Abstract
Treatment of HIV-1 infection has produced dramatic success for many patients. Nevertheless, viral resistance continues to limit the efficacy of currently available agents in many patients. The CCR5 antagonists are a new class of antiretroviral agents that target a necessary coreceptor for viral entry of many strains of HIV-1. Recently, the first agent within this class, maraviroc, was approved by a number of regulatory agencies, including the Food and Drug Administration. Herein we review the role of the CCR5 receptor in HIV-1 infection and potential methods to target it in anti-HIV-1 therapy. We review the various categories of agents and discuss specific agents that have progressed to clinical study. We discuss in detail the recently approved, first in class CCR5 antagonist, maraviroc, and discuss aspects of resistance to CCR5 antagonism and the potential role of CCR5 antagonism in the management of HIV-1 infection.
Introduction
The widespread use of highly active antiretroviral therapy (HAART) has profoundly affected the treatment and epidemiology of HIV-1 infection within the developed world, where HIV-1 infection has largely become a chronic illness (CitationPalella et al 1998). HAART’s dramatic success has contributed in saving at least 3 million years of life in the US since 1989 and will aid a patient living with HIV-1 to live more than 13 years longer today than if they had been diagnosed in 1988 (CitationWalensky et al 2006). Despite tremendous impact, patient benefit from HAART is not simple or uniform; 25% of patients starting HAART either do not achieve viral suppression or lose it within 2 to 3 years, frequently due to viral resistance (CitationBartlett et al 2001; CitationMocroft et al 2002; CitationHolmberg et al 2003). Moreover, the rate of acquired resistance in patients recently infected with HIV-1 has grown from 13.2% during the period 1995 to 1998 to 24.1% during 2003 to 2004, including some with rapid progression to AIDS (CitationMarkowitz et al 2005; CitationShet et al 2006).
In spite of the recalcitrant nature of HIV-1 viral resistance, recent advances have been substantial. The approval of darunavir, a protease inhibitor with potent efficacy against multi-drug resistant strains of HIV-1, has helped shift the emphasis of HIV-1 salvage treatment from preserving immune function to complete suppression of viral replication and immune reconstitution (CitationHammer et al 2006). With the advent of additional classes of agents such as CCR5 and integrase antagonists, patients with extensive multi-drug resistance will likely be able to achieve an undetectable viral load. Nevertheless, resistance to these new agents has already been seen in vitro and will inevitably arise clinically (CitationMosley et al 2006; CitationCooper et al 2007; CitationSteigbigel et al 2007). HIV clinical investigators must be prepared to overcome these defenses by refining the current use of HAART and wisely integrating new agents, such as CCR5 antagonists, in order to minimize the impact of HIV-1 viral resistance on patients and populations (CitationSchooley and Mellors 2007).
Herein we review the role of the CCR5 receptor in HIV-1 infection and potential methods to target it in anti-HIV-1 therapy. We review the various categories of agents and discuss specific agents that have progressed to clinical study. In particular, we discuss in detail the recently approved, first in class CCR5 antagonist, maraviroc, and discuss aspects of resistance to CCR5 antagonism and the potential role of CCR5 antagonism in the management of HIV-1 infection.
Viral entry and CCR5
The mechanism by which HIV-1 infects cells was a prime target for early HIV-1 researchers. In 1984, the CD4 molecule was identified as necessary for HIV-1 replication within host cells (CitationDalgleish et al 1984). Later studies showed that CD4 alone was not sufficient for HIV-1 infection of a host cell and 2 years later, the chemokine receptor CCR5 was identified as a major co-receptor (CitationDragic et al 1996).
The proteins required for HIV-1 entry into the cell are encoded by the env gene, the product of which is the precursor to both the gp120 and gp41 glycoproteins (CitationChan et al 1997). Gp120 associates with the CD4 receptor on the surface of the host cell; gp41 spans the viral envelope and mediates viral fusion with the host cell. The two glycoproteins associate non-covalently on the viral envelope as a heterodimer and then further assemble as a trimer to form the fusion mediating structure (CitationKwong et al 1998).
