Abstract
Objective:
To evaluate health care resource utilization in patients with schizophrenia who continued newly prescribed antipsychotic medications, compared with those switching to different treatments.
Methods:
Adults with schizophrenia in the California Medicaid (MediCal) database who initiated treatment with index medications in 1998–2001, were classified as having: 1) abandoned antipsychotic medications; 2) switched to another medication; or 3) continued with the index antipsychotic, for up to 6 months after the index date.
Results:
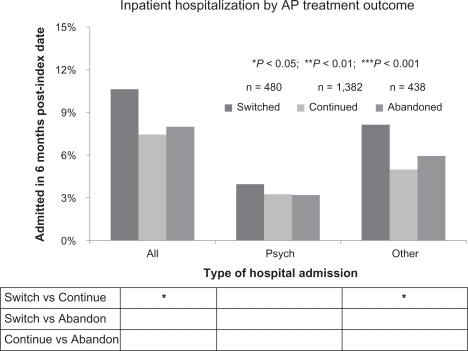
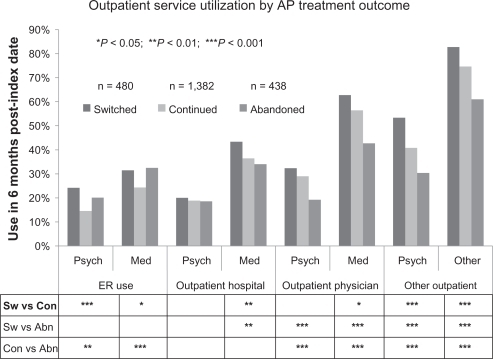
Of 2300 patients meeting eligibility criteria, 1382 (60.1%) continued index medications, 480 (20.9%) switched, and 438 (19.0%) abandoned antipsychotic treatment. Utilization in several resource categories occurred significantly more frequently among patients whose regimens were switched (vs those continuing index medications). These included using psychiatric (24.2% vs 14.5%; P < 0.001) or nonpsychiatric (31.5% vs 24.3%; P < 0.05) emergency services; being admitted to a hospital (10.6% vs 7.4%; P < 0.05); making nonpsychiatric outpatient hospital visits (43.3% vs 36.4%; P < 0.05) or nonpsychiatric physician visits (62.7% vs 56.4%; P < 0.05); and using other outpatient psychiatric (53.3% vs 40.7%; P < 0.001) or nonpsychiatric (82.7% vs 74.6%; P < 0.001) services.
Conclusions:
Switching antipsychotic medications is associated with significantly increased health care resource utilization (vs continuing treatment).
Introduction
Many patients with schizophrenia experience suboptimal treatment outcomes with their initially prescribed antipsychotic agent and require a clinically warranted medication switch.Citation1–Citation4 Although medication switches represent sound “rescue” options, they are also typically indicative of suboptimal treatment outcomes with the first therapy.Citation5–Citation8 Patients for whom psychotropic medications prove to be ineffective may experience worse or more prolonged symptoms, have more marked progression of their illness, and, in severe cases, harm themselves or others.Citation9–Citation11 However, the implications of such adverse treatment outcomes with respect to health care resource utilization are unclear. The objective of the present study was to compare health care resource utilization among patients with schizophrenia who switched to a different antipsychotic medication, with resource utilization among those who continued on their newly prescribed antipsychotic medication.
Methods
Study design and population
This exploratory retrospective analysis evaluated a sample of patients from the MediCal administrative claims database treated during the period of October 1, 1998 through September 30, 2001. MediCal is a large, prepaid health plan with an enrollment of approximately 8.5 million participants in 2001.Citation12
The index date was the earliest date of an antipsychotic medication prescription for which there was no prescription for the same medication in the preceding 90 days. Eligible patients were aged 18 to 50 years and continuously enrolled in Medicaid from 90 days before the index date until 180 days after the index date. In addition, patients were required to meet 1 of the following definitions of schizophrenia: a) 1 inpatient or 2 or more outpatient claims with an International Classification of Diseases, Ninth Revision (ICD-9) diagnostic code of 295.xx in the year before the index date; or b) 1 outpatient claim with an ICD-9 diagnostic code of 295.xx before or on the index date and 1 or more claims with the same diagnostic code within 180 days of the index date. Eligible patients were also required to have initiated a single index antipsychotic on the index date. Patients dually enrolled in Medicaid and Medicare were excluded because the MediCal database did not contain detailed claims on Medicare-covered inpatient hospitalizations.
