Abstract
Introduction:
Prevention of medication errors is a priority for health services worldwide. Pharmacists routinely screen prescriptions for potential problems, including prescribing errors. This study describes prescribing problems reported by community pharmacists and discusses them from an error prevention perspective.
Method
For one month, nine community pharmacists documented prescribing problems, interventions made, and the proximal causes of the problems. The results were presented to local GPs and pharmacists at a meeting and feedback was invited.
Results
For 32 403 items dispensed, pharmacists reported 196 prescribing problems (0.6%). The reporting rates ranged from 0.2%–1.9% between pharmacists and were inversely correlated to dispensing volume. Prescriptions containing incomplete or incorrect information accounted for two-thirds of the problems. Lack of information on the prescriptions and transcribing/typing errors were the most frequently cited proximal causes. A few pitfalls of computerized prescribing were observed.
Conclusion
Although rates of prescribing problems reported were relatively low, community pharmacists and patients remain important safeguards. This study identified potential causes of prescribing errors, and illustrated areas which could be improved in the design of computerized prescribing systems, and the communication and sharing of information between GPs and pharmacists.
Introduction
Prevention of medication errors has been recognized as a priority in health care systems worldwide, as exemplified in the publication of the Institute of Medicine, USA's report To err is human (CitationKohn et al 1999) and the document An organisation with a memory (CitationDepartment of Health 2000) by the Department of Health, UK. Multiple defensive mechanisms are required in a complicated healthcare system to achieve this goal (CitationReason 2000). Prevention of errors at the prescribing stage is one of the important steps towards reducing medication errors. Although prescribing errors have been systematically studied in hospitals (CitationLeape et al 1995; CitationLesar et al 1997; CitationDean et al 2002), similar information derived from primary care settings is scant.
Community pharmacists routinely screen prescriptions for potential problems, including prescribing errors, before the drugs are dispensed. They are in an ideal position to identify, record, rectify, and prevent prescribing errors.
Prescribing problems have been classified as errors of omission and errors of commission, which require reactive and proactive interventions, respectively, by pharmacists to rectify them (CitationRupp 1991). This classification, based on the factual presentation of the prescribing problems, is useful for differentiating problems which are overt and less likely to cause harm (errors of omission) from those which are not always obvious and are potentially more dangerous. However, not all prescribing problems arise from errors, and this warrants further clarification when prevention of prescribing errors is to be considered.
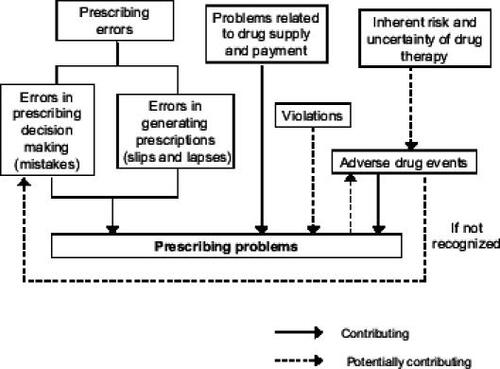
As illustrated in , some prescribing problems are caused by errors, which can occur at different stages: those occurring at decision-making are termed mistakes, while those happening during prescription-generation can be caused by either slips (doing something different from the initial intention; for example, writing methotrexate 7.5 mg daily instead of weekly), or lapses (forgetting to do something as intended such as signing the prescription). These errors are theoretically preventable and are the focus of error prevention strategies. Other prescribing problems can arise from the inherent risk of drug therapy or the process associated with the supply and reimbursement of the medications. While these problems do not represent errors in the first instance, they can be regarded as errors if they are not recognized and are repeated in subsequent prescriptions. Sometimes, problems may arise from prescribers' intentional violation of guidelines or rules (for example, prescribing propranolol in response to a strong request by a patient despite knowing he or she has a history of asthma).
Although several studies have documented community pharmacists' interventions on prescribing problems (CitationJones 1978; CitationRupp et al 1992; CitationFielding et al 1993–1994; CitationGreene 1995a, Citation1995b; CitationClaesson et al 1995; CitationCaleo et al 1996; CitationHawksworth et al 1999; CitationShah et al 2001; Citationvan Mil et al 2001; CitationWestein et al 2001; CitationQuinlan et al 2002; CitationBenrimoj et al 2003a, Citation2003b), most of them have focused on the recognition, documentation, and resolution of prescribing problems and have not addressed these problems from a preventive perspective.
Based on the framework shown in and discussed above, the objectives of this paper are to describe prescribing problems reported by community pharmacists, and to discuss these problems from an error-prevention perspective.
