Abstract
We look at the case of a 39-year-old female patient suffering from a sudden decrease in her left visual acuity (0.08). Her macular edema was examined using optical coherence tomography, and her optic disc blood flow was examined with laser speckle flowgraphy (LSFG). Additionally, the degree of seriousness of the central vein occlusion was evaluated through fluorescein angiography (FA). Ocular fundus findings revealed central vein occlusion associated with macular edema, and FA determined her disease type as a nonischemic-central vein occlusion. Daily doses of 100 mg of aspirin were administered orally to the patient. Upon administration, her ocular blood flow almost immediately increased. In this study, we demonstrate the potential of LSFG as a means to investigate ocular blood flow.
Introduction
Laser speckle flowgraphy (LSFG) can noninvasively measure both major and minute vessels of the retinal blood flow in real time.Citation1 This method can visualize retinal blood flow by using laser dispersion.Citation2 The obtained data indicate a relative value of retinal blood flow levels and therefore can easily be compared consecutively.Citation2 As far as we can ascertain, to date no study is available that describes the effects of internal medicines toward optic nerve head (ONH) blood flow levels in patients with retinal vein occlusion, although several drugs, including anticoagulants, are frequently used in our clinic. We report herewith a unique case of (nonischemic) central retinal vein occlusion (NI-CRVO) associated with macular edema successfully treated by oral aspirin administration. The case caused significant improvement of the ONH blood flow levels through LSFG and retinal hemodynamics through fluorescein angiography (FA).
Case report
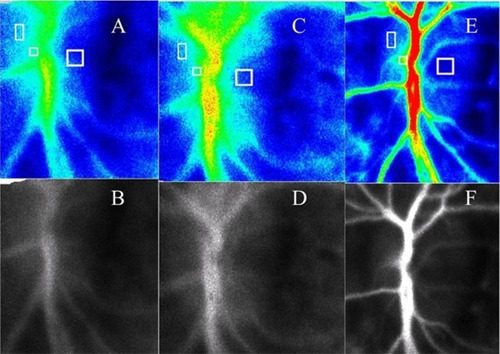
A 39-year-old woman noticed a sudden decrease in her left visual acuity and was referred to our hospital two days later. Her decimal visual acuity was 1.2/OD and 0.08/OS. Ocular fundus findings included massive dilatation of the retinal veins, widespread dot-blot hemorrhages, and multiple cotton-wool spots (). In addition, macular edema was determined by optical coherence tomography (Zeiss Straus OCT; OCT3, Carl Zeiss Meditec, Jena, Germany) (). Based on these findings, and because FA showed no presence of nonischemic lesions, she was diagnosed as having nonischemic central retinal vein occlusion (NI-CRVO) associated with macular edema. LSFG indicated ONH blood flow levels were markedly decreased (). No systemic diseases, including hypertension, were detected. Oral aspirin treatment was then administered to the patient (100 mg/day). The macular edema and the ONH circulation, particularly the central retinal artery (CRA) blood flow, improved a few days after the aspirin administration was initiated (, ), and her left visual acuity also improved to 0.8. Three months later, her visual acuity was restored to 1.2, and macular edema had disappeared completely (). In terms of ocular hemodynamics, LSFG showed a further increase of CRA blood flow and no abnormal findings by FA ().
Figure 1 The flourescein angiography photograph (B) shows a fluorescence block for multiple dot subretinal hemorrhage, cotton-wool spots and vein meandering with the color fundus photograph (A), but it does not show the avascular area. Three months later, the fundus photograph (C) shows an almost normal retina appearance although dot subretinal hemorrhage and cotton-wool spots remain. The flourescein angiography photograph (D) shows no abnormality. The OCT shows remarkable macular edema, with the macular thickness indicated at 638 μm (E). (F) Macular thickness the following day shows 220 μm. The retinal thickness was reduced to 140 μm three months later.
