorders. One future step that could combine clinical care and research is further investigation of care management models. These models of assessment and treatment utilize a care manager to efficiently identify patients with depression and anxiety. The care manager then coordinates treatment between patient, primary care physician, and consulting psychiatrist in a longitudinal manner. Such models have been used in outpatient medical settings and have been found to significantly improve depression and anxiety outcomes in a cost-effective manner.Citation153–Citation156 Most recently, such a model led to improved outcomes in depressed patients undergoing cardiac surgery.Citation157 Patients with a history of acute cardiovascular disease, such as ACS, represent a population who may most benefit from care management programs, given the strong link between depression/anxiety and medical outcomes.
Disclosures
The authors report no conflicts of interest relevant to this research.
References
- GraceSLAbbeySEIrvineJShnekZMStewartDEProspective examination of anxiety persistence and its relationship to cardiac symptoms and recurrent cardiac eventsPsychother Psychosom20047334435215479989
- HuffmanJCSmithFABlaisMABeiserMEJanuzziJLFricchioneGLRecognition and treatment of depression and anxiety in patients with acute myocardial infarctionAm J Cardiol20069831932416860016
- KapteinKIde JongePvan den BrinkRHKorfJCourse of depressive symptoms after myocardial infarction and cardiac prognosis: a latent class analysisPsychosom Med20066866266816987947
- ZiegelsteinRCKimSYKaoDCan doctors and nurses recognize depression in patients hospitalized with an acute myocardial infarction in the absence of formal screeningPsychosom Med20056739339715911901
- BarthJSchumacherMHerrmann-LingenCDepression as a risk factor for mortality in patients with coronary heart disease: a meta-analysisPsychosom Med20046680281315564343
- Frasure-SmithNLesperanceFDepression and anxiety as predictors of 2-year cardiac events in patients with stable coronary artery diseaseArch Gen Psychiatry200865627118180430
- Frasure-SmithNLesperanceFTalajicMDepression and 18-month prognosis after myocardial infarctionCirculation19959199910057531624
- KubzanskyLDKawachiIGoing to the heart of the matter: do negative emotions cause coronary heart diseaseJ Psychosom Res20004832333710880655
- BerkmanLFBlumenthalJBurgMEffects of treating depression and low perceived social support on clinical events after myocardial infarction: the Enhancing Recovery in Coronary Heart Disease Patients (ENRICHD) Randomized TrialJAMA20032893106311612813116
- GlassmanAHO’ConnorCMCaliffRMSertraline treatment of major depression in patients with acute MI or unstable anginaJAMA200228870170912169073
- HuffmanJCSternTAThe use of benzodiazepines in the treatment of chest pain: a review of the literatureJ Emerg Med20032542743714654185
- GilbodySSheldonTHouseAScreening and case-finding instruments for depression: a meta-analysisCMAJ2008178997100318390942
- World Health OrganizationThe World Health Report 2004-changing history2004 Available at http://www.who.int/whr/2004/annex/topic/en/annex_2_en.pdfAccessed on January 10, 2010
- Lloyd-JonesDAdamsRJBrownTMHeart Disease and Stroke Statistics-2010 Update. A report from the American Heart AssociationCirculation2010121e46e21520019324
- WulsinLRIs depression a major risk factor for coronary disease? A systematic review of the epidemiologic evidenceHarv Rev Psychiatry200412799315204803
- CarneyRMFreedlandKEShepsDSDepression is a risk factor for mortality in coronary heart diseasePsychosom Med20046679980115564342
- FishbeinMCThe vulnerable and unstable atherosclerotic plaqueCardiovasc Pathol20101961118835793
- HanssonGKInflammation, atherosclerosis, and coronary artery diseaseN Engl J Med20053521685169515843671
- YamadaDMTopolEJImportance of microembolization and inflammation in atherosclerotic heart diseaseAm Heart J2000140S9010211100003
