Abstract
Objective
Report the case of a patient with Crohn’s disease and ligneous conjunctivitis.
Methods
Interventional case report of a 27-year old female patient, with a 4-year history of Crohn’s disease, was seen for right eye conjunctival ulcer after resolved chemical trauma. Conjunctival biopsy was performed for histopathology, immunofluorescence microscopy, and immunohistochemistry testing.
Results
Microbiology tests were negative for bacteria and fungi. PCR was negative for atypical mycobacteria and Herpes. Ocular Crohn’s disease, Whipple disease, and amyloidosis were ruled out. Immunofluorescence microscopy revealed characteristic IgG κ and λ light chain deposits, and fibrin deposition was confirmed through Lendrum’s Martius, Scarlet, and Blue technique. Endogenous plasminogen levels were normal. Recurrent ulcers did not resolve after treatment with infliximab, but only after four surgeries, topical steroids, 1% cyclosporine, heparin (5000 units/ml), and hyaluronidase (1.5 mg/ml). After 9 months of follow-up, nasal symblepharon was observed as sequela.
Conclusions
We report the case of a patient with unilateral ligneous conjunctivitis, triggered by chemical injury, and Crohn’s disease.
Introduction
Ligneous conjunctivitis (LC) is a rare form of chronic conjunctivitis characterized by the development of fibrin-rich, woody-like pseudomembraneous tissue in the tarsal conjunctiva (CitationSchuster and Seregard 2003). It occurs in association with external irritants and ocular surgery (CitationSchuster and Seregard 2003).
Plasminogen deficiency has recently been found to be the most common cause of LC, and the lesions are the result of an impaired wound healing response (CitationSchuster and Seregard 2003). LC seems to be the most common symptom of this systemic disorder, since it usually occurs with other mucosal involvement (CitationSchuster and Seregard 2003).
Crohn’s disease (CD) is an inflammatory bowel disease with ocular involvement as an extraintestinal manifestation. The eye disease commonly presents as anterior uveitis and, rarely, with naevus and conjunctival or lid ulcers (CitationLendrum et al 1962; CitationSchuettenberg 1991; CitationHegab and al-Mutawa 1994; CitationZoli et al 1997; CitationDiaz-Valle et al 2004). Based on clinical evolution and histopathology findings, we report a rare case of a patient with CD and LC triggered by chemical injury.
Case report
A 27-year-old female patient presented at our center with a 6-week history of right eye pain and ulceration. The symptoms appeared one month after a resolved conjunctival chemical burn with 17% hydrochloric acid. The recurrent corneal and conjunctival ulcers progressed despite topical corticosteroids, 1%, cyclosporine A (CsA), antibiotics, and artificial tears. The patient also had a 4-year history of aggressive CD, confirmed by intestinal biopsy, which required immunosuppressive therapy with azathioprine, anti-TNF-alpha treatment, and intestinal resection. Her CD had been stable for last 6 months.
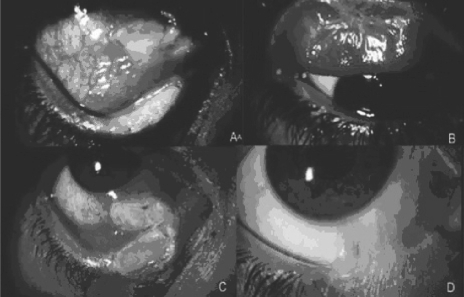
Visual acuity was 20/200 for her right eye and 20/20 for the left eye. Our initial slit-lamp examination of her right eye revealed plaque-like ulcerations in the nasal bulbar conjunctiva and in the inferior and superior tarsal conjunctivas (). The left eye was normal. Systemic workup ruled out sarcoidosis, systemic vasculitis, rickettsias, brucella, syphilis, chlamydia, Lyme disease, and HIV.
Figure 1 Initial right eye slit-lamp examination. The nasal bulbar and inferior conjunctivas (A) and the superior tarsal conjunctiva (B) had plaque-like ulcerations. The initial conjunctival ulceration was followed by a recurrence of the inferior tarsal ulcer (C). A nasal symblepharon remained as a sequela after a 9-month followup (D).
