Abstract
Background and aim
Antiviral therapy with peg-interferon and ribavirin induces sustained virus eradication in 40%–80% of patients with chronic hepatitis C virus (HCV). We investigated patient views on their involvement in therapeutic decision making and on the desirability of disease and treatment-related outcomes.
Methods
The control preferences and visual analog scales were administered in a pencil and paper format to a series of 45 patients in order to assess their decisional role, preferences for scenarios of HCV disease and antiviral treatment, and estimates of success required to recommend treatment.
Results
The preferred decisional role of patients was passive in 26 (58%), collaborative in 12 (27%) and active in 7 (15%). Median preference scores ranged from 0.30 to 0.90 for scenarios of disease, from 0.05 to 0.80 for side effects and from 25% to 100% for estimates of benefit to recommend treatment.
Conclusions
Our patients prefer to defer to the doctor the final decision in starting therapy in a context of shared decision making. Reported preferences for HCV scenarios are in the range discussed in the literature. The wide variability in the values attributed to side effects by patients with chronic hepatitis C as well as in expected probabilities of successful treatment suggests a need for decision analysis tailored to the individual patient.
Introduction
Hepatitis C virus (HCV) infection affects 170 million people worldwide (four million in USA and about five million in western Europe).Citation1,Citation2 Although the majority of those with chronic hepatitis C infection are not going to develop complications, 15%–40% may develop cirrhosis, liver failure, or hepatocellular carcinoma (HCC).Citation3 Chronic hepatitis C is generally asymptomatic but has been associated with reduced health-related quality of life in the early stages.Citation4 Standard therapy is represented by combined use of pegylated interferon and ribavirin for 3–12 months. Such a regimen benefits 40%–80% of patients, depending on HCV genotype,Citation5 and has been shown to be cost-effective from a societal perspective.Citation6
Perception of health by patients with HCV infection or harm from antiviral therapy strongly depends on the information given during the medical examination. It has been shown that the patient’s treatment decisions are influenced by multiple factors besides the risks and benefits of antiviral therapy or the physician’s recommendations. Social issues, some heuristics, particular conceptualizations of the illness, and considering therapy as a protected value are all factors which determine the patient’s acceptation or refusal of therapy.Citation7
The patient’s perspective is becoming more important in health care policy decisions worldwide. It is also becoming more and more common for patients to take an active role when medical decisions have to be made.Citation8 Research on cancer suggests that role preferences vary considerably and that whilst most patients prefer a collaborative role, a significant minority prefer a passive or active role.Citation9 To our knowledge no information exists regarding the common decision-making roles of patients with chronic hepatitis C in approaching a decision about treatment.
It is also well known that each individual patient provides different information about his/her own health state or disabilities, thus disclosing different preferences in drug therapy decisions with uncertain outcomes.Citation10,Citation11 Utility measurement is a method of determining an individual’s preference for a certain outcome represented by a quantitative score (utility). A systematic review of the available literature on health-state utilities for liver disease has been very recently published, producing estimates for major states of hepatitis C such as moderate disease, compensated cirrhosis, decompensated cirrhosis, and post-liver transplant.Citation12
Both the desired/perceived decision-making role and the patient’s views on desirability of disease and treatment-related outcomes are factors influencing the decision to start therapy and may be relevant for a perspective of shared decision making in chronic hepatitis C as in other clinical settings. To gain insight into these issues, we planned a pilot study to administer to a consecutive series of patients a questionnaire evaluating in a simple way their health status, the role they feel to play in decision making about antiviral therapy, and their preferences for some health scenarios related to chronic HCV and its treatment.
Materials and methods
The research protocol was approved by the local Ethical Committee. Participation in our study was proposed to a consecutive series of outpatients with biopsy proven chronic hepatitis C eligible for an Italian multicenter observational outcome study of pegylated interferon (alfa-2a or alfa-2b) and ribavirin.Citation13
Eligibility criteria were: age 18–65 years; serum alanine aminotransferase ALT above the upper normal limit for at least six months; anti-HCV sero-positivity and detectable HCV viremia. Patients were treatment-naïve or previous relapsers or nonresponders and had clinical findings and laboratory parameters indicative of compensated liver disease. None had evidence of an ongoing cause of liver disease other than HCV.
