Abstract
The aim of the present clinical trial was to determine the efficacy and safety of low-dose administration of tacrolimus in combination with methotrexate (MTX) in rheumatoid arthritis (RA) patients with an insufficient clinical response to MTX alone. Eleven patients with active RA, despite treatment with MTX, were enrolled and given tacrolimus in combination with MTX for 24 weeks. The primary endpoint was the assessment of clinical improvement using the European League against Rheumatism criteria. Administration of tacrolimus to RA patients with an insufficient response to MTX produced significant improvement in the Disease Activity Score 28 after 8–24 weeks. In addition, after 24 weeks, 50% and 25% of patients had achieved moderate and good responses, respectively, and there were significant reductions in the Modified Health Assessment Questionnaire, the rheumatoid factor and serum matrix metalloproteinase-3 levels. The present preliminary study suggests that low-dose tacrolimus in combination with MTX is well tolerated and provides both clinical and economic benefits.
Introduction
Rheumatoid arthritis (RA) is a chronic, progressive disease that requires early diagnosis and aggressive treatment to minimize morbidity.Citation1,Citation2 Disease-modifying antirheumatic drugs (DMARDs) are used to reduce inflammation and slow the progression of articular damage. Methotrexate (MTX) is the most widely used DMARD because of its favorable efficacy, record of safety, and ability to produce a prolonged response.Citation3,Citation4 Many patients, however, have an insufficient clinical response to MTX. In those patients, biologics such as infliximab or etanercept are used along with MTX. Although biologics are beneficial for patients with partial responses to MTX, their high cost makes them unobtainable for many RA patients. In these patients, combination therapies of MTX and other DMARDs have been considered.
Tacrolimus, a calcineurin inhibitor, was developed as an immunosuppressive agent and has been used in patients following organ transplantation, as well as in those with rheumatoid arthritis (RA) in Japan. Tacrolimus, a novel immunosuppressant, has been isolated from the fermentation broth of Streptomyces tsukubaenis Nr 9993 as a colorless prism, and the molecular formula was determined to be C44H69NO12.H2O. The compound suppresses immune responses in vitro and in vivo in miceCitation5 and inhibits T cell activation, thereby suppressing the production of tumor necrosis factor-α and other inflammatory cytokines involved in the development of RA.Citation6 FK506 (tacrolimus) inhibits both interleukin-2 and gamma-interferon secretion of PBMCs stimulated with PHA in a dose-dependent manner.Citation7 Yamagami T et al showed a novel mechamism for the action of physiological concentrations of FK506 in RA that regulates the production of glistatin/thymidine phosphorylase in fibroblast-like synoviocytes.Citation8 There are many reports about the efficacy and safety to RA patients.Citation9–Citation11 Moreover, there is also a report to systemic lupus erytematosus,Citation12 Churg–Strauss symdrome,Citation13 and the RA associated with MDS.Citation14
To reduce the economic cost and the risk of immoderate immune suppression from combination therapy, it would be beneficial to examine the efficacy of therapy with low-dose administration of tacrolimus in combination with MTX in patients with RA. The aim of the present clinical trial was to determine the efficacy and safety of low-dose tacrolimus in combination with MTX to control the signs and symptoms of RA in patients with an insufficient clinical response to MTX alone.
Methods
Study design and population
Eleven patients who fulfilled the American College of Rheumatology (ACR) 1987 revised criteria for RACitation15 between June 2009 and November 2009 participated in this prospective, open, nonplacebo-controlled study. RA disease activity was evaluated using the Disease Activity Score (DAS) 28.Citation16 Patients who had moderate or severe disease activity (DAS28 > 3.2) at baseline despite treatment with MTX for more than 3 months were enrolled and given tacrolimus. Tacrolimus is typically given at a dosage of 3 mg/day to patients with RA. In the present study, we used a starting dosage of 1 mg/day. Our purpose was to examine the combined use in low dose (1 mg), and when an effect was insufficient, patients changed to an other treatment. All other DMARDs were discontinued except MTX, but stable doses of nonsteroidal anti-inflammatory drugs and oral corticosteroids (<10 mg/day prednisone or its equivalent) were allowed. When DAS28 < 2.6 was achieved, prednisolone started dose down by 1 mg.
