Abstract
Objective:
The evaluation of central corneal thickness (CCT) in subjects with pesudoexfoliation glaucoma (PEXG), primary open-angle glaucoma (POAG), and in normotensive individuals with or without pseudoexfoliation syndrome (PXS).
Study design/patients and methods:
CCT was evaluated with ultrasound pachymetry in a total of 179 individuals: 32 had bilateral PEXG, 55 had bilateral POAG, 35 had PXS, and 57 were healthy individuals without PXS.
Results:
CCT in PEXG eyes (526.00 ± 34.30 μm) was significantly thinner compared to POAG eyes (549.36 ± 39.3 μm) (P = 0.027) and normal control eyes with (550.64 ± 39.0 μm) or without PXS (547.36 ± 33.1 μm), (P = 0.039 and 0.048 respectively). No statistically significant difference was found comparing CCT values of POAG eyes to control group eyes.
Conclusion:
The evaluation of CCT is necessary in all patients with glaucoma and especially in those with PEXG due to the thinner cornea and the risk of underestimation of intraocular pressure.
Keywords:
Introduction
In routine clinical practice, intraocular pressure (IOP) is one of the most important parameters in the detection and monitoring of glaucoma. Goldmann applanation tonometry (GAT) has become the international “gold standard” for IOP measurements. The effect of central corneal thickness (CCT) on IOP readings using GAT has become a topic of much interest.Citation1–Citation7 A thick cornea would overestimate IOP and a thin one would underestimate it. Moreover the Ocular Hypertension Treatment Study (OHTS) designated CCT as a strong predictor for the development of primary open-angle glaucoma (POAG) in patients with ocular hypertension (OHT).Citation8 Although the relationship between CCT and stage of glaucoma damage seems to be related to IOP measuring error, recent studies recognize CCT as an intrinsic ocular factor in the pathogenesis and progression of glaucoma.Citation9–Citation11
Being aware of these evidence, CCT assessment has been extensively studied in patients with POAG and has been shown to be thinnerCitation12–Citation14 or similar4,Citation15–Citation19 to control individuals.
Pseudoexfoliation glaucoma (PEXG) is generally accepted as being more unpredictable and resistant to the treatment (surgical or medical) compared to POAG. Furthermore, the conversion of hypertensives with pseudoexfoliation syndrome (PXS) to glaucoma has been found to be more common than conversion of ocular hypertensives without PXS.20 In that way, evaluation of CCT in subjects with PXS or PEXG could be essential for early diagnosis and suitable management of the glaucoma. However, there are very few studies conducted in a small number of patients in the literature measuring the CCT in this type of glaucoma and their results are controversial.Citation4,Citation6,Citation12,Citation13,Citation15,Citation16,Citation21,Citation22
The aim of this study is the evaluation of central CCT in patients with PEXG, POAG, and in normotensive individuals with or without PXS.
Patients and methods
A total of 179 subjects (179 eyes), all Caucasians, were included in this cross-sectional study by a single observer. All subjects where examined in University Eye Clinic of Ioannina, within the context of routine examinations at the Glaucoma department between September 2007 and March 2008. Thirty-two subjects (32 eyes) had bilateral PEXG and 55 subjects (55 eyes) had bilateral POAG. The type of glaucoma had been diagnosed in previous appointments. Ninety two individuals (92 eyes) without glaucoma or OHT were also included in the study, comprising the control group. Thirty-five subjects (35 eyes) had bilateral PXS and 57 individuals (57 eyes) were normal without PXS.
All eyes underwent a full ophthalmologic examination, including applanation tonometry, gonioscopy, fundoscopy, and repeated Humphrey 24–2 static threshold perimetry (at least three examinations).
Data such as age, gender, ocular and medical history, number, type, and duration of antiglaucomatous medical therapy were also recorded.