Definitions and assessments
Patients were designated by medication start categories on the basis of prescriptions filled before the index date (). Patients with no antipsychotic prescriptions filled in the year preceding the index date were defined as new users; those who filled an antipsychotic prescription 91 to 365 days before the index date, but did not fill a prescription in the 90 days immediately preceding the index date, were defined as restarters. Those who filled prescriptions for any antipsychotic during the 90 days before the index date were defined as established users.
Table 1 Patient characteristics by start categories
Prescription claims were tracked beginning on the index date to determine if patients continued their index medication, and these data were used to assign patients to outcome categories. “Continued” patients filled pharmacy claims for the index medication (alone or with augmentation) during the reference period, defined as days 91 to 180 after the index date. “Switched” patients discontinued the index medication and switched to a nonindex antipsychotic, as documented by pharmacy claims during the reference period. “Abandoned” patients discontinued antipsychotics altogether (no antipsychotic pharmacy claims) during the reference period. Medicaid service utilization was assessed for 180 days after the index date. Categories of service use included emergency room (ER) visits, inpatient hospitalizations, outpatient hospital care, physician visits, and other outpatient services. Service use for each of these categories was analyzed according to whether the service was coded as psychiatric or nonpsychiatric, with each patient categorized according to whether they did or did not use that type of service. We did not conduct analyses according to the intensity of service use by patients.
Baseline patient characteristics were determined retrospectively for both the start and outcome categories. High-intensity comorbidities were ascertained using the diagnostic categories defined in the Chronic Illness and Disability Payment System (CDPS), a diagnostic classification system employed by Medicaid to make health-based payments.Citation13 Diagnoses recorded in the medical claims are categorized by diagnostic category (eg, psychiatric, cardiovascular, cancer, diabetes) and within each diagnostic category, a ranking of intensity from very high to extra low based upon the Medicaid costs associated with treating patients in that group. For example in the psychiatric category, schizophrenia is classified as high; bipolar affective disorder as medium; and other depression, panic disorder, and phobic disorder each as low. We defined high-intensity comorbidities as those with CDPS rankings of high or very high.”
Statistical analyses
Chi-square analyses were conducted to compare proportions of patients utilizing health care services between start and outcome categories. Tests of significance were conducted at an a priori two-tailed α = 0.05.
Results
Of 64,324 unique antipsychotic users during the study period, 3990 met the study inclusion criteria, and 2300 were Medicaid-only recipients eligible for the study. In all, 622 (27.0%) patients were categorized as new users, 632 (27.5%) as restarters, and 1046 (45.5%) as established users.
Six months after the index date, 1382 (60.1%) patients continued on their index medication, 480 (20.9%) switched to another antipsychotic, and 438 (19.0%) abandoned antipsychotic treatment (). As shown in , individuals who abandoned antipsychotic medications had a significantly different race/ethnic distribution than those who continued (P < 0.001) and those who switched (P = 0.001). The group who abandoned antipsychotic treatment included relatively more individuals categorized as black. It should be noted that all groups had over 25% listed as unknown. Patients who switched antipsychotic medications had a significantly higher mean number of comorbid conditions versus those continuing (P < 0.001) and versus those abandoning (P = 0.001) index medications. Previous psychiatric ER visits were significantly more common among patients who abandoned antipsychotics compared to those who continued (P < 0.001) and those who switched (P = 0.007), respectively and among patients who switched antipsychotics compared to those who continued (P = 0.020). Similar to the prior psychiatric ER visit findings, those who abandoned antipsychotics experienced higher rates of previous psychiatric hospitalizations compared to those who continued (P = 0.005) and those who switched (P = 0.015), respectively.
