Abstract
The lower eyelid retractors consist of double layers, the posterior layer of which is the main tractional component. Therefore, shortening of the posterior layer of the lower eyelid retractors causes lower eyelid retraction or cicatricial entropion. Based on this concept, we report a modified lower eyelid lengthening surgery involving complete recession of the posterior layer of the lower eyelid retractors by way of a transcutaneous approach that leaves the palpebral conjunctiva intact and inserts ear cartilage as a rigid spacer between the lower edge of the tarsal plate and the recessed anterior layer of the lower eyelid retractors. This procedure completely extirpated the preoperative maladjusted states of lower eyelid retraction and cicatricial entropion. Our procedure also prevented postoperative discomfort of the ocular surface due to the intact palpebral conjunctiva. As well, lower eyelid mobility and contour were good and within their respective permissible ranges. The lower eyelid lengthening surgery focusing on the posterior layer of the lower eyelid retractors using auricular cartilage via a transcutaneous approach is a useful procedure for lower eyelid retraction or cicatricial entropion.
Introduction
Shortening of the posterior lamella of the lower eyelid causes lower eyelid retraction (CitationHenderson 1965; CitationHarvey and Anderson 1981; CitationBaylis et al 1985; CitationBartley and Kay 1989; CitationKerstern et al 1990; CitationCohen and Shorr 1992; CitationGardner et al 1992; CitationOlver et al 1998; CitationFay et al 2001; CitationWearne et al 2001; CitationMoon et al 2005; CitationPatel et al 2005) or entropion (CitationBartley and Kay 1989; CitationCohen and Shorr 1992; CitationGoldberg et al 1999), for which the shortened posterior lamella needs to be lengthened for treatment (CitationHenderson 1965; CitationHarvey and Anderson 1981; CitationBaylis et al 1985; CitationBartley and Kay 1989; CitationKerstern et al 1990; CitationCohen and Shorr 1992; CitationGardner et al 1992; CitationOlver et al 1998; CitationGoldberg et al 1999; CitationFay et al 2001; CitationWearne et al 2001; CitationMoon et al 2005; CitationPatel et al 2005). The posterior layer of the lower eyelid retractors has to be targeted then because it represents the site of the pathology of such diseases (CitationKakizaki et al 2006a). Although the lower eyelid retractors were originally thought to consist of a complicated single layer (CitationHawes and Dortzbach 1982), they have now been revealed to be composed of a definite double layer (CitationKakizaki et al 2006a), consisting of anterior and posterior layers. The posterior layer, which is comprised of dense fibers of the capsulopalpebral fascia with scattered smooth muscle fibers and continues to the tarsus, is the main tractional component of the lower eyelid retractors (CitationKakizaki et al 2006a). Surgical operations targeting the posterior layer of the lower eyelid retractors for involutional lower eyelid entropion (CitationKakizaki et al 2007a) or reverse ptosis (CitationKakizaki et al 2007b), the pathologies of which are in the lower eyelid retractors, have been reported with good results.