Inclusion criteria for subjects with POAG were: untreated IOP more than 22 mmHg on at least two diurnal curves, open-normal angle, glaucomatous optic disc and at least three Humphrey visual field tests with glaucomatous defects. Inclusion criteria for subjects with PEXG were: untreated IOP more than 22 mmHg, open angle, glaucomatous optic disc, at least three Humphrey visual field tests with glaucomatous defects and presence of typical pseudoexfoliative material at the anterior lens capsule and/or at the pupillary margin. On the day of examination, IOP measured by GAT was less than 21 mmHg in all individuals with glaucoma.
Control group included subjects with IOP less than 21 mmHg, at three different successive measurements, open angle, normal optic disc, and Humphrey visual field tests and no family history of glaucoma. The control group was also evaluated for the presence of pseudoexfoliation syndrome (presence of typical pseudoexfoliative material at the anterior lens capsule and/or at the pupillary margin).
Subjects with ocular disease other than glaucoma, contact lens users and patients that had undergone ocular surgery or laser photocoagulation treatment were excluded. Also, subjects with myopia or hypermetropia greater then 3D or astigmatism more than 1D that could potentially effect our measurements were not included.
In all understudy groups, IOP was measured using calibrated GAT. Two measurements were made. If the two readings were within 2 mmHg, the mean of the two measurements was used. If the two readings were separated by more than 2 mmHg, a third measurement was made and the median became the recorded IOP.
The estimation of optic disc cupping (vertical C/D ratio) and retinal nerve fiber layer (RNFL)-average thickness (Avg. Thick.) was made with optical coherence tomography (Zeiss Stratus; Carl Zeiss, Inc., Valhalla, NY, USA).
Ultrasound pachymetry (Pacline; OPTIKON 2000 S.p.A, Rome, Italy) was used to obtain morning measurements, at least two hours after awakening, of central corneal thickness by a single observer. Repeated sets of five readings at the center of the cornea were taken, after a drop of anesthetic, until the standard deviation for the five readings were 5 μm or less. Pachymetry always precedes applanation tonometry. One eye was randomly selected from each patient and analyzed in the study.
The measurements in each glaucoma type subgroup were compared against the age and sex matched control group.
Statistical analysis was performed with SPSS (v.15 for Windows XP; SPSS Inc., Chicago, IL, USA). One-way analysis of variance, Student’s t-test and Chi squared (χ2) test were used. One-way analysis of variance (ANOVA) using the Tukey post-hoc test was used to identify which groups (PXEG, POAG, control with or without PXS) differed from each other. We considered values of P < 0.05 to be statistically significant.
Results
Eighty-seven subjects with glaucoma (32 with PEXG, 55 with POAG) and 92 control subjects (35 with PXS, 57 without PXS) met the inclusion criteria of the study. The demographic characteristics of each group are summarized in . All groups are similar in age and gender. Mean IOP measurements of subjects with glaucoma (POAG, PEXG) and of control group were below 21 mmHg, thus avoiding false measurements due to corneal edema (). PEXG individuals had statistically significant more severe glaucomatous optic nerve damage, as this is revealed by C/D ratio and RNFL thickness, compared to subjects with POAG (; Student’s t-test, P = 0.03 and 0.01, respectively).
Table 1 Characteristics for each of the investigated groups
As far as the glaucoma subgroups are concerned, the study showed that they did not vary in type of topical antiglaucoma medication treatment. Topical carbonic anhydrase inhibitors and prostaglandine analogues were given to a similar percentage of patients in the two glaucoma subgroups. Also, the duration of topical antiglaucoma treatment was similar in both glaucoma subgroups.