Table 2 Patient characteristics by outcome categories
Aggregate treatment outcome comparisons
As shown in , significantly higher proportions of patients who switched antipsychotic medications were admitted to any hospital (10.6% vs 7.4%; P < 0.05 vs those continuing), including medical admissions (8.1% vs 5.0%; P < 0.05) but not psychiatric admissions.
Individuals who switched antipsychotics were also significantly more likely to use a range of outpatient health care services, with the pattern for those who abandoned differing by whether it was ER-related or not (). Patients who switched and those who abandoned antipsychotics used the ER significantly more frequently than those who continued, regardless of whether the ER visit was categorized as psychiatric or medical. With the exception of outpatient psychiatric hospital visits, where no significant differences were observed, the general pattern for the remaining outpatient service categories was switching patients having the highest rate of service use, followed by those who continued and those who abandoned having the lowest rates of service use. All of these comparisons were statistically significant with the exception of continued versus abandoned in the medical outpatient hospitalization and switched versus continued in the psychiatric outpatient physician categories.
Treatment outcome comparisons by medication start type
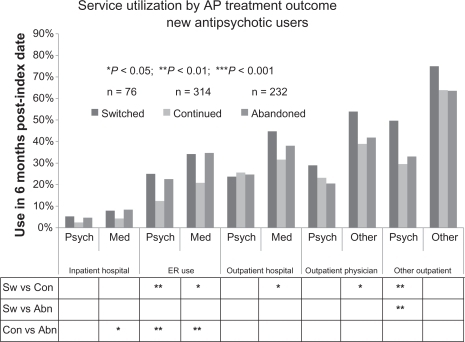
New antipsychotic users
As shown in , patients who switched antipsychotic medications were in general more likely to utilize health care resources than their counterparts who continued on their index medications. Both ER-use categories, medical outpatient hospital visits, other outpatient physician, and other outpatient visits were all significant. The only switched versus abandoned comparison which reached significance was for other outpatient psychiatric visits which were higher among those who switched. Patients who abandoned were significantly more likely to use the ER (for both psychiatric and medical types of visits) and were also significantly more likely to experience a medical inpatient hospitalization than were those who continued.
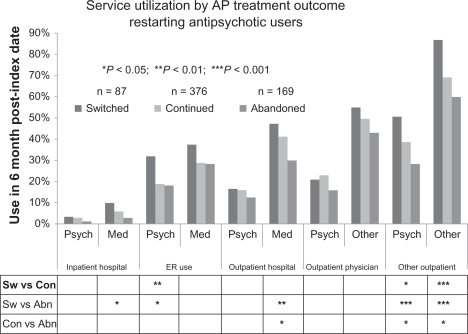
Restarting antipsychotic users
As shown in , restarting patients who switched medications experienced significantly higher rates of psychiatric ER use and both psychiatric and other outpatient service use compared to those who continued. These 3 service categories were also significantly higher in patients who switched compared to the patients who abandoned, as were medical inpatient hospitalization and medical outpatient hospital services. Compared to those who abandoned, patients who continued their antipsychotics utilized significantly higher rates of medical outpatient hospital services and both psychiatric and other outpatient services.
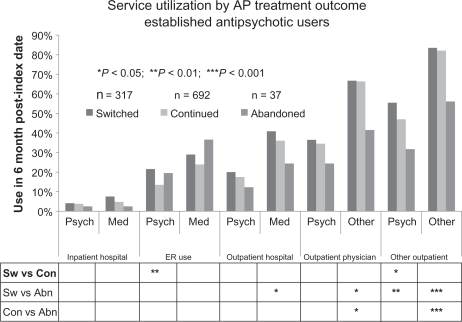
Established antipsychotic users
As shown in , established patients who switched medications experienced higher rates of psychiatric ER use and psychiatric other outpatient services compared to those who continued. Compared to those who abandoned, patients who switched also experienced higher rates of medical outpatient services, other outpatient physician services and both other and psychiatric other outpatient services. Patients who continued their antipsychotics utilized more medical outpatient physician and medical other outpatient services compared to those who abandoned. Abandoned patients utilized comparable rates of ER services to those who switched; however, there was a small sample size in this cohort.
