Abstract
Purpose:
To clarify the presence of oxidative stress in glaucoma and discuss whether free radicals contribute to neovascular glaucoma (NVG) and non-NVG.
Methods:
Two patient groups were formed: the NVG group (n = 10) and the non-NVG group (n = 17). Free radicals in aqueous humor were detected by measuring the electron spin resonance (ESR). To identify free radical species, either superoxide dismutase (SOD) or catalase was added to the aqueous humor and compared with aqueous humor in which SOD or catalase was not added.
Results:
In the NVG group, free radical waveforms were detected that differed from ascorbate-free radical (AFR) in all cases. Under SOD was added, the characteristic waveforms disappeared and the AFR of a specific waveform appeared. After catalase was added, the waveforms were unchanged. In the non-NVG group, the AFR of specific waveforms were detected in all cases. In 4 cases, the waveforms detected the presence of a trace of superoxide.
Conclusions:
In the NVG group, superoxides were detected, suggesting that superoxide scavenging activity was decreased markedly. L-ascorbic acid likely has an antioxidative function in the non-NVG group, suggesting that the aqueous humor in the NVG group was under higher oxidative stress compared with the non-NVG group.
Introduction
Free radicals are highly reactive due to their extreme instability. In biologic reactions, free radicals have been reported to be involved in tissue disorders caused by peroxidation. In ophthalmology, oxidative stress has been reported to induce and facilitate progression of cataracts and diabetic retinopathy.Citation1,Citation2 In glaucoma, antioxidant levels decrease in the aqueous humor in patients with primary open-angle glaucoma (POAG) compared with in the aqueous humor of patients with cataracts, suggesting that peroxidation may be involved in the development of glaucoma.Citation3 However, no studies have reported the results of direct measurement of free radicals in the aqueous humor in patients with glaucoma. In the current study, we measured the levels of free radicals in the aqueous humor of patients with glaucoma by electron spin resonance (ESR) to determine if there is a relationship between free radicals and neovascular glaucoma (NVG) and non-NVG.
Subjects and methods
The study included 10 eyes with NVG (mean patient age, 67 ± 10 years; men, 7 eyes; women: 3 eyes) and 17 eyes with non-NVG (mean patient age, 60 ± 14 years; men, 8 eyes; women: 9 eyes) examined at the Department of Ophthalmology, Dokkyo Medical University Koshigaya Hospital, Japan. The non-NVG group included 11 eyes with POAG, 5 eyes with primary angle closure glaucoma (PACG), and 1 eye with normal tension glaucoma (NTG) (, ). In accordance with the 2000 World Medical Association Declaration of Helsinki (Edinburgh, Scotland, 2000) informed consent was obtained from all subjects after they had received a detailed verbal explanation of the study before aqueous humor specimens were collected.
Table 1A Patient demographic data
Table 1B Patient demographic data
The aqueous humor specimens were obtained using a 27-gauge needle during trabeculectomy and immediately frozen with liquid nitrogen followed by measurement of free radicals by ESR spin trapping. The ESR measurement conditions are shown in . Free radicals were measured after mixing 10 μL of 5,5-dimethyl-1-pyrroline-N-oxide, the trapping agent, in 140 μL of ultrapure water followed by 20 μL of aqueous humor.
Table 2 ESR measurement conditions
A superoxide scavenger of Cu, Zn-superoxide dismutase (SOD) and a hydrogen peroxide scavenger of catalase were used as active oxygen scavengers to identify the free radicals species formed. When SOD or catalase were added, the measurement solution of free radicals added to SOD or catalase to make up for 140 μL of ultrapure water which in the case of non-addition of SOD or catalase to aqueous humor, and similarly measured by ESR. The measurement solution was added to 40 μL of Cu, Zn-SOD (10 U/μL) and then to 100 μL of ultrapure water, or 140 μL of catalase (22 U/μL). The volumes of DMPO and aqueous humor were the same as previously described.