Regarding CCT, our results showed the following mean measurements in the groups under study: 526.00 ± 34.30 μm in eyes with PEXG, 549.36 ± 39.3 μm in eyes with POAG, 550.64 ± 39.0 μm in the control group with PXS, and 547.36 ± 33.1 in the control group without PXS (, ). No statistically significant difference was found when comparing CCT values of subjects with POAG to control group with or without PXS (one-way ANOVA test, P = 0.999 and 0.991, respectively). However, subjects with PEXG had statistically significant thinner cornea compared to all the other groups (one-way ANOVA test: POAG group, P = 0.027; control group with PXS, P = 0.039; and control without PXS, P = 0.048). Finally CCT was similar between control groups with or without pseudoexfoliation (one-way ANOVA test, P = 0.992).
Figure 1 Central corneal thickness (CCT) in glaucoma subgroups and control group. The CCT values were measured with the PACLINE OPTICON 2000 S.p.A. The mean CCT with error bars in the different glaucoma and control groups are plotted.
Abbreviations: POAG, primary open-angle glaucoma; PEXG, pseudoexfoliation glaucoma; CTL-PXS, control group with pseudoexfoliation syndrome; CTL, control group without pseudoexfoliation syndrome; CI, confidence interval.
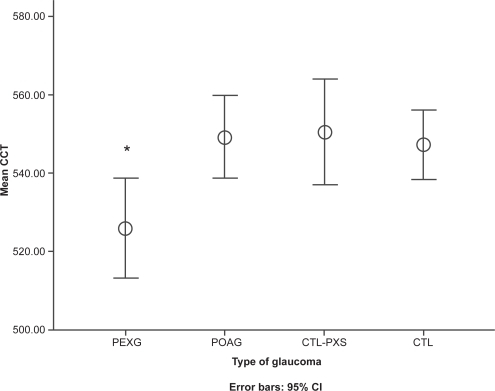
Table 2 Central corneal thickness in glaucoma subgroups and control group
Discussion
It is well known that CCT affects IOP measurements using Goldmann applanation tonometry.Citation1–Citation7 Furthermore, OHTSCitation8 demonstrated that CCT is also an important and independent risk factor for progression to initial glaucoma damage among persons with ocular hypertension. This could be attributed either to the fact that thinner corneas give lower measured IOP levels and these eyes may be subjected to less aggressive IOP-lowering therapy, or thinner corneas may be a risk factor due to an association with the response of the corneoscleral shell and ocular vasculature to IOP-induced stress.
In our study, CCT in POAG eyes did not have any significant difference compared to normal eyes. Our results are in concordance with many published studies.Citation4,Citation15–Citation19,Citation22 Ventura and colleagues,Citation16 Herndon and colleagues,Citation6 and Copt and colleaguesCitation19 compared CCT in patients suffering from POAG and in normal people and concluded that CCT does not differ significantly in these two groups. Although the small sample sizes of these studies could be an issue, Shah and colleagues,Citation4 Jonas and colleagues,Citation18 and Lee and colleaguesCitation17 came to the same conclusion when the CCT of 335, 215, and 343 eyes with POAG, respectively, were compared to normal eyes. On the contrary, according to other reports, CCT in POAG patients was found to be thinner compared to normal individuals.Citation12–Citation14 This difference could be attributed to the different ethnical make-up of the study populations.Citation12 Investigators have shown that CCT is thinner in African Americans compared to Asians and Caucasians.Citation23–Citation25 Furthermore, more African Americans are likely to be in the POAG group since the incidence of POAG is higher in this race. However these demographic data are not presented in most of the above reports. Alternatively, it has been shownCitation26 that CCT is a powerful clinical factor in determining glaucoma severity at the initial examination by a glaucoma specialist. POAG patients with lower CCT had worse baseline visual fields than patients presenting thicker CCT.Citation18,Citation27–Citation29 In the light of this evidence, differences of the glaucoma stage between POAG groups among the various studies could be at least partially responsible for the disparate conclusions.