Method
Definition of prescribing problems
Prescribing problems in this study were defined as any problems identified in the process of dispensing that might (1) interfere with the dispensing of prescriptions, such as incomplete prescriptions and prescriptions with incorrect information; or (2) be potentially harmful to the patients, such as potentially hazardous drug–drug interactions, inappropriate doses or directions, contraindications, adverse drug reactions, allergy to drugs, and drug duplications. As prescribing problems cover a wide range of unsatisfactory situations varying in their importance and potential impact, the use of this definition allowed pharmacists to record only those problems that have impact on medication safety or on the efficiency of dispensing.
Study participation
All eleven community pharmacies in an area of Nottingham, England were invited to participate in this study. One pharmacy declined due to a heavy workload and lack of interest, and another was unable to participate because there was no full-time pharmacist. The remaining nine pharmacies agreed to participate. These participating pharmacies included two independent pharmacies, three local multiples, three regional multiples (with 10–50 branches), and a large nationwide chain pharmacy.
Data collection
A data collection form was designed and distributed to all participating pharmacies in January 2000. It was piloted in one participating pharmacy for one month and in the other pharmacies for one week. This data collection form was revised according to the feedback from the pharmacists and the final data collection form used in the study is available from the authors.
Formal data collection started in April 2000 and finished at the end of January 2001. Each of the participating pharmacies was allocated one month during this period to collect data. It was envisaged that most pharmacies would be extremely busy in December, and so none of the Prescribing errors reported by community pharmacists pharmacies were asked to collect data during this month.
Data collected in this study included:
The dates when problematic prescriptions were presented to the pharmacists
Age and gender of the patients
Brief descriptions of the problems
Interventions made by the pharmacists
Estimated time the pharmacists spent dealing with these problems.
The pharmacists were asked to code the origin of the prescription (local practices, other practices, dentists, or hospital), type of problem, intervention made, and proximal causes of the problems according to the coding list provided with the data collection form. The proximal causes were adapted from CitationLeape et al (1995) and were defined as “the apparent reasons for the prescribing problems; they are broad categories that are useful for focusing further inquiry and may not be true causes”. Prescribing problems were recorded whether the prescriptions were eventually dispensed or not.
Data validation and coding
One of the investigators (Yen-Fu Chen) visited the participating pharmacies at least once a week during their data collection month to collect prescribing problems that were being recorded, to obtain incomplete information whenever possible, and to clarify any queries regarding data collection and coding. As the majority of the reported problems turned out to be in the “incomplete/incorrect/ illegible prescriptions/product unavailable” category, these problems were further classified by the investigator after data collection.
As part of data validation, a sample of prescriptions dispensed by each pharmacy during the data collection month was screened for potentially hazardous drug combinations by the investigator using a standard drug interaction computer program. This also allowed the collection of additional information on potentially hazardous drug combinations which has been described elsewhere (CitationChen et al 2002).
Ethical approval and confidentiality of the data
Ethical approval for this study was obtained from the local research ethics committee. No identifiable information (such as names and addresses) on prescriptions was recorded, and information on potentially hazardous drug combinations was fed back to the participating pharmacists.
Data analysis
Descriptive statistics were computed by the Statistical Package for the Social Sciences (Release 9.0) software. Pearson's correlation coefficient was used to examine the relationship between dispensing volume and prescribing problems reported.
Feedback from local pharmacists and general practitioners
The results of the study were presented to local GPs and pharmacists at a meeting. Feedback was invited from the participants of the meeting concerning data collection, causes of the prescribing problems, possible preventive measures, and solutions. Relevant comments were used to inform the discussion section of this paper. Since it was not our intention to carry out a qualitative study, no formal qualitative research methods were used during the collection and analysis of the data from the meeting.
Results
Problem reporting rate
Overall, 32 403 items were dispensed by the participating pharmacies during the data collection months. The pharmacists reported 201 prescribing problems, representing a reporting rate of 0.6% (6 prescribing problems reported per 1000 items dispensed). Five of these were ruled to be outside the scope of this study: four of them involved GPs asking for information on medications or their usage before or during prescribing, and one related to dispensed controlled drugs not being collected by the patient. They have therefore been excluded from all subsequent analysis. The 196 remaining prescribing problems related to 194 prescriptions (two had two problems).