The transconjunctival approach has been always taken in lower eyelid lengthening surgeries (CitationHenderson 1965; CitationHarvey and Anderson 1981; CitationBaylis et al 1985; CitationBartley and Kay 1989; CitationKerstern et al 1990; CitationCohen and Shorr 1992; CitationGardner et al 1992; CitationOlver et al 1998; CitationGoldberg et al 1999; CitationFay et al 2001; CitationWearne et al 2001; CitationMoon et al 2005; CitationPatel et al 2005; CitationBen Simon et al 2006). The shortened posterior lamellae of the lower eyelid retractors can be lengthened by spacer techniques (CitationBaylis et al 1985; CitationBartley and Kay 1989; CitationKerstern et al 1990; CitationCohen and Shorr 1992; CitationGardner et al 1992; CitationGoldberg et al 1999; CitationFay et al 2001; CitationWearne et al 2001; CitationMoon et al 2005; CitationPatel et al 2005; CitationBen Simon et al 2006) or nonspacer techniques, such as recession, tenotomy or extirpation of the lower eyelid retractors (CitationHenderson 1965; CitationHarvey and Anderson 1981; CitationOlver et al 1998). Since the latter techniques have limited indications (CitationOlver et al 1998; CitationWearne et al 2001) because of their lack of rigidity or postoperative fibrous contracture, spacer techniques are usually selected (CitationCohen and Shorr 1992; CitationOlver et al 1998; CitationWearne et al 2001). The hard palate mucosa and nasal turbinate mucosa are often used as autologous spacers (CitationBartley and Kay 1989; CitationKersten et al 1990; CitationCohen and Shorr 1992; CitationWearne et al 2001; CitationPatel et al 2005; CitationBen Simon et al 2006), since they have a mucosal surface of appropriate rigidity (CitationCohen and Shorr 1992; CitationWearne et al 2001). Although keratinization can occur, it only irritates the ocular surface (CitationKersten et al 1990; CitationBen Simon et al 2006; CitationCohen and Shorr 1992). As an alternative material, ear cartilage is sometimes used via a transconjunctival approach (CitationBaylis et al 1985; CitationMoon et al 2005), and some of this remains exposed and requires removal (CitationKersten et al 1990). Although acellular human dermis is sometimes used as a substitution for autologous materials, evaluations of its use are not consistent because of a tendency to contract (CitationSullivan and Dailey 2003; CitationLi et al 2005). In many cases, the transconjunctival approach for lower eyelid lengthening is not suitable for maintaining a stable environment of the ocular surface. Successfully keeping the palpebral conjunctiva intact, namely a trans-cutaneous approach, is essential for maintaining a sound ocular surface environment.
In the present study, we report a modified lower eyelid lengthening surgery that completely recesses the posterior layer of the lower eyelid retractors by way of a transcutaneous approach to keep the palpebral conjunctiva intact. Ear cartilage is inserted between the lower edge of the tarsal plate and the recessed anterior layer of the lower eyelid retractors. We used ear cartilage as a rigid spacer (CitationOlver et al 1998) since it does not produce any exudates or keratin, whereas hard palate mucosa does (CitationCohen and Shorr 1992) and so is not suitable for confined spaces.
Patients and methods
The outcomes of patients receiving lower eyelid lengthening surgery between 2005 and 2006 were reviewed, as a retrospective case series, from clinical records held at the Department of Ophthalmology, Aichi Medical University. A total of 6 lower eyelids in 5 patients were then included in the study. The average age of the patients was 41.5 years (range: 24–79 years).
Indications for the surgery are thyroid-related lower eyelid retraction and cicatricial lower eyelid entropion, the pathological foci of which are in the lower eyelid retractors. Cases without pathological foci in the lower eyelid retractors, such as marginal entropion or compromised orbicularis action, were not included in this study.
Preoperative data of lower eyelid retraction patients are shown in . The position of the lower eyelid was measured relative to the lower corneal limbus in the primary position of gaze. Overall, 3 eyelids in 2 patients with thyroid-associated ophthalmopathy (TAO) showed lower eyelid retractions with entropion. Of these 2 patients, 1 (bilateral 3-mm retraction) demonstrated proptosis (19 mm OU) after a repeated modified Hotz procedure for lower eyelid entropion (CitationDuke-Elder SS and MacFaul PA 1976). Modified Hotz procedure is used for entropion surgeries in which, via a trans-cutaneous incision, the pretarsal part of the orbicularis oculi muscle and the lower edge of the tarsus are sutured to evert the lower eyelid margin. On the other hand, the other patient (5-mm right and 4-mm left retractions) showed proptosis (26 mm OU) after right-sided twice-repeated modified Hotz procedures for lower eyelid entropion (CitationDuke-Elder SS and MacFaul PA 1976). Despite the large amount of proptosis, this patient chose not to undergo orbital decompression and so only underwent an operation on the right lower eye-lid. As well, 1 left eyelid in 1 patient without proptosis (16 mm OU) showed a simple lower eyelid retraction after an earlier surgery for a squint (inferior rectus muscle recession) (CitationWearne et al 2001) due to an eye movement disorder caused by TAO. The other 2 right eyelids each had cicatricial entropion after repeated modified Hotz procedures for lower eyelid entropion (CitationDuke-Elder SS and MacFaul PA 1976).