The primary endpoint was the assessment of clinical improvement in the DAS28 using the European League against Rheumatism (EULAR) response criteria.Citation17 Secondary endpoints were the assessment of changes in the Modified Health Assessment Questionnaire (mHAQ),Citation18 serum levels of rheumatoid factor (RF) and matrix metalloproteinase-3 (MMP-3), and the incidence of remission and adverse events. Serum levels of C-reactive protein (CRP), RF, and MMP-3 were determined using latex photometric immunoassays, while the erythrocyte sedimentation rate (ESR) was determined using the Westergren method. At baseline, demographic data and present medications were recorded; a complete history was taken; and a physical examination and routine laboratory examinations, including whole blood counts, tests of renal and hepatic function, and urinalysis, were carried out at 3- to 6-week intervals to screen for adverse clinical side effects. The aforementioned clinical parameters were assessed at baseline and after 12 and 24 weeks of tacrolimus-MTX combination therapy. The present clinical trial was performed in accordance with protocols approved by the Human Subjects Research Committee at our institution, and informed consent was obtained from all patients.
Statistical analysis
The data are expressed as the mean ± standard error (SE). For a comparison of the groups, chi-square analysis was applied for discrete variables, and the Kruskal–Wallis analysis of variance (ANOVA) was used for continuous variables. Changes in variables after intervention were evaluated using the Wilcoxon test for paired observations. P values less than 0.05 were considered significant.
Results
The patient characteristics are summarized in . At the start of this trial, the mean age of the patients was 65.5 (range: 49–82) years, and disease duration was 8.8 (0.5–14) years. Baseline DAS28 for the 11 patients was 4.51 (2.95–6.17); MTX dosage and duration were 8.73 (8–12) mg/week and 3.18 (0.5–10) years, respectively; and mHAQ was 0.58 (0.125–1). The dosage of MTX administered to our patients was somewhat lower than that reported in other countries; this likely reflects the lower effective and recommended dosages of MTX (6–8 mg per week) in Japanese RA patients, which is in accordance with the results of a double-blind, placebo-controlled (phase II–III) trial among Japanese RA patients. Adverse events were observed in one RA patient with diabetes mellitus which was discontinued after 8 weeks because of a mild increase in blood glucose levels. The patient soon recovered without any additional medications. Furthermore, treatment was discontinued in one patient at 4 weeks, in one patient at 8 weeks, and in one patient at 20 weeks due to increases in RA disease activity or a lack of response to the combination therapy. Ten patients spent 8 weeks; nine patients spent 20 weeks; and eight patients spent 24 weeks receiving the combination therapy and completed the assessments and clinical examinations. The RA patients with an insufficient response to MTX who received the tacrolimus-MTX combination showed highly significant improvement in the DAS28 after 4 weeks (n = 10, baseline: 4.51 ± 0.31 to 4.03 ± 0.28, P < 0.005), 12 weeks (n = 9, baseline: 4.59 ± 0.34 to 3.38 ± 0.29, P < 0.01) and 24 weeks (n = 8, baseline: 4.45 ± 0.35 to 3.12 ± 0.34, P < 0.01) (). In addition, after 12 weeks, 44.4% of patients achieved a moderate response based on the EULAR criteria, and after 24 weeks, the number of those patients were maintained (). There were no significant differences between the poor response group and the moderate-good response group with respect to mean disease duration, MTX dosage or basal DAS28 and CRP levels (data not shown). Notably, clinical remission (DAS28 < 2.6) was observed in one RA patient after 24 weeks of combination therapy. In addition to the DAS28, significant reductions in serum CRP levels were observed after 12 weeks (n = 9, baseline: 1.92 ± 0.70 to 0.86 ± 0.34, P < 0.05) and 24 weeks (n = 8, baseline: 2.09 ± 0.77 to 0.51 ± 0.18, P < 0.01) (). Moreover, there were significant improvements in mHAQ responses after both 12 weeks (n = 9, baseline: 0.54 ± 0.10 to 0.24 ± 0.06, P < 0.01) and 24 weeks (n = 8, baseline: 0.58 ± 0.11 to 0.20 ± 0.06, P < 0.01), with 75% of the patients experiencing 50% improvement in their mHAQ responses after 12 and 24 weeks ().
