Abstract
A 70-year-old man with thyroid associated ophthalmopathy showed inflammatory swelling of the left inferior oblique muscle that was significantly improved by steroid pulse therapy and radiotherapy. Sagittal T2-weighted magnetic resonance images were useful to detect the lesion and to evaluate the effects of treatment.
Introduction
Inferior oblique muscle involvement in thyroid associated ophthalmopathy (TAO) has long been completely disregarded (CitationNugent et al 1990; CitationAydin et al 2003). However, such involvement has recently been reported (CitationKakizaki et al 2007). Although the case showed inflammation in the inferior oblique muscle, this appeared to be an old inflammation. Indeed, post-therapeutic improvement of the inflammation was a little difficult to judge from magnetic resonance imaging (MRI).
Here, we report a case of inferior oblique muscle involvement in TAO with typical inflammation, in which post-therapeutic improvement could easily be confirmed by MRI.
Case report
The chief complaint of a 70-year-old man presenting with TAO was diplopia. He was in an euthyroid state with increases of thyrotropin receptor antibody and thyroid-stimulating antibody. To evaluate an orbital inflammation, MRI was undertaken with a 1.5-Tesla system (GE SIGNA: GE Medical Systems, Waukeshaw, WI, USA) using a custom-designed 5 inch surface coil. Slice thickness was 3 mm, interslice gap 0.5 mm, and field of view 140 mm × 140 mm with a 256 × 192 matrix. Sagittal T2-weighted spin echo sequences (echo time, 80 ms; repetition time, 2,500 ms) sliced parallel to the optic nerve demonstrated swelling of the left inferior oblique muscle () compared with the contralateral homonymous muscle (). Coronal T2-weighted spin echo sequences () also showed this swelling, which was revealed as inflammatory by comparing coronal T1-weighted spin echo sequences (echo time, 12 ms; repetition time, 600 ms; ). As well as left inferior oblique muscle involvement, bilateral inferior () and medial rectus muscles (not shown) were enlarged.
Figure 1 Figures 1A, B, C Consecutive sagittal slices of the left orbit. Figure 1B is the slice in which both the inferior and the superior recti muscles are most clearly shown. Figure IA is one slice medial to Figure 1B, and Figure 1C is the slice lateral to Figure 1B. Swelling of the left inferior oblique muscle (IO) is shown on sagittal T2-weighted magnetic resonance imaging (MRI).The inferior rectus muscle (IR) is also enlarged. Figure 1C does not clearly show the inferior oblique muscle, but is presented for an easier understanding of the inferior oblique swelling in Figures 1A and B.
Figures 1D, E, F Consecutive sagittal slices of the right orbit. Figure 1E shows the slice in which both the inferior and the superior recti muscles are most clearly shown. Figure 1D is one slice medial to Figure 1E, and Figure 1F is the slice lateral to Figure 1E. The right normal sized IO is shown on sagittal T2-weighted MRI. However, the IR is slightly enlarged. Figure 1F does not clearly show the inferior oblique muscle, but it is presented for a comparison with Figure 1C.
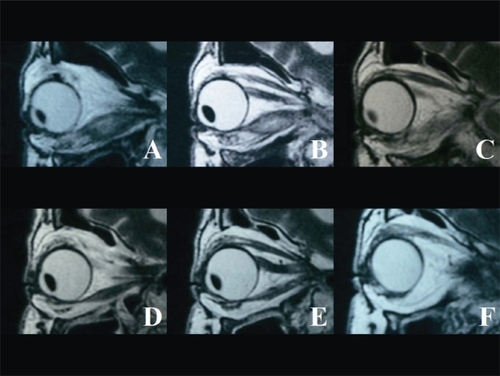
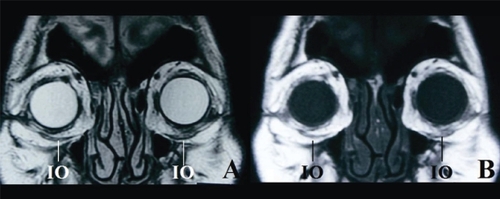
Figure 2 Figure 2A The left IO is inflamed and enlarged on coronal T2-weighted MRI. By comparing with Figure 2B, the inflammation can be clearly seen.
Figure 2B The swollen left IO includes some adipose tissue on coronal T1-weighted MRI.