Table 1 Preoperative data of lower eyelid retraction patients
The lower eyelid mobility during a downward gaze and the contour of the lower eyelids were also estimated. Clinical data of the lower eyelid retraction cases were analyzed by Wilcoxon signed ranks test using the SPSS software 8.0 (SPSS, Chicago, Illinois). Statistical significance was defined as P < 0.05.
Surgical technique
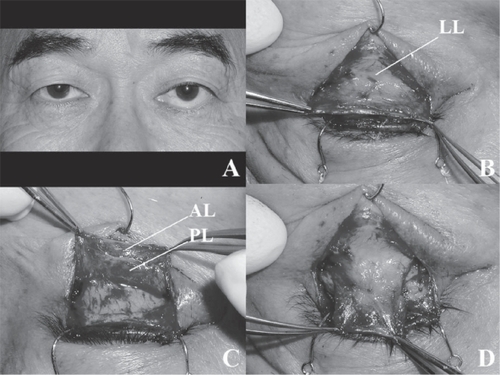
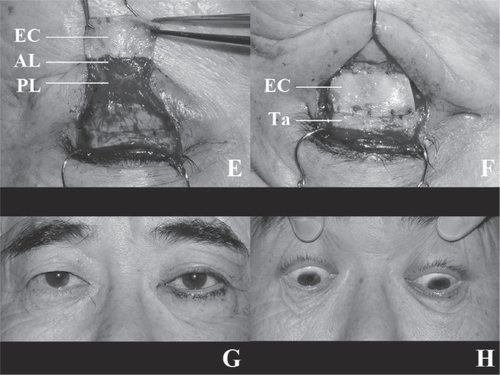
Details of our operative methods for the exposure of the sheet-like lower lid retractors have been reported elsewhere (CitationKakizaki et al 2005, Citation2007a); actually as described for involutional entropion repair. For a retracted lower eyelid (), first, local anaesthesia was performed with 2 ml of 2% lidocaine and epinephrine (1:100,000 dilution). After exposing the retractors as much as possible (), the double layers of the retractors were clearly discerned (). In the cases here, the posterior layer of the lower eyelid retractors was always shrunken toward the orbit. Next, the lateral and medial horns of the lower eyelid retractors were incised at a width of 17 mm to disconnect the traction via the horns (). The harvested auricular cartilage was then interposed between the lower edge of the tarsus and the distal edge of the anterior layer of the lower eyelid retractors, while the posterior layer remained unfixed to any structures (). The cartilage was fixed with 5 sutures on each of the distal and proximal sides (). The volume of harvested auricular cartilage for the retraction patients was twice that of the retraction from the lower corneal limbus (CitationKersten et al 1990) with 1 mm of extra volume in the proximal and distal margins, respectively, for sutures, while the height of the harvested auricular cartilage for the entropion patients was 4 mm (CitationCohen and Shorr 1992) (horizontal length in both groups was always constant at 17 mm). At the end of the procedure, the pretarsal orbicularis oculi muscle and the lower edge of the tarsus were secured at three points, which were permanently confined so that they did not touch the cilia on the ocular surface. The skin was sutured with interrupted 6–0 nylon sutures (); after which two tarsorrhaphy sutures were placed (CitationFeldman et al 1992; CitationMcInnes et al 2006).
Figure 1 Figure 1A A 3-mm left lower eyelid retraction caused by previous surgery for a squint (inferior rectus muscle recession) is shown.
Figure 1B The anterior surface of the lower eyelid retractors is shown. Part of the Lockwood ligament can be seen.
Figure 1C The posterior surface of the lower eyelid retractors is shown. The double layers of the retractors can be clearly discerned. The posterior layer of the lower eyelid retractors is always shorter than the anterior layer.
Figure 1D The lateral and medial horns of the lower eyelid retractors are incised at the width of 17 mm.
Figure 1E The harvested auricular cartilage is interposed between the lower edge of the tarsus and the distal edge of the anterior layer of the lower eyelid retractors while the posterior layer remains unfixed to any structure. The volume of the harvested cartilage for the retraction patients is twice the retraction from the lower corneal limbus with 1 mm of extra volume in the proximal and distal margins, respectively, for sutures. The height of the harvested cartilage for the entropion patients is 4 mm (horizontal length in both groups is always constant at 17 mm).
