Abstract
We report a case of paraneoplastic retinopathy associated with a retroperitoneal liposarcoma. A 42-year-old man was referred to our hospital with complaints of night blindness and blurred vision in the peripheral field. Electroretinograms showed a progressive amplitude reduction in his both eyes. Abdominal magnetic resonance imaging showed a large retroperitoneal mass, and pathologic examination revealed a dedifferentiated liposarcoma. Western blot analysis showed an antiretinal antibody in the serum of our patient, and his serum reacted with the photoreceptors of a bovine retina. To the best of our knowledge, this is the first case of paraneoplastic retinopathy associated with a liposarcoma.
Introduction
Paraneoplastic retinopathy (PR) is a progressive retinal disease caused by antibodies generated from neoplasms distant from the eye.Citation1–Citation3 The retinopathy can develop either before or after the diagnosis of the neoplasm. Patients with PR usually have night blindness, photopsia, ring scotoma, attenuated retinal arteriole, and abnomal electroretinograms (ERGs). PR is thought to be mediated by an autoimmune mechanism, and is associated with the presence of antiretinal autoantibodies in the serum.
Various types of neoplasms are known to cause PR, including malignancies of the lung, breast, cervix, colon, prostate/bladder, uterus/endometrium, and blood cells. Only two cases of PR associated with a sarcoma, a malignant tumor arising from mesenchymal cells, have been reported.Citation4,Citation5 We report a case of PR associated with a retroperitoneal liposarcoma. The patient’s visual symptoms preceded the discovery of the tumor by six months.
Case report
A 42-year-old man was referred to our hospital with complaints of night blindness and blurred vision in the peripheral field. He did not have any systemic or eye diseases including a malignant tumor, and the family history revealed no other members to have any eye diseases.
At the initial examination, his best-corrected visual acuity was 1.0 in both eyes, but Goldmann perimetry showed defects in the mid-peripheral visual fields in both eyes (). Ophthalmoscopy showed that the fundus was nearly normal, but fluorescein angiography demonstrated mottled hyperfluorescence along the vascular arcades (). The ERG amplitudes of both the rod and cone components were reduced (, middle column). Based on these findings, we diagnosed him as having a rod-cone dystrophy.
Figure 1 Ophthalmologic findings in a case of paraneoplastic retinopathy. A) Visual field obtained by Goldmann perimetry showing ring scotomas in both eyes. B) Fundus photographs of our patient. C) Fluorescein angiograms of our patient. D) Results of full-field ERGs. The ERG amplitudes of both the rod and cone components are reduced and were smaller at the six-month followup examination.
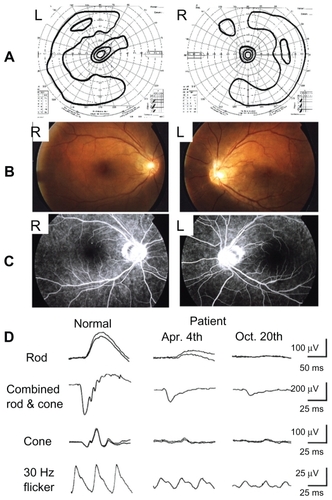
However, his symptoms progressively worsened, and the amplitudes of the ERGs were further reduced six months after the initial examination (, right column). We then suspected PR, and performed systematic magnetic resonance imaging (MRI). The abdominal MRI showed a large retroperitoneal mass (, arrow) which compressed the left kidney.
Figure 2 Systemic and histologic findings in a case of paraneoplastic retinopathy. A) Abdominal MRI showing a large retroperitoneal mass (arrow), which compressed the left kidney. B) Western blot analysis of patient’s serum using bovine retinal protein. The serum reacted to an 83 kD antigen (arrow). C) Immunohistochemical analysis using patient’s serum demonstrates autoreactivity against the photoreceptors of bovine retina. D) Gross appearance of tumor. E) Microscopic appearance of retroperitoneal tumor (× 20). Two characteristic patterns of well differentiated liposarcoma (asterisk) and dedifferentiated fibrotic sarcomatoid tissue (arrow) can be seen.