Bulbar, upper, and lower fornix conjunctival resections were performed on the affected eye. Tissue specimens from the resection were processed for special stains including Gram and acridine orange for bacteria, calcofluor and periodic acid Schiff (PAS) stains for fungi and/or Whipple disease, and Congo red for amyloidosis. The presence of atypical mycobacteria and Herpes were determined by polymerase chain reaction (BIOTOOLS B and M Labs, Madrid, Spain). All of the tests were negative.
Tissue sections for routine histopathological examination were stained with hematoxylin and eosin (H&E) and PAS stains. Fibrin deposits were assessed by Lendrum’s Martius, Scarlet, and Bluetechnique (MSB) technique (CitationLendrum et al 1962).
Immunofluorescence microscopy for IgG and κ, λ light chain deposits was performed with polyclonal antihuman antibodies from BioGenex Laboratories (San Ramon, CA, USA) and DAKO Corp. (Carpintería, CA, USA), respectively. The secondary antibody was FITC-conjugated anti-rabbit IgG (Sigma, St. Louis, MO, USA).
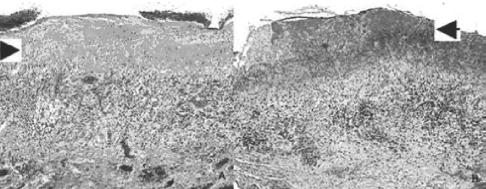
Histopathology reported surface ulcerations with an underlying thick band of hyaline-like eosinophilic material, granulation tissue, and lymphocytic infiltration (). Abundant fibrin deposition was confirmed with the MSB technique (). No granulomas were found. Histopathology and IF findings were compatible with LC. Her systemic plasminogen values were tested and “verbally reported” within normal limits (0.7–1.0 U/ml), on two separate occasions.
Figure 2 Histopathology of conjunctival biopsies. The superficial ulceration had an underlying thick band of hyaline-like eosinophilic material, probably composed of fibrin (arrow). Granulation tissue and lymphocytic infiltration were apparent in H&E (A) and fibrin (arrow) was confirmed with Lendrum staining (B). The tissue sample was negative for Congo red.
After the conjunctival resection, her symptoms and signs resolved, but then recurred two weeks later (). Her gastroenterologist indicated treatment with 3 doses of infliximab (5 mg/kg/day, Remicade, Schering-Plough, Kenilworth, NJ), but ocular signs did not improve. A second surgical excision was performed and treatment with 1% CsA three times a day (tid) initiated.
Three weeks later, a third excision was performed, since the lesion recurred, became very painful, and progressed toward the inferior palpebral skin. Otorrhinolaryngology evaluation was solicited and reported as normal.
Topical heparin (5000 units/ml) tid and fluorometholone tid was added. Due to further progression, a fourth excision was performed one month later, and topical hyaluronidase (1.5 mg/ml) tid added. Six months after treatment, the lesions resolved but an inferior nasal symblepharon developed as sequela, after a 9-month follow-up. ().
Discussion
Ocular involvement, as an extraintestinal manifestations of inflammatory bowel disease, occurs in less than 12% of cases (CitationGhanchi and Rembacken 2003). It manifests as uveitis, episcleritis, scleritis, nonspecific follicular conjunctivitis, lid marginal ulcers, during active or inactive disease (CitationSalmon et al 1991; CitationSchuettenberg 1991; CitationHegab and al-Mutawa 1994; CitationZoli et al 1997; CitationGhanchi and Rembacken 2003; CitationDiaz-Valle et al 2004). She had been asymptomatic for over one year with no treatment and remained as such throughout her ocular disease.
Previously reported cases of lid margin and conjunctival ulcers in CD have resolved after systemic and topical corticosteroid treatment (CitationHegab and al-Mutawa 1994; CitationDiaz-Valle et al 2004). We initially believed these conjunctival ulcers were due to her CD, which is why infliximab therapy was administered, after consulting with her gastroenterologist, however she did not respond. In addition, histopathology findings were more compatible with LC, since no granulomas were reported, which could have been triggered by previous chemical injury (CitationSchuster and Seregard 2003).