Concerning CCT in subjects with PEXG and PXS, references in the literature are limited and to a certain degree ambiguous. Previous studies have shown that CCT in patients with PEXG is thinner compared to the control individuals.Citation12,Citation13,Citation15 More specifically, studies by Aghaian and colleaguesCitation12 using an ultrasonic pachymeter have shown that the CCT in patients with PEXG is statistically significant thinner compared to normal individuals. Bechmann and colleaguesCitation13 reached the same conclusion with optical coherence tomography. However, according to other investigators, although CCT was lower in PEXG compared to control subjects this difference was not statistically significant.Citation4,Citation6,Citation16,Citation21,Citation22 The basis for these discordant results is unclear. The small number of included subjects could be a limitation at these studies and could also account for the controversial results.
In their study, Hepsen and colleaguesCitation30 reported that the mean CCT (546.4 μm) in eyes with PXS was not significantly different compared to control eyes (542.9 μm) using optical pachymetry. When those eyes were subcategorized, according to IOP, the CCT was significantly thinner in normotensive PXS eyes compared to those with hypertensive PXS and PEXG eyes. However, hypertensive PXS and PEXG eyes had an IOP higher than 21 mmHg and this could affect the CCT measurements, considering also the fact that corneal endothelial density is decreased in PXS eyes.Citation21
We included a higher number of PEXG subjects in our study compared to the reports above. We further subcategorized the control individuals depending on the presence or not of PXS. Our results showed that PEXG eyes had thinner CCT compared to POAG and normal eyes (with or without PXS).
Kniestedt and colleaguesCitation25 compared PEXG to POAG patients and came to the same conclusion although the POAG group in that study was multiracial. Other reports did not show a difference in CCT between PEXG and POAG subjects, but either the number of PEXG eyes was smallCitation4,Citation16,Citation22 or the POAG group was multiracial.Citation12 Differences in the usage of carbonic anhydrase inhibitors and prostaglandin analogues as antiglaucoma medications has been shown to affect CCT readings,Citation6,Citation31–Citation33 but could not explain our result since there was no variation between the two glaucoma groups concerning their treatment.
A question that arises from our findings is why eyes with PEXG present a thinner cornea compared to those with POAG and PXS.
In our study, subjects with PEXG were recruited from the hospital where they presented with more advanced, glaucoma alterations and thinner CCT compared to subjects with POAG. This fact could be attributed to a delay in the diagnosis or to deficient treatment of subjects with PEXG by their ophthalmologists prior to their visit to our glaucoma department. Indeed, the systematic underestimation of IOP in people with undiagnosed PEXG and thinner corneas, taking into account the nature of PEXG and PXS as having major variations in IOP, deprived the ophthalmologist of the diagnostic value of the most important risk factor (IOP) for the development of glaucoma as well as of the possibility of achieving “target pressure”. Because of this, subjects developed more advanced glaucomatous alterations which led them to a more specialized glaucoma unit in our geographical area in order to be re-evaluated (glaucoma department, University Hospital). This is further confirmed by previous studies, where a significant negative correlation was found between CCT and C/D ratio,Citation25,Citation26 which indicates that patients with thin corneas are more likely to be found in an advance stage of glaucoma at their first presentation. In this way, subjects with advanced PEXG and thin CCT probably enriched our sample and their comparison with less advanced POAG subjects and PXS individuals gave us this statistical result.
If we take for granted that the CCT is an independent biological risk factor, then the co-existence of PXS and thin cornea may increase the risk for development of PEXG. There are studies that indicate a possible biological link between aspects of the front of the eye that can be measured, such as thickness or material properties of the cornea, and the structure, deformability, or physiology of the optic disc, lamina cibrosa, and peripapillary sclera. Findings by OHTSCitation8 and other studiesCitation9–Citation11 have generated an enormous interest in the material properties of the ocular coats of the eye and the likelihood that they may be an underlying factor in some aspects of the genetic susceptibility to glaucoma. Leske and colleaguesCitation9 used confocal scanning laser opthalmoscopy to measure the movement of lamina cibrosa after profound IOP lowering. They found that the lamina moved forward more in patients with thin corneas than in those with thick corneas. Pakravan and colleaguesCitation10 reported that CCT was linked to disc size and thicker corneas were associated with smaller optic disc. Finally, Toh and colleaguesCitation11 showed that CCT is among the most heritable aspects of ocular structure. There may be a biological link between the anterior chamber of the eye (such as CCT) and the peripapillary scleral tissue as well as the properties of the lamina cibrosa. If such a biological link is real then the co-existence of thin CCT with another predisposing factor for the development of glaucoma such as PXS increases the risk of glaucoma in those individuals.