Forty-five patients agreed to participate and provided written informed consent before entry into the study. A questionnaire was administered during the first visit after the diagnostic work-up, before starting treatment. In our clinical practice, it is during this visit that harm and benefit of antiviral therapy are thoroughly discussed with the patient in order to get informed consent to treatment. We formalized this approach and surveyed patients, using a pencil-and-paper format, by a questionnaire that consisted of five parts including:
Demographic data consisting of age, gender, level of education, employment and marital status;
A simple assessment of health status;
An assessment of decision-making role through the choice of one among five statements, according to the control preferences scaleCitation14 (see );
An evaluation of patient’s preferences (utilities) for six health scenarios with HCV, according to Cotler and colleagues.Citation15 Utilities were assessed by asking to each patient to indicate a judgment of relative desirability of each scenario by placing a mark on a visual analog scale (VAS) ranging from 0 (death) to 1 (health without hepatitis C). Scenarios described four possible disease outcomes (chronic hepatitis or cirrhosis without and with symptoms) and two treatment outcomes (adverse events, sustained response) that would be part of any discussion on benefit and harm of antiviral therapy for chronic hepatitis C. The study instrument published by Cotler and colleaguesCitation15 was translated in Italian and slightly modified by excluding the health state 3 “hepatitis C with moderate symptoms, no cirrhosis”, and by including a scenario representing sustained response (see for descriptions).
Patient’s judgment of what threshold of probability of treatment success they would consider minimally acceptable to start drug treatment. This judgment was indicated by placing a mark on a VAS representing probabilities of achieving sustained viral eradication ranging from 0% to 100%.
The content of the descriptions and response scales of the study instrument have been tested for clarity, comprehension, and relevance in physicians and patients from the United States.Citation15
All analyses were carried out using StatsDirect statistical software (version 2.6.1, 19.1.2007; StatsDirect, Cheshire, UK) and STATA software (v. 8.0; Stata Corporation, College Station, TX, USA). Box plots were used to describe patient’s preference values (utilities).
Results
Patient demographic data and disease characteristics are summarized in . The majority of patients were naïve, infected with genotype 1, and highly viremic. Cirrhosis was present at histology in 14 patients (31%). Almost 70% of patients had a high school educational level and a full employment status. Accordingly, all patients completed the first three parts of the questionnaire. However, five patients (11%) refused to complete the assessment of utilities of clinical scenarios because of “tiredness and confusion” and four (9%) were excluded because of illogical assessment (ie, value for cirrhosis higher than value for asymptomatic chronic hepatitis).
Table 1 Baseline characteristics of 45 enrolled patients
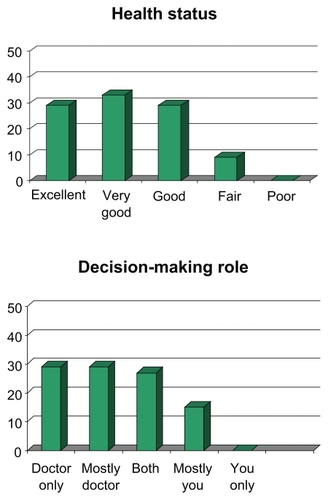
Assessment of health status was good to excellent in 90% of patients (). Only a minority of patients (15%) preferred an active decisional role, that is they favored a personal decision about therapy fully independent from the doctor’s opinion, and almost one third agreed for a shared decision (collaborative role). On the other hand, almost 60% of patients stated that the decision to start therapy is a matter of judgment for the health professional.
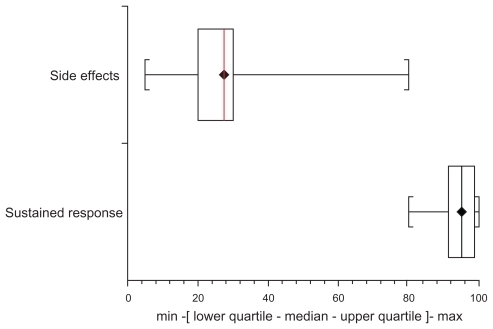
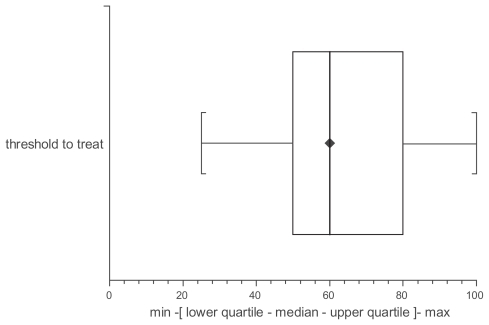
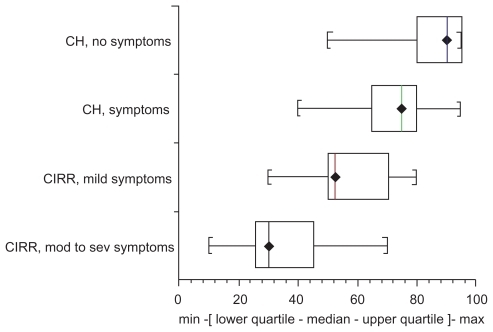
The descriptive statistics of preference values obtained from 36 patients is reported in and . As expected, median values decreased consistently between asymptomatic and symptomatic chronic hepatitis and cirrhosis. The distribution of median utility values, reported within the box plots, showed declining patient’s estimates from the status scenario 1 (0.90) to the status scenario 4 (0.30). In other words patients assigned decrements of quality of life from 10% in asymptomatic chronic hepatitis to 70% in symptomatic cirrhosis. Looking at quartiles and range of estimates for each scenario, a large variability is evident in particularly for scenario describing side effects of treatment (range 0.05 to 0.80). The probability of treatment success that the patient considered to recommend treatment that showed wide estimates ranging from 25% to 100% ().
