Abstract
Purpose:
To determine the intravitreal levels of vascular endothelial growth factor (VEGF) in eyes with anterior hyaloidal fibrovascular proliferation (AHFVP).
Methods:
Three eyes of three patients who underwent vitrectomy for proliferative diabetic retinopathy (PDR) and subsequently developed an AHFVP (AHFVP group) were studied. We measured the level of VEGF in vitreous samples collected at the primary and following operations by enzyme-linked immunosorbent assay. The vitreous levels of VEGF in 25 eyes of 22 patients with PDR were also studied as controls (PDR group).
Results:
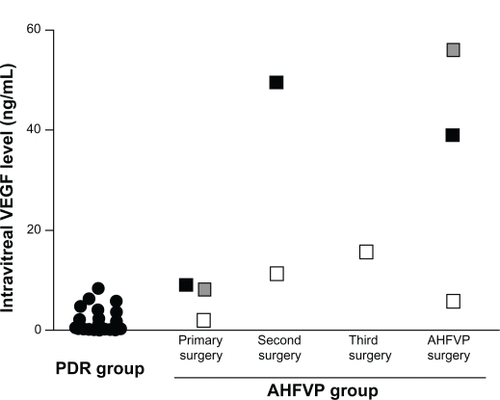
The averaged VEGF level in the samples collected at the primary surgery was 1.98 ± 2.23 ng/mL in the PDR group, and it was 9.07, 1.94, and 8.07 ng/mL in the AHFVP cases. After the primary surgery, the VEGF level rose up to 49.50, 15.60, and 50.60 ng/mL at the subsequent surgeries for respective cases of the AHFVP group. These levels of VEGF were more than five times higher than the baseline at the primary surgery.
Conclusion:
The subsequent increase of the VEGF level after the primary surgery in eyes with an AHFVP suggests that the vitreous levels of VEGF are associated with the development of the AHFVP although only three eyes were studied.
Keywords:
Introduction
An anterior hyaloidal fibrovascular proliferation (AHFVP) is a fibrous vascular proliferation in the peripheral retina that can cause vitreous hemorrhage, retinal detachment, and ocular hypotension. These changes can then result in poor vision.Citation1 An AHFVP develops postoperatively mainly in young patients with severe proliferative diabetic retinopathy (PDR) despite a complete removal of the vitreous and extensive retinal photocoagulation of the peripheral retina.
We questioned whether vascular endothelial growth factor (VEGF) plays a role in the development of AHFVPs because earlier studies found that the progression of diabetic retinopathy was associated with the vitreal levels of VEGF.Citation2 Thus, the VEGF level in the vitreous is higher in eyes with more severe diabetic retinopathy, and the level affects the visual outcome negatively after vitrectomy.Citation3 However, it has not been determined whether VEGF contributes to the development of AHFVPs.
The purpose of this study was to determine the level of VEGF in the vitreous of eyes with PDR at the primary surgery and also in eyes that developed an AHFVP after the surgery. We compared the VEGF level in vitreous samples collected at the time of the primary vitrectomy from patients who developed an AHFVP with that in patients with PDR who did not develop AHFVP.
Materials and methods
Patients
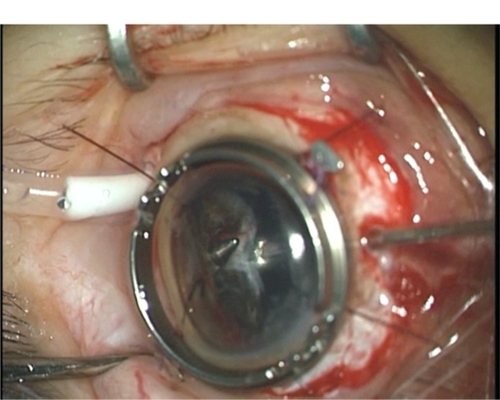
Three eyes of three patients (two men and one woman) who developed an AHFVP after vitrectomy for PDR were studied and placed in the AHFVP group. They were treated at the Vitreoretinal Disease Unit of the Iwate Medical University Hospital from July 2003 through June 2006. The three patients with an AHFVP had insulin-dependent diabetes. AHFVP was diagnosed in the eyes that had annular fibrovascular tissue at the vitreous base during the vitreous surgery (). The ages of the patients were 24, 32, and 49 years. Twenty-five eyes of 22 patients (18 men and four women) who underwent vitrectomy for PDR from February 2005 to March 2007 were studied as controls and placed in the PDR group. Their mean age was 43.2 ± 12.9 years with a range of 22–67 years. The difference in the ages between the PDR and AHFVP groups was not significant.
