Abstract
A theoretical model demonstrates the influence of the globe’s size on the effects of its intraocular pressure (IOP) and on its motility. Large globes seem more susceptible to the damaging consequences of elevated IOP, and move with greater difficulty than small ones. Routine measurement of axial length (AxL) may accordingly enhance precision in the diagnosis and management of glaucoma and strabismus.
Introduction
As instruments for estimating the globe’s size by measuring its axial length (AxL), mostly by ultrasonography, have become more readily available and user friendly (CitationKushner 2006), it seemed beneficial to briefly explore their utility in the diagnosis and treatment of glaucoma and strabismus with the aim of promoting their routine employment on the way to enhancing quality of care. Size being a geometrical entity, and pressure and motility being physical ones, the following meta-analysis focuses mainly on these disciplines as a starting point and foundation for ultimate clinical application, recognizing full well the limitation of physical models representing complex biological events.
Terms and definitions
Axial length denotes here the linear distance clinically measured from the anterior apex of the cornea to the anterior surface of the opposite retina. Addition of the thickness of the retina and sclera renders the actual geometrical distance about 1–1.5 mm longer, but because of the higher curvature of the cornea the average external diameter of the entire sphere is about 0.5 mm shorter than this. For purposes of physical analysis we accept Duke-Elder (1973, p. 97–99): “On the whole it [the eye] is approximately spherical except in the higher degrees of axial myopia when the sagittal diameter is greatest.” Only the principal forces, and ocular movements in abstract horizontal and vertical meridians, are here considered.
Acrophthalmos means here an abnormally long globe, similar to acrocephalos (long head) or acromphalos (long navel). Brachomphalos is a short globe, similar to brachycephalos and brachydont (short tooth). These terms, measured in millimeters, replace here myopia and hyperopia which were often used to designate the globe’s size, because the latter are measured in optical units of diopters, and do not always relate to size, as Priestly Smith said (1891, p. 122): “Small eyes are not necessarily hypermetropic, and hypermetropic eyes are not necessarily small.” For instance, the terms “Myopic disc” or “Myopic degeneration with retinal detachment” actually referred to physically long globes rather than near-sighted ones (CitationSoheilian et al 2007), while Hyperopia as a risk factor in angle closure (CitationLowe 1969), or in esodeviation, implied short globes. Furthermore, studies that related glaucoma to “myopia” did not usually distinguish between refractive myopia and axial myopia, an important determinant of the tonometric pressure reading in these two forms (CitationMitchell et al 1999; CitationGrodum et al 2001).
Intraocular pressure (IOP) is here given in ‘units’ instead of the wishful ‘mm Hg’ because the clinical tonometric measurements are not direct manometric ones but merely estimates which vary according to the instrument used and to the globe’s physical structure. Precise language is of relevance when communicating clinical or other precise data (CitationCrooke 1981).
Intraocular pressure
The newborn’s globe is soft and small, growing larger as its IOP increases with the begining of aqueous humor production (CitationKinsey 1945). Some have therefore seen the IOP as the impetus to the globe’s growth (similar to an inflating balloon) or to its excessive growth that leads to axial myopia (CitationBarraquer 1971; CitationGraul et al 2002). With increased volume the globe’s coats also become thinner.
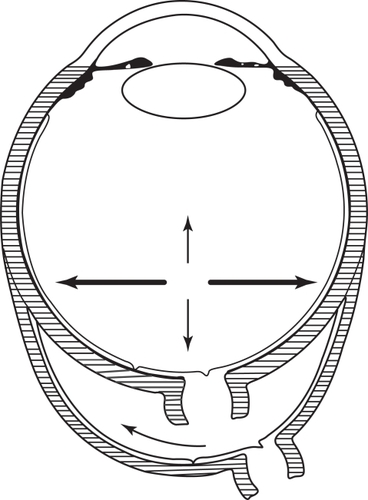
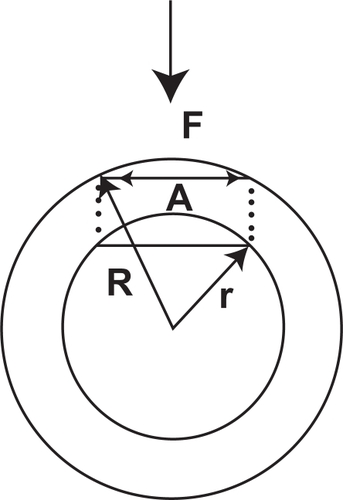
By definition, pressure (P) is directly proportional to its generating force (F) and inversely proportional to the surface area (A) to which it is applied perpendicularly: P = F/A. Goldmann chose for his tonometer a constant area of applanation where resistance of the average cornea to the applanating force was conteracted by the attractive force of the average tear film. Nevertheless, the force needed to applanate the flatter area of a large globe is smaller than the one needed for the steeper cornea of a small globe, where the volume displaced is also relatively larger (), (CitationMark 1973).