On exposure of the virus to a cell expressing CD4, gp120 interacts with the CD4 molecule, thereby inducing a conformational change in gp120 that enables binding to the chemokine receptor (see ). Binding of gp120 to the chemokine receptor (either CCR5 or CXCR4) generates a conformational change in gp41, leading to insertion of a lipophilic region of gp41, known as the fusion peptide, into the lipid bilayer of the host cell. A transitional intermediate state is created in which gp41 is inserted into both the viral envelope and the cellular membrane. The virus and the cell are brought together as gp41 folds on itself in a hairpin structure, thereby bringing the viral envelope into close proximity with the cell membrane of the CD4+ host cell. Fusion is initiated, and the viral core contents are spilled into the cytoplasm (CitationChan et al 1998; CitationEckert et al 2001).
Figure 1 HIV-1 entry via CD4 and coreceptor binding gp120 binds to CD4 (A) and undergoes conformational changes that expose the co-receptor binding site (B) and enable binding to the chemokine receptor (C). Structural changes are then induced in gp41 that extend the helical domains to form a ‘pre-hairpin intermediate’ (D). The hydrophobic fusion peptide inserts into the target cell membrane, causing gp41 to span between the virus and cell membranes. The gp41 helices then fold into a six-helix bundle, bringing together the N-terminal and C-terminal domains and thus the viral and cellular membranes (E). Contact between the membranes allows mixing of the outer leaflets followed by the development of a fusion pore (G). gp120 is omitted from panels F and G for the sake of clarity. Reprinted with permission from CitationStarr-Spires LD, Collman RG. 2002. HIV-1 entry and entry inhibitors as therapeutic agents. Clin Lab Med, 22:681–701. Copright 2002 © Elsevier.
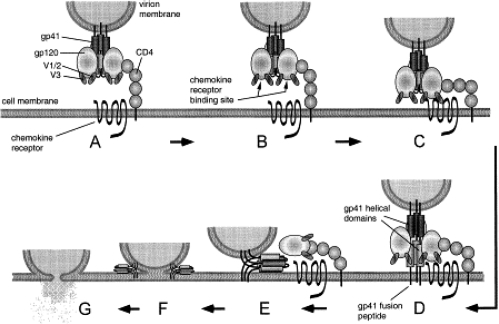
Figure 2 Development of maraviroc from the high-throughput screening hit UK-107,543. Reprinted with permission from CitationDorr P, Westby M, Dobbs S, et al 2005. Maraviroc (UK-427,857), a potent, orally bioavailable, and selective small-molecule inhibitor of chemokine receptor CCR5 with broad-spectrum anti-human immunodeficiency virus type 1 activity. Antimicrob Agents Chemother, 49:4721-32. Copyright © American Society of Microbiology.
Structure, location, and function of CCR5
Similar to other G-protein coupled receptors, chemokine receptors have a seven transmembrane structure. The N-terminus is extracellular and participates in binding of the chemokine; the C-terminus is intracellular and serves as the site for β-arrestin binding. β-arrestins facilitate G-protein independent cell signaling in addition to binding the chemokine receptor to clathrin for endocytosis and subsequent recycling (CitationZhao et al 1998; CitationOppermann 2004; CitationSignoret et al 2005). Two separate co-receptors for HIV-1 infection have been identified: CCR5 and CXCR4. There is substantial genetic variability within the amino acid sequence of gp120 molecule on the viral envelope, determining to which chemokine receptor the gp120 will bind (CitationPastore et al 2006).
The ligands for CCR5 and CXCR4 are chemokines, which are small molecules in the cytokine family that promote chemotaxis and cellular activation; on binding to their receptor on the target cell, an intracellular signaling cascade is initiated via a G-protein release from the intracellular domain of the receptor (CitationOppermann 2004). Native ligands for CCR5 include chemokines MIP-1α (macrophage inflammatory protein), MIP-1β, and RANTES (regulated on activation, normal T-cell expressed and secreted), which have been giving standard nomenclature CCL3, CCL4, and CCL5, respectively; CCR5 is expressed on immune cells, including effector and memory T-cells, natural killer cells, and antigen presenting cells (CitationBlanpain et al 1999; CitationRuffing et al 1998). As is exemplified by CCR5 and its ligands, the host defense mechanism is both complex and redundant. A single chemokine receptor can be activated by different chemokines, and similarly, a single chemokine may also activate multiple different chemokine receptors. This redundancy provides a back up plan to counteract the strategies and mutations microbes use to circumvent the host defense system.
