Abstract
Purpose:
This study compares the effect of topical diclofenac with that of betamethasone against postoperative increase of intraocular pressure (IOP) after cataract surgery in normal patients, and also investigated the risk factors for postoperative increase of IOP in each group.
Methods:
Fifty consecutive patients without systemic disease who have bilateral and symmetrical cataracts underwent uncomplicated cataract surgery in both eyes (100 eyes in total). Postoperatively, topical diclofenac was applied 4 times daily to one eye, and topical betamethasone to the other eye in each patient. IOP and best corrected logMAR visual acuity (BCVA) in each eye were measured up to 8 weeks. Total surgery time and effective phacoemulsification time (EPT) for each case was recorded.
Results:
BCVA in both diclofenac- and betamethasone-treated eyes significantly improved after the cataract surgery; however, no statistical difference in VA was noted between the diclofenac- and betamethasone-treated eyes throughout the observation period. IOP in the diclofenac-treated eyes decreased with time, in contrast to the IOP in the betamethasone-treated eyes, which showed a slight increase. At 4 and 8 weeks postoperatively, there was significant difference between these two eye groups. Multiple regression analysis revealed that postoperative increase in IOP at 8 weeks in the betamethasone-treated eyes was closely correlated with total surgery time and EPT, but the IOP in the diclofenac-treated eyes showed no correlation with any surgical or clinical parameters.
Conclusions:
Postoperative increase in IOP after cataract surgery was affected by total surgery time and EPT in the betamethasone-treated eye. The time for surgery and EPT is longer in complicated cases including patients with a hard nucleus or small pupils, and also longer for beginning surgeons and in older patients. In these cases, diclofenac in place of betamethasone as a postoperative topical antiinflammatory drug is recommended for the prevention of postoperative increase in IOP.
Modern cataract surgery uses a small incision and a shorter operation time; therefore, postoperative inflammation is rarely seen. Nevertheless, cataract surgery for severe cases, including cataract grade greater than Emery classification level IV, sometimes takes longer time for emulsification, and causes post-operative inflammation and a subsequent increase in intraocular pressure (IOP), which causes possible neuronal damage. Thus, to reduce the risk of inflammation after cataract surgery, a topical antiinflammatory drug application is widely used.Citation1,Citation2 Two classes of compounds are available: corticosteroids and nonsteroidal antiinflammatory drugs (NSAIDs). Although both drugs are effective in suppressing postoperative inflammation, corticosteroids have been reported to increase IOP.Citation3,Citation4 Diclofenac is a NSAID which inhibits prostaglandin synthesis,Citation5 and previous studies have assessed the effectiveness of diclofenac in treating ocular inflammation.Citation6–Citation8 Although it has been reported that diclofenac does not cause postoperative increase of IOP,Citation9 case-control studies have not been perfomed. A case-control study should be conducted in patients with eligible eyes, where one eye was treated with betamethasone and the other eye with diclofenac. These cases should be conducted in patients without systemic conditions.
In this paper, a prospective case-control compared and evaluated eyes treated with topical corticosteroids and those treated with topical NSAIDs for postoperative increase in IOP after cataract surgery. Also, the relationship between postoperative IOP and clinical factors, including age, gender, preoperative IOP, total surgery time, sonication time, and sonication power was investigated using multiple regression analysis. The final goal of this study was to determine which cases are at risk for postoperative increase in IOP and should be treated with topical administration of NSAIDs.
Methods
Patient eligibility
In this prospective study, patients had uncomplicated senile cataracts in both eyes from grade III to IV based on Emery’s classification.Citation10 Exclusion criteria were ocular hypertension (IOP > 21 mmHg), glaucoma requiring ocular medication, pseudoexfoliation, uveitis, an endothelial cell count less than 1500 cells/mm2, corneal opacity, high myopia, previous ocular surgery, systemic disease affecting the inflammatory response such as diabetes mellitus, collagen disease requiring long-term systemic steroids or antiinflammatory drugs, and severe hypertension. Patients whose cataract grades were not symmetrical in both eyes were also excluded in this study. Intraoperative exclusion criteria were iatrogenic iris damage, retained cortical matter, and a serious complication such as posterior capsule rupture. 50 consecutive patients (21 male; 29 female) participated in this study.