Figure 1 A smaller force (F) is needed to applanate the same area (A) in a larger globe (R) than a smaller one (r).
Laplace’s equation applies these circumstances specifically to elastic spheres, such as the growing globe: P = 2T/r, where T denotes the tangential (not perpendicular) shearing stress on the surface, and r stands for the radius, that is, the size of the sphere (CitationSzczudlowski 1979; CitationCahane and Bartov 1992). It follows that for a given pressure P, its effect on stretching the sclera or retina is greater in a large globe [2T = Pr] than a small one, whereas at the same time the perpendicularly applied counter-pressure diminishes.
When Jonas CitationFriedenwald (1937) began researching calibration of impression tonometers (Schiotz) he introduced an equation for ‘scleral rigidity’ where the tonometric reading was inversely proportional to ocular volume, the larger the globe the lower the reading on the tonometer for the same intraocular force (CitationWeekers and Grieten 1964). The value of the coefficient itself was found to be considerably reduced in high axial myopia (acrophthalmia) (CitationDraeger 1966). Lower tonometric readings in high volume globes were then discovered also with the applanation method (CitationLeighton 1974). In 513 adult eyes we found a 0.29 unit (“mmHg”) decrease in tonometric reading for every one millimeter increase in axial length, and the 30 longest eyes were over 1 unit softer than the 30 shortest ones (CitationMark et al 2002).
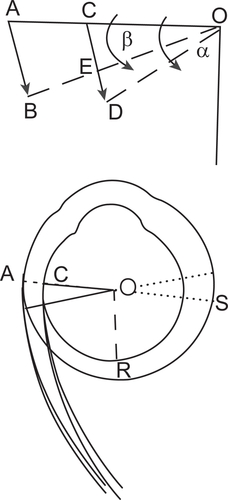
When pressure in a container of any shape is increased, it assumes the form of a sphere because a sphere contains the maximum volume under the minimum surface area. Therefore, as the IOP in en elongated ellipsoid globe is directed towards forming it into a sphere, it is more effective on the lateral walls than on the anterior-posterior axis (); it thus stretches the retina in the fundus, as manifested by the myopic (acrophthalmic) cup and crescent (CitationCurtin and Karlin 1971) and distorted brightness distribution (CitationWestheimer 1968). For the same reason it is also easier to indent or applanate an ellipsoid shape, where there is room for expansion, than an already spherical one (CitationMark 2002). Acrophthalmic globes are in this manner exposed to triple jeopardy of damage due to increased IOP: 1.) According to Laplace the force of stretch on the surface is higher in larger globes. 2.) It is also higher in elongated globes. 3.) The tonometric reading is deceptively low. All this, not counting the as yet in vivo unmeasurable malleability or elasticity of the ocular coats. The fact that increased IOP was the cause of the glaucomatous visual-field defect was convincingly shown experimentally (CitationGafner and Goldmann 1955).
On the other hand, smaller and shorter globes are at risk for angle-closure and acute glaucoma (CitationLowe 1969). Our study confirmed that the globes of women were over one millimeter shorter than those of men, and women are well known to be affected by acute angle-closure more often than men.
Knowledge of AxL may thus clinically alert us to the potential for angle closure, suggesting provocative tests or peripheral iridotomy in short globes. Their higher tonometic record may partially explain “ocular hypertension”. Large globes caution us to be vigilant to visual-field loss caused by deceptively low tonometric readings (“low/normal tension glaucoma”). Additional in vivo data of scleral thickness promises to further our knowledge on the effect of IOP and its measurement.
Ocular motility
“Near-sighted eyes often have limited motility”, said Helmholtz, who gave his own horizontal range of motion as 100° and vertically 90°. Having mentioned earlier that myopic eyes are longer, he must have meant acrophthalmic eyes rather than refractive “myopes” (CitationHelmholtz 1896). Southall called them “sluggish” (CitationSouthall 1937). This motility deficit is somewhat ameliorated by the enlarged visual-field due to the prismatic effect of corrective concave glasses (but not contact-lenses).