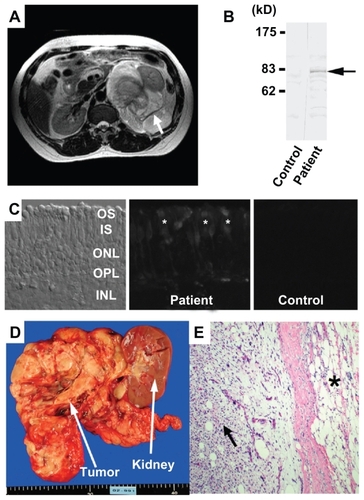
We also performed Western blot analysis using bovine retinal proteins to determine whether there were any antiretinal antibodies in the serum of our patient. A retinal protein of approximately 83 kD (, arrow) was detected in the serum of this patient. We also confirmed that the serum reacted with the photoreceptors of a bovine retina ().
We then diagnosed our patient as having PR associated with retroperitoneal tumor, and the tumor as well as the left kidney was removed (). Pathologic examination revealed a dedifferentiated liposarcoma that contained the characteristic two patterns of a well differentiated liposarcoma (, asterisk) and dedifferentiated fibrotic sarcomatoid tissue (, arrow). After the tumor was resected, he received chemotherapy but he had a recurrence with metastasis. His status became unknown after he moved to his hometown for terminal care.
Comments
A PubMed search for cases of PR associated with a sarcoma yielded two cases.Citation4,Citation5 One case involved a uterine sarcoma, and the other a rhabdomyosarcoma of the thorax. To the best of our knowledge, this is the first case of PR associated with a liposarcoma. A liposarcoma is a malignancy of fat cells that occurs in deep soft tissue and is mostly seen in the limbs and retroperitoneum.Citation6 It is the most common soft tissue sarcoma and accounts for approximately 20% of all mesenchymal tumors. Most of the patients with liposarcoma have no symptoms until the tumor becomes large and causes pain or functional disturbances in neighboring organs.
We detected an antiretinal antibody in the serum of our patient, and found that the serum reacted with the photoreceptors of a bovine retina, suggesting that this antibody caused the retinopathy of our patient. However, we did not confirm that this antibody actually reacted to the tumor proteins of our patient. Thus, additional experiments are needed because it is known that the antiretinal antibody can be produced not only in PR, but also in other retinal degenerative diseases as a secondary complication of retinal cell death.Citation7
Our experience with this case demonstrated that it is important for ophthalmologists to be aware that liposarcoma can be the cause of PR. In these cases, the visual symptoms may precede the discovery of this tumor, because liposarcoma usually grows silently in deep soft tissues without any local symptoms.
Acknowledgments
Grant support for this research was received from Health Sciences Research Grants (H16-sensory-001) from the Ministry of Health, Labor and Welfare, Japan, and Ministry of Education, Culture, Science and Technology (Numbers 18591913 and 18390466), Japan.
Disclosures
The authors report no conflicts of interest in this work.
References
- ThirkillCEFitzGeraldPSergottRCCancer-associated retinopathy (CAR syndrome) with antibodies reacting with retinal, optic-nerve, and cancer cellsN Engl J Med1989321158915942555714
- AdamusGAutoantibody targets and their cancer relationship in the pathogenicity of paraneoplastic retinopathyAutoimmun Rev2009841041419168157
- ChanJWParaneoplastic retinopathies and optic neuropathiesSurv Ophthalmol200348123812559325
- EltabbakhGHHoogerlandDLKayMCParaneoplastic retinopathy associated with uterine sarcomaGynecol Oncol1995581201237789878
- HammersteinWJürgensHGöbelURetinal degeneration and embryonal rhabdomyosarcoma of the thoraxFortschr Ophthalmol1991884634651757033
- FerrarioTKarakousisCPRetroperitoneal sarcomas: Grade and survivalArch Surg200313824825112611567
- HeckenlivelyJRFerreyraHAAutoimmune retinopathy: A review and summarySemin Immunopathol20083012713418408929