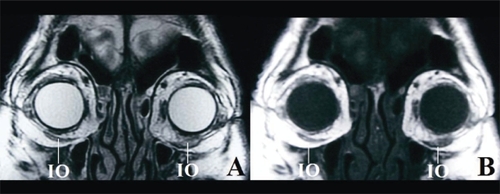
To reduce the inflammation from these involvements, steroid pulse therapy (500 mg/day methylpredonisolone for 3 days and repeated the following week) and radiotherapy (20 Gy over 10 days at 2 Gy/day) were instituted as treatment. One month after these treatments, sagittal T2-weighted images (T2WI; ) demonstrated the resolution of the inflammation in the left inferior oblique muscle simultaneously with decreased muscle size. The size of the contralateral homonymous muscle was not changed between prior and post therapy (). Coronal T2WI () and T1-weighted images () also illustrated the resolution of the left inferior oblique inflammation. The other muscular lesions were also improved, but the inflammation of the left inferior rectus muscle remained (figure not shown), resulting in the persistent diplopia.
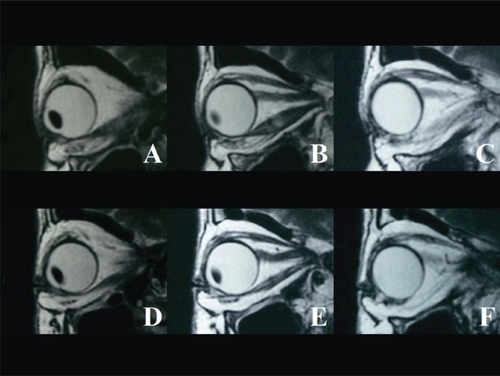
Figure 3 Figures 3A, B, C Consecutive sagittal slices of the left orbit. Figure 3B is the slice in which both the inferior and the superior recti muscles are most clearly shown. Figure 3A is one slice medial to Figure 3B, and Figure 3C is the slice lateral to Figure 3B. Resolved inflammation with simultaneous volume reduction of the inferior oblique muscle (IO) is illustrated on sagittal T2-weighted magnetic resonance imaging (MRI). Figure 3C does not clearly show the IO, but it is presented for an easier understanding of the IO swelling in Figures 3A and B.
Figures 3D, E, F Consecutive sagittal slices of the right orbit. Figure 3E is the slice in which both the inferior and the superior recti muscles are most clearly shown. Figure 3D is one slice medial to Figure 3E, and Figure 3F is the slice lateral to Figure 3E.The size of the contralateral IO is not changed between prior-and post-therapy on sagittal T2-weighted MRI. However, the inferior rectus muscle is slightly enlarged. Figure 3F does not clearly show the IO, but it is presented for comparison with Figure 3C.
Discussion
Extraocular muscle involvements are representative symptoms of TAO (CitationDickinson and Perros 2001), but inferior oblique muscle involvement has long been disregarded (CitationNugent et al 1990; CitationDickinson and Perros 2001; CitationAydin et al 2003). However, we recently reported a case of TAO with inferior oblique muscle involvement (CitationKakizaki et al 2007). Here, we presented another case involving inflammatory swelling of the inferior oblique muscle that significantly resolved after medical intervention.
Sagittal MRI images are useful to detect such lesions (CitationKakizaki et al 2007). Size differences were easily noticed by comparing the lesion with the contralateral homonymous muscle without swelling. The muscle swelling of the inferior oblique muscle could also be detected from careful observations of the coronal images, although sagittal T2WI can more clearly demonstrate a lesion of the inferior oblique muscle.
Ophthalmologists need to consider the possibility of inferior oblique muscle involvement in TAO.
Acknowledgements
The author greatly appreciates the assistance of Ryota Ohno (Department of Radiology, Aichi Medical University, Aichi, Japan) for interpretation of RMN data.
Disclosure
The authors have no financial support and interest related to this manuscript.
References
- AydinKGüvenKSencerS2003A new MRI method for the quantitative evaluation of extraocular muscle size in thyroid ophthalmopathyNeuroradiology451848712684723
- DickinsonAJPerrosP2001Controversies in the clinical evaluation of active thyroid-associated orbitopathy: use of a detailed protocol with comparative photographs for objective assessmentClin Endoclinol55283303
- KakizakiHZakoMIwakiM2007Thyroid associated inferior oblique myopathyOphthalmologyin press.
- NugentRABelkinRINeigelJM1990Graves orbitopathy: correlation of CT and clinical findingsRadiology177675822243967