All patients received a comprehensive ocular examination before treatment and were followed for periodic examinations after the treatments. After informing the patient of the purpose of this study and the possible outcomes, informed consent was obtained from all patients prior to the intervention. This study was also approved by the Ethics Committee for Clinical Research at NTT East Japan Tohoku Hospital using procedures which conformed to the tenets of the Declaration of Helsinki.
Study design
All patients had cataract surgery performed in both eyes within a 1 week interval. Before cataract surgery, a topical antimicrobial drug, gatifloxacin hydrate 0.3% ophthalmic solution (Gatiflo®; Senju Pharmaceutical Co. Ltd., Osaka, Japan), was administered 4 times/day in both eyes of each patient. The surgical technique used in this study consisted of a continuous curvilinear capsulorrhexis (CCC), phacoemulsification, and implantation of a foldable acrylic IOL (Acryfold® YA-65BB; HOYA medicals, Tokyo, Japan) into the lens capsule through a 3.0 mm corneoscleral incision. Phacoemulsification was done with an Alcon Legacy 20000™ unit with standard cassettes and tubing. The incision was not sutured. In each patient, cataract surgery in the eye with the worst visual acuity was done first, then surgery in the other eye was completed within a week. If the visual acuity in both eyes was the same, then the right eye was chosen first. The effect of 0.1% diclofenac (Diclod®; Wakamoto Pharmaceutical Co. Ltd., Tokyo, Japan), which is a phenylacetic acid derivative, on IOP after cataract surgery was compared to that of 0.1% betamethasone sodium phosphate (Rindelon®, Shionogi Co. Ltd., Osaka, Japan), which is a topical corticosteroid.
After the next-day examination (defined as day 1), topical administration of an antiinflammatory drug was started; 0.1% diclofenac and 0.3% gatifloxacin were topically applied 4 times/day to the left eye, and 0.1% betamethasone and 0.3% gatifloxacin were topically applied 4 times/day to the right eye. Drug applications were continued for at least 8 weeks after the surgery.
Total surgery time (minutes) was recorded in each case. The sonication time (seconds) and mean phaco power (percentage) were also noted from the phaco unit’s display. The sonication time was defined as the time the foot pedal remained in position 3. The mean phaco power was defined as the power used during sonication time. The effective phaco time (EPT) was calculated using the following formula: EPT = sonication time X mean phaco power/100.
IOP and best corrected logMAR visual acuity (BCVA) in each eye were measured preoperatively and postoperatively at 3 and 7 days, and at 4 and 8 weeks after cataract surgery. The IOP data were obtained using pneumotonometry.
Statistical analysis
The data are presented as mean ± standard deviation. Statistical differences between follow-up points of the clinical course in the same eyes were assessed using the Wilcoxon signed-rank test, and the differences between the right and left eyes were assessed using the Mann Whitney U test (SPSS ver. 11; SPSS Inc., Chicago, IL, USA).
To clarify the change in IOP, delta IOP (ΔIOP), defined as a subtraction in IOP at 8 weeks postoperatively from IOP at the preoperative exam, was calculated in each eye. To investigate the correlation between ΔIOP and clinical parameters, Pearson’s correlation coefficient (r), and a p value were calculated. Since the number of samples was 50, a |r| value of more than 0.3 was considered a statistically significant correlation. In all cases, p < 0.05 was considered to be significant.
To clarify which parameters contribute to ΔIOP, multiple regression analysis was performed. From multiple regression analysis, a standard partial regression coefficient (b) and a p value in each clinical factor were calculated. Each amount of |b| value reflects a degree of contribution for each factor to the prognosis. To confirm the “goodness-of-fit” in each multiple regression equation, analysis of variance (ANOVA) was performed and a p value of less than 0.05 was considered a good fit.