CCR5 is heavily involved in both initiating and amplifying the immune response. At the time of microbial invasion, conserved antigens on the microbe bind to toll-like receptors on the surface of macrophages and immature dendritic cells, which release cytokines and chemokines in response. CCR5 expressing cells are then drawn toward the site of invasion by the high concentration of CCR5 binding chemokines; they ingest pathogens, mature, and then migrate to lymphoid tissue where they then prime the adaptive immune response by presenting the microbial antigens to naive B- and T-lymphocytes (CitationWong et al 2003). Antigen-specific T-lymphocytes can also release CCR5-binding chemokines, which bind to endothelial cells and components of the extracellular matrix. CCR5 expressing cells roll along the surface of the endothelium and are drawn to the increased chemokine gradient at the site of infection (CitationWong et al 2003, CitationLuther et al 2001). Of note, while CCR5 has several identified agonists, CXCR4 has only one (Stromal derived factor-1).
Distribution of CCR5-tropic virus in the HIV-positive
HIV-1 is capable of using either CCR5 or CXCR4 as a co-receptor in vivo; in vitro, it has been shown to use other chemokine receptors (CitationUnutmaz et al 1998). Some strains of HIV-1, known as R5, use only CCR5 as the co-receptor to gain access to the host cell. Other strains, X4 strains, use only CXCR4 as its co-receptor. Dual or mixed (D/M) strains, also known as R5X4 strains, can use both CCR5 and CXCR4.
In early infection, the vast majority (70%–80%) of strains isolated from treatment-naïve patients are CCR5-tropic or R5 viruses (CitationBrumme et al 2005; CitationMoyle et al 2005), whereas X4 strains, previously known as syncytium-inducing variants, are seen in 30%–60% of treatment-experienced patients and arise later in the natural history of HIV-1 infection. They are associated with accelerated progression to AIDS and lymphocyte depletion. It is unclear whether the appearance of variants that use CXCR4 as a co-receptor is a cause or an effect of immunodeficiency (CitationKoot et al 1993; CitationConnor et al 1997; CitationMelby et al 2006; CitationWilkin et al 2007). It should be noted that R5 strains still persist late into the course of disease, so the CCR5 co-receptor may still be an important pharmaceutical target even in advanced stages of disease (CitationWilkin et al 2007).
Natural variant of CCR5
In 1996, a 32 base pair mutation in the gene for CCR5, known as Δ32, was shown to protect against HIV-1 infection (CitationHuang et al 1996). The mutant allele codes for a dysfunctional truncated protein that is not expressed on the surface of the cell. The frequency of the allele is approximately 10%–14% in the white population, particularly those of Northern European descent, but is seldom seen in Asians or Africans; approximately 1% of the Caucasian population is homozygous for the deletion (CitationLiu et al 1996). Infection of Δ32 homozygotes is exceedingly rare, and when it occurs is caused by viruses using CXCR4 as a co-receptor for viral entry; heterozygotes can be infected with the HIV-1 virus but tend to have a longer disease course (CitationDean et al 1996; CitationLiu et al 1996; CitationSamson et al 1996). Patients who are homozygous for the Δ32 mutation are phenotypically normal, without readily apparent negative effects or decreased life expectancy. The preserved functional phenotype of Δ32 homozygotes is attributable to the redundancy present in the host defense system. Interestingly, mutations in murine CXCR4 (or its only known native ligand, Stromal factor-1) are lethal in the embryo (CitationLapidot 2001).