Figure 1 Effect of tacrolimus-MTX combination therapy on the DAS28 in patients with RA. The DAS28 in RA patients was assessed from baseline to 24 weeks after the addition of tacrolimus to MTX therapy. Significant improvements in the DAS28 were seen at 4 weeks (*P < 0.005) and after 12–24 weeks (**P < 0.01) of tacrolimus-MTX combination therapy compared with baseline.
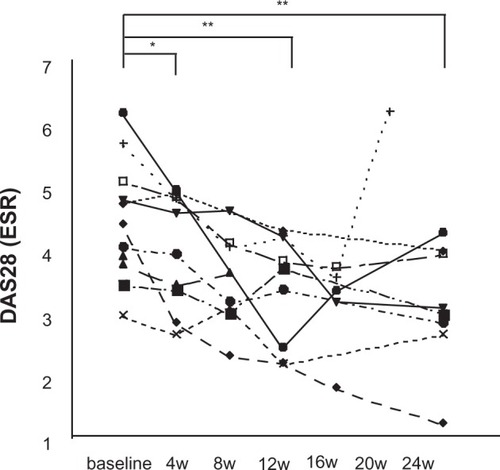
Figure 2 Effect of tacrolimus-MTX combination therapy on serum CRP levels in patients with RA. Serum CRP levels were assessed from baseline to 24 weeks after the addition of tacrolimus to MTX therapy. Significant reductions in serum CRP levels were seen after 12 weeks (*P < 0.05) and 24 weeks (**P < 0.01) of tacrolimus-MTX combination therapy compared with baseline.
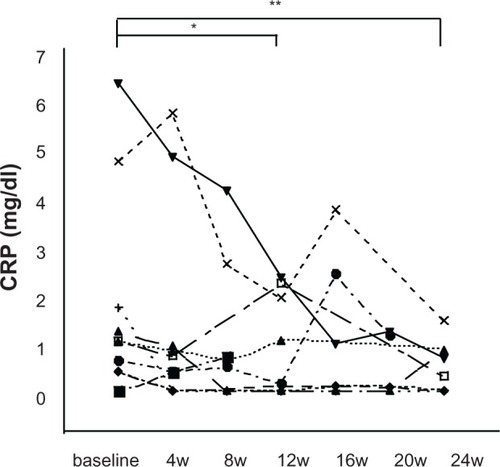
Figure 3 Effect of tacrolimus-MTX combination therapy on mHAQ responses in patients with RA. Significant improvements in mHAQ responses were seen after both 12 (*P < 0.01) and 24 (*P < 0.01) weeks of tacrolimus-MTX therapy.
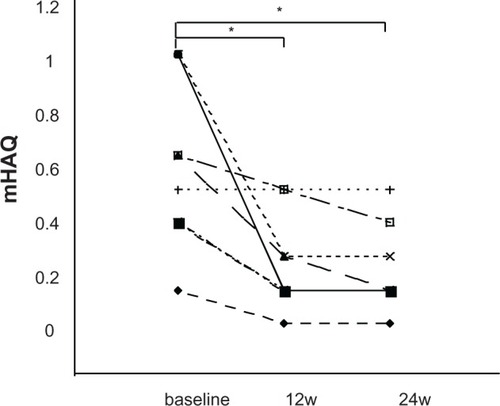
Table 1 Clinical characteristics of the patients enrolled in patient trial
Table 2 Percentage of patients who achieved moderate and good response in the EULAR response criteria
Changes in the levels of serum parameters
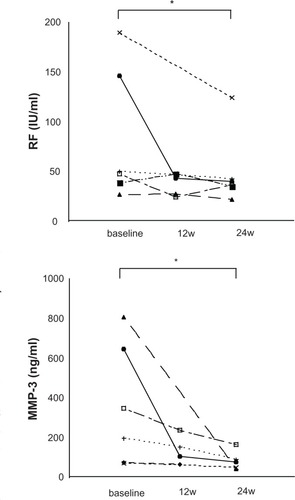
We next assessed changes in serum RF and MMP-3 levels. There was a significant reduction in serum RF levels after 24 weeks (n= 6, baseline: 82.6 ± 27.1 to 50.2 ± 15.1, P < 0.05) (). Similarly, there was a significant reduction in serum MMP-3 levels after 24 weeks (n = 5, baseline: 407.7 ± 137.0 to 80.0 ± 21.9, P < 0.05) ().