Results
The ages of the patients ranged from 60 to 83 years with a mean of 74.8 ± 5.4 years. Twenty seven of 50 patients underwent cataract surgery in the right eye first, and then 1 week later in the other eye, while the remaining 23 patients underwent cataract surgery first in the left eye and then in the right eye. The surgery was performed by a single surgeon (MS) and took less than 15 minutes, and no complications occurred.
Alteration of BCVA before and after the cataract surgery
Before cataract surgery, BCVA in the betamethasone-treated (right) eye was logMAR 0.348 ± 0.222, and BCVA in the diclofenac-treated (left) eye was logMAR 0.363 ± 0.233, thus showing no statistically significant difference in BCVA (p = 0.785). After the surgery, BCVA in all eyes improved, and at the final period of 8 weeks after surgery, BCVA in the right eye was logMAR −0.026 ± 0.056, and in the left eye logMAR −0.028 ± 0.057, so that no statistically significant difference existed between the two groups of eyes 1.992).
Change in IOP after topical administration of antiinflammatory drugs
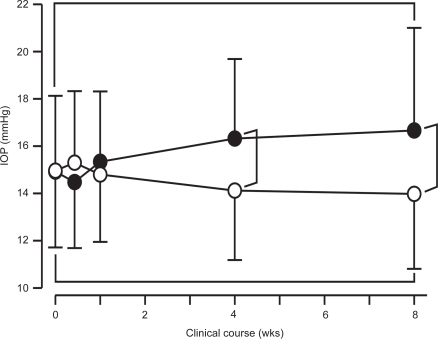
Before cataract surgery, IOP in the betamethasone-treated (right) eye was 14.9 ± 3.2 mmHg, and IOP in the diclofenac-treated (left) eye was 15.0 ± 3.2 mmHg, thus showing no statistically significant difference between these two groups (p = 0.986). As shown in Figure , IOP in the betamethasone-treated eyes gradually increased to 16.7 ± 4.3 mmHg (p = 0.001). In contrast, IOP in the diclofenac-treated eyes gradually decreased to 14.0 ± 3.2 mmHg (p = 0.01). There was a statistically significant difference in IOP between each of these groups at 4 (p < 0.001) and 8 weeks (p < 0.001).
Figure 1 Clinical course in IOP after the cataract surgery in eyes with postoperative topical administration of betamethasone (closed circle) and that of diclofenac (open circle). The vertical bar indicates standard deviation of the mean. After 4 postoperative weeks, IOP in the betamethasone-treated eye showed a significant increase with compared to that in diclofenac-treated eye. The asterisk (*) indicates statistical significance (p < 0.05).
Relationship between ΔIOP and total surgery time
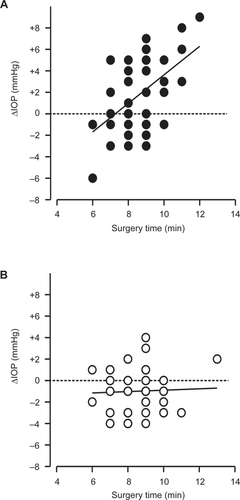
The total surgery time was 8.58 ± 1.28 min in the betamethasone-treated (right) eyes, and 8.74 ± 1.29 min in the diclofenac-treated (left) eyes, which shows no statistically significant difference between either group of eyes (p = 0.472). To investigate the correlation between ΔIOP and total surgery time, Pearson’s correlation coefficient was calculated from each plot (Figure ). ΔIOP in the betamethasone-treated eyes was closely correlated with the total surgery time (Figure ; r = 0.499, p = 0.002); in contrast, ΔIOP in the diclofenac-treated eyes showed no correlation with the total surgery time (Figure ; r = 0.044, p = 0.763).
Figure 2 Relationship between the ΔIOP and total surgery time in uneventful cataract surgery in postoperative betamethasone-treated eyes (A) and diclofenac-treated eyes (B) Strong correlation was observed in betamethasone-treated eye (r = 0.499, p = 0.002), in contrast little correlation was seen in diclofenac-treated eyes (r = 0.044, p = 0.763).