- MorrowDACannonCPRifaiNAbility of minor elevations of troponins I and T to predict benefit from an early invasive strategy in patients with unstable angina and non-ST elevation myocardial infarction: results from a randomized trialJAMA20012862405241211712935
- HsuLFMakKHLauKWClinical outcomes of patients with diabetes mellitus and acute myocardial infarction treated with primary angioplasty or fibrinolysisHeart20028826026512181218
- RudischBNemeroffCBEpidemiology of comorbid coronary artery disease and depressionBiol Psychiatry20035422724012893099
- LesperanceFFrasure-SmithNJuneauMTherouxPDepression and 1-year prognosis in unstable anginaArch Intern Med20001601354136010809041
- van MelleJPde JongePSpijkermanTAPrognostic association of depression following myocardial infarction with mortality and cardiovascular events: a meta-analysisPsychosom Med20046681482215564344
- NarrowWERaeDSRobinsLNRegierDARevised prevalence estimates of mental disorders in the United States: using a clinical significance criterion to reconcile 2 surveys’ estimatesArch Gen Psychiatry20025911512311825131
- ValensteinMVijanSZeberJEBoehmKButtarAThe cost-utility of screening for depression in primary careAnn Intern Med200113434536011242495
- GlassmanAHBiggerJTGaffneyMShapiroPASwensonJROnset of major depression associated with acute coronary syndromes: relationship of onset, major depressive disorder history, and episode severity to sertraline benefitArch Gen Psychiatry20066328328816520433
- LesperanceFFrasure-SmithNKoszyckiDEffects of citalopram and interpersonal psychotherapy on depression in patients with coronary artery disease: the Canadian Cardiac Randomized Evaluation of Antidepressant and Psychotherapy Efficacy (CREATE) trialJAMA200729736737917244833
- MartensEJSmithORWinterJDenolletJPedersenSSCardiac history, prior depression and personality predict course of depressive symptoms after myocardial infarctionPsychol Med20083825726417868502
- Frasure-SmithNLesperanceFTalajicMDepression following myocardial infarction. Impact on 6-month survivalJAMA1993270181918258411525
- HuffmanJCSmithFABlaisMATaylorAMJanuzziJLFricchioneGLPre-existing major depression predicts in-hospital cardiac complications after acute myocardial infarctionPsychosomatics20084930931618621936
- HanssenTANordrehaugJEEideGEBjellandIRokneBAnxiety and depression after acute myocardial infarction: an 18-month follow-up study with repeated measures and comparison with a reference populationEur J Cardiovasc Prev Rehabil20091665165919707149
- JanuzziJLJrSternTAPasternakRCDeSanctisRWThe influence of anxiety and depression on outcomes of patients with coronary artery diseaseArch Intern Med20001601913192110888966
- LaneDCarrollDRingCBeeversDGLipGYMortality and quality of life 12 months after myocardial infarction: effects of depression and anxietyPsychosom Med20016322123011292269
- CroweJMRunionsJEbbesenLSOldridgeNBStreinerDLAnxiety and depression after acute myocardial infarctionHeart Lung199625981078682691
- PedersenSSSmithORDe VriesJAppelsADenolletJCourse of anxiety symptoms over an 18-month period in exhausted patients post percutaneous coronary interventionPsychosom Med20087034935518378871
- MurphyBMElliottPCWorcesterMUTrajectories and predictors of anxiety and depression in women during the 12 months following an acute cardiac eventBr J Health Psychol20081313515317535492
- DoeringLVMoserDKRiegelBPersistent comorbid symptoms of depression and anxiety predict mortality in heart diseaseInt J Cardiol2009
- FanAZStrineTWJilesRMokdadAHDepression and anxiety associated with cardiovascular disease among persons aged 45 years and older in 38 states of the United States, 2006Prev Med20084644545018377971
- RothenbacherDHahmannHWustenBKoenigWBrennerHSymptoms of anxiety and depression in patients with stable coronary heart disease: prognostic value and consideration of pathogenetic linksEur J Cardiovasc Prev Rehabil20071454755417667646