Figure 1F The cartilage is fixed with 5 sutures on each of the distal and proximal sides. The suture on the right upper edge is masked by the recessed anterior layer of the lower eyelid retractors in this image.
Figure 1G Sufficient elevation of the lower eyelid is shown. The skin is sutured with interrupted 6–0 nylon sutures.
Figure 1H The rehabilitated left lower eyelid moves down sufficiently during a downward gaze.
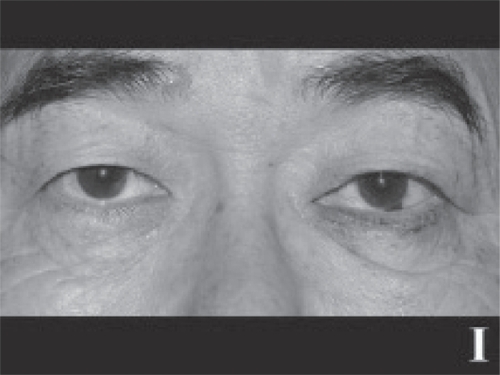
Figure 1I The contour of the left lower eyelid is within the permissible range.
Results
The retracted lower eyelids were all elevated successfully to around the lower corneal limbi, with an average elevation of 2.88 mm (). However, outcomes were not statistically significant (P = 0.066). The entropion eyelids were improved in all cases. Although the minimum observation period was 3 months (ranging up to 23 months, mean follow-up time: 11.6 months), no exacerbation of the lower eyelid retraction or recurrence of entropion occurred. The lower eyelid moved down sufficiently during a downward gaze () and the contour was within a permissible range (). Examples of preoperative and postoperative case photographs are shown in .
Figure 2 Figure 2A The patient shows 5-mm right and 4-mm left retractions from the lower corneal limbi with proptosis of 26 mm OU. Just the right lower eyelid took two Hotz procedures for the lower eyelid entropion.
Figure 2B After lower eyelid lengthening surgery, the right lower eyelid retraction and cicatricial entropion are sufficiently improved.

Table 2 Postoperative data of lower eyelid retraction patients
Discussion
The lower eyelid lengthening procedure described here was clearly shown to recess the main tractional component of the posterior layer of the lower eyelid retractors. The palpebral conjunctiva remained intact, which prevented any postoperative discomfort of the ocular surface. Lower eyelid mobility was good and the contour was within a permissible range. We utilised the concept of recession of the lower eyelid retractors (CitationHenderson 1965), in which a lack of rigidity or fibrous contracture (CitationOlver et al 1998) are the main causes of the recurrence of retractions or entropion. These adverse effects were overcome using the skeletal structure of ear cartilage. Since we aimed at complete nullification of the posterior layer of the lower eyelid retractors, the spacer was only sutured to the anterior layer of the lower eyelid retractors.
Detaching the lower eyelid retractors from the subjacent conjunctiva has been thought difficult (CitationJones 1968). Therefore, lower eyelid lengthening surgeries have, to date, been performed via a trans-conjunctival approach. This procedure has always been successful in recessing the posterior layer of the lower eyelid retractors, to which both structural and epithelial elements were reconstructed using a spacer (CitationOlver et al 1998; CitationFay et al 2001). However, not every spacer was suitable for the ocular surface due to keratinization or mechanical irritation (CitationKersten et al 1990), and so patients often experienced discomfort on the ocular surface. Although most of these adverse symptoms improved over the postoperative time course (CitationKersten et al 1990), patients were obliged to endure rather unpleasant conditions. We therefore believe that it is obviously logical not to harm the palpebral conjunctiva during recession of the lower eyelid retractors.
