Abstract
Purpose:
To report an unusual case of myopic peripapillary retinal detachment (PPRD) imaged by optical coherence tomography (OCT).
Methods:
Observational case report.
Results:
OCT showed a nonreflective space between the retinal pigment epithelium and the neurosensory retina with the presence of bridging tissue that could be defined as an outer retinal schisis, which is not typical of myopic PPRD.
Conclusion:
This case suggests that the spectrum of PPRD in pathological myopia may extend beyond that already described.
Introduction
Peripapillary retinal detachment (PPRD) can occur in a variety of diseases, including pathologic myopia, peripapillary choroidal neovascularization (idiopathic or secondary to other conditions such as age-related macular degeneration) and polypoidal choroidal vasculopathy. When associated with pathologic myopia, PPRD appears on fundus examination as a yellow-orange, well-defined dome-shaped lesion, which usually lies inferior to the optic disc; the visual symptoms are minimal, although perimetric defects may be present in as many as 71% of cases, and the evolution seems slow (CitationFreund et al 2003; CitationShimada et al 2006). Recently this condition has been imaged by optical coherence tomography (OCT), which disclosed a localized detachment of both the retinal pigment epithelium (RPE) and retina (CitationFreund et al 2003; CitationShimada et al 2006). The aim of this study was to describe a case of PPRD which showed unusual features.
Case report
A 38-year-old man came to us complaining of a relative scotoma in the visual field of his right eye. Best-corrected visual acuity was 20/25 OD (and 20/160 OS because of chorioretinal myopic atrophy). In the right eye the refractive error was −19 diopters and the axial length was 30.5 mm. On fundus examination and fluorescein angiography (FA), a perifoveal retinal hemorrhage was evident. The disc was tilted and surrounded by a yellow-orange, slightly elevated lesion, consistent with a PPRD, which hampered the visualization of the underlying choroidal vessels. On the nasal side of the optic disc a pale yellow round lesion, suggestive of RPE and choriocapillar atrophy, was present. The patient at that time did not undergo OCT. During the following six months the hemorrhage and the visual complaint progressively disappeared.
At fundus examination two years later, the peripapillary detachment was still evident, with no detectable enlargement (). When OCT was performed, a nonreflective space could be detected between the RPE and the neurosensory retina all around the optic disc. Such a space revealed some bridging tissue (probably Muller’s cells), which led us to classify it as an outer retinal layer schisis (). The nonreflective space extended temporally up to 1.1 mm from the fovea. No epiretinal membranes were detected. The scans crossing the optic nerve head confirmed the lack of an optic disc pit. Neither FA nor indocyanine green angiography (ICGA) disclosed any choroidal neovascularization.
Figure 1 Fundus photography with a line showing the OCT scan. The photograph demonstrates the presence of a tilted disc surrounded by a slightly elevated yellow-orange lesion, consistent with a PPRD, which hampered visualization of the underlying choroidal vessels.
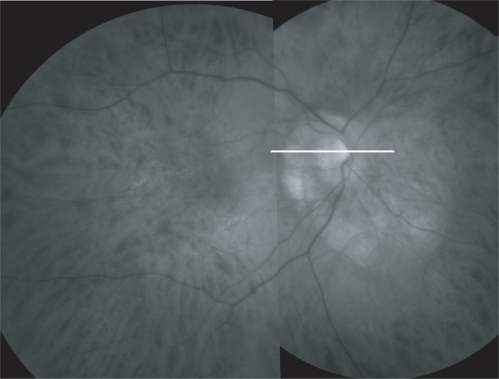
Figure 2 The OCT image of the right eye demonstrates the presence of a nonreflective space between the RPE and the neurosensory retina all around the optic disc. The presence of some bridging tissue (probably Muller’s cells) led us to classify it as an outer retinal layer schisis. No epiretinal membranes were detected. The scans crossing the optic nerve head confirmed the lack of an optic disc pit.

Discussion
Myopia-associated PPRD has been recently described as a distinct entity. Three papers have reported the OCT findings of such a condition (CitationFreund et al 2003; CitationToranzo et al 2005; CitationShimada et al 2006). CitationShimada and coauthors (2006) described the largest series (31 eyes): in all cases OCT revealed a localized detachment caused by fluid accumulation beneath both the neurosensory retina and the RPE. Previous case reports had already described similar findings. Although CitationToranzo and coauthors (2005) claimed significant differences when illustrating their case in comparison to those reported by CitationBailey Freund and coauthors (2003) (they also gave a different name to this condition: intrachoroidal cavitation), a careful analysis of the pictures that both groups published actually reveals quite similar features, including a localized detachment of the RPE and retina and a flat profile of the RPE. Fluorescein angiography (FA) also showed similar images, revealing among other things the lack of the early, localized hyperfluorescence that would be expected in case of RPE detachment.
On fundus examination the case herein reported was quite similar to those previously described, due to the presence of the peripapillary, slightly elevated yellow-orange lesion precluding visualization of the underlying choroidal vessels; the extension into the temporal and superior quadrants (in addition to the inferior one) has already been reported (CitationFreund et al 2003). OCT, however, provided quite a different picture. The detachment, in fact, was located between the neurosensory retina and the RPE, which was still in contact with the choroid. Given the presence of bridging tissue between the RPE and the neuroretina, it would seem more appropriate to define this space as an outer retinal schisis, which is not typical of myopic PPRD. Retinal schisis may be found in association with an optic disc pit, but in this case the inner retinal layers are usually involved (CitationRutledge et al 1996); since no optic disc anomalies were observed in our patient, we felt that this diagnosis could be reasonably ruled out. Outer retinal schisis can be observed in myopic macular retinoschisis, although in such a case the central macula is involved, not the peripapillary retina (CitationBenhamou et al 2002). Other conditions that need to be differentiated include all diseases likely to induce a peripapillary neuroretinal and/or RPE detachment in a young adult, such as peripapillary choroidal neovascularization (either idiopathic or secondary), polypoidal choroidal vasculopathy and central serous chorioretinopathy. All these conditions were ruled out by FA and ICGA.
In conclusion, this case suggests that the spectrum of PPRD in pathological myopia may extend beyond the already described picture of RPE detachment and/or intrachoroidal cavitation and include retinal alterations that closely resemble macular retinoschisis, but are located next to the optic disc.
References
- BenhamouNMassinPHaouchineB2002Macular retinoschisis in highly myopic eyesAm J Ophthalmol13379480012036671
- FreundKBCiardellaAPYannuzziLA2003Peripapillary detachment in pathologic myopiaArch Ophthalmol12119720412583785
- RutledgeBKPuliafitoCADukerJS1996Optical coherence tomography of macular lesions associated with optic nerve head pitsOphthalmology1031047538684793
- ShimadaNOhno-MatsuiKYoshidaT2006Characteristics of peripapillary detachment in pathologic myopiaArch Ophthalmol124465216401784
- ToranzoJCohenSYErginayA2005Peripapillary intrachoroidal cavitation in myopiaAm J Ophthalmol140731216226529