Figure 4 Effect of tacrolimus-MTX combination therapy on serum RF levels and serum MMP-3 levels in patients with RA. A) Serum RF levels and serum MMP-3 levels were assessed at baseline and 12 and 24 weeks after the addition of tacrolimus to MTX therapy. Significant reductions (*P < 0.05) in serum RF levels were seen after 24 weeks of tacrolimus-MTX combination therapy compared with baseline. B) Significant reductions (*P < 0.05) in serum MMP-3 levels were seen after 24 weeks of tacrolimus-MTX combination therapy compared with baseline.
Dosage of medicine
We were able to decrease the dosage of oral corticosteroids in two patients. The dosage for one patient was reduced from 4 mg to 2 mg after 24 weeks, and the dosage for another patient was reduced from 1 mg to nothing after 24 weeks. The dosages of any other medicines (MTX and nonsteroidal anti-inflammatory drugs) remained the same before and after treatment.
Discussion
The data presented in this study show that the administration of a tacrolimus-MTX combination to RA patients with an insufficient response to MTX led to a highly significant improvement of the DAS28 and the EULAR response criteria after 8–24 weeks (). In addition, there was a significant improvement in mHAQ responses, suggesting beneficial effects on quality of life.Citation19 We also found significant serological effects following tacrolimus administration, including a significant reduction in MMP-3 levels after 24 weeks. Given earlier findings that elevated serum MMP-3 levels may contribute to the progression of joint destruction,Citation20,Citation21 we suggest that tacrolimus-MTX combination therapy may exert a beneficial effect on the clinical course of patients with active RA.
After failure with MTX, combination therapy with other DMARDs or biologics is considered.Citation22 Although s ulfasalazine (SSP) is widely used in combination with MTX because they are both inexpensive and readily available to everyone, there are conflicting results with regard to their efficacy. Whereas Capell et al showed that SSP-MTX combination therapy provides significant beneficial clinical effects compared with MTX monotherapy,Citation23 others have reported that SSP provides no beneficial additive or synergistic effects in combination with MTX.Citation24 Additionally, although clinical trials of combination therapies with MTX plus other immunosuppressants or strong DMARDs, including cyclosporine A (CsA) and leflunomide, have shown beneficial effects in RA patients with high disease activity, there is an increased risk of adverse effects with these generally acting drugs.Citation25,Citation26 Kasama et al showed that low-dose mizoribine in combination with MTX is well tolerated and provides clinical benefits.Citation27 In contrast, another study administered tacrolimus at 3 mg/day to 80 RA patients with high disease activity and found an inadequate effect of MTX. Seven patients (12.5%) withdrew from the study because of adverse events, possibly related to treatment with tacrolimus.Citation28 One study administered tacrolimus at 1–3 mg per day to RA patients with an inadequate response to MTX and found significant improvement in the DAS28 (ESR), DAS28 (CRP), tender joint counts, swelling joint counts, CRP, and general health score.Citation29 Similar to our study, Furst DE reported that tender joints, ESR, and ACR 50 showed improvement in RA patients who were treated with the addition of tacrolimus at 1 mg per day.Citation10 Moreover, some studies that added low-dose tacrolimus to the treatment of patients who were non-responders to tumor necrosis factor inhibitor therapies and found improvements in RA.Citation30,Citation31 Clinical studies have demonstrated the efficacy of tacrolimus in RA patients with an insufficient response to MTX (summarized in ). Thus, the addition of low-dose tacrolimus is thought to lead to improvement in rheumatoid arthritis. P-glycoprotein (P-gp), a member of the ATP-binding cassette transporter family, causes drug resistance via the exclusion of intracellular drugs. Tacrolimus, a P-gp inhibitor, can improve the effect of MTX by blocking P-gp.Citation32
Table 3 Reports of clinical efficacy of tacrolimus therapy in RA patients with an insufficient response to MTX
In conclusion, there were no significant side effects of the addition of tacrolimus to MTX therapy in terms of safety. Decreases were seen in the DAS28 (ESR) and mHAQ values, and it was also possible to reduce the dose of corticosteroids in two patients. Furthermore, the use of tacrolimus at only 1 mg per day presents an extremely economical approach. By improving drug resistance, it is thought that the effect on the non-Japanese RA patients can be expected enough. We suggest that tacrolimus-MTX combination therapy be attempted prior to the administration of biological therapies.