- TodaroJFShenBJRaffaSDTilkemeierPLNiauraRPrevalence of anxiety disorders in men and women with established coronary heart diseaseJ Cardiopulm Rehabil Prev200727869117558244
- BankierBJanuzziJLLittmanABThe high prevalence of multiple psychiatric disorders in stable outpatients with coronary heart diseasePsychosom Med20046664565015385686
- Muller-TaschTFrankensteinLHolzapfelNPanic disorder in patients with chronic heart failureJ Psychosom Res20086429930318291245
- HuffmanJCPollackMHPredicting panic disorder among patients with chest pain: an analysis of the literaturePsychosomatics20034422223612724504
- FleetRLavoieKBeitmanBDIs panic disorder associated with coronary artery disease? A critical review of the literatureJ Psychosom Res20004834735610880657
- FordDEMeadLAChangPPCooper-PatrickLWangNYKlagMJDepression is a risk factor for coronary artery disease in men: the precursors studyArch Intern Med1998158142214269665350
- WulsinLRSingalBMDo depressive symptoms increase the risk for the onset of coronary disease? A systematic quantitative reviewPsychosom Med20036520121012651987
- CarneyRMRichMWFreedlandKEMajor depressive disorder predicts cardiac events in patients with coronary artery diseasePsychosom Med1988506276332976950
- AxonRNZhaoYEgedeLEAssociation of depressive symptoms with all-cause and ischemic heart disease mortality in adults with self-reported hypertensionAm J Hypertens201023303719893497
- CarneyRMFreedlandKEDepression, mortality, and medical morbidity in patients with coronary heart diseaseBiol Psychiatry20035424124712893100
- de JongePSpijkermanTAvan den BrinkRHOrmelJDepression after myocardial infarction is a risk factor for declining health related quality of life and increased disability and cardiac complaints at 12 monthsHeart200692323915890765
- GlassmanAHBiggerJTJrGaffneyMPsychiatric characteristics associated with long-term mortality among 361 patients having an acute coronary syndrome and major depression: seven-year follow-up of SADHART participantsArch Gen Psychiatry2009661022102919736359
- CarneyRMFreedlandKETreatment-resistant depression and mortality after acute coronary syndromeAm J Psychiatry200916641041719289455
- de JongePHonigAvan MelleJPNonresponse to treatment for depression following myocardial infarction: association with subsequent cardiac eventsAm J Psychiatry20071641371137817728422
- DickensCMcGowanLPercivalCAssociation between depressive episode before first myocardial infarction and worse cardiac failure following infarctionPsychosomatics20054652352816288131
- KubzanskyLDDavidsonKWRozanskiAThe clinical impact of negative psychological states: expanding the spectrum of risk for coronary artery diseasePsychosom Med200567Suppl 1S101415953792
- KubzanskyLDKawachiISpiroA3rdWeissSTVokonasPSSparrowDIs worrying bad for your heart? A prospective study of worry and coronary heart disease in the Normative Aging StudyCirculation1997958188249054737
- HuffmanJCSmithFABlaisMAJanuzziJLFricchioneGLAnxiety, independent of depressive symptoms, is associated with in-hospital cardiac complications after acute myocardial infarctionJ Psychosom Res20086555756319027445
- MoserDKDracupKIs anxiety early after myocardial infarction associated with subsequent ischemic and arrhythmic eventsPsychosom Med1996583954018902890
- MoserDKRiegelBMcKinleySDoeringLVAnKSheahanSImpact of anxiety and perceived control on in-hospital complications after acute myocardial infarctionPsychosom Med200769101617244843
- MayouRAGillDThompsonDRDepression and anxiety as predictors of outcome after myocardial infarctionPsychosom Med20006221221910772399
- StrikJJDenolletJLousbergRHonigAComparing symptoms of depression and anxiety as predictors of cardiac events and increased health care consumption after myocardial infarctionJ Am Coll Cardiol2003421801180714642691
- RutledgeTLinkeSEKrantzDSComorbid depression and anxiety symptoms as predictors of cardiovascular events: results from the NHLBI-sponsored women’s ischemia syndrome evaluation (WISE) studyPsychosom Med20097195896419834049
