Abstract
Periocular xanthogranulomatous diseases are a rare group of disorders which are characterized by a predilection to affect the orbit and ocular adnexa and special histopathological features, in particular infiltrates comprising non-Langerhans-derived foamy histiocytes and Touton giant cells. The differential diagnosis is difficult and occasionally definite diagnosis cannot be established even after clinical and histopathological findings are taken together. We describe a case of a middle-aged man who presented with a 10-year history of voluminous eyelid swelling with concomitant late-onset atopic manifestations, namely bronchial asthma and allergic rhinitis with nasal polyps. After thorough clinical and laboratory investigation, including a biopsy of the eyelid, we classified the patient’s disease to a rare entity that has been relatively recently described: periocular xanthogranuloma associated with adult-onset asthma. In a review of the literature, no prospective trials concerning the treatment of this disease were found. The literature mainly contained case reports and case series in which corticosteroids and chemotherapy with alkylating agents have been reported to be beneficial. We treated our patient with a combination of oral corticosteroids and cyclophosphamide pulses and we observed substantial regression of the eyelid masses together with a normalization of systemic immunologic abnormalities.
Introduction
Xanthogranulomatous diseases of the orbit are a group of rare disorders of unknown etiology and pathogenesis affecting the skin and subcutaneous tissues of the periorbital areas and the ocular adnexa. They are a form of non-Langerhans cell histiocytosis. The group displays considerable heterogeneity with some patients manifesting only local symptoms and signs at the face, and others manifesting systemic disorders, while its severity spans from an indolent disease to an invasive disease that may even lead to death.Citation1 Diagnosis is difficult and in some cases clinicopathological investigation fails to provide a classification more specific than non-Langerhans histiocyte proliferative disorder. Its treatment is largely empirical due to the rarity of the disease. Most published data concern small case series or case reports. Below we present a case of a man with long-standing periorbital xanthogranuloma who was treated with cyclophosphamide (CYC) and methylprednisolone (MP). Informed consent and approval of the Local Institutional Ethical Committee was obtained.
Case report
A 53-year-old Caucasian man presented to our outpatient rheumatology clinic for bilateral periorbital swelling. It had first started 10 years earlier with gradual swelling of both upper and lower eyelids and cheeks. The swelling was painless with a yellow–orange discoloration without other abnormalities of the overlying skin. It was so voluminous that it limited the opening of the eyes and distorted the patient’s physiognomy. Two years prior to the periorbital swelling he had developed bronchial asthma and allergic rhinitis with nasal polyps. Later, hypertension, benign prostate hyperplasia, and depression occurred. His family history also revealed hypertension and cardiovascular events. A few years before presenting to us, he had been investigated in a dermatologic hospital where he had an eyelid biopsy performed, consistent with xanthogranuloma. He was treated with immunoglobulin infusions, corticosteroids per os and isotretinoin without sustained improvement.
On physical examination, his vital signs were normal. There was obvious swelling of all four eyelids, the cheeks and temples which consisted of a painless, soft, slightly lobular tissue (). The patient’s vision and ocular motility were not affected, although the opening of the eyes was limited. The rest of his physical examination was unremarkable.
Laboratory investigation showed eosinophilia (total eosinophils 1085/μL) and elevated acute phase reactants (erythrocyte sedimentation rate 53 mm/hour; C-reactive protein 9 mg/L [normal < 6 mg/L]). Urinalysis, liver and kidney biochemistry, serum lipid profile and thyroid hormones were normal. Antithyroid autoantibodies were negative. Immunological tests showed elevated IgG immunoglobulin (2500 mg/dL, normal 751–1560 mg/dL), a slightly depressed IgA and normal IgE levels. Serum protein electrophoresis showed diffuse hypergammaglobulinemia without evidence of a monoclonal protein. Serum complement levels (C3 and C4) were low. Rheumatoid factor, antinuclear antibodies and anti-neutrophil cytoplasmic antibodies were negative.