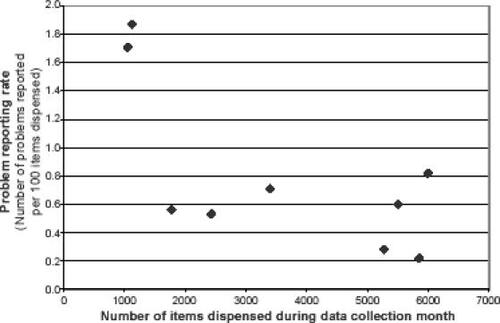
The reporting rate varied substantially between pharmacies, ranging from 0.2%–1.9% (see ). There was a negative correlation between dispensing volume and reporting rate (Pearson's correlation coefficient –0.69, p = 0.041), and the two pharmacies with lowest dispensing volume had highest reporting rate.
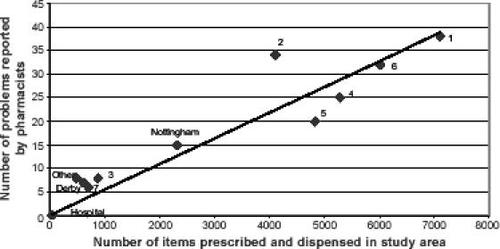
As shown by , the number of prescribing problems reported by the pharmacists for each general practice (or area) correlates well with the number of items dispensed in the study area (Pearson's correlation coefficient 0.94, p < 0.001). Problem rates ranged from 0.4%–1.6% for the practices or areas. Only a small number of prescriptions from hospitals were dispensed and no problem was reported for these prescriptions.
Figure 3 Prescribing volume and number of prescribing problems reported for each general practice or area. Keys: 1–7: local practices; Nottingham: other practices in the Nottingham Health Authority; Derby: practices in the Derbyshire (neighbouring) Health Authority; Other: other health authorities and dental practices; Hospital: local hospitals
Types of prescribing problems
The types of problems and frequency reported by the community pharmacists are summarized in , along with some examples. The majority of prescribing problems arose from prescriptions having incomplete or incorrect information, or the prescribed items being not available. These represent 67% (131/196) of all problems reported. Potentially hazardous drug combinations were reported in 17 cases (9%), followed by inappropriate direction/ instruction in 15 cases (8%). Each of the remaining types of problems accounted for 5% or less of overall problems.
Table 1 Type, frequency, and proximal causes of prescribing problems reported by community pharmacists
Interventions made by pharmacists
The pharmacists obtained additional information from the patients and pharmacy medication records and resolved 21% (41/196) of the problems without any contact with the general practices. More than half of the problems concerning potential drug interactions, adverse drug reactions, inappropriate directions, and missing quantities were dealt with in this way.
In 29% (57/196) of cases, the pharmacists made their own decision to dispense the medication, but the prescription had to be returned to the surgery for alteration. The majority of these involved unsigned prescriptions, prescriptions lacking endorsement by a GP to conform to regulatory/ administrative requirements, and incorrect pack size.
Receptionists were contacted for 17% (33/196) of the prescribing problems and prescribing GPs for a further 26% (50/196). Two-thirds (33/50) of contacts with GPs resulted in changes to prescriptions. Patients were referred back to their GP for 5% (9/196) of the problems.
Overall the participating pharmacists estimated spending an average of 5.7 minutes per problem (minimum 0.2, median 5, maximum 48). This is equivalent to approximately half an hour per week for each pharmacy.
Proximal causes of prescribing problems
The pharmacists were asked to suggest proximal causes for each prescribing problems that they identified. The most frequent two proximal causes for each type of problem are listed in . Lack of information on the prescription was cited most frequently and accounted for 31% (60/196) of all prescribing problems. The missing information involved various parts of a prescription, including signature, strength, quantity, product information (for dressings or devices), and endorsement required for certain drugs such as SLS (Selected List Scheme) for sildenafil. In most cases, it was not possible to ascertain the true underlying reason for the omission of information.
Transcribing/typing errors were thought to be associated with 23% (30/196) of the reported problems. They were the major cause suggested for incorrect prescriptions. Examples include inappropriate directions, instructions, or doses, such as “Fucithalmic 2 hourly” instead of twice daily, and “simvastatin 1 o.m.” (in the morning) instead of “1 o.n.” (at night); incorrect strength or dosage form, such as writing “Co-amoxiclav 250/62 tablets” while the correct strength for tablets is 250/125 and for suspension is 250/62; and incorrect quantities, such as “Gaviscon® 1 ml” or “Diastix® 0 strip”. Errors in transcribing messages from hospitals were also observed in this study. In one case, Cacit® tablets were prescribed by a GP when the hospital had requested Didronel PMO® which contains both Cacit® tablets and disodium etidronate tablets. In another case, the transcribing error resulted in an incorrect dosage instruction. The GP prescribed risedronate 30 mg 1/2 tablet, but the pharmacist identified this as inappropriate because the tablet was film coated and should not be split. It turned out that the hospital doctor had intended one tablet 1/2 an hour before food. In another case, a patient needing betamethasone drops was prescribed a beclomethasone nasal spray possibly due to the confusion between drug names. In four cases, the prescription given to the patient had another patient's name on it. In three of those cases the patients had similar names.