- Morel-KoppMCMcLeanLChenQThe association of depression with platelet activation: evidence for a treatment effectJ Thromb Haemost2009757358119192119
- MusselmanDLMarzecUMManatungaAPlatelet reactivity in depressed patients treated with paroxetine: preliminary findingsArch Gen Psychiatry20005787588210986551
- MusselmanDLTomerAManatungaAKExaggerated platelet reactivity in major depressionAm J Psychiatry1996153131313178831440
- MiyataKShimokawaHHigoTSarpogrelate, a selective 5-HT2A serotonergic receptor antagonist, inhibits serotonin-induced coronary artery spasm in a porcine modelJ Cardiovasc Pharmacol20003529430110672864
- VikenesKFarstadMNordrehaugJESerotonin is associated with coronary artery disease and cardiac eventsCirculation199910048348910430761
- Maurer-SpurejEPittendreighCSolomonsKThe influence of selective serotonin reuptake inhibitors on human platelet serotoninThromb Haemost20049111912814691577
- SchinsAHamulyakKScharpeSWhole blood serotonin and platelet activation in depressed post-myocardial infarction patientsLife Sci20047663765015567189
- AroraRCMeltzerHYIncreased serotonin2 (5-HT2) receptor binding as measured by 3H-lysergic acid diethylamide (3H-LSD) in the blood platelets of depressed patientsLife Sci1989447257342927243
- HrdinaPDBakishDRavindranAChudzikJCavazzoniPLapierreYDPlatelet serotonergic indices in major depression: up- regulation of 5-HT2A receptors unchanged by antidepressant treatmentPsychiatry Res19976673859075272
- NemeroffCBKnightDLFranksJCraigheadWEKrishnanKRFurther studies on platelet serotonin transporter binding in depressionAm J Psychiatry1994151162316257943450
- GeiserFMeierCWegenerIAssociation between anxiety and factors of coagulation and fibrinolysisPsychother Psychosom20087737738318716423
- PivacNMuck-SelerDJakovljevicMPlatelet 5-HT levels and hypothalamic- pituitary-adrenal axis activity in schizophrenic patients with positive and negative symptomsNeuropsychobiology19973619219211439
- InyLJPecknoldJSuranyi-CadotteBEStudies of a neurochemical link between depression, anxiety, and stress from [3H]imipramine and [3H]paroxetine binding on human plateletsBiol Psychiatry1994362812917993954
- PleinHBerkMThe platelet intracellular calcium response to serotonin and thrombin in patients with panic disorderEur Neuropsychopharmacol1999910711010082235
- MuldoonMFHerbertTBPattersonSMKamenevaMRaibleRManuckSBEffects of acute psychological stress on serum lipid levels, hemoconcentration, and blood viscosityArch Intern Med19951556156207887757
- LevineSPTowellBLSuarezAMKnieriemLKHarrisMMGeorgeJNPlatelet activation and secretion associated with emotional stressCirculation198571112911342986876
- LibbyPMolecular bases of the acute coronary syndromesCirculation199591284428507758192
- MoyerCFSajuthiDTulliHWilliamsJKSynthesis of IL-1 alpha and IL-1 beta by arterial cells in atherosclerosisAm J Pathol19911389519602012178
- HeeschenCHammCWBruemmerJSimoonsMLPredictive value of C-reactive protein and troponin T in patients with unstable angina: a comparative analysis. CAPTURE Investigators. Chimeric c7E3 AntiPlatelet Therapy in Unstable angina REfractory to standard treatment trialJ Am Coll Cardiol2000351535154210807457
- O’BrienSMScottLVDinanTGCytokines: abnormalities in major depression and implications for pharmacological treatmentHum Psychopharmacol20041939740315303243
- PitsavosCPanagiotakosDBPapageorgiouCTsetsekouESoldatosCStefanadisCAnxiety in relation to inflammation and coagulation markers, among healthy adults: the ATTICA studyAtherosclerosis200618532032616005881
- von KanelRBegreSAbbasCCSanerHGanderMLSchmidJPInflammatory biomarkers in patients with posttraumatic stress disorder caused by myocardial infarction and the role of depressive symptomsNeuroimmunomodulation201017394619816056
- von KanelRHeppUKraemerBEvidence for low-grade systemic proinflammatory activity in patients with posttraumatic stress disorderJ Psychiatr Res20074174475216901505