Finally, we showed that CCT was not affected by the presence of pseudoexfoliation in individuals without glaucoma and our result is in agreement with previous studies.Citation34,Citation35 On the contrary, Inoue and colleaguesCitation21 reported thinner corneas in individuals with PXS compared to the control. Finally, Puska and colleaguesCitation36 reported that CCT in eyes with PXS was thicker than the CCT found on the other eye of the same patient that did not have PXS.
In conclusion, our report demonstrates that CCT in subjects with PEXG was statistically significant thinner compared to the CCT of the rest understudy group and specially compared to CCT of individuals with PXS. This may be a statistic result but it could also indicate a possible independent biological role of CCT as a risk factor for the development of glaucoma in subjects with PXS. In that way CCT must be assessed in patients with PXS in order to avoid the underestimation of IOP (in cases with thin cornea). In addition, CCT must be determined in all glaucoma patients in order to achieve “target pressure”, especially in patients with PEXG due to the nature of the disease (major variations of IOP).
Disclosures
The authors report no conflicts of interest in this work.
References
- GoldmannHSchmidtTUeber applanationtonometrieOphthalmologica195713422124113484216
- EhlersNBramsenTSperlingSApplanation tonometry and central corneal thicknessActa Ophthalmol (Copenh)19755334431172910
- DoughtyMJZamanMLHuman corneal thickness and its impact on intraocular pressure measures: a review and metaanalysis approachSurv Ophthalmol20004436740810734239
- ShahSChatterjeeAMathaiMRelationship between corneal thickness and measured intraocular pressure in a general ophthalmology clinicOphthalmology19991062154216010571352
- BrandtJDBeiserJAKassMACentral corneal thickness in the Ocular Hypertension Treatment Study (OHTS)Ophthalmology20011081779178811581049
- HerndonLWChoudhriSACoxTCentral corneal thickness in normal, glaucomatous, and ocular hypertensive eyesArch Ophthalmol1997115113711419298054
- HermanDCHodgeDOBourneWMIncreased corneal thickness in patients with ocular hypertensionArch Ophthalmol2001119333433611231765
- GordonMOBeiserJABrandtJDThe Ocular Hypertension Treatment Study: baseline factors that predict the onset of primary open-angle glaucomaArch Ophthalmol2002120714720discussion 829–830.12049575
- LeskeMRHafezASDescovitsDRelationship between central corneal thickness and changes of optic nerve head topography and blood flow after intraocular pressure reduction in open-angle glaucoma and ocular hypertensionArch Opthalmol20061241115681572
- PakravanMParsaASanagouMCentral corneal thickness and correlation to disc size: a potential link to susceptibility to glaucomaBr J Ophthalmol2007911262816973656
- TohTLiewSHMac KinnonJRCentral corneal thickness is highly heritable: the twin eye studyInvest Opthalmol Vis Sci2005461037183722
- AghaianEChoeJELinSCentral corneal thickness of Caucasians, Chinese, Hispanic, Filipinos, African Americans, and Japanese in a glaucoma clinicOpthalmology200411122112219
- BechmannMThielMGRoesenBCentral corneal thickness-determined with optical coherence tomography in various types of glaucomaBr J Opthalmol200084688691
- WolfsRCKlaverCCVingerlingJRDistribution of central corneal thickness and its association with intraocular pressureAm J Opthalmol1997123767772