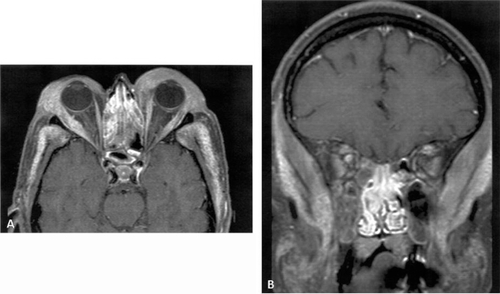
X-rays of the chest and the long bones were normal. A magnetic resonance imaging (MRI) of the orbits demonstrated eyelid swelling, mucosal thickening of all sinuses and abnormal signal and contrast uptake of the temporal, masseter and pterygoid muscles bilaterally corresponding to infiltration by a pathological process. Moreover, the oculomotor muscles were swollen and infiltrated with pathological signal intensity (). Computed tomography (CT) of the lungs showed small interstitial nodules, bronchiolitis-like opacities and hilar lymph node enlargement (up to 2 cm). Abdominal CT was unremarkable. Pulmonary function tests showed mild expiratory flow limitation. Pure protein derivative skin test was negative.
Figure 2 Axial A) and coronal B) contrast-enhanced fat-suppressed T1-weighted MR images showing bilateral eyelid, lateral rectus oculomotor, masticatory and temporal muscle enlargement and enhancement.
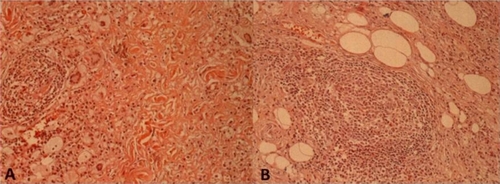
A new biopsy of the left upper eyelid showed large areas of xanthogranulomatous infiltration throughout the reticular dermis into the subcutaneous fat. The granulomatous infiltrate was composed of lymphocytes, epithelioid cells, foamy histiocytes and giant cells, many of them of Touton type. Foreign body giant cells were also present. The lymphocytes were numerous and nodular lymphocytic aggregates were occasionally present (). There was no evidence of necrobiosis, but foci of fibrosis could be observed. Immunohistochemistry showed that the histiocytes were CD68 positive and S-100 negative.
Figure 3 Diffuse infiltrate rich in lymphocytes, foamy histiocytes, and giant cells (hematoxylin and eosin: x250). A) Giant cells of Touton type, B) nodular lymphoid infiltrate.
Clinical differential diagnosis included xanthelasma, thyroid disease, sarcoidosis, allergic granulomatosis, non-Langerhans histiocytoses (juvenile xanthogranuloma, papular xanthoma, xanthoma disseminatum), periocular xanthogranuloma with adult-onset asthma (PXAOA), necrobiotic xanthogranuloma (NXG) and Erdheim–Chester disease (ECd). Immunological and histopathologic studies excluded the first four diagnoses. Considering that the patient suffered from an infiltrative nonmalignant non-Langerhans histiocytic disorder that was limited to facial structures and was associated with elevated acute phase reactants, a polyclonal activation of the humoral arm of the adaptive immunity, and atopic manifestations, we favored the diagnosis of PXAOA.
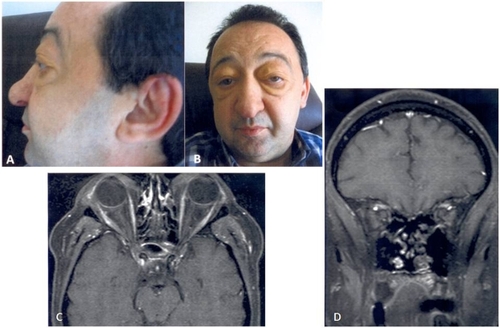
The patient was treated with 6 monthly infusions of CYC 750 mg/m2 body surface area and MP 0.8 mg/kg body weight per os with gradual tapering. After completion of all six CYC infusions the periorbital swelling had significantly regressed (), complement levels had normalized and a repeat MRI of the orbits showed regression of the swelling and of the abnormal signal of the eyelids and the masticatory and oculomotor muscles (). MP was further tapered, while azathioprine was added to maintain the effect of the CYC/MP combination and allow for further corticosteroid tapering.
Figure 4 Six months of treatment. Significant regression of eyelid swelling (A, B). Follow-up MRI: axial (C) and coronal (D) contrast-enhanced fat-suppressed T1-weighted MR images shows normalization of eyelid, lateral rectus oculomotor, masticatory and temporal muscle.