Auricular cartilage, which is hardly absorbed even in the long term (CitationOrtiz-Monasterio et al 1981), is seen as a desirable spacer in a confined space because it does not produce any exudates or keratin (CitationCohen and Shorr 1992). However, it can present some adverse effects via the transconjunctival approach (CitationKersten et al 1990). Since the harvested cartilage is resilient, it has a curved contour, and a shallow incision on the concave surface can increase its flexibility and allow it to be flattened (CitationMoon et al 2005). However, the margin of the cartilage is easily trimmed for fitting into the recipient bed (CitationMoon et al 2005). Although a lower eyelid with inserted ear cartilage have been thought to be immobile during a downward gaze (CitationKersten et al 1990; CitationWearne et al 2001; CitationMoon et al 2005), and to have an unnatural lid contour (CitationKersten et al 1990; CitationWearne et al 2001; CitationMoon et al 2005), none of the patients in the present study exhibited any of these adverse states. Thus, we believe ear cartilage is an appropriate material for lengthening lower eyelids.
The orbicularis action can cause lower eyelid entropion (CitationCollin and Rathbun 1978). That is, the pretarsal part of the orbicularis oculi muscle is always stable on the tarsus, but the preseptal part can move comparatively freely and override the pretarsal part (CitationKakizaki et al 2006b). The trans-cutaneous approach can prevent this overriding because of anterior cicatrisation. As well, fixing sutures between the tarsus and the pretarsal part of the orbicularis oculi muscle may help prevent the overriding of the preseptal part onto the pretarsal part. As anterior cicatrisation does not occur in the trans-conjunctival approach, the trans-cutaneous approach is more effective.
The scar might cause, however, further vertical traction on the lower eyelid and result in a less favorable outcome, because the main problem with trans-cutaneous lower eyelid surgery is scar formation in the anterior and middle lamellae of eyelids (skin, orbicularis and orbital septum) (CitationShorr and Fallor 1985; CitationShorr 1995). However, the operative invasion in the present procedure was essentially limited in the posterior lamella. As well, we did not remove any skin and did not dissect the layer between the orbicularis oculi muscle and the orbital septum, which enabled the anterior and middle lamellae to have an appropriate volume. In addition, the retracted or shortened posterior lamella was elongated by the auricular cartilage. For these reasons, we believe further vertical traction on the lower eyelid does not occur so severely as to affect the vertical lower eyelid height.
A midface lift with lateral canthal resuspension has recently been applied to lower eyelid retractions, such as in post-blepharoplasty, midface descent, and thyroid-related orbitopathy (CitationBen Simon et al 2006). It is important to note in the present procedure whether the anterior or middle lamella is targeted or not for therapy. Thyroid-related lower eyelid retraction, the main pathology for which is in the posterior lamella, is well treated by just our present procedure. As well, for entities including anterior and middle lamellae as well as the posterior lamella (CitationShorr 1995; CitationLi et al 2005), such as in post-blepharoplasty lower eyelid retraction, our procedure also can help improve the pathology, simultaneously with rehabilitation of the anterior and middle lamellae. However, the present procedure cannot be separately applied to the cases with just anterior or middle lamellar cicatrix (CitationShorr and Fallor 1985; CitationShorr 1995) because our method only targets the posterior lamellar pathology.
Because of the small sample size, statistically significant outcomes could not be demonstrated in this study. However, the lower eyelid lengthening procedure clearly elevated retracted or cicatricial lower eyelids, and improved cicatricial entropion. Lower eyelid lengthening surgery focusing on the posterior layer of the lower eyelid retractors using auricular cartilage insertion via a transcutaneous approach was shown to be a useful procedure for lower eyelid retraction or cicatricial entropion.
Disclosure
There is no financial support or interest related to this manuscript.