- BrennanAMFargnoliJLWilliamsCJPhobic anxiety is associated with higher serum concentrations of adipokines and cytokines in women with diabetesDiabetes Care20093292693119223611
- BankierBBarajasJMartinez-RumayorAJanuzziJLAssociation between C-reactive protein and generalized anxiety disorder in stable coronary heart disease patientsEur Heart J2008292212221718603621
- BuccellettiEGilardiEScainiEHeart rate variability and myocardial infarction: systematic literature review and metanalysisEur Rev Med Pharmacol Sci20091329930719694345
- FrenneauxMPAutonomic changes in patients with heart failure and in post-myocardial infarction patientsHeart2004901248125515486114
- CarneyRMFreedlandKEDepression and heart rate variability in patients with coronary heart diseaseCleve Clin J Med200976Suppl 2S131719376975
- CarneyRMBlumenthalJASteinPKDepression, heart rate variability, and acute myocardial infarctionCirculation20011042024202811673340
- SteinPKCarneyRMFreedlandKESevere depression is associated with markedly reduced heart rate variability in patients with stable coronary heart diseaseJ Psychosom Res20004849350010880671
- KawachiISparrowDVokonasPSWeissSTDecreased heart rate variability in men with phobic anxiety (data from the Normative Aging Study)Am J Cardiol1995758828857732994
- FrancisJLWeinsteinAAKrantzDSAssociation between symptoms of depression and anxiety with heart rate variability in patients with implantable cardioverter defibrillatorsPsychosom Med20097182182719661191
- LettHSBlumenthalJABabyakMADepression as a risk factor for coronary artery disease: evidence, mechanisms, and treatmentPsychosom Med20046630531515184688
- ResslerKJNemeroffCBRole of serotonergic and noradrenergic systems in the pathophysiology of depression and anxiety disordersDepress Anxiety200012Suppl 121911098410
- RothWTDoberenzSDietelASympathetic activation in broadly defined generalized anxiety disorderJ Psychiatr Res20084220521217250853
- ThayerJFFriedmanBHBorkovecTDAutonomic characteristics of generalized anxiety disorder and worryBiol Psychiatry1996392552668645772
- Hoehn-SaricRMcLeodDRFunderburkFKowalskiPSomatic symptoms and physiologic responses in generalized anxiety disorder and panic disorder: an ambulatory monitor studyArch Gen Psychiatry20046191392115351770
- de JagerJDekkerJMKooyAEndothelial dysfunction and low-grade inflammation explain much of the excess cardiovascular mortality in individuals with type 2 diabetes: the Hoorn StudyArterioscler Thromb Vasc Biol2006261086109316514084
- FischerDRossaSLandmesserUEndothelial dysfunction in patients with chronic heart failure is independently associated with increased incidence of hospitalization, cardiac transplantation, or deathEur Heart J200526656915615801
- KatzSDHryniewiczKHriljacIVascular endothelial dysfunction and mortality risk in patients with chronic heart failureCirculation200511131031415655134
- PizziCManzoliLManciniSCostaGMAnalysis of potential predictors of depression among coronary heart disease risk factors including heart rate variability, markers of inflammation, and endothelial functionEur Heart J2008291110111718400765
- SherwoodAHinderliterALWatkinsLLWaughRABlumenthalJAImpaired endothelial function in coronary heart disease patients with depressive symptomatologyJ Am Coll Cardiol20054665665916098431
- HarrisKFMatthewsKASutton-TyrrellKKullerLHAssociations between psychological traits and endothelial function in postmeno-pausal womenPsychosom Med20036540240912764213
- NaritaKMurataTHamadaTAssociation between trait anxiety and endothelial function observed in elderly males but not in young malesInt Psychogeriatr20071994795417147843
- NaritaKMurataTHamadaTInteractions among higher trait anxiety, sympathetic activity, and endothelial function in the elderlyJ Psychiatr Res20074141842716494899
- HuffmanJCSmithFAFricchioneGLJanuzziJLNadelmanSPirlWFDepression and failure of cholesterol lowering after acute myocardial infarctionPrim Care Companion J Clin Psychiatry201012e1e6