Figure 1 Intraoperative photograph of Case 1 with AHFVP undergoing membrane removal with vitreous cutter.
This research was conducted in accordance with the Institutional Guidelines of Iwate Medical University, and the procedures conformed to the tenets of the Declaration of Helsinki. An informed consent was obtained for the vitrectomy from all subjects after a full explanation of the nature of the experiment.
Sample collection and measurement of VEGF levels
Vitreous samples were collected at the beginning of the vitreous surgery. In cases that developed AHFVP, samples were also collected at each vitrectomy to treat the AHFVP. The intravitreal VEGF levels were measured by enzyme-linked immunosorbent assay (ELISA) using a kit for human VEGF (Quantikine; R&D Systems, Minneapolis, Minnesota, US). We incubated 200 μL of each sample in 96-well plates coated with human immunoglobulin G (IgG)-specific goat IgG for 2 hours at room temperature. After the incubation, the plate was washed, and a peroxidase-conjugated antibody was added and incubated for 2 hours at room temperature. The plate was washed again, and the substrate was added, and the optical density was measured at 450 and 620 nm using an absorption spectrophotometer. A standard curve was plotted from measurements made with the standard solutions and used to determine the concentration of VEGF in the sample.
Results
VEGF levels in control eyes with proliferative diabetic retinopathy
The averaged level of VEGF in the PDR group that did not develop AHFVP was 1.98 ± 2.23 ng/mL (mean ± standard deviation) ().
Clinical features of AHFVP cases
The VEGF levels in the vitreous humor are plotted for the three patients who developed an AHFVP after the primary vitrectomy ().
In Case 1 (black squares), the VEGF level was 9.07 ng/mL at the primary vitrectomy, which also included cataract surgery. The VEGF level was markedly increased to 49.50 ng/mL in a vitreous sample collected during trabeculectomy for neovascular glaucoma 7 weeks postoperatively even though the peripheral retina had been ablated by retinal photocoagulation at the primary operation. Vitreous hemorrhage developed 8 months after the primary surgery, and a third vitrectomy was performed. AHFVP was detected at the time of this surgery (). The VEGF level at this vitrectomy was still high at 39.00 ng/mL.
In Case 2 (white square in ), the VEGF level at the primary vitrectomy was 1.94 ng/mL, which was comparable to that in the PDR group (). Three weeks later, a second vitrectomy was performed to remove a persistent vitreous hemorrhage, and the VEGF level in the vitreal sample had increased to 11.20 ng/mL despite an ablation of the peripheral retina by photocoagulation at the primary operation. Seven weeks later, we performed membrane peeling and additional photocoagulation because of a reproliferation, and the VEGF level at this time was 15.60 ng/mL. Seven months after the first operation, vitreous hemorrhage recurred, and a 4th operation was performed. During the surgery an AHFVP was identified, and the vitreous sample collected showed that the VEGF level was decreased but still high at 5.70 ng/mL.
In Case 3 (gray square in ), the VEGF level was 8.07 ng/mL at the primary vitrectomy with cataract surgery and trabeculectomy. Six months later, the operated eye developed hyphema. During the 2nd operation, an AHFVP was identified, and the vitreal sample showed that the VEGF level was markedly increased to 50.60 ng/mL.
The VEGF level of the AHFVP group overlapped that of the PDR group at the primary surgery. However, the VEGF concentration in the AHFVP group was increased after the primary surgery beyond the upper limit in the PDR group (). The VEGF level at subsequent surgeries was more than five times higher than the baseline at the primary surgery in all AHFVP cases.
Discussion
Our results demonstrated that the VEGF level in the vitreous sample considerably increased after the primary surgery in eyes that developed AHFVP. This suggests a pathological association between the intravitreal VEGF level and the development of AHFVP.