However, recent evidence suggests Δ32 homozygotes may have immunological consequences. Early researchers proposed that the mutation, in its early age, may have provided protection against Yersinia pestis (CitationStephens et al 1998), the microbial agent of the bubonic plague; others have suggested that protection against smallpox may have been the survival advantage (CitationGalvani et al 2003). The area remains controversial, and recent population studies indicate that evolution of CCR5 may have been neutral (CitationSabeti et al 2005). Another study demonstrated longer survival and delayed rejection of renal allografts in Δ32 homozygotes (CitationFischereder et al 2001), and CCR5Δ32 may be protective against the development of rheumatoid arthritis and persistent hepatitis B infection (CitationPrahalad et al 2006; CitationThio et al 2007). The Δ32 mutation has also been associated with increased mortality from encephalopathy caused by West Nile Virus (CitationGlass et al 2006). Additional studies will likely reveal other previously unrecognized complications or benefits associated with absence, dysfunction, or blockade of CCR5.
Targeting CCR5
A number of potential mechanisms are under investigation to inhibit HIV-1 binding and fusion to human cells. These include agents to block CD4 binding by viral gp120, inhibit CCR5 or CXCR4 co-receptor binding by gp120, as well as inhibit gp41 mediated fusion of the viral and cellular lipid bilayers as the Food and Drug Administration (FDA)-approved agent enfuvirtide does (CitationGuo et al 2003; CitationJacobson et al 2004; CitationOldfield et al 2005; CitationKadow et al 2006; CitationMoyle et al 2007). While it is beyond the scope of this review to discuss every agent, we will review developmentally advanced agents and the various tactics under study for the antagonism of CCR5.
With the initial discovery that CCR5 was an HIV-1 co-receptor and its endogenous ligands, (MIP-1α, MIP-1β, and RANTES) able to suppress HIV-1 replication, efforts centered on pharmacologically reproducing the effects of these chemokines. This antiviral effect is related to the ligands’ ability to internalize the receptor and deprive it from being expressed on the cell surface (CitationCocchi et al 1995). The promise of these modified chemokines and other novel agents has been difficult to bring to fruition thus far and their future remains uncertain (CitationSimmons et al 1997; CitationQin et al 2003; CitationHartley et al 2004; CitationAnderson and Akkina 2007). Another unique approach attempts to employ a zinc finger nuclease to bind, cleave, and cause mutagenesis in the CCR5 gene and thereby inhibit normal transcription and protein expression (CitationJouvenot et al 2005; CitationMani et al 2005).
Monoclonal antibodies targeting CCR5 have also been developed with CCR5mAb004 of Human Genome Sciences (Rockville, MD, USA), and PRO 140 of Progenics Pharmaceuticals (Tarrytown, NY, USA) progressing to early phase human trials. Each is a mouse-derived but humanized monoclonal antibody capable of blocking CCR5 without activation of the receptor (CitationOlson et al 1999; CitationRoschke et al 2004). A phase I study in 63 HIV-positive patients with CCR5-tropic virus demonstrated CCR5mAb004 to be safe and well tolerated with substantial anti-viral efficacy for up to 28 days after a single dose (CitationLalezari et al 2006). Subjects were randomized to 5 cohorts with an 8:2 ratio of placebo to active drug. Subjects were infused with a single dose of placebo or CCR5mAb004 at 1 of 5 dosages, 0.4, 2, 8, 20, or 40 mg/kg of body weight, and followed for 8 weeks. Greater antiviral response was observed at higher doses with 55% of subjects receiving doses of 8 mg/kg or greater and 50% in the highest dose cohort demonstrating at least a 1 log10 drop in HIV viral load. Further investigation of a more potent, next generation antibody is anticipated.
PRO 140, considered a fast-track product by the FDA, recently reported positive proof-of-concept study results. A phase I study in 39 HIV-positive patients with CCR5-tropic virus demonstrated PRO 140 to be safe, well tolerated and a potent inhibitor of HIV-1 replication with a mean maximal viral load reduction of 1.83 log10 in the highest dose group (5 mg/kg) after a single dose (CitationJacobson et al 2007). All patients receiving the highest dose had a viral load reduction of at least 1 log10. PRO140 binds to the N terminus and second extracellular domain of CCR5 and acts as a direct competitive inhibitor of HIV binding. The small-molecule antagonists to be discussed bind in a hydrophobic pocket of CCR5 formed by transmembrane helices, and act through allosteric effects. As such, the two classes of CCR5 antagonists work through different mechanisms, and virus resistant to the small molecule antagonists maintain sensitivity to PRO140 (CitationKuhmann et al 2004; CitationMarozsan et al 2005). In addition, in vitro studies demonstrate potentially synergistic effects with the small-molecule CCR5 antagonists (CitationMurga et al 2006; CitationJi et al 2007). Though PRO 140 requires parenteral administration, the interval of administration ultimately determined could be long enough to be reasonably convenient. The preliminary results are encouraging.