- ZiegelsteinRCFauerbachJAStevensSSRomanelliJRichterDPBushDEPatients with depression are less likely to follow recommendations to reduce cardiac risk during recovery from a myocardial infarctionArch Intern Med20001601818182310871976
- WhooleyMAde JongePVittinghoffEDepressive symptoms, health behaviors, and risk of cardiovascular events in patients with coronary heart diseaseJAMA20083002379238819033588
- KuhlEAFauerbachJABushDEZiegelsteinRCRelation of anxiety and adherence to risk-reducing recommendations following myocardial infarctionAm J Cardiol20091031629163419539067
- LaneDCarrollDRingCBeeversDGLipGYPredictors of attendance at cardiac rehabilitation after myocardial infarctionJ Psychosom Res20015149750111602219
- AdesPAWaldmannMLMcCannWJWeaverSOPredictors of cardiac rehabilitation participation in older coronary patientsArch Intern Med1992152103310351580707
- McGradyAMcGinnisRBadenhopDBentleMRajputMEffects of depression and anxiety on adherence to cardiac rehabilitationJ Cardiopulm Rehabil Prev20092935836419940639
- CaseyEHughesJWWaechterDJosephsonRRosneckJDepression predicts failure to complete phase-II cardiac rehabilitationJ Behav Med20083142143118719990
- GlassmanAHRooseSPRisks of antidepressants in the elderly: tricyclic antidepressants and arrhythmia-revising risksGerontology199440Suppl 115208020766
- CohenHWGibsonGAldermanMHExcess risk of myocardial infarction in patients treated with antidepressant medications: association with use of tricyclic agentsAm J Med20001082811059434
- ShapiroPALesperanceFFrasure-SmithNAn open-label preliminary trial of sertraline for treatment of major depression after acute myocardial infarction (the SADHAT Trial). Sertraline Anti-Depressant Heart Attack TrialAm Heart J19991371100110610347338
- StrikJJHonigALousbergREfficacy and safety of fluoxetine in the treatment of patients with major depression after first myocardial infarction: findings from a double-blind, placebo-controlled trialPsychosom Med20006278378911138997
- TaylorCBYoungbloodMECatellierDEffects of antidepressant medication on morbidity and mortality in depressed patients after myocardial infarctionArch Gen Psychiatry20056279279815997021
- PollockBGLaghrissi-ThodeFWagnerWREvaluation of platelet activation in depressed patients with ischemic heart disease after paroxetine or nortriptyline treatmentJ Clin Psychopharmacol20002013714010770450
- SerebruanyVLGlassmanAHMalininAIPlatelet/endothelial biomarkers in depressed patients treated with the selective serotonin reuptake inhibitor sertraline after acute coronary events: the Sertraline AntiDepressant Heart Attack Randomized Trial (SADHART) Platelet SubstudyCirculation200310893994412912814
- HonigAKuyperAMScheneAHTreatment of post-myocardial infarction depressive disorder: a randomized, placebo-controlled trial with mirtazapinePsychosom Med20076960661317846258
- van MelleJPde JongePHonigAEffects of antidepressant treatment following myocardial infarctionBr J Psychiatry200719046046617541103
- RigottiNAThorndikeANReganSBupropion for smokers hospitalized with acute cardiovascular diseaseAm J Med20061191080108717145253
- ThaseMEEffects of venlafaxine on blood pressure: a meta-analysis of original data from 3744 depressed patientsJ Clin Psychiatry1998595025089818630
- CotePCampeauLBourassaMGTherapeutic implications of diazepam in patients with elevated left ventricular filling pressureAm Heart J1976917477511274825
- CotePNobleJBourassaMGSystemic vasodilatation following diazepam after combined sympathetic and parasympathetic blockade in patients with coronary heart diseaseCathet Cardiovasc Diagn197623693801000625
- ArbanasGArbanasDDujamKAdverse effects of benzodiazepines in psychiatric outpatientsPsychiatr Danub20092110310719270632
- WheatleyDThe value of anti-anxiety drugs in the management of cardiac diseaseActa Med Scand Suppl19826602192306127907
- NortonPJPriceECA meta-analytic review of adult cognitivebehavioral treatment outcome across the anxiety disordersJ Nerv Ment Dis200719552153117568301