Results
NVG group
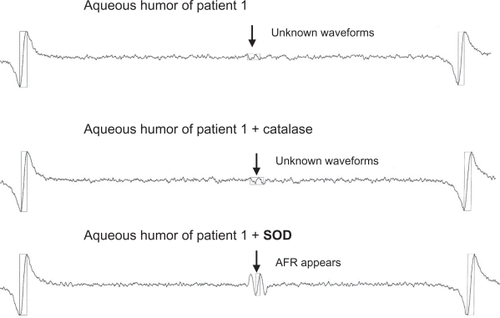
Free radical waveforms were detected that differed from AFR in all 10 cases. The waveforms in all cases did not change under catalase was added but did change to AFR with specific waveforms after SOD was added ().
Non-NVG group
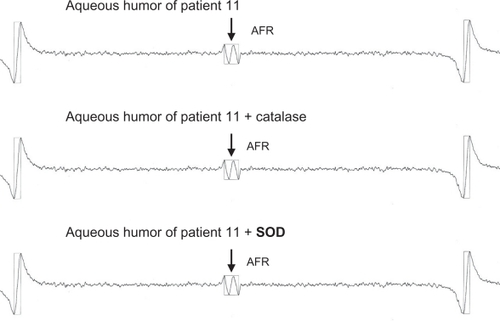
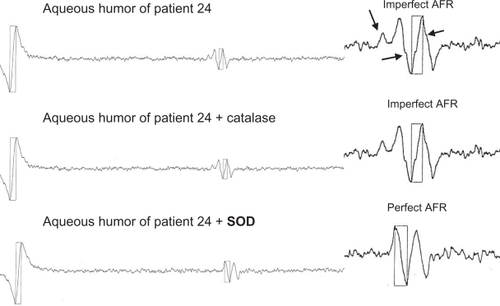
The ESR spectra were roughly divided into two patterns. In 13 of the 17 cases, AFR spectra were observed and the waveforms did not change after catalase or SOD was added (). In 4 of the 17 cases, slight variations with slightly incomplete AFR waveforms were observed. These waveforms did not change after catalase was added, but did change to complete AFR waveforms after SOD was added ().
Discussion
Fong et alCitation4 reported on ascorbic acid and peroxidation reactions in the aqueous humor of patients with POAG. These patients can be classified as those with only extremely low levels of ascorbic acid and those with high levels of ascorbic acid in the aqueous humor in the presence of glaucoma. Those with extremely low levels of ascorbic acid in the aqueous humor are susceptible to peroxidation stimulation. However, no free radicals were detected in the aqueous humor.
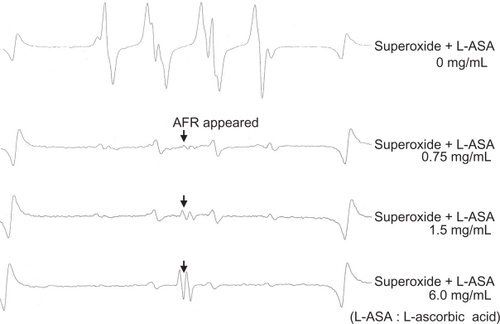
In the current study, we report for the first time the detection of free radicals in the aqueous humor of patients with glaucoma. AFR is formed by a reaction between L-ascorbic acid and superoxide. Moreover, since oxidized ascorbic acid is formed when superoxide reacts with AFR, AFR form intermediate products during the conversion from the reduced type to the oxidized type of ascorbic acid. shows ESR reaction spectra following in vitro formation of superoxide with a xanthine-xanthine oxidase system after different concentrations of L-ascorbic acid were added. The uppermost waveform is that of superoxide alone without L-ascorbic acid. The concentration of L-ascorbic acid increases moving downward and approaches the waveform of the AFR. The waveforms of the aqueous humor in the NVG group approximate the state of the second waveform from the top, confirming that the concentration of L-ascorbic acid is low relative to that of superoxide. The waveforms of the aqueous humor of the non-NVG group approach the state of the bottom waveform, confirming that the concentration of L-ascorbic acid is high relative to that of superoxide. The values of L-ascorbic acid measured in the aqueous humor specimens of the non-NVG group were equivalent to those in the specimens containing a high level of ascorbic acid reported by Fong et al while the values in the NVG group were equivalent to the extremely low values of ascorbic acid reported by Fong et al.Citation4
Figure 4 In vitro formation of superoxide with a xanthine-xanthine oxidase system followed by the addition of different concentrations of L-ascorbic acid.