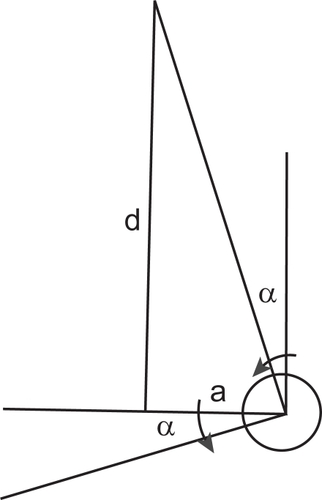
In order for a large globe to rotate a certain angle β (, top) its surface at A is moved a certain distance AB (The small amounts under consideration here minimize the difference between arc and chord values). However, an equally large displacement on a smaller globe (CD = AB) results in a larger angle α of rotation (α > β). Conversely, when both globes need rotate an equal angle (say β) the surface of the larger one moves a longer distance than the smaller (AB > CE). The angle of rotation is proportional to the distance that the end-point A or C is moved and to the length of the radius OA or OC, where AB/OA = tangent β. That is, in order to rotate a globe a given angle, its surface must move the farther the longer its radius (AxL, size).
Figure 3 Schematic representation of moving forces acting on the surface of globes of different size.
We deal here with basic kinematics rather than the more complex dynamics. There, Archimedes’ principle of the lever would also apply, where for equal displacements a stronger force is required at the end of a shorter lever OC than a longer one OA. The effect of the rotational force depends therefore not only on the force of the muscle’s contraction and its length but also on the length of the rotated arm – the globe’s size (CitationGillies 1984).
A numeric example may illustrate the theoretical principle. In order to focus at a normal reading distance (d) of say 13” (330 mm), each eye separated by a normal papillary distance of 60 mm (2a) must rotate inward at an angle α of about 5° (): a/d = 30/330 = 0.09; tan 0.09 = 5°. In order for small globes with a radius of say 11 mm (AxL about ∼22 mm) to converge this amount, their medial surfaces at C must move backwards almost 1 mm (CE, ) [CE = 11 × tan 5° = 1]. This surface of larger globes, with a radius of say 16 mm (AxL ∼ 32), must recede approximately 1.5 mm to achieve the same result [AB = 16 × tan 5° = 1.5], an increase of almost 50%. The opposite side of the globes (at S) must of course advance in the opposite (forward) direction.
When converging to a given near point, a pair of large globes must move farther than smaller ones, or, the stimulus for their convergence must be stronger (assuming equally strong muscles). With equal stimuli, the large eyes (often myopic) will show convergence insufficiency, a common clinical occurrence. For the same reason, small globes (often hyperopic) may exhibit excessive convergence at near, or esophoria. In cases of significant disparity in size of the same pair (“anisometropia”) the smaller eye may overshoot its target, or the larger one will be deficient, solely by dint of their different sizes, no matter what their refractive or accommodative status. Recognizing at the same time that the accuracy of focusing at near depends on a number of other hard to measure and complex psychophysical factors of space perception, aside from simple mechanical and optical ones (CitationMark 1962).
The clinical applicability of these principles to surgery, which is more an art than science, has been well covered in the literature (CitationGillies 1982; CitationKushner and Vrabec 1987; CitationKushner 1993). It is limited by the complex anatomical circumstances and functional variations (CitationMiller 1989). Furthermore, in pediatric patients Axl measurements are difficult and the globe grows with age. Therefore “Experienced surgeons will establish their own ‘tables’ for the amount they will recess or resect a muscle for a certain measured deviation” (CitationWagner 2005). Nevertheless, “We agree with Kushner et al that despite the approximation involved, the use of A scan is superior to other methods of estimating the amount of extraocular muscle surgery required” (CitationGillies 1991). “A statistically highly significant negative correlation was found between the axial length and the response to strabismus surgery” (CitationKrzizok 1994), that is, the larger the globe the smaller the response to the same surgery.
Suppose one wished to straighten an eye diagnosed with esotropia of 20 prism diopters (∼10°). If its AxL were about 22 mm, the medial rectus ought to be theoretically recessed 2 mm, and the lateral advanced (or shortened) 2 mm. If, however, AxL was 32 mm, the displacement of the insertions must measure almost 3 mm in order to achieve the same effect, for 2 mm of surgery will result in under correction.
In conclusion, I have tried to impress upon the reader the significant influence of globe size, measured by its axial length, on the effects and measurement of its intraocular pressure and on its motility. The geometrical and physical models serve as simplified skeletons upon which the complex biological components of anatomy, neurology, and biochemistry may then be fleshed. Future statistical data on the relation of AxL to eso and exo deviation, in addition to the customary refractive data, will be helpful. So may be in vivo data on scleral thickness. At present, the routine addition to our clinical armamentarium of measurable Axl data promises to enhance the quality of our diagnosis and management of glaucoma and of strabismus.