Seventeen percent (33/196) of the reported problems related to repeat prescriptions. They include problems of missing requested items and duplications of the same drug. Several repeat prescriptions contained incomplete and incorrect information which may have been carried over from previous prescriptions.
Lack of knowledge of the drug or product has possibly contributed to 15% (29/196) of the prescribing problems. All three cases of inappropriate doses attributable to lack of knowledge of the drug related to medications for children under the age of twelve. Interestingly, only one of them involved an excessive dose whereas the other two involved doses which were too low. In another three cases, it was suspected that some patients were given wrong instructions regarding the technique of using inhalers by a GP.
Poor communication was cited as a possible cause for twenty-five problems (13%). It was mainly associated with inappropriate instructions and incorrect drug items or dosage forms. Poor communication had occurred between different parties at various stages: between patients and practice staff (items on the repeat prescriptions were different from what the patients wanted); between GPs and patients (inconsistency between GPs' oral instructions understood by the patients and the instructions written on the prescriptions, or GPs not being aware of patients' problems in using medications); between hospitals and general practices (hospital letters misread by GPs or practice staff); and between pharmacies and general practices (pharmacist's written message to GP not heeded).
In 26 cases (13%), the pharmacists acted upon prescriptions to highlight potential drug-related problems. No actual errors were presented on these prescriptions. Fourteen out of seventeen potentially hazardous drug combinations and three out of nine potentially inappropriate doses reported by the pharmacists fell into this category.
Discussion
Prescribing problem rate and problem reporting
Pharmacists in this study reported an overall prescribing problem rate of 0.6%. This figure is relatively low compared with the overall rates reported in a number of previous studies (CitationRupp et al 1992; CitationFielding et al 1993–1994; CitationClaesson et al 1995; CitationCaleo et al 1996; CitationShah et al 2001), but is very similar to the result (0.7%) of another study recently done in the UK (CitationQuinlan et al 2002). Several issues need to be addressed when comparisons are made between studies.
Firstly, the definition of prescribing problems and errors differs between studies. In particular, problems relating to errors of omission (such as indication not specified; CitationClaesson et al 1995) and reimbursement procedures vary substantially. When incomplete prescriptions and other procedural problems are excluded, however, the results between various studies are fairly consistent (approximately 0.4%) (CitationClaesson et al 1995; CitationCaleo et al 1996; CitationHawksworth et al 1999; CitationQuinlan et al 2002). Nevertheless, the potential problem of underreporting warrants further discussion.
There was a nearly ten-fold variation in the problem reporting rates among the participating pharmacies in this study. Differences of this magnitude have been observed in other studies involving multiple pharmacies (CitationRupp et al 1992; CitationGreene 1995a; CitationCaleo et al 1996; CitationHawksworth et al 1999; CitationBenrimoj et al 2003a). The substantial differences between pharmacies are likely to have arisen from a combination of many factors, including pharmacists' experience and perception of prescribing problems, the incentive for problem reporting, dispensing volume and workload in the pharmacy, the degree to which pharmacy computer systems can help with problem identification, true difference in problem rates in different locations, and fluctuation in problem rates due to special local circumstances or simple chance.
A negative correlation between dispensing volume and problem reporting rates (or observed intervention rates) was found in this study and previous studies (CitationRupp et al 1992; CitationHawksworth et al 1999). It is plausible that as their dispensing workload increases, pharmacists may find it more difficult to report problems or make interventions. Nevertheless, it should be noted that the interplay of the factors mentioned above means that other explanations are possible. Also, it should be noted that the correlation found in our study was not particularly strong and no correlation was identified in some other studies (CitationCaleo et al 1996; Citationvan Mil et al 2001).