Discussion
Nonmalignant non-Langerhans histiocytoses are classified on the basis of the cell types that predominate in the histopathologic specimens and on whether the lesions are solitary, multiple or systemic.Citation2 Diseases with predominant xanthomatized histiocytes, such as juvenile xanthogranuloma, papular xanthoma, xanthoma disseminatum, etc, form a major part of this group. Pathologically, they typically demonstrate an abundance of foamy histiocytes and Touton giant cells. The age of disease onset, the specific skin changes and the potential involvement of other organs and tissues, including the orbit and ocular adnexa, varies according to the particular disease subtype.Citation3,Citation4
NXG displays histopathologic features similar to xanthogranulomas, ie, foamy cells and Touton giant cells in relation with areas of collagen degeneration, lymphoid aggregates or follicles occasionally with germinal centers, plasma cell foci and cholesterol clefts.Citation5 It affects equally men and women in their sixth decade and usually involves the periorbital areas, trunk, and proximal parts of the extremities. Lesions initially resemble xanthelasmas, but they gradually progress to indurate yellow-brownish plaques with a tendency to ulcerate and even cause destructive skin changes. Ocular manifestations include conjunctivitis, scleritis, corneal perforation, uveitis and orbital mass. It is often associated with immune dysfunction, namely monoclonal paraproteinemia (80%), hypocomplementemia and cryoglobulinemia, whereas it occasionally is associated with multiple myeloma, non-Hodgkin lymphoma (NHL) or other hematologic dyscrasias.Citation6 Association with bronchial asthma is weak, if any.Citation4 The cause of the disease remains elusive, although it is presumed that special functional properties of the paraprotein are responsible for an aberrant immune response.Citation6
ECd is characterized by abnormal and aggressive proliferation of non-Langerhans foamy histiocytes. The main manifestations are osteosclerosis of the diaphyses and metaphyses of the long bones and diabetes insipidus due to pituitary involvement. Ocular manifestations include xanthelasma-like lesions and exophthalmos and respiratory involvement includes pulmonary infiltrates, fibrosis and pleural effusion.Citation4,Citation7
Recently, Jakobiec and colleaguesCitation4 described six patients with periocular xanthogranuloma and concomitant asthma. They termed the condition periocular xanthogranuloma with adult-onset asthma. One of the patients, on whom a necrobiotic lesion was observed later in the disease course, developed paraproteinemia as well. Hence, the researchers suggested there might be an overlap between NXG and PXAOA. Whether they form different aspects of the same disease spectrum or are different diseases is not clearly evident. On clinical grounds, relating PXAOA and NXG might have therapeutic and prognostic implications, particularly regarding the risk for hematologic dyscrasias.
Sivak-Callcott and colleaguesCitation1 reviewed 137 cases of adult xanthogranulomatous disease of the orbit and ocular adnexa, among them 21 cases of PXAOA, 72 cases of NXG and 36 cases of ECd. Patients with PXAOA often had signs of immune dysfunction, such as polyclonal gammapathy and reactive lymphadenopathy, while one patient developed Burkitt’s lymphoma and another NHL. Histopathologically NXG more often showed pallisading epithelioid histiocytes together with necrobiosis, while large lymphocytic aggregates were more common in PXAOA. Fibrosis was more evident in ECd.
Our patient had periorbital disease with concurrent immunological abnormalities, namely mediastinal lymphadenopathy, hypocomplementemia, and diffuse hypergammaglobulinemia. Furthermore, atopic phenomena (asthma, rhinosinusitis, eosinophilia) were present. These had appeared close to the onset of the eyelid swelling. ECd diagnosis was rejected because there was no bone involvement, while lung manifestations in ECd do not include asthma.Citation4 Juvenile xanthogranuloma can be differentiated on clinical grounds (lesions are usually solitary, but, when multifocal, other parts besides the eyelids are commonly affected).Citation3 Xanthoma disseminatum can be excluded, since the patient exhibited no axillary or inguinal lesions and no mucosal involvement.Citation3 Papular xanthoma histologically rarely exhibits inflammatory infiltrates.Citation3
Regarding NXG, whereas no sites of necrobiosis were evident in two histopathological examinations, the presence of such lesions elsewhere in the pathological tissue cannot be excluded. Furthermore, foci of fibrosis were observed that might represent scarring of a previously necrobiotic focus. However, ulceration or ocular inflammation had never occurred in 10 years and no monoclonal B-cell abnormality could be observed. For those reasons we classified the patient as suffering from PXAOA.