Discussion
In this retrospective administrative claims database analysis, patients who switched from their index medication to a different antipsychotic medication within 6 months were significantly more likely to use a number of health care resources, including making ER visits and being hospitalized, compared with their counterparts who continued on their index antipsychotic medications. It is unclear whether the greater resource use observed among individuals who switched medications is a downstream consequence of the switch, a function of baseline differences in severity, or some combination of the two. The greater number of comorbid conditions and higher rates of prior psychiatric ER use among switchers compared to those who continue, suggests that baseline severity is an important contributor to the higher use of services in the outcome period. Rapid changes in antipsychotic treatment may result from a poor match between patient and medication (ie, inadequate response or intolerability of side effects), erratic clinical decision making, erratic patient behavior, poorly integrated accessible systems of care, difficulties with access to care, and/or the cost of care (including medication copayments).
Patients who switched antipsychotic medications were more likely to use a number of health care services, including hospitalization in particular. Some general medical service utilization could be related to management of medication side effects. It is not clear why switching antipsychotic medications was associated with more frequent hospitalization for nonpsychiatric conditions. However, these findings are broadly consistent with higher rates of acute relapses into active psychosis requiring intensive or emergent care in patients who discontinue treatment. Such patients may experience substantial medical complications or physical injury resulting from acute psychotic relapses with attendant deficits in judgment, including suboptimal self-care of medical conditions; dangerous behavioral responses to delusions; agitation; violence; being victimized; and/or making suicide attempts.Citation10,Citation11 The distinction between psychiatric and medical service use is somewhat artificial and subject to the accuracy with which the reason(s) for the visit is coded.
Similar to patients who switched, those who abandoned their index antipsychotic also utilized more ER services than those who continued. For the majority of other services, however, abandoned patients utilized fewer resources than both those who continued and those who switched. One possible explanation for this finding is that patients who abandon their medication may be poorly engaged in proactive psychiatric care.
Although smaller sample sizes in some of the cohorts limited the ability to draw definitive conclusions, it is worthwhile to examine differences in resource utilization patterns among the new, restarting, and established patient cohorts. ER Use: The new and established cohorts had very similar patterns of ER use. For both psychiatric and medical ER visits, those who switched and those who abandoned their index antipsychotic each used the ER more frequently than those who continued. Among restarting users, however, those who switched antipsychotics used the ER more frequently than both other groups.
Non-ER outpatient services
Among established users, those who switched used outpatient services at least as frequently as those who continued and generally more frequently than those who abandoned. Among restarting antipsychotic users, however, switchers tended to use services most frequently, followed by those who continue and finally those who abandon. Among new antipsychotic users, those who switched used outpatient services with the greatest frequency in many categories. Unlike the restarting and established cohorts, however, service use for the abandoned group was often equivalent to that of the cohort who continued. Event rates <10% for inpatient hospitalization made it difficult to discern a clear pattern.
Compared with their counterparts who continued on their index medications, patients who switched had significantly more comorbid conditions at baseline and were significantly more likely to have previously visited the ER. Consequently, it is unclear whether the higher rate of ER use among switchers during the follow-up period represented a continuation of the previous trend, a consequence of the medication switch, or some combination of these factors. Regardless of the reason, the increased use of these medical services warrants close inspection, and future research should seek to characterize the proportion of ER service use specifically attributable to switching.