Omission of prescriber's signature and other information
In this study, the most frequent prescribing problem relating to incomplete prescriptions was lack of a prescriber's signature and there were similar findings in two other recent studies carried out in the UK (CitationShah et al 2001; CitationQuinlan et al 2002). As most prescriptions from British general practices are now computer-generated, signing prescriptions is currently the only step in the prescription-generating process that cannot be performed by a computer. The relative high frequency of missing signatures in relation to other errors of omission in these studies may be seen as indirect evidence indicating the effectiveness of using computers to reduce omission errors. The proposed electronic signatures for prescriptions may further reduce this type of error (CitationAnonymous 2004).
Given the legal responsibility behind the act of signing prescriptions, the significance of the omission of signatures on prescriptions could depend on the underlying causes. If the GP had checked the prescription but forgot to sign it due to memory lapse, the error could be difficult to prevent but nonetheless would not do much harm. If, however, the GP overlooked a prescription when quickly checking through a pile of prescriptions, the error could represent a potential failure in the system which deserves further attention. It was not possible, however, to determine the actual underlying causes for the omission of signatures in this study.
Benefits and pitfalls of computerized prescribing
Computerized prescribing offers substantial benefits such as speed, improved legibility, and automated record keeping. Most of the omission errors mentioned above could be prevented by making changes to computer systems to force prescribers to provide all necessary information when generating prescriptions. Having a single electronic medical record shared by both primary and secondary care may also reduce errors which occur when transcribing information from hospital correspondence to general practice records.
On the other hand, the findings of this study also highlight several potential pitfalls with computerized prescribing. For instance, the use of “drop down menus” means that it is possible to select the wrong drug from an alphabetical list of preparations such as in the case of betamethasone and beclomethasone, or select the wrong patient from a list of similar names (CitationFerner and Coleman 2005). Several errors reported by the pharmacists illustrated the possibility of incorrect or outdated instructions being carried over to repeat prescriptions. These problems are likely to occur for medications requiring initial loading doses or involving regimens in which the doses are gradually built up or stepped down. A further example raised in the group discussion with GPs is the possibility of issuing a prescription with the wrong patient's name – and hence generating an incorrect medication record – if the prescribing doctor forgets to switch computer records between patients. These cases demonstrate some limitations of computerized prescribing in preventing errors and the importance of other measures of error reduction and mitigation.
Sharing of information and communication between GPs and pharmacists
As described earlier, not all prescribing problems arise from errors. Although pharmacists reported seventeen potentially hazardous drug combinations, they contacted prescribers in less than half of the cases and only one prescription was subsequently altered. Virtually all the hazardous drug combinations were associated with either increased risk of toxicity or possible reduction of efficacy and none of them were absolute contraindications, which would indicate an error. These combinations usually require monitoring of treatment and provision of additional advice to patients. Community pharmacists are frequently confronted with difficult situations in which information such as blood test results or patients' medical histories are not available to allow assessment of medication safety. In these cases pharmacists usually have to rely on their experience and information from the patient to make a judgment about whether to contact the prescriber for clarification. There is a strong argument for community pharmacists having better access to relevant patient information, which would allow them to monitor drug therapy while reducing unnecessary contact with prescribers. It is also possible that access to patients' medical history and biochemical data could increase the detection of errors associated with prescribing decisions.
Among the nine reported problems related to inappropriate doses, four of them involved medications for children and in two of these cases the doses were subsequently changed. The pharmacists appeared to maintain high vigilance regarding medications for children. Given the limited clinical information currently available to pharmacists, attempts to differentiate between prescribing errors in dosage and prescribers' intentional use of exceptional doses could be a major challenge. Similar situations occur with potentially hazardous drug combinations and potentially contraindicated medications mentioned earlier. Unnecessary queries to prescribers could delay the dispensing of the medication, undermine patients' confidence, and increase workload for both the prescribers and the pharmacists. However, taking no action without prescribers' assurance could put patients at risk of harm. A suggestion made by local pharmacists and GPs was that GPs add a message to the prescriptions when knowingly prescribing an unusual dose or potentially hazardous drug(s). Pharmacists could then be more confident about the appropriateness of the prescriptions and avoid unnecessary queries.
Error defence by pharmacists and patients
It has been suggested previously that prescribers' decision making processes vary (CitationDenig et al 2002) and important elements of prescribing can sometimes be ignored. In this study, pharmacists elicited patients' past history of adverse drug reactions and drug allergy and the prescribers subsequently changed prescriptions in two cases. This pharmacist “safety net” remains an important mechanism in preventing adverse drug events caused by errors. In other cases, patients discussed potential adverse drug reactions with the pharmacists, who assessed the potential benefit and risk and provided advice to alleviate possible side effects. The importance of patients themselves in detecting errors at the final stage of medication use process cannot be overstressed. Ensuring that patients have sufficient understanding of their medications may also prevent errors when they request repeat prescriptions or when they see a different doctor.