Based on these results, , shows the free radicals detected in the aqueous humor of patients with glaucoma. Waveforms of the free radicals that differed from the AFR were detected in the NVG group; these waveforms did not change after catalase was added but did change to AFR after SOD was added. Since the waveforms changed as a result of SOD, these free radicals were determined to be superoxides. AFR was detected in 13 of 17 cases in the non-NVG group. Imperfect AFR waveforms were observed in the remaining 4 cases; these waveforms converted to complete AFR of specific waveforms only after SOD was added, which indicated that these free radicals contained a small amount of superoxide in the AFR (, ).
Table 3A Free radicals in aqueous humor of patients with glaucoma
Table 3B Free radicals in aqueous humor of patients with glaucoma
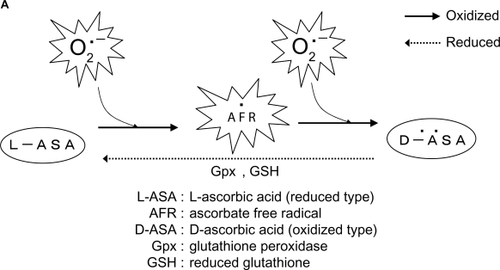
AFR is generated from L-ascorbic acid as a result of oxidation of L-ascorbic acid by unpaired electrons of superoxides, and so on. Moreover, the oxidized type of dehydroascorbic acid is reduced by the reaction between glutathione peroxidase (Gpx) and reduced glutathione (GSH) (). Based on this, we constructed a hypothetical model of the reactivity of free radicals in the aqueous humor of patients with glaucoma based on the results of the current study. Since superoxides were detected in the NVG group, the activity of superoxide scavengers such as SOD, L-ascorbic acid, and GSH decreased markedly in the aqueous humor of this group, resulting in the presence of a superoxide. In the NVG group, we believe that the L-ascorbic acid captured a large amount of superoxides and was subjected to peroxidation to the state of oxidized ascorbic acid through the AFR stage, resulting in the superoxide detection by ESR without elimination by ascorbic acid (). In addition, AFR may have been detected in the NVG group after SOD was added because excessive superoxide that had formed were eliminated, causing the L-ascorbic acid to remain at the AFR stage without undergoing peroxidation to the stage of dehydroascorbic acid ().
Figure 5 A) AFRs are generated from L-ascorbic acid as a result of L-ascorbic acid oxidation by unpaired electrons of superoxides. Moreover, the oxidized type of dehydroascorbic acid is reduced by the action of Gpx and GSH. B) In the NVG group, L-ascorbic acid captures a large amount of superoxides and is subjected to peroxidation to the state of oxidized ascorbic acid through the AFR stage, resulting in superoxides being detected without being eliminated by ascorbic acid. C) In the NVG group following addition of SOD, excessive superoxides are eliminated, causing the L-ascorbic acid to remain at the AFR stage without being peroxidated to oxidized L-ascorbic acid. D) In the non-NVG group, no superoxides are present to the degree they are present in the NVG group, enabling the L-ascorbic acid to eliminate superoxides and resulting in the detection of AFRs.