The management of the condition remains empirical, due to its rarity. Surgical excision is often followed by disease recurrence and scarring.Citation4,Citation6 Orbital radiotherapy and topical corticosteroids have been used with variable results in some cases of NXG.Citation5,Citation6,Citation8 Patients with PXAOA often admit improvement of periorbital swelling, whenever treated with systemic corticosteroids for their asthma.Citation4,Citation9 There have also been various reports of PXAOA responding to systemic corticosteroids, but the disease often recurs after corticosteroid withdrawal, as was the case for our own patient as well.Citation10 There are also several reports of effective treatment of NXG with chemotherapeutic agents particularly alkylating agents, such as chrorambucil, melphalan and CYC alone or in combination with corticosteroids.Citation5,Citation6,Citation8,Citation11,Citation12 Jakobiec suggests that patients without systemic disease receive a course of high-dose systemic steroids and periorbital radiotherapy; if the disease does not respond, then light chemotherapy with corticosteroids could be administered.Citation4
Long-term outcomes of PXAOA following various therapeutic modalities are rarely reported. Two of three patients reported by Jakobiec relapsed after surgery and corticosteroids were only temporarily effective in one of them. One patient with concomitant monoclonal gammapathy responded to combined chemotherapy.Citation4 In the series by Sivak-Callcott, surgery was successful in six out of eight and corticosteroids in two out of two cases of PXAOA.Citation1 A 46-year-old patient worsened after topical radiotherapy and later, following treatment with a combination of corticosteroids and cyclosporine A, he developed a lymphoma. The disease ultimately responded to bone marrow suppressive treatment and longterm low dose prednisone. Another patient, though, responded to the corticosteroids-cyclosporine A combination. Overall, no deaths due to PXAOA were reported.Citation1
In rheumatology considerable experience exists concerning the use of CYC in inflammatory diseases owing to B-cell dysregulation, such as lupus nephritis, or granulomatous autoimmune diseases, such as Wegener’s granulomatosis and Churg–Strauss syndrome. We thus treated the patient with 6 monthly CYC infusions and MP aiming at a rapid suppression of the inflammatory process and a disease regression that would sustain after corticosteroid withdrawal.
As regards prognosis, the potential overlap between PXAOA and NXG and the known association of NXG with hematologic malignancies require close follow-up of the patient in order to timely uncover a potential emerging malignancy. Thus, regular clinical evaluation, full blood count, inflammatory markers, and serum protein electrophoresis should be performed.
Disclosures
The authors report no conflicts of interest in this work.
References
- Sivak-CallcottJARootmanJRasmussenSLAdult xanthogranulomatous disease of the orbit and ocular adnexa: new immunohistochemical findings and clinical reviewBr J Ophthalmol20069060260816622091
- ZelgerBWSidoroffAOrchardGNon-Langerhans cell histiocytoses. A new unifying conceptAm J Dermatopathol1996184905048902096
- Macrophage/monocyte disordersJamesDWBergerTGElstonDMAndrews’ Diseases of the Skin–Clinical Dermatology10th editionPhiladelphia, PAElsevier2006714718
- JakobiecFAMillsMDHidayatAAPeriocular xanthogranulomas associated with severe adult–onset asthmaTrans Am Ophthalmol Soc199391991258140711
- MehreganDAWinkelmannRKNecrobiotic xanthogranulomaArch Dermatol1992128941001739294
- Fernández-HerreraJPedrazJNecrobiotic xanthogranulomaSemin Cutan Med Surg20072610811317544963
- Veyssier-BelotCCacoubPCaparros–LefebvreDErdheim–Chester disease. Clinical and radiologic characteristics of 59 casesMedicine (Baltimore)1996751571698965684
- WoodAJWagnerMVAbbottJJNecrobiotic xanthogranuloma: a review of 17 cases with emphasis on clinical and pathologic correlationArch Dermatol200914527928419289757
- VickVLWilsonMWFlemingJCOrbital and eyelid manifestations of xanthogranulomatous diseasesOrbit20062522122516987770
- HammondMDNiemiEWWardTPAdult orbital xanthogranuloma with associated adult–onset asthmaOphthal Plast Reconstr Surg200420329332
- MeyerSSzeimiesRMLandthalerMCyclophosphamide–dexamethasone pulsed therapy for treatment of recalcitrant necrobiotic xanthogranuloma with paraproteinemia and ocular involvementBr J Dermatol200515344344516086766
- KhanIJAzamNASullivanSCNecrobiotic xanthogranuloma successfully treated with a combination of dexamethasone and oral cyclophosphamideCan J Ophthalmol20094433533619491994