References
- BartleyGBKayPP1989Posterior lamellar eyelid reconstruction with a hard palate mucosal graftAm J Ophthalmol107609122729410
- BaylisHIPermanKIFettDR1985Autogenous auricular cartilage grafting for lower eyelid retractionOphthal Plast Reconstr Surg1237
- Ben SimonGJLeeSSchwarczRM2006Subperiosteal midface lift with or without a hard palate mucosal graft for correction of lower eyelid retractionOphthalmology11318697316884780
- CohenMSShorrN1992Eyelid reconstruction with hard palate mucosa graftsOphthal Plast Reconstr Surg818395
- CollinJRORathbunJE1978Involutional entropion. A review with evaluation of a procesureArch Ophthalmol96105864418757
- Duke-ElderSSMacFaulPA1976Abnormalities of the palpebral apertureSystem of Ophthalmology vol. XIII– The Ocular adnexaLondonHenry Kimpton57381
- FayAMPierothLRubinPA2001An animal model of lower eyelid spacer grafting with a cellular dermisOphthal Plast Reconstr Surg172705
- FeldmanKAPuttermanAMFarberMD1992Surgical treatment of thyroid-related lower eyelid retraction: a modified approachOphthal Plast Reconstr Surg827886
- GardnerTAKennerdellJSBuergerGF1992Treatment of dysthyroid lower lid retraction with autogenous tarsus transplantsOphthal Plast Reconstr Surg82631
- GoldbergRAJoshiARMcCannJD1999Management of severe cicatricial entropion using shared mucosal graftsArch Ophthalmol1171255910496405
- HarveyJTAndersonRL1981The aponeurotic approach to eyelid retractionOphthalmology88513246894973
- HawesMJDortzbachRK1982The microscopic anatomy of the lower eyelid retractorsArch Ophthalmol100131387103816
- HendersonJW1965Relief of eyelid retraction: A surgical procedureArch Ophthalmol742051614318497
- JonesLT1968A new concept of the orbital fascia and rectus muscle sheaths and its surgical implicationsTrans Am Acad Ophthalmol7275564
- KakizakiHZakoMMitoH2005Modified operation to correctly detect and fix the lower eyelid retractor in involutional entropionJpn J Ophthalmol49330216075339
- KakizakiHZhaoJNakanoT2006aThe lower eyelid retractor consists of definite double layersOphthalmology11323465016996613
- KakizakiHZhaoJZakoM2006bMicroscopic anatomy of asian lower eyelidsOphthal Plast Reconstr Surg224303
- KakizakiHZakoMKinoshitaS2007aPosterior layer advancement of the lower eyelid retractor in involutional entropion repairOphthal Plast Reconstr SurgIn press.
- KakizakiHZakoMIwakiM2007bReverse ptosis repair targeting the posterior layer of the lower lid retractorOphthal Plast Reconstr SurgIn press.
- KerstenRCKulwinDRLevartovskyS1990Management of lower-lid retraction with hard-palate mucosa graftingArch Ophthalmol1081339432400351
- LiTGShorrNGoldbergRA2005Comparison of the efficacy of hard palate grafts with acellular human dermis grafts in lower eyelid surgeryPlast Reconstr Surg116873816141830
- McInnesAWBurroughsJRAndersonRL2006Temporary suture tarsorrhaphyAm J Ophthalmol142344616876529
- MoonJWChoungHKKhwargSI2005Correction of lower lid retraction combined with entropion using an ear cartilage graft in the anophthalmic socketKorean J Ophthalmol19161716209275
- OlverJMRoseGEKhawPT1998Correction of lower eyelid retraction in thyroid eye disease: a randomised controlled trial of retractor tenotomy with adjuvant antimetabolite versus scleral graftBr J Ophthalmol82174809613385
- Ortiz-MonasterioFOlmedoAOscoyLO1981The use of cartilage grafts in primary aesthetic rhinoplastyPlast Reconstr Surg675976057232580
- PatelMPShapiroMDSpinelliHM2005Combined hard palate spacer graft, midface suspension, and lateral canthoplasty for lower eyelid retraction: a tripartite approachPlast Reconstr Surg11521051415923862
- ShorrNFallorMK1985“Madame Butterfly” procedure: combined cheek and lateral canthal suspension procedure for post-blepharoplasty, “round eye,” and lower eyelid retractionOphthal Plast Reconstr Surg122935
- ShorrN1995“Madame Butterfly” procedure: Total lower eyelid reconstruction in three layers utilizing a hard palate graft: Management of the unhappy post-blepharoplasty patient with round eye and scleral showInt J Aesthetic Restorative Surg3326
- SullivanSADaileyRA2003Graft contraction: a comparison of acellular dermis versus hard palate mucosa in lower eyelid surgeryOphthal Plast Reconstr Surg191424
- WearneMJSandyCRoseGE2001Autogenous hard palate mucosa: the ideal lower eyelid spacer?Br J Ophthalmol851183711567962