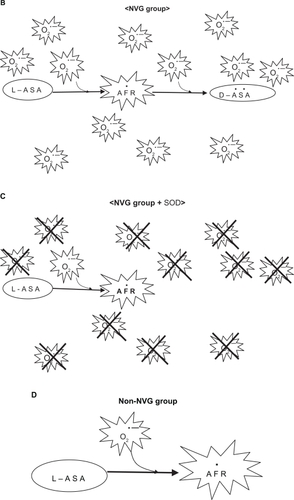
AFR was detected in the non-NVG group. Since super-oxide scavengers such as SOD, L-ascorbic acid, and GSH function in the aqueous humor of this group, superoxide was not present to the degree they were present in the NVG group, which enabled L-ascorbic acid to eliminate superoxides, resulting in the detection of AFR by ESR (). Ferreira et alCitation3 reported that the total levels of antioxidants in the aqueous humor decreased in POAG compared with eyes with cataracts, resulting in damage due to oxidative stress. Since SOD and Gpx activities increased without change catalase, there may have been a decrease in other antioxidants in the form of L-ascorbic acid and GSH. In the current study, since AFR were detected in all subjects in the non-NVG group, a decrease in L-ascorbic acid and GSH caused by the conversion of L-ascorbic acid to an AFR agreed with the total decrease in the levels of antioxidants reported by Ferreira et al.Citation3 Babizhayev and BuninCitation5 reported increased levels of lipid peroxides in the aqueous humor, trabecular meshwork, and Schlemm’s canal in POAG compared with control eyes, and suggested that lipid peroxidation was responsible for destruction of the trabecular meshwork and Schlemm’s canal. In addition, Bunin et alCitation6 reported that destruction of the drainage system in POAG is accelerated by lipid peroxidation. Yan et alCitation7 reported that hydrogen peroxide (H2O2) of a reactive oxygen is present in the aqueous humor and affects the drainage function of the aqueous humor in various animal experiments. After examining the damage to this drainage function caused by peroxidation of aqueous humor in an experiment in which the aqueous humor in porcine eyes was refluxed with 3 mM H2O2, Yan et al reported that although drainage increased at a normal ocular tension of 7.5 mmHg, drainage decreased at high ocular tension of 30 mmHg.
In the current study, although the involvement of H2O2 can be excluded because no changes were observed after catalase was added, lipid peroxidation might have been accelerated by superoxides that formed in the NVG group, which in turn might have induced destruction of the trabecular meshwork, Schlemm’s canal, and other components of the drainage system. On the other hand, active oxygen has been reported to be involved in vascularization. In the vitreous, we reported that low levels of superoxide scavenging activity, L-ascorbic acid and GSH are present, but there are high levels of lipid peroxides and H2O2 levels in diabetic retinopathyCitation2 and that there is a correlation between vascular endothelium growth factors and hydrogen peroxide in proliferative diabetic retinopathy.Citation8 Consequently, the superoxide detected in the aqueous humor of the NVG group in the current study might have been involved in vascularization of the anterior chamber of subjects of the NVG group as well. It is necessary to conduct additional studies that include are larger number of subjects.
Acknowledgements
The authors wish to thank Prof. Makoto Chikuda, Associate Prof. Koji Kadoya, and Dr. Tetsuya Mutou, Department of Ophthalmology, and Ms Yumiko Sumioka, Department of Clinical Research, Dokkyo Medical University Koshigaya Hospital, for supporting this study. The measurements in this study were performed at Koshigaya Division of Clinical Research, Institute for Medical Science, Dokkyo Medical University Koshigaya Hospital.
Disclosure
The authors have no proprietary interest in any aspect of this report.
References
- VinsonJAOxidative stress in cataractsPathophysiology20061315116216765571
- LinJTanakaYAraiKCopper ions and peroxidative reactions in the vitreous bodies of patients with diabetic retinopathyFocus Diabetic Retinopathy199855559
- FerreiraSMLernerSFBrunziniREvelsonPALlesuySFOxidative stress markers in aqueous humor of glaucoma patientsAm J Ophthalmol2004137626914700645
- FongDEtzelKLeePFLinTYLamKWFactors affecting ascorbate oxidation in aqueous humorCurr Eye Res198763573613105963
- BabizhayevMABuninA YaLipid peroxidation in open-angle glaucomaActa Ophthalmol (Copenh)1989673713772801038
- BuninAIBabizhaevMASuprunAVParticipation of the lipid peroxidation process in the destruction of the drainage system of the eye in open-angle glaucomaVestn Oftalmol198510113164002445
- YanDBTropeGEEthierCRMenonIAWakehamAEffects of hydrogen peroxide-induced oxidative damage on outflow facility and washout in pig eyesInvest Ophthalmol Vis Sci199132251525201869406
- MatsumotoYTakahashiMOgataMRelationship between glycoxidation and cytokines in the vitreous of eyes with diabetic retinopathyJpn J Ophthalmol20024640641212225819