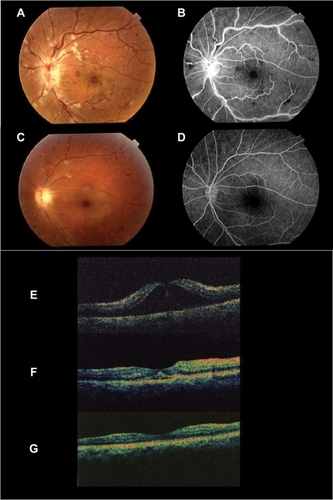
Figure 2 Optic nerve head blood flow levels by LSFG. We show examinations with LSFG from the first and second days, as well as three months later. B, D, and F are monochrome-converted images of A, C and E, respectively, which makes observing optic nerve heads and vessels easier. The square shows the blood flow (A, C, E) measurement part of CRA, both the optic nerve head of the nasal side as well as the temporal side. The blood flow rate in the CRA improved by 84.3%, on the temporal side it improved by 32% and that of the nasal side showed a 3.9% improvement. Three months later, the CRA blood flow rate was shown to have improved by 253%, although that of the temporal side and nasal side of ONH decreased by 10% and 15%, respectively.
Discussion
Retinal vein occlusion (RVO) is the second most common retinal vascular disease after diabetic retinopathy, affecting not only the elderly, but also young patients.Citation3 NI-CRVO is a disorder associated with macular edema and can heal spontaneously, but the time period in which macular edema heals is unknown. In NI-CRVO, retinal vein thrombosis or unidentified immunity-related vasculitis causes increased venous pressure and, as a result, may lead to retinal capillary decompensation with macular edema.Citation4 We investigated this by utilizing PubMed internet research concerning the connection between the increment of the central retinal artery flow and rapid recovery from macular edema. Unfortunately, we could not find pertinent information on this matter. The pathogen of the CRVO in young people suggested a systemic disorder or arteriovenous communications of the retina.Citation3 However we did not find any systemic disorders or retinal vessels abnormalities in the patient. Her retinal symptoms showed remarkable improvement after oral aspirin administration. We considered the possibility that thrombotic release of the central retinal vein was accompanied with CRA blood flow improvement based on reports that CRVO is caused by CRA thrombosis.Citation5 Due to the fact that CRA blood flow change was rapid, LSFG seems to be an optimal method to measure the short-term hemodynamics. As for the examination for FA, an evaluation of the vasa sanguinea retinae hemodynamics is possible, but quantifying retinal blood flow improvement is difficult unless a special device is utilized.Citation6 Moreover, FA is invasive and repeated experimentation over a short period is difficult. In the present report, a significant increase in the ONH blood flow levels due to an increase of LSFG was recognized upon oral administration of aspirin, and this correlated with macular edema reduction by OCT and visual acuity improvement. It is unknown whether macular edema and central retinal artery blood flow were improved by aspirin administration or by natural causes, but implication of LSFG evaluation of the hemodynamics of the ONH circulation may be a promising tool for monitoring the progression of retinal vascular diseases.
Disclosures
The authors report no conflicts of interest in this work.
References
- GoroWHitoshiFShojiKImaging of choroidal hemodynamics in eyes with polypoidal choroidal vasculopathy using laser speckle phenomenonJpn J Ophthalmol20085217518118661267
- YasuhiroTMakotoAKenTMiyukiNAtsuoTHitoshiFReal-time measurement of human optic nerve head and choroid circulation, using the laser speckle phenomenonJpn J Ophthalmol19974149549147189
- GiuffréGRandazzo-PapaGPalumboCCentral retinal vein occlusion in young peopleDocumenta Ophthalmologica1992801271321425127
- VerougstraeteCDemolSMacular edema in retinal vein occlusionBull Soc Belge Ophthalmol19912403547
- HolminNPlomanKGThrombosis of central vein of retina treated with heparinLancet19381664
- HickamJBFrayserRA photographic method for measuring the mean retinal circulation time using fluoresceinInvest Ophthalmol196548768844953505