- LindenWPhillipsMJLeclercJPsychological treatment of cardiac patients: a meta-analysisEur Heart J2007282972298417984133
- BlumenthalJABabyakMAMooreKAEffects of exercise training on older patients with major depressionArch Intern Med19991592349235610547175
- De MoorMHBeemALStubbeJHBoomsmaDIDe GeusEJRegular exercise, anxiety, depression and personality: a population-based studyPrev Med20064227327916439008
- BlumenthalJABabyakMADoraiswamyPMExercise and pharmacotherapy in the treatment of major depressive disorderPsychosom Med20076958759617846259
- BlumenthalJASherwoodAGulletteECExercise and weight loss reduce blood pressure in men and women with mild hypertension: effects on cardiovascular, metabolic, and hemodynamic functioningArch Intern Med20001601947195810888969
- HuffmanJCSternTANeuropsychiatric consequences of cardiovascular medicationsDialogues Clin Neurosci20079294517506224
- Buydens-BrancheyLBrancheyMHudsonJFergesonPLow HDL cholesterol, aggression and altered central serotonergic activityPsychiatry Res2000939310210725526
- NeatonJDBlackburnHJacobsDSerum cholesterol level and mortality findings for men screened in the Multiple Risk Factor Intervention Trial. Multiple Risk Factor Intervention Trial Research GroupArch Intern Med1992152149015001627030
- ShinJYSulsJMartinRAre cholesterol and depression inversely related? A meta-analysis of the association between two cardiac risk factorsAnn Behav Med200836334318787911
- SullivanPFJoycePRBulikCMMulderRTOakley-BrowneMTotal cholesterol and suicidality in depressionBiol Psychiatry1994364724777811844
- ManfrediniRCaraccioloSSalmiRBoariBTomelliAGalleraniMThe association of low serum cholesterol with depression and suicidal behaviours: new hypotheses for the missing linkJ Int Med Res20002824725711191718
- HMG-CoA reductase inhibitors for hypercholesterolemiaN Engl J Med1988319122212233173461
- DavidsonMHSteinEAHunninghakeDBLipid-altering efficacy and safety of simvastatin 80 mg/day: worldwide long-term experience in patients with hypercholesterolemiaNutr Metab Cardiovasc Dis20001025326211213534
- HallasJEvidence of depression provoked by cardiovascular medication: a prescription sequence symmetry analysisEpidemiology199674784848862977
- ThiessenBQWallaceSMBlackburnJLWilsonTWBergmanUIncreased prescribing of antidepressants subsequent to beta-blocker therapyArch Intern Med1990150228622901978648
- Perez-StableEJHallidayRGardinerPSThe effects of propranolol on cognitive function and quality of life: a randomized trial among patients with diastolic hypertensionAm J Med200010835936510759091
- StoudemireABrownJTHarrisRTPropranolol and depression: a reevaluation based on a pilot clinical trialPsychiatr Med198422112186400597
- KoDTHebertPRCoffeyCSSedrakyanACurtisJPKrumholzHMBeta-blocker therapy and symptoms of depression, fatigue, and sexual dysfunctionJAMA200228835135712117400
- FlemingerSGreenwoodRJOliverDLPharmacological management for agitation and aggression in people with acquired brain injuryCochrane Database Syst Rev2003CD00329912535468
- VaivaGDucrocqFJezequelKImmediate treatment with propranolol decreases posttraumatic stress disorder two months after traumaBiol Psychiatry20035494794914573324
- KatonWJVon KorffMLinEHThe Pathways Study: a randomized trial of collaborative care in patients with diabetes and depressionArch Gen Psychiatry2004611042104915466678
- SimonGEKatonWJLinEHCost-effectiveness of systematic depression treatment among people with diabetes mellitusArch Gen Psychiatry200764657217199056
- UnutzerJKatonWCallahanCMCollaborative care management of late-life depression in the primary care setting: a randomized controlled trialJAMA20022882836284512472325
- UnutzerJKatonWJFanMYLong-term cost effects of collaborative care for late-life depressionAm J Manag Care2008149510018269305
- RollmanBLBelnapBHLeMenagerMSTelephone-delivered collaborative care for treating post-CABG depression: a randomized controlled trialJAMA20093022095210319918088