Figure 2 Box plots of preference values for HCV disease outcomes assessed by visual analog score.
Discussion
Current health care policy advocates patient participation in treatment decision making. In this pilot study we explored the preferred level of involvement in treatment decisions of a small series of patients from Italy with chronic hepatitis C, and used utility-based methods to measure how they valued the health states or disabilities that result from such disease and its treatment. Chronic hepatitis C is a long-term condition in which self-management and participation in treatment decision making must be encouraged. Because the communication skills of professionals are central to facilitating patient participation we used a simple approach by selecting well known user-friendly instruments. We underline that many respondents in this study identified communication as an area requiring improvement, and many would have liked to be more involved in treatment decision making.
Our findings confirm the results of previous studiesCitation8,Citation9,Citation16,Citation17 showing that respondents had identifiable preferences, from active through to passive, regarding their level of participation in treatment decision making. In general, patients wish to be more involved in decisions regarding a minor illness more than a major illness,Citation18 and women tend to desire more involvement than do men in clinical decisions.Citation19 In our study, most patients felt they had little or no role in treatment decisions. Near 60% of them most preferred one of the passive decisional roles from the control preference scale. However, the most passive option was least preferred by more than half of respondents and almost 30% of respondents chose the D option which involves some, if limited, patient involvement, rather than the E option where the patient entirely defers decision making to health professionals. Thus, most respondents preferred some input into decision making. Typically, this extended to individuals feeling included in the decision and having their views respected.
Table 2 Assessment of decision-making role by CPS
Overall, while most patients were happy to defer overall control of treatment decision making to doctors, our data supports the notion of partnership. Our results are close with those of a study evaluating patients with hemato-oncological diseases showing that 60% among 117 interviewed patients desired more a passive than an active role.Citation20 Moreover, in a telephone survey of elderly patients with chronic heart failure 21% of patients preferred an active role versus 31% favoring a collaborative role and 48% a passive role in decision making.Citation21
According to a previous studyCitation15 we used utility analysis to evaluate patient’s perceptions of hepatitis C-related health states and patient’s threshold to recommend treatment. Although the rating scale method does not have its roots in expected utility theory, ie, it is not strictly utility, we believe it is similar to and has measurement advantages over true utilities.Citation14 We found that the majority of patients understood descriptions of health states and were able to provide an utility assessment of the scenarios using a VAS. The validity of the health state construct was supported by the significant decline of utilities assigned with increasing health state severity (from chronic hepatitis to cirrhosis). Although derived from a small sample our estimates are similar to those reported in previous studies which have directly assessed utilities from patients by using the rating scale method as well as other methods ().
Table 3 Patient’s utilities of health states with HCV by rating scale method
Potential factors causing variability of utility estimates could be due to both the tool used (VAS generates the lowest estimates of all the methods, with standard gamble and time trade-off having much higher estimates), the type of respondent (patients, nondiseased subjects, health professionals), and geographical and cultural differences. We recruited individuals from a tertiary care setting representing a population of European HCV-infected patients with no known risk factors eligible for antiviral treatment. The results derived from this convenience sample might be different from those that could have been derived should have the sample been randomly drawn from all eligible participants in the general population with chronic HCV infection.
It is of interest that the median rating for life with side effects of antiviral therapy was 0.25, suggesting a perceived 75% reduction from good health during time on therapy. Thus, patients viewed side effects unfavorably at least in the proposed scenario. Moreover, the large range of patient ratings is striking and indicate that patient views about the impact of side effects on health status varies substantially. We don’t know the difference in disutility of each patient among different adverse events, ie, flu-like versus depression or alopecia, or the value patients could assign to possible life-threatening adverse event such as a severe infection. This information is lacking in the literature but it is very important for the generation of recommendations for treatment.Citation25 As the ratings of adverse events overlap with the ratings of future disease scenarios (without or with symptoms) and as patients’ estimates of benefit in recommended treatment are also largely variable, it seems that decision analysis could be of help in decision making.