References
- BarraquerJIVarasJMJr1971Annotations concerning the relation of forces and pressure in eyes during physical growthAnn Ophtalmol34257
- CahaneMBartovE1992Axial length and scleral thickness effect on susceptibility to glaucomatous damage: a theoretical model implementing Laplace’s lawOphthalmic Res2428041475075
- CrookeCP1981Communication in ophthalmologyTrans Ophthalmol Soc UK10240921
- CurtinBJKarlinBD1971Axial length measurements and fundus changes of the myopic eyeAm J Ophthalmol7142535099937
- DraegerJ1966TonometryNew YorkHafner Publishing Co
- Duke-ElderS1973The centre of rotaion In: System of Ophthalmology6St LouisCV Mosby979
- FriedenwaldJS1937Tonometer calibrationAm J Ophthalmol209851024
- GafnerFHGoldmannH1955Experimentelle Untersuchungen über Zusammenhang von Augendrucksteigung und GesichtsfeldschädigungOphthalmologica1303576113297345
- GilliesWEMcIndoeA1982The use of ultrasonography in determining the amount of extraocular muscle surgery in strabismusAus J Ophthalmol101914
- GilliesWEHughesA1984Results in 50 cases of strabismus after graduated surgery designed by A sacn ultrasonographyBr J Ophthalmol6879056388626
- GilliesWEBrooksAMV1991Strabismus surgery landmarks and axial lengthOphthalmology9817551812887
- GraulTAKimCSAlwardWL2002Progressive axial myopia in a juvenile patient with traumatic glaucomaAm J Ophthalmol133700211992870
- GrodumKHeijlABengtssonB2001Refractive error and glaucomaActa Ophthalmol Scand79560611782219
- HelmholtzH1896Handbuch der Physiologischen Optik2nd edHamburgVoss615
- KinseyVA1945Development of secretory function of ciliary bodyArch Ophthalmol344158
- KrzizokTGrafMKaufmannH1994Effect of bulbus length on reduction of squint angle after suture fixationOphthalmologe9168768173254
- KushnerBFisherMLuccheseNMortonG1993Factors influencing response to strabismus surgeryArch Ophthalmol1117598424728
- KushnerBJLuccheseNJMortonGV1991Variation in axial length and anatomical landmarks in strabismus patientsOphthalmology9840062023763
- KushnerBJ2006Perspective on strabismusArch Ophthalmol1241321616966628
- KushnerBJVrabecM1987Theoretical effects of surgery on length tension relationships in extraocular musclesJ Pediatric Ophthalmol2412631
- LeightonDA1974Der modifizierende Einfluss der Augapfelgrösse bei KlaukomenKlin Monatsbl Augenheilk1644758
- LoweRF1969Corneal radius and ocular correlations: in normal eyes and eyes with angle-closure glaucomaAm J Ophthalmol6786485785849
- LeydheckerW1960Statistisch oder individuell “normal”In: Glaukom BerlinSpringer
- MarkHH1973Corneal curvature in applanation tonometryAm J Ophthalmol7622344725005
- MarkHHRobinsKPMarkTL2002Axial length in applanation tonometryJ Cataract Refract Surg28504611973098
- MarkHH2002Myopia and glaucomaActa Ophtalmol Scand802301
- MarkHH1962On the accuracy of accommodationBr J Ophthalmol663941
- MillerJM1989Functional anatomy of normal human rectus musclesVision Res29223402800349
- MitchellPHourihanFSandbachJ1999The relationship between glaucoma and myopia: the Blue Mountain Eye StudyOphthalmology1062010510519600
- PhillipsCIQuickMC1960Impression tonometry and the effect of eye volume variationBr J Ophthalmol441496314432607
- SmithP1891On the pathology and treatment of glaucomaLondonJ & A Churchill
- SoheilianMGhaseminejadAKYazdaniS2007Surgical management of retinal detachment in highly myopic eyes with macular holeOphthalmic Lasers Imaging381522
- SouthallJPC1937Physiological OpticsNew YorkDover135
- SzczudlowskiK1979Glaucoma hypothesis: Application of the law of LaplaceMed Hypotheses54816459994
- WagnerR2005Surgical management of strabismus In: Harley’s Pediatric Ophthalmology5th edPhiladelphiaLippincott Williams & Wilkins1979
- WeekersRGrietenJ1964Coefficient de rigidité ou coefficient de capacité oculaire?Ophthalmologica147677314113268
- WestheimerG1968Entopic visualization of Stiles-Crawford effectArch Ophthalmol7958485646037