Encouragement of error reporting and sharing of information may help people to learn from previous errors (CitationDepartment of Health 2000). The simple method of data collection adopted in this study and the collaboration of local GPs and pharmacists provides a useful model for the primary care setting.
Conclusion
The incidence of prescribing problems reported by community pharmacists in this study was relatively low compared with previous studies. Most of the prescribing problems reported were attributable to errors in the prescription-generating process. Lack of information on the prescription and transcribing/typing errors were the most frequently cited possible causes.
This study has illustrated the role that community pharmacists have in the detection, rectification, and prevention of prescribing problems. Future problems might be prevented by improving communication and sharing of information between GPs and pharmacists and by making changes to the design of computerized prescribing systems.
Acknowledgments
This study was funded by National Health Services Research & Development Support Funding for Primary Care, UK. We are grateful to the community pharmacists and other staff in the participating pharmacies and local GPs, for their help and co-operation. At the time of data collection and analysis, Yen-Fu Chen and Michael Dewey were affiliated with the Trent Institute for Health Services Research, University of Nottingham, Nottingham, UK. Part of this study was presented as a poster in the British Pharmaceutical Conference, 23–25 September 2002, Manchester, UK.
References
- AnonymousElectronic prescription signatures planPharm J2004273176
- BenrimojSILangfordJHBerryGClinical intervention rates in community pharmacy: a randomised trial of the effect of education and a professional allowanceInt J Pharm Pract2003a117180
- BenrimojSILangfordJHBerryGClinical significance of clinical interventions in community pharmacy: a randomised trial of the effect of education and a professional allowanceInt J Pharm Pract2003b11817
- CaleoSBenrimojSCollinsDClinical evaluation of community pharmacists' interventionsInt J Pharm Pract199642217
- ChenY-FNeilKEAveryAJPrescriptions with potentially hazardous/contraindicated drug combinations presented to community pharmaciesInt J Pharm Pract200210SupplR29
- ClaessonCBBurmanKNilssonJLGPrescription errors detected by Swedish pharmacistsInt J Pharm Pract199531516
- DeanBSchachterMVincentCCauses of prescribing errors in hospital inpatients: a prospective studyLancet20023591373811978334
- DenigPWittemanCLMSchoutenHWScope and nature of prescribing decisions made by general practitionersQual Saf Health Care2002111374312448805
- Department of HealthAn organisation with a memory2000LondonThe Stationery Office
- FernerREColemanJAnticipating, preventing and investigating medication errorsClin Med20055121515745190
- FieldingDHillDStrattonTValue added: solving prescription problemsCan Pharm J1993–19941265058
- GreeneRSurvey of prescription anomalies in community pharmacies: (1) prescription monitoringPharm J1995a25447681
- GreeneRSurvey of prescription anomalies in community pharmacies: (2) interventions and outcomesPharm J1995b2548735
- HawksworthGMCorlettAJWrightDJClinical pharmacy interventions by community pharmacists during the dispensing processBr J Clin Pharm199947695700
- JonesDRErrors on doctors' prescriptionsBr J Gen Pract1978285435
- KohnLTCorriganJMDonaldsonMSTo err is human – building a safer health system1999WashingtonNatl Acad Pr
- LeapeLLBatesDWCullenDJSystems analysis of adverse drug eventsJAMA199527435437791256
- LesarTSLomaestroBMPohlHMedication-prescribing errors in a teaching hospital: a 9-year experienceArch Intern Med19971571569769236558
- QuinlanPAshcroftDMBlenkinsoppAMedication errors: a baseline survey of interventions recorded during the dispensing process in community pharmaciesInt J Pharm Pract200210SupplR67
- ReasonJHuman error: models and managementBMJ20003207687010720363
- RuppMTScreening for prescribing errorsAm Pharm1991NS317181957804
- RuppMTDe YoungMSchondelmeyerSWPrescribing problems and pharmacist interventions in community practiceMed Care199230926401405798
- ShahSNHAslamMAveryAJA survey of prescription errors in general practicePharm J20012678602
- van MilJWFvan HeelMCDBoersmaMInterventions and documentation for drug-related problems in Dutch community pharmaciesAm J Health Syst Pharm20015814283111494789
- WesteinMPDHeringsRMCLeufkensHGMDeterminants of pharmacists' interventions linked to prescription processingPharm World Sci2001239810111468883