Future studies are also needed to further evaluate the actual costs and cost-effectiveness of switching antipsychotic treatments. Perhaps not surprisingly, one recent post-hoc analysis of an open-label study concluded that switching from one atypical antipsychotic to another because of inadequate efficacy or tolerability resulted in quality-of-life benefits (increased health utilities) and was projected to be cost effective.Citation14 In contrast to other pharmacoeconomic analyses of schizophrenia treatments,Citation15–Citation18 the present study estimated health care costs indirectly via rates of health care resource utilization and did not capture health and other care not covered by Medicaid. These include medications during inpatient treatment, as well as privately paid treatment, charity care, family care, and shelter care. As noted in the Methods, this study did not distinguish between individuals using a particular service once and those with multiple visits or prolonged inpatient stays. Such an examination is necessary to assess the full economic impact of switching antipsychotics. The present study also compared health care utilization among patients switching (vs those continuing or abandoning) any antipsychotic medication; however, there may be differences in treatment adherence between individual antipsychotic agents.Citation19
Other potential limitations of this study include its: 1) retrospective and exploratory nature; 2) limited follow-up period (6 months); and 3) definition of continued treatment adherence on the basis of prescriptions filled, which are not necessarily accurate barometers of actual medication use. As in other exploratory analyses, data were not adjusted for multiple comparisons. Further, an observational study cannot exclude potential biases resulting from unmeasured and other confounders. One potential confound is an imbalance of established antipsychotic medication users (45.5% of eligible patients); these users had significantly more comorbid conditions than new users or restarters, and patients switching medications also had significantly more comorbidities than those who continued on, or abandoned, their index medications. It is possible that some of these comorbidities are related to medication side effects that may have motivated either the index or the subsequent antipsychotic medication change.
In many administrative claims database analyses such as this one, baseline patient-level data and on-treatment clinical information are limited. For example, in the present analysis, data on race/ethnicity were not available for approximately 25% of participants. On the basis of a limited baseline period of 1 year before the index date and an average patient age of 37 years, it is unlikely that all patients in the “new-user” category were actually completely treatment naïve.
Given limited patient-level data, the data also could not be rigorously analyzed according to the reason for treatment discontinuation (eg, suboptimal efficacy, tolerability), which can influence health care resource utilization. By predefined eligibility criteria, the age at the index date ranged from 18 to 50 years to exclude children, adolescents, and patients with dementia. Thus, our findings may not be generalizable to these patient segments. Our analysis was also based on Medicaid data from a single state (California) and hence may not be representative of the overall Medicaid population with schizophrenia. Our findings are also not necessarily generalizable to the overall US schizophrenia population and may not apply to dual-eligible Medicaid recipients with schizophrenia. In light of these considerations, our results need to be further evaluated in larger, longer-term prospective studies conducted in naturalistic clinical settings and involving more heterogeneous patient populations.
Because our evaluation period was limited to days 91 to 180 after the index date, it is not possible to conclude that all patients defined as having abandoned therapy did not actually obtain other forms of care at a later date. On the other hand, our 90-day reference period to define medication abandonment was longer than has been reported in other analyses. Two previous administrative claims studies reported increased rates of hospitalization with gaps as short as 10 days.Citation20,Citation21 We selected a 90-day refill gap to reduce the number of individuals misclassified as having abandoned antipsychotic treatment. However, one possible consequence of this decision is that some individuals classified as having switched antipsychotics in our study, would have been considered as having a clinically significant gap (ie, abandoning therapy) in other studies. Previous studies have also demonstrated higher hospitalization rates associated with longer medication gaps.Citation20 Therefore, it is possible that differences in service use between those switching antipsychotic medications or continuing their index medications in the present study might have been smaller if our analysis had employed a shorter reference period to define abandonment. To the extent that both medication switching and abandonment represent suboptimal medication treatment outcomes, however, this distinction may be less critical.
Conclusion
Patients who switch antipsychotic treatments experience significantly increased health resource utilization compared with their counterparts remaining on their initial medications. Future studies are needed to confirm these findings and identify potential baseline or on-treatment predictors of favorable treatment responses, in order to minimize adverse human and economic outcomes of switching.
Acknowledgements
This study was supported by Eli Lilly and Company (Indianapolis, IN), which had a role in study design, data acquisition and analysis, and publication of the findings. Assistance in manuscript preparation was provided by Robin D LeWinter, PhD and Stephen W Gutkin of Rete Biomedical Communications Corp. (Wyckoff, NJ), with support from the study sponsor.
