Abstract
We report on a patient in whom intractable infectious keratitis and subsequent lamellar flap necrosis necessitating flap amputation after laser in situ keratomileusis (LASIK). A 34-year-old woman undergoing LASIK complained of blurred vision and pain in the left eye. The best spectacle-corrected visual acuity was 0.01, and slit-lamp examination showed a marked presence of stromal infiltrates involving the flap and the underlying stroma in that eye. The patient was treated topically with hourly instillation of micronomicin, levofloxacin, and cefmenoxime, together with systemic administration of imipenem, but the left eye developed corneal flap necrosis. We performed surgical debridement of the diseased stroma and excised the lamellar flap. Since nontuberculous mycobacterium was detected on the surgical instruments, we then added oral clarithromycin, and substituted systemic administration of amikacin with that of imipenem. At one month after the flap removal, the visual acuity gradually improved to 0.7, but the stromal opacity of the central cornea and hyperopic shift of +3.0 diopters remained. LASIK can cause intractable keratitis, resulting in significant visual disturbance that presumably results from insufficient antisepsis of the medical instruments used for this surgery, supporting the importance of strict sterilization of these instruments.
Introduction
Laser in situ keratomileusis (LASIK) has gained popularity as an effective means of correcting refractive errors. The onset of infectious keratitis after LASIK has been reported to be a rare complication, but may lead to impairment of visual performance.Citation1–Citation3 It has been demonstrated that infectious keratitis caused by mycobacterium occurs after LASIK.Citation2–Citation5 We present a case in which intractable infectious keratitis and subsequent lamellar flap necrosis necessitating flap amputation, both presumably resulting from inappropriate sterilization of surgical instruments, occur after LASIK, resulting in significant visual disturbance.
Case report
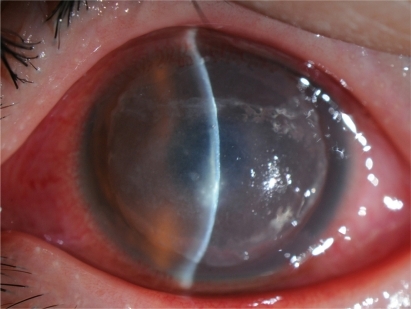
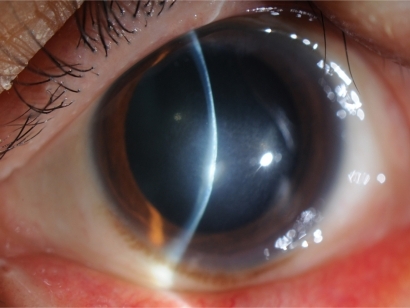
A 34-year-old woman who had undergone bilateral LASIK one month earlier at another eye clinic was referred to our hospital complaining of blurred vision and pain in the left eye. The best spectacle-corrected visual acuity (BSCVA) on the initial visit was 0.01, and slit-lamp examination showed a marked presence of stromal infiltrates involving the flap and the underlying stroma in that eye (). Other ophthalmic examination findings were unremarkable. Corneal scrapings were taken, but the results were negative. The stromal bed was irrigated with micronomicin solutions, and the flap was repositioned at the end of the procedure. The patient was treated topically with hourly instillation of 0.3% micronomicin, 0.5% levofloxacin, and 0.5% cefmenoxime, together with systemic administration of imipenem (2 g/day). One week after our initial treatment, the left eye developed corneal flap necrosis and deterioration of other clinical findings. After obtaining informed consent, we performed surgical debridement of the diseased stroma and excised the lamellar flap to facilitate drug penetration. Since the health care center disclosed that nontuberculous mycobacterium was detected on the surgical instruments, including the microkeratomes, we then added oral clarithromycin (400 mg/day), and substituted systemic administration of amikacin (400 mg/day) with that of imipenem as the treatment regimen. At one month after the flap removal, the BSCVA gradually improved to 0.7, but the stromal opacity of the central cornea and hyperopic shift of +3.0 diopters (D) remained (). No complications (such as iatrogenic keratectasia or recurrent infection) occurred during the three-month observation period.
Discussion
Mycobacterium is an aerobic, Gram-positive bacterium that is present extensively in the environment, for example, in dust, water, soil, and on animals. It has been reported to be one of the major causative organisms of infectious keratitis after LASIK, appearing especially in the late postoperative period.Citation2–Citation5 A cluster of 67 cases of infectious keratitis after LASIK appeared between September 2008 and January 2009 in the referring institution and nontuberculous mycobacterium was isolated from surgical instruments, according to the health care center. Moreover, the antibiotic therapy used initially was not very effective against this post-LASIK keratitis. Thus, we strongly suspect that this infection was caused by nontuberculous mycobacterium, possibly due to intraoperative contamination, although we did not identify the causative organism in our cultures of corneal scrapings. If the organism cultured from corneal scrapings had been in accordance with nontuberculous mycobacterium isolated from surgical instruments, we would have been able to confirm the authenticity of the results. The information from the health care center appears to support the importance of strict sterilization of the medical instruments used for refractive surgery.
This case report emphasizes the difficulties of management of infectious keratitis after LASIK. The patient was treated empirically without microbiologic investigation, resulting in delay of diagnosis and appropriate therapy in this institution. Although a variety of organisms may be involved in infectious keratitis occurring after LASIK,Citation1–Citation3 we should bear in mind that nontuberculous mycobacterium is a possible source of severe post-LASIK infection.
Our findings indicate that LASIK can cause intractable keratitis, resulting in significant visual disturbance that presumably results from insufficient antisepsis of the medical instruments used for this surgery. Surgeons must be responsible for strict sterilization, since this can reduce the risk of infectious keratitis after refractive surgery.
Disclosures
The authors have no financial or proprietary interests in the materials presented herein.
References
- GimbelHVPennoEEvan WestenbruggeJAFerensowiczMFurlongMTIncidence and management of intraoperative and early postoperative complications in 1000 consecutive laser in situ keratomileusis casesOphthalmology1998105183918479787353
- SolomonRDonnenfeldEDAzarDTInfectious keratitis after laser in situ keratomileusis: results of an ASCRS surveyJ Cataract Refract Surg2003292001200614604725
- ChangMAJainSAzarDTInfections following laser in situ keratomileusis: an integration of the published literatureSurv Ophthalmol20044926928015110665
- WinthropKLSteinbergEBHolmesGEpidemic and sporadic cases of nontuberculous mycobacterial keratitis associated with laser in situ keratomileusisAm J Ophthalmol200313522322412566028
- JohnTVelottaENontuberculous (atypical) mycobacterial keratitis after LASIK: current status and clinical implicationsCornea20052424525515778593