The strength of our study include the novelty of assessing hepatitis C patient views on their role in therapeutic decision making by means of established scales. In fact, to our knowledge, this was not assessed previously in a population of liver patients. However, our study suffers from some methodological limitations such an unique geographical location and a limited sample size, so that characteristics of small subgroups could not be investigated. Evidence of the association of factors such age, gender, level of education, marital status, socioeconomic status, and health status with preferences for involvement in treatment decision making or with health utilities of patients with chronic hepatitis C remain inconclusive and should be assessed in future studies.
In conclusion, our patients prefer to defer to the doctor the final decision in starting therapy in a context of shared decision making. Preferences for HCV scenarios are in the range reported in the literature. The wide variability in the values attributed by patients with chronic hepatitis C to both scenarios of health with HCV and health with antiviral treatment as well as in expected probabilities of cure suggests a need for decision analysis tailored to the individual patient. Further research is needed to identify predictors of preferences for active or passive patient roles and further utility analysis is needed to generate data on the values patients assign to single side effects from antiviral therapy.
Acknowledgments
The author thanks Giuseppina Zummo for help with the English version of the paper and Scott J Cotler for the instrument to assess utilities.
Disclosures
The authors report no conflicts of interest in this work.
References
- World Health OrganizationHepatitis C Fact Sheet Available from: http://www.who.int/immunization/topics/hepatitis/en/index.htmlAccessed on October 10, 2009
- TrepoCPradatPHepatitis C virus infection in Western EuropeJ Hepatol199931808310622565
- SeeffLBNatural history of chronic hepatitis CHepatology200236S354612407575
- YounossiZKallmanJKincaidJThe effects of HCV infection and management on health-related quality of lifeHepatology20074580681617326207
- FriedMWShiffmanMLReddyKRPeginterferon alfa-2a plus ribavirin for chronic hepatitis CN Engl J Med200234797598212324553
- RajendraAWongJBEconomics of chronic hepatitis B and hepatitis CJ Hepatol20074760861717697724
- FrankaelLLMcGrawSWongcharatraweeSWhat do patients consider when making decisions about chronic hepatitis C?Am J Med20051181387139116378783
- DeberRBKraetschmerNIrvineJWhat role do patients wish to play in treatment decision making?Arch Intern Med199615613141414208678709
- HubbardGKiddLDonaghyEPreferences for involvement in treatment decision making of patients with cancer: a review of the literatureEur J Oncol Nurs20081229931818486552
- TorranceGWUtility approach to measuring health-related quality of lifeJ Chronic Dis1987405936003298297
- ErakerSASoxHCAssessment of patient’s preferences for therapeutic outcomesMed Decis Making1981129397052402
- McLermonDJDillonJDonnanPTHealth-state utilities in liver disease. A systematic reviewMed Decis Making20082858259218424560
- CraxiAPiccininoFAlbertiAPredictors of SVR in naive HCV1 patients in real life practice: the PROBEJ Hepatol200848Suppl 2S291
- DegnerLFSloanJAVankateshPThe Control Preferences ScaleCan J Nurs Res19972921439505581
- CotlerSJPatilRMcNuttRAPatient’s values for health states associated with hepatitis C and physicians’ estimates of those valuesAm J Gastroenterol2001962730273611569703
- CaressALBeaverKLukerKInvolvement in treatment decisions: what do adults with asthma want and what do they get? Result of a cross-sectional surveyThorax20056019920515741435
- ChamotECharvetAPernegerTVWomen’s preferences for doctor’s involvement in decisions about mammographyMed Decis Making20042437938515271276
- EndeJLewisKAshAMeasuring patients’ desire for autonomy: decision making and information-seeking preferences among medical patientsJ Gen Intern Med1989423302644407
- AroraNKMcHorneyCAPatient preferences for medical decision making: who really wants to participateMed Care20003833534110718358
- ErnstJBrählerEAldaoudADesired and perceived participation in medical decision-making in patients with haemato-oncological diseasesLeuk Res2009720 [Epub ahead of press]
- RodriguezKLAppeltCJSwitzerGEVeterans’ decision-making preferences and perceived involvement in care for chronic heart failureHeart Lung20083744044818992627
- FrobergDGKaneRLMethodology for measuring health-state preferences II: Scaling methodsJ Clin Epidemiol1989424594712732774
- ChongCAGulamHusseinAHeathcoteJEHealth state utilities and quality of life in hepatitis C patientsAm J Gastroenterol20039863063812650799
- ShermanKEShermanSNChenierTHealth values of patients with chronic hepatitis C infectionArch Intern Med20041642377238215557419
- SinclairJCCookRJPaukerSGWhen should an effective treatment be used? Derivation of the threshold number needed to treat and the minimum rate for treatmentJ Clin Epidemiol20015425326211223323
Appendix
Appendix 1 Decision-making role by control preferences scale
Appendix 2 Description of six scenarios of health with HCV (Cotler, modified)