Relationship between ΔIOP and EPT
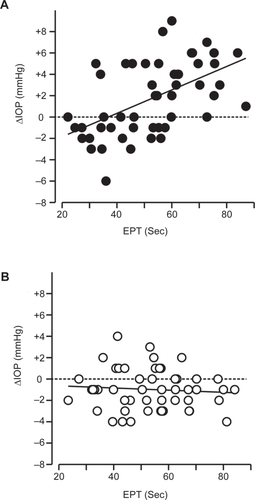
The EPT was 52.7 ± 16.6 sec in the betamethasone-treated (right) eyes, and 53.5 ± 14.9 sec in the diclofenac-treated (left) eyes, which shows no statistically significant difference between both groups of eyes (p = 0.206). To investigate the correlation between ΔIOP and the EPT, Pearson’s correlation coefficient was calculated from each plot (Figure ). ΔIOP in the betamethasone-treated eyes was closely correlated with the EPT (r = 0.535, p < 0.001); in contrast, the ΔIOP in the diclofenac-treated eyes showed no correlation with the EPT (r = −0.080, p = 0.584).
Figure 3 Relationship between the ΔIOP and EPT in uneventful cataract surgery in postoperative betamethasone-treated eyes (A) and diclofenac-treated eyes (B) Strong correlation was observed in betamethasone-treated eye (r = 0.535, p < 0.001), in contrast little correlation was seen in diclofenac-treated eyes (r = −0.080, p = 0.584).
Contribution of clinical factors to ΔIOP after cataract surgery
To investigate which clinical factors contributed to the ΔIOP, multiple regression analysis was performed. The clinical factors were age, gender, preoperative IOP, preoperative BCVA, total surgery time, and EPT. In the betamethasone-treated (right) eyes, ΔIOP was +1.74 ± 3.41 mmHg, and the standard partial regression |b| of total surgery time (p = 0.019) and EPT (p = 0.002) was significantly higher than the other factors, indicating that surgery time and EPT contribute to an increase in IOP. The exact probability of this multiple regression equation was confirmed by analysis of variance (ANOVA; p = 0.0001) (Table ). In contrast, in the diclofenac-treated eyes, ΔIOP was −0.98 ± 1.89 mmHg, and there was no statistically significant amount of |b|; therefore, a decrease in IOP was not caused by any clinical factors (Table ).
Table 1 Multiple regression analysis for alteration of ΔIOP in betamethasone-treated eyes
ANOVA table from multiple regression equation of y = improvement of VA
Table 2 Multiple regression analysis for alteration of ΔIOP in diclofenac-treated eyes
ANOVA table from multiple regression equation of y = improvement of VA
Discussion
This prospective case-control study is unique because each patient had one eye treated with betamethasone and the other eye treated with diclofenac after cataract surgery. In these cases, where patients had both eyes treated, systemic conditions can be excluded.
After uneventful cataract surgery in a normal patient, the major findings of this study are as follows. 1) postoperative IOP was slightly increased in eyes treated with betamethasone, which was dependent upon total surgery time and EPT. 2) In contrast, postoperative IOP in eyes treated with diclofenac was slightly decreased, and was not affected by surgery time or EPT.
According to a recent study, IOP in the nonglaucomatous eye is reduced following uneventful cataract surgery.Citation11 In our study, IOP in the diclofenac-treated eyes also showed a significant reduction after cataract surgery. In contrast, IOP in the betamethasone-treated eyes showed significant increase. Interestingly, within 1 week after the surgery, there was no significant difference in IOP between the two groups; however, at 4 and 8 weeks postoperatively, IOP in the corticosteroid (betamethasone)-treated eyes was significantly higher than that in NSAID (diclofenac)-treated eyes. It is well known that topical corticosteroid-induced IOP elevation is observed after 3 weeks of administration.Citation12 Therefore, IOP elevation after surgery in the betamethasone-treated eyes is possibly “steroid-induced ocular hypertension.”