LC is a rare disease, with a prevalence of 1.6 per million in Europe, and due to the inheritance of an autosomal recessive gene (CitationSchuster and Seregard 2003). It involves a great variety of systemic manifestations including periodontitis, renal calculi, vulvovaginitis, respiratory disease, otitis media, dermatologic lesions, and hydrocephalus, among others (CitationSchuster and Seregard 2003). Our patient did not report any of these systemic manifestations other than an ocular chemical burn one month before the lesions appeared.
LC patients may have decreased levels of plasminogen, which arrests wound healing at the granulation tissue formation stage, and subsequently forms a fibrin-rich pseudomembranous tissue (CitationSchuster and Seregard 2003). However, normal serum plasminogen levels do not exclude LC because it is not a diagnostic criterion, but a predisposing factor, as would be in this case.
Other triggers for the development of LC include exposure to chemical irritants and conjunctival surgery (CitationSchuster and Seregard 2003). In this patient, exposure to chemical irritants could have triggered the LC, which recurred after multiple surgical interventions.
This patient’s conjunctival ulcers healed after topical CsA, heparin, and hyaluronidase therapy, which have been reported as effective treatments for LC (CitationSchuster and Seregard 2003).
The fact that conjunctival cicatrizing sequela is not characteristic of LC also challenged our initial diagnosis, although corneal scarring has been reported as a LC sequela, however the previous chemical burn strongly supported this diagnosis (CitationHidayat and Riddle 1987).
Histopathologically, LC is characterized by subepithelial, eosinophilic, amorphous material admixed with acute and chronic inflammatory cells, positive PAS staining, and negative Congo red staining (CitationHidayat and Riddle 1987; CitationHolland et al 1989; CitationKlebe et al 1999). In this case histopathology findings, abundant fibrin deposition, chronic inflammation with granulation tissue and lymphocytes, absence of granulomas, and negative Congo red staining, coincided with LC (CitationHidayat and Riddle 1987; CitationHolland et al 1989; CitationKlebe et al 1999; CitationSchuster and Seregard 2003).
Given the history of her immunobiological disease, triggering chemical burn, clinical progression despite infliximab therapy, characteristic histopathology, multiple recurrences, and resolution after combined surgical and topical treatments, LC was our final diagnosis. The LC in this CD patient was refractory to conventional treatments, however the coexistence between both diseases can be considered as casual.
We present a rare case of LC, triggered by conjunctival chemical injury, casually coexisting in a patient with CD.
Acknowledgments
Dr. S Seregard of St. Erik’s Eye Hospital, Stockholm Sweden, for performing the MSB technique for fibrin deposition confirmation. Graciana Fuentes-Páez was supported by a grant from Carolina Foundation, Ministry of Foreign Affairs, Spain. The authors have no conflict or commercial interest.
References
- Diaz-ValleDBenitez del CastilloJMFernández AceneroMJ2004Bilateral lid marginal ulcers as the inicial manifestation of Crohn’s diseaseAm J Ophthalmol138292415289143
- GhanchiFDRembackenBJ2003Inflammatory bowel disease and the eyeSurv Ophthalmol486637614609712
- HegabSMal-MutawaSA1994Conjunctival ulcer in a patient with Crohn’s diseaseOphthalmic Surg96389
- HidayatAARiddlePJ1987Ligneous conjunctivitis. A clinicopathologic study of 17 casesOphthalmology94949593658371
- HollandEJChanCCKuwabaraT1989Immunohistologic findings and results of treatment with cyclosporine in ligneous conjunctivitisAm J Ophthalmol10716062643880
- KlebeSWalkowTHartmannC1999Immunohistological findings in a patient with unusual late onset manifestation of ligneous conjunctivitisBr J Ophthalmol838789
- LendrumACSliddersWFraserDS1962Studies on the character and staining of fibrinJ Clin Pathol154011313929601
- SalmonJFWrightJPMurrayAD1991Ocular inflammation in Crohn’s diseaseOphthalmology9848042052301
- SchuettenbergSP1991Nodular scleritis, episcleritis, and anterior uveitis as ocular complications of Crohn’s diseaseJ Am Optom Assoc62377811813533
- SchusterVSeregardS2003Ligneous conjunctivitisSurv Ophthalmol483698812850227
- ZoliGCareMParazzaM1997Ocular naevus and hyperaemia with dilation of the conjunctival vessels: an early manifestation of Crohn’s disease?Ital J Gastroenterol Hepatol2927029646221