By far the largest group and furthest in development of CCR5 antagonists are the small-molecule inhibitors. Typically cheaper to produce than peptides with better oral bioavailability, these agents also demonstrate significant potency across diverse clades with half maximal inhibitory concentrations (IC50) measured in nanomoles. As is the case with many small-molecule inhibitors of G-coupled proteins, these agents appear to bind a pocket within the transmembrane helices, alter extracellular CCR5 conformation, and thereby inhibit HIV-1 binding (CitationDragic et al 2000). Agents that have progressed from simple labels to scientific names end in the suffix–viroc, eg, vicriviroc, to denote their action of viral receptor occupancy. Small-molecule antagonists include: TAK-779, TAK-220, Tak-652, AK602/ONO4128/GSK-873140/aplaviroc, SCH-C/SCH-351125, SCH-D/SCH-417690/vicriviroc, and UK-427,857/maraviroc. In addition to the recently approved maraviroc, which we discuss in greater detail in the following section, a number of other agents merit discussion.
The first small-molecule CCR5 antagonist published was TAK-779 of Takeda Chemical Industries (Osaka, Japan) (CitationBaba et al 1999). Though a potent inhibitor of CCR5-tropic HIV-1 in vitro, development was curtailed due to the need for subcutaneous administration and the attendant difficulties with injection site reactions. More recent focus has been placed on TAK-220 and TAK-652, each with nanomolar inhibition of HIV-1 in vitro and oral bioavailability (CitationBaba et al 2005; CitationTakashima et al 2005). A single-dose phase I study has been completed for TAK-652 and demonstrates favorable initial safety and pharmacokinetic data (CitationBaba et al 2005). Further clinical data are awaited.
Spirodiketopiperazine derivatives have been under active development by Ono Pharmaceuticals (Osaka, Japan) in collaboration with GlaxoSmithKline (Research Triangle Park, NC, USA). E913 potently suppresses the replication of laboratory and primary CCR5-tropic HIV-1 strains, including viruses resistant to available antiretroviral medications (CitationMaeda et al 2001). However aplaviroc (AK602/ONO4128/GSK-873140) demonstrates a 2-fold increase in activity versus HIV-1 isolates at sub-nanomolar concentration both in vitro and in vivo mouse model, and became the lead analogue under development (CitationMaeda et al 2004; CitationNakata et al 2005). In early phase study, a maximum dose of 600 mg twice a day for 10 days demonstrated a 1.66 log10 mean reduction in viral load and was well tolerated (CitationLalezari et al 2005). However during phase IIb trials three subjects developed severe hepatotoxicity, which was deemed secondary to drug-induced hepatitis. Moreover, 1 of the first 44 subjects enrolled in a phase III trial of aplaviroc developed severe hepatotoxicity, and the trials and development of aplaviroc were stopped (CitationCrabb 2006).
CCR5 antagonist, SCH351125 or SCH-C, was the first agent developed by Schering-Plough Corporation (Kenilworth, NJ, USA) due to its antiviral potency-- nanomolar IC50 concentrations for a range of CCR5-tropic HIV-1 isolates-- and advantageous pharmacokinetic characteristics (CitationStrizki et al 2001). The first CCR5 antagonist to enter clinical efficacy studies, SCH-C at a dose of 25 mg twice daily demonstrated a 0.5–1 log drop in viral load in 10 of 12 subjects (CitationReynes et al 2002). However, antiviral effect was not uniform and QTc interval prolongation prompted further optimization work. This resulted in Sch-417690 or SCH-D, later known as vicriviroc. Vicriviroc is 2–40 times more potent than SCH-C against primary HIV-1 isolates in vitro, has excellent oral bioavailability, and an improved safety profile (CitationStrizki et al 2005).