It has been reported that VEGF is upregulated by inflammatory cytokines such as IL-1 and TNF-α.Citation4,Citation5 Our AHFVP cases underwent intensive retinal photocoagulation with long operation times that could possibly have upregulated these inflammatory cytokines, which would then upregulate the expression of VEGF. If they are upregulated, then studies should be performed to see if suppressing these inflammatory cytokines by triamcinolone acetonide can prevent the development of AHFVP.
Anti-VEGF therapy, eg, by bevacizmab, has been shown to be an effective therapy for the neovascularization in eyes with PDR.Citation6 Based on our results that VEGF may play a role in the development of AHFVP, anti-VEGF treatment may be effective as an adjunctive treatment in preventing the development of AHFVP. Because anti-VEGF therapy was not available during the study period, we could not test this hypothesis. Future studies are necessary to determine the efficacy of anti-VEGF therapy for AHFVP.
There are some limitations of this study. First, AHFVP is a rare complication so that we were able to study only three patients. Second, the level of VEGF level was quite variable among cases in the AHFVP group. However, the VEGF level in the eyes with AHFVP was higher than the highest level in the PDR group after the primary surgery and at the subsequent vitrectomies. The VEGF level was increased to more than five times higher than the baseline level at the primary surgery in all AHFVP cases. The increase of the VEGF level is much higher than that reported in diabetic patients who underwent vitrectomy.Citation7 These findings support our conclusion that the intravitreal level of VEGF is associated with the development of an AHFVP.
In case 2, the VEGF level was higher than the normal range; however, the VEGF level at onset of AHFVP was lower than the other cases. From this, we suggest that the development of AHFVP may be caused by not only VEGF but also other factors. Although VEGF plays a major role in progression of diabetic retinopathy, the level at the onset of AHFVP may be different in each case, and could be affected by sensitivities of the receptors, inhibitors,Citation8 and other factors associated with the upregulation of VEGF.Citation9 We examined only the VEGF level as main factor of diabetic retinopathy. However, other factors may also maintain the neovascularization, and further studies will be necessary to determine whether other factors are involved in the development of AHFVP. Our results suggest that not only anti-VEGF therapy but also anti-cytokine therapy should be considered in future studies.
Our results strongly suggest that intravitreal VEGF plays an important role in development of AHFVP. Therefore, it would be useful to measure the VEGF level in the vitreous during the vitreous surgery for diabetic retinopathy to be able to predict the possibility of a development of AHFVP.
Acknowledgments/disclosure
Funding/support: none; financial disclosure: none.
References
- LewisHAbramsGWWiliamsGAAnterior hyaloidal fibrovascular proliferation after diabetic retinoathyAm J Ophthalmol19871046076152446501
- AielloLPAveryRLArriggPGVascular endothelial growth factor in ocular fluid of patients with diabetic retinopathy and other retinal disordersN Engl J Med1994331148014877526212
- FunatsuHYamashitaHNomaHRisk evaluation of outcome of vitreous surgery for proliferative diabetic retinopathy based on vitreous level of vascular endothelial growth factor and angiotensin IIBr J Ophthalmol2004881064106815258026
- KvantaAExpression and regulation of vascular endothelial growth factor in choroidal fibroblastsCurr Eye Res199514101510208585929
- YoshidaSOnoMShonoTInvolvement of interleukin-8, vascular endothelial growth factor, and basic fibroblast growth factor in tumor necrosis factor alpha-dependent angiogenesisMol Cell Biol199717401540239199336
- JorgeRCostaRACalucciDIntravitreal bevacizumab (Avastin) for persistent new vessels in diabetic retinopathy (IBEPE study)Retina2006261006101317151487
- ItakuraHKishiSKotajimaNPersistent secretion of vascular endothelial growth factor into the vitreous cavity in proliferative diabetic retinopathyOphthalmology20041111880188415465550
- OgataNNishikawaMNishimuraTUnbalanced vitreous levels of pigment epithelium-derived factor and vascular endothelial growth factor in diabetic retinopathyAm J Ophthalmol200213434835312208245
- FunatsuHYamashitaHNakanishiYAngiotensin II and vascular endothelial growth factor in the vitreous fluid of patients with proliferative diabetic retinopathyBr J Ophthalmol20028631131511864890