Abstract
Purpose
To report a case of acute visual loss after endoscopic spinal surgery.
Methods
A patient was immediately referred to our department after epidural endoscopy with severe bilateral visual impairment and underwent complete ophthalmologic examination.
Results
Visual acuity was decreased in both eyes. Fundus examination revealed the presence of retinal and vitreous hemorrhages bilaterally. Four months later, visual acuity increased and the hemorrhages were remarkably resolved.
Conclusion
The present case represents an extremely rare incidence of intraocular hemorrhage following epiduroscopy.
Keywords:
Case report
A 45-year old man suffered from low back pain unresponsive to pharmacologic treatment, radiating to the left hip and left lower extremity, due to a back injury 4 years ago. Other medical history was noncontributory and he was otherwise healthy without hypertension, diabetes mellitus, cardiovascular disease, or blood clotting abnormalities.
The patient underwent an epidural endoscopy and endoscopic adhesiolysis in the level of L4–L5 and O5S1 by infusion of 120 cc of normal saline. At the end of the procedure the patient received an epidural injection of 80 mg methylprednisolone.
After the operation the general condition of the patient was good without clinical signs of elevated cerebrospinal pressure and blood pressure and heart rate remained stable. However, a few hours later, he became aware of a major decrease of vision in both eyes and was immediately admitted to the department of ophthalmology.
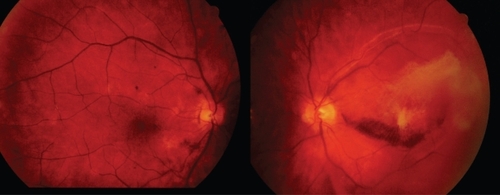
At presentation, best corrected visual acuity (BCVA) was 20/400 RE and counting fingers LE. The ophthalmic examination revealed the presence of extensive scattered preretinal, subhyaloid, and subretinal hemorrhages in both eyes and especially in the LE (). Ocular history before the operation did not reveal any ocular disease and BCVA was 20/20 in both eyes.
Figure 1 Fundus photograph of OD (left) and LE (right) showing subhyaloid, preretinal and retinal hemorrhages 1 week after the spinal surgery.
Three weeks after surgery, BCVA was 20/100 RE and counting fingers LE. Intra-ocular pressure and anterior segments showed no abnormalities in both eyes. Examination of the fundus showed mild vitreous hemorrhage with extensive intraretinal and subretinal hemorrhages involving the macula especially of the LE.
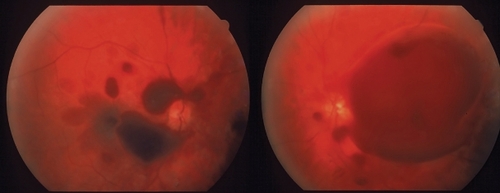
Four months after the operation, BCVA was 20/30 in both eyes. Despite the improved vision the patient still noted a central scotoma in both eyes. Fundus examination revealed a remarkable resolution of the retinal and subretinal hemorrhages bilaterally with mild pigmentary changes of the macula especially of the LE ().
Discussion
Intraocular hemorrhages often occur in association with acute subarachnoid hemorrhage and secondary aneurysms of the anterior communicating and internal carotid arteries (CitationTerson 1900). The present case represents an extremely rare incidence of intraocular hemorrhage following epiduroscopy and endoscopic adhesiolysis (CitationAmirikia et al 2000; CitationBrian et al 2005). Several mechanisms have been proposed to explain the occurrence of intraocular hemorrhage (CitationPurdy et al 1998). It seems that a sudden increase of the epidural pressure after the epiduroscopy causes cerebrospinal fluid to effuse through the communication of the subarachnoid space within the optic nerve sheath and subsequently compresses the optic nerve and its vasculature. Specifically, the retinochoroidal anastomosis and the central retinal vein are occluded resulting in venous stasis allowing extravasation of blood through the vessels causing subhyaloid, retinal, and subretinal hemorrhages. The different types of hemorrhages suggest an acute generalized extravasation of blood within the various layers of the posterior segment opposed to the direct tracking of blood from within the optic nerve sheath. More particularly, intracranial pressure can be directly affected if the dura is punctured and fluid is added to the subarachnoid space. The visual prognosis is considered to be good, with recovery occurring within 6 months (CitationTabandeh 2000). Surgery may be required for persistent vitreous hemorrhage and secondary complications.
In conclusion the present case is rare and it represents a rare complication of a rather common operation. However, as endoscopic spinal procedures become widely established, it is anticipated that similar cases will be recognized more frequently in the future. Therefore, surgeons should be aware of the possibility of possible vision loss after this procedure.
Disclosure
The authors report no conflicts of interest.
References
- AmirikiaAScottIUMurrayTG2000Acute bilateral visual loss associated with retinal hemorrhages following epiduroscopyArch Ophthalmol118287910676802
- BrianJGHeavnerEJ2005Visual impairment following epidural fluid injections and epiduroscopy: A reviewPain Med63677416266357
- PurdyEPGurjitAS1998Visual loss after lumbar epidural steroid injectionAnesth Analg86119229428864
- TabandehH2000Intraocular hemorrhages associated with endoscopic spinal surgeryAm J Ophthalmol1296889010844075
- TersonA1900De l’ hémorragie dans cérébrale hémorragie dans le corps vitré au cours de l’ hémorragie cérébraleClin Ophtalmol630912