- GorezisSGartziosCStefaniotouMComparative results of central corneal thickness measurements in primary open-angle glaucoma, pseudoexfoliation glaucoma, and ocular hypertensionOphthalmic Surg Lasers Imaging2008391172118254346
- VenturaACSBohnkeMMojonDSCentral corneal thickness measurements in patients with normal tension glaucoma, primary open angle glaucoma, pseudoexfoliation glaucoma, or ocular hypertensionBr J Ophthalmol20018579279511423450
- LeeESKimCYHaSJCentral corneal thickness of Korean patients with glaucomaOphthalmology2007114592793017316807
- JonasJBHolbachLCentral corneal thickness and thickness of the lamina cribrosa in human eyesInvest Opthalmol Vis Sci200546412751279
- CoptRPThomasRMermoudACorneal thickness in ocular hypertension, primary open-angle glaucoma, and normal tension glaucomaArch Opthalmol19991171416
- GrodumKHeijlABengtssonBRisk of glaucoma in ocular hypertension with and without pseudoexfoliationOphthalmology2005112338639015745763
- InoueKOkugawaKOshikaTMorphological study of corneal endothelium and corneal thickness in pseudoexfoliation syndromeJpn J Opthalmol200347235239
- YagciREksiogluUMidilliogluICentral corneal thickness in primary open angle glaucoma, pseudoexfoliative glaucoma, ocular hypertension, and normal populationEur J Ophthalmol200515332432815944999
- DohadwalaAAMungerRDamjiKFPositive correlation between Tono-Pen intraocular pressure and central corneal thicknessOphthalmology199810510184918549787354
- BrandtJDBeiserJAKassMACentral corneal thickness in the Ocular Hypertension Treatment Study (OHTS)Ophthalmology2001108101779178811581049
- KniestedtCLinSChoeJCorrelation between intraocular pressure, central corneal thickness, stage of glaucoma, and demographic patient data: prospective analysis of biophysical parameters in tertiary glaucoma practice populationsJ Glaucoma2006152919716633220
- HerndonLWWeizerJSStinnettSSCentral corneal thickness as a risk factor for advanced glaucoma damageArch Ophthalmol20041221172114718289
- PapadiaMSofianosCIesterMCorneal thickness and visual field damage in glaucoma patientsEye200721794394716645628
- ChauhanBCHutchisonDMLeBlancRPCentral corneal thickness and progression of the visual field and optic disc in glaucomaBr J Ophthalmol20058981008101216024855
- Sullivan-MeeMHalversonKDSaxonMCCentral corneal thickness and normal tension glaucoma: a cross-sectional studyOptometry200677313414016513514
- HepsenIFYagciRKeskinUCorneal curvature and central corneal thickness in eyes with pseudoexfoliation syndromeCan J Ophthalmol200742567768017891195
- ArcieriESPierre FilhoPTWakamatsuTHThe effects of prostaglandin analogues on the blood aqueous barrier and corneal thickness of phakic patients with primary open-angle glaucoma and ocular hypertensionEye200822217918316936646
- SenENalcaciogluPYaziciAComparison of the effects of latanoprost and bimatoprost on central corneal thicknessJ Glaucoma200817539840218703951
- WilkersonMCyrlinMLippaEAFour-week safety and efficacy study of dorzolamide, a novel, active topical carbonic anhydrase inhibitorArch Ophthalmol199311110134313508216014
- DetorakisETKoukoulaSChrisohoouFCentral corneal mechanical sensitivity in pseudoexfoliation syndromeCornea200524668869116015087
- ArnarssonADamjiKFSverrissonTPseudoexfoliation in the Reykjavik Eye Study: prevalence and related ophthalmological variablesActa Ophthalmol Scand200785882282718028119
- PuskaPVassaraKHarjuMCorneal thickness and corneal endothelium in normotensive subjects with unilateral pseudoexfoliation syndromeGraefes Arch Clin Exp Opthalmol2000238659663