Disclosure
No conflicts of interest were declared in relation to this paper.
References
- LeeDMWeinblattMERheumatoid arthritisLancet200135890391111567728
- JenkinsJKHardyKJMcMurrayRWThe pathogenesis of rheumatoid arthritis: a guide to therapyAm J Med Sci200232317118012003371
- WeinblattMEEfficacy of methotrexate in rheumatoid arthritisBr J Rheumatol199534Suppl 243488535649
- Guidelines for the management of rheumatoid arthritis: 2002 UpdateArthritis Rheum20024632834611840435
- KinoTHatanakaHHashimotoMFK-506, a novel immunosuppressant isolated from a Streptomyces. I. Fermentation, isolation, and physico-chemical and biological characteristicsJ Antibiot (Tokyo)198740124912552445721
- SakumaSKatoYNishigakiFFK506 potently inhibits T cell activation induced TNF-alpha and IL-1beta production in vitro by human peripheral blood mononuclear cellsBr J Pharmacol20001301655166310928971
- YoshimuraNMatsuiSHamashimaTOkaTEffect of a new immunosuppressive agent, FK506, on human lymphocyte responses in vitro. II. Inhibition of the production of IL-2 and gamma-IFN, but not B cell-stimulating factor 2Transplantation1989473563592465593
- YamagamiTWaguri-NagayaYIkutaKAoyamaMAsaiKOtsukaTFK506 inhibition of gliostatin/thymidine phosphorylase production induced by tumor necrosis factor-alpha in rheumatoid fibroblast-like synoviocytesRheumatol Int2010318 Epub ahead of print
- GremillionRBPoseverJOManekNWestJPvan Volen-HovenRFTacrolimus (FK506) in the treatment of severe, refractory rheumatoid arthritis: initial experience in 12 patientsJ Rheumatol1999262332233610555886
- FurstDESaagKFleischmannMREfficacy of tacrolimus in rheumatoid arthritis patients who have been treated unsuccessfully with methotrexate: a six-month, double-blind, randomized, dose-ranging studyArthritis Rheum2002462020202812209503
- SuzukiKKamedaHAmanoKSingle center prospective study of tacrolimus efficacy and safety in treatment of rheumatoid arthritisRheumatol Int20092943143619127365
- SuzukiKKamedaHAmanoKSingle center prospective study of tacrolimus efficacy and safety in the treatment of various manifestations in systemic lupus erythematosusRheumatol Int2010219 Epub ahead of print
- NiiyamaSAmohYSuzukiKWadaTKatsuokaKEfficacy of tacrolimus against Churg-Strauss syndrome in a patient with myasthenia gravisRheumatol Int20103084784819582460
- NozakiYNagareYKinoshitaKUraseFFunauchiMSuccessful treatment using tacrolimus plus corticosteroid in a patient with RA associated with MDSRheumatol Int20082848749017764011
- ArnettFCEdworthySMBlochDAThe American Rheumatism Association 1987 revised criteria for the classification of rheumatoid arthritisArthritis Rheum1988313153243358796
- van der HeijdeDMvan ‘t HofMAvan RielPLJudging disease activity in clinical practice in rheumatoid arthritis: first step in the development of a disease activity scoreAnn Rheum Dis1990499169202256738
- van GestelAMPrevooMLvan ‘t HofMAvan RijswijkMHvan de PutteLBvan RielPLDevelopment and validation of the European League Against Rheumatism response criteria for rheumatoid arthritis. Comparison with the preliminary American College of Rheumatology and the World Health Organization/International League Against Rheumatism CriteriaArthritis Rheum19963934408546736