Although the pathogenesis of steroid-induced ocular hypertension still remains unknown, corticosteroid affects cytoskeleton, an extracellular matrix in trabecular meshwork cells,Citation13 leading to an increase in the outflow resistance of aqueous humor. However, corticosteroids did not always induce ocular hypertension in all cases. Previous reports indicated 69% of normal eyes had IOP elevations of at least 5 mmHg and were classified as steroid responders.Citation14 In this study 18 of 50 eyes showed more than 5 mmHg of ΔIOP; in contrast, 23 eyes showed less than 0 mmHg of ΔIOP, therefore, those 18 patients were considered steroid responders. In these 18 patients, ΔIOP in the other (diclofenac-treated) eyes showed less than 2 mmHg (mean −0.67 ± 2.0 mmHg); therefore, diclofenac did not induce ocular hypertension even in steroid responders.
The most interesting result in this study is that an increase of ΔIOP after uneventful cataract surgery in betamethasone-treated eyes was related to surgery time and EPT. Longer surgery time and/or EPT usually caused more postoperative inflammation. Generally, it takes more time and/or sonication power to perform cataract surgery in complicated cases including those of patients with a hard nucleus and/or small pupils. Also, beginning surgeons and older patients need more time for surgery. In these cases, diclofenac seems to have some advantages compared with betamethasone for preventing postoperative increases in IOP.
Acknowledgements
The authors thank Dr Norio Sugimoto in Theranostic Instruments Research Laboratories for his technical support of statistical analyses and useful comments.
Disclosure
The authors have no competing financial interests in this work.
References
- RowenSPreoperative and postoperative medications used for cataract surgeryCurr Opin Ophthalmol199910293510387316
- NelsonMLMartidisAManaging cystoid macular edema after cataract surgeryCurr Opin Ophthalmol200314394312544809
- KerseyJPBroadwayDCCorticosteroid-induced glaucoma: a review of the literatireEye2006204071615877093
- JonesR3rdRheeDJCorticosteroid-induced ocular hypertension and glaucoma: a brief review and update of the literatureCurr Opin Ophthalmol200617163716552251
- GoaKLChrispPOcular diclofenac: A review of its pharmacology and clinical use in cataract surgery, and potential in other inflammatory ocular conditionsDrugs and Aging19922473861493352
- AraieMSawaMTakaseMTopical flurbiprofen and diclofenac suppress blood-aqueous barrier breakdown in cataract surgeryJpn J Ophthalmol198327535426656015
- FlachAJKraffMCSandersDRThe quantitative effect of 0.5% ketorolac tromethamine solution and 0.1% dexamethasone sodium phosphate solution on postsurgical blood aqueous barrierArch Ophthalmol198810648033355415
- Othenin-GirardPTrittenJJPittetNDexamethasone versus diclofenac sodium eyedrops to treat inflammation after cataract surgeryJ Cataract Refract Surg1994209128133491
- StrelowSASherwoodMBBroncatoLJThe effect of diclofenac sopdium ophthalmic solution on intraocular pressure following cataract extractionOphthalmic Surg19922317051574284
- EmeryJMMcIntyreDJPatient Selection in Extracapsular Cataract SurgerySt Louis, MOMosby-Year Book Inc198395100
- IssaSAPachecoJMahmoodUA novel index for predicting intraocular pressure reduction following cataract surgeryBr J Ophthalmol200589543615834080
- GeromettaRPodosSMCandiaOASteroid-induced ocular hypertension in normal cattleArch Ophthalmol20041221492715477461
- WordingerRJClarkAFEffects of glucocorticoids on the trabecular meshwork: towards a bettter understanding of glaucomaProg Retin Eye Res1999186296710438153
- BartlettJDWoolleyTWAdamsCMIdentification of high intraocular pressure responders to topical ophthalmic corticosteroidsJ Ocular Pharmacol199393545