Disclosure
Drs Phillips and Ball are employees of and minor shareholders in the study sponsor. Dr Noordsy has served as a consultant or speaker and/or has received research funding from AstraZeneca, Eli Lilly, Janssen, Merck, and Pfizer. Mr Linde-Zwirble has served as a consultant and speaker for Eli Lilly.
References
- KahnRSFleischhackerWWBoterHEffectiveness of antipsychotic drugs in first-episode schizophrenia and schizophreniform disorder: an open randomised clinical trialLancet200837196181085109718374841
- LiebermanJAStroupTSMcEvoyJPEffectiveness of antipsychotic drugs in patients with chronic schizophreniaN Engl J Med2005353121209122316172203
- Liu-SeifertHAdamsDHKinonBJDiscontinuation of treatment of schizophrenic patients is driven by poor symptom response: a pooled post-hoc analysis of four atypical antipsychotic drugsBMC Med200532116375765
- WeidenPJSwitching antipsychotics: an updated review with a focus on quetiapineJ Psychopharmacol200620110411816204323
- AlmondSKnappMFrancoisCToumiMBrughaTRelapse in schizophrenia: costs, clinical outcomes and quality of lifeBr J Psychiatry200418434635115056580
- LeslieDLRosenheckRAFrom conventional to atypical antipsychotics and back: dynamic processes in the diffusion of new medicationsAm J Psychiatry200215991534154012202274
- StroupTSLiebermanJAMcEvoyJPEffectiveness of olanzapine, quetiapine, risperidone, and ziprasidone in patients with chronic schizophrenia following discontinuation of a previous atypical antipsychoticAm J Psychiatry2006163461162216585435
- WeidenPJOlfsonMCost of relapse in schizophreniaSchizophr Bull19952134194297481573
- HensleyPLNurnbergHGFormulary restriction of selective serotonin reuptake inhibitors for depression: potential pitfallsPharmacoeconomics2001191097398211735668
- HeiläHIsometsäETHenrikssonMMHeikkinenMEMarttunenMJLönnqvistJKSuicide victims with schizophrenia in different treatment phases and adequacy of antipsychotic medicationJ Clin Psychiatry199960320020810192600
- LaderMWhat is relapse in schizophrenia?Int Clin Psychopharmacol19959Suppl 5597622834
- Fiscal Year 2001 National MSIS Tables (2004). [cited 2009 April 27] Available from: http://www.cms.hhs.gov/MedicaidDataSourcesGenInfo/02_MSISData.asp
- KronickRGilmerTDreyfusTImproving health-based payment for Medicaid beneficiaries: CDPSHealth Care Financ Rev2000213296411481767
- JärbrinkKKreifNBenedictAQuality of life and drug costs associated with switching antipsychotic medication to once-daily extended release quetiapine fumarate in patients with schizophreniaCurr Med Res Opin200925370971619196221
- GibsonPJDamlerRJacksonEAThe impact of olanzapine, risperidone, or haloperidol on the cost of schizophrenia care in a Medicaid populationValue Health200471223514720128
- GilmerTPDolderCRLacroJPAdherence to treatment with antip-sychotic medication and health care costs among Medicaid beneficiaries with schizophreniaAm J Psychiatry2004161469269915056516
- KnappMKingDPugnerKNon-adherence to antipsychotic medication regimens: associations with resource use and costsBr J Psychiatry200418450951615172945
- SvarstadBLShiremanTISweeneyJKUsing drug claims data to assess the relationship of medication adherence with hospitalization and costsPsychiatr Serv200152680581111376229
- YuAPBen-HamadiRBirnbaumHGComparing the treatment patterns of patients with schizophrenia treated with olanzapine and quetiapine in the Pennsylvania Medicaid populationCurr Med Res Opin200925375576419199435
- WeidenPJKozmaCGroggALocklearJPartial compliance and risk of rehospitalization among California Medicaid patients with schizophreniaPsychiatr Serv200455888689115292538
- LawMRSoumeraiSBRoss-DegnanDAdamsASA longitudinal study of medication nonadherence and hospitalization risk in schizophreniaJ Clin Psychiatry2008691475318312037