- ZieblandSFitzpatrickRJenkinsonCMowatAComparison of two approaches to measuring change in health status in rheumatoid arthritis: the Health Assessment Questionnaire (HAQ) and modified HAQAnn Rheum Dis199251120212051466596
- LubeckDPHealth-related quality of life measurements and studies in rheumatoid arthritisAm J Manag Care2002881182012234022
- YamanakaHMatsudaYTanakaMSerum matrix metalloproteinase 3 as a predictor of the degree of joint destruction during the six months after measurement, in patients with early rheumatoid arthritisArthritis Rheum20004385285810765930
- AinolaMMMandelinJALiljestromMPLiTFHukkanenMVKonttinenYTPannus invasion and cartilage degradation in rheumatoid arthritis: involvement of MMP-3 and interleukin-1betaClin Exp Rheumatol20052364465016173240
- MunsterTFurstDEPharmacotherapeutic strategies for disease-modifying antirheumatic drug (DMARD) combinations to treat rheumatoid arthritis (RA)Clin Exp Rheumatol199917S29S3610589354
- CapellHAMadhokRPorterDRCombination therapy with sulfasalazine and methotrexate is more effective than either drug alone in patients with rheumatoid arthritis with a suboptimal response to sulfasalazine: results from the double-blind placebo-controlled MASCOT studyAnn Rheum Dis20076623524116926184
- HaagsmaCJvan RielPLde JongAJvan de PutteLBCombination of sulphasalazine and methotrexate versus the single components in early rheumatoid arthritis: a randomized, controlled, double-blind, 52 week clinical trialBr J Rheumatol199736108210889374925
- GerardsAHLandeweRBPrinsAPCyclosporin A monotherapy versus cyclosporin A and methotrexate combination therapy in patients with early rheumatoid arthritis: a double blind randomised placebo controlled trialAnn Rheum Dis20036229129612634224
- KremerJGenoveseMCannonGWCombination leflunomide and methotrexate (MTX) therapy for patients with active rheumatoid arthritis failing MTX monotherapy: open-label extension of a randomized, double-blind, placebo controlled trialJ Rheumatol2004311521153115290730
- KasamaTWakabayashiKOdaiTEffects of low-dose mizoribine pulse therapy in combination with methotrexate in rheumatoid arthritis patients with an insufficient response to methotrexateMod Rheumatol20091939540019440813
- KremerJMHabrosJSKolbaKSTacrolimus in rheumatoid arthritis patients receiving concomitant methotrexate: a six-month, open-label studyArthritis Rheum2003482763276814558080
- MoritaYSasaeYSakutaTSatohMSasakiTKashiharaNEfficacy of low-dose tacrolimus added to methotrexate in patients with rheumatoid arthritis in Japan: a retrospective studyMod Rheumatol20081837938418463945
- YokotaKAkiyamaYAsanumaYMiyoshiFSatoKMimuraTEfficacy of tacrolimus in infliximab-refractory progressive rheumatoid arthritisRheumatol Int20092945946118802706
- NaniwaTWatanabeMBannoSMaedaTAdding low dose tacrolimus in rheumatoid arthritis patients with an inadequate response to tumor necrosis factor inhibitor therapiesRheumatol Int2009291287129119153737
- TsujimuraSSaitoKNawataMNakayamadaSTanakaYOvercoming drug resistance induced by P-glycoprotein on lymphocytes in patients with refractory rheumatoid arthritisAnn Rheum Dis20086738038817660216