In early phase study, vicriviroc was well tolerated up to 50 mg twice daily and produced 1.5 to 1.6 log reductions in HIV-1 viral load at doses of 25 mg and 50 mg twice daily in treatment-naïve subjects (CitationSchurmann et al 2007). However, treatment-naïve subjects with R5-tropic virus fared less well in a phase II study comparing vicriviroc to efavirenz (EFV), both combined with zidovudine/lamivudine (AZT/3TC as fixed dose Combivir® [GlaxoSmithKline]). Subjects began the study receiving either placebo or vicriviroc monotherapy (25, 50, or 75 mg once daily) for 2 weeks. Thereafter AZT/3TC was added to subjects receiving vicriviroc, while subjects receiving placebo were given EFV and AZT/3TC instead. Though vicriviroc produced a 0.9–1.3 log10 greater reduction in viral load than placebo, preliminary analysis demonstrated virologic breakthrough (RNA ≥ 50 copies/mL) during follow-up in 2 of 24 (8%) of the placebo/AZT/3TC/EFV group versus 13 of 23 (57%), 10 of 22 (45%), and 5 of 23 (22%) in the 25, 50, and 75 mg arms of vicriviroc, respectively (CitationGreaves et al 2006). The study was subsequently terminated prematurely on recommendation of the data safety monitoring board. Neither tropism shifts nor elevated vicriviroc IC50 measurements accounted for the higher rate of virologic breakthrough. However, all subjects with virologic breakthrough and genotypic data available had treatment-emergent M184V mutations, suggesting that vicriviroc was underdosed. Such results have provoked calls that there is a near unassailable standard of care in treatment-naïve regimens, eg, EFV-based, and that these potent regimens should be embraced (CitationDeeks 2006).
Phase II vicriviroc results have been more encouraging among treatment-experienced subjects. In an AIDS Clinical Trial Group study, ACTG A5211, 24 week and recently presented 48 week data has shown that vicriviroc provided a significant advantage over placebo when added to optimized background regimen (CitationGulick et al 2007a, Citationb). Both the 10 mg and the 15 mg once daily doses were shown to provide durable virologic suppression and significant immunologic benefit: HIV-1 RNA decreases of 1.9 and 1.4 logs, and CD4+ cell count increases of 96 and 130 cells/mm3 were seen in the 10 mg and 15 mg arms, respectively. Moreover, 37% of subjects in the 10 mg vicriviroc group and 27% of those in the 15 mg group had a HIV-1 viral load below 50 copies/mL at week 48. However, the 5 mg dose study arm was discontinued early based on recommendation from the Study Monitoring Committee and the study was also unblinded following reports of 5 malignancies in subjects receiving vicriviroc. Further follow-up of 39 subjects enrolled in an open label extension study reported no new malignancies and in September 2007, it was announced that two phase III studies, entitled VICTOR-E3 and VICTOR-E4, had begun to evaluate the safety and effectiveness of 30 mg of vicriviroc plus optimized background therapy (OBT) in treatment-experienced subjects (CitationGulick et al 2007c).
Maraviroc
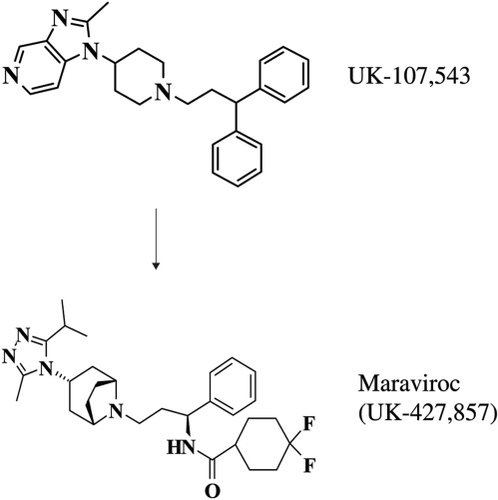
With greater understanding of the role and impact of the CCR5 receptor in the transmission and progression of HIV-1 disease, numerous efforts to pharmacologically target the CCR5 receptor began. Drug development work at Pfizer Inc. (Kent, UK) resulted in the development of UK-427,857 or maraviroc (CitationDorr et al 2005; CitationWood and Armour 2005). Opening effort centered on a high throughput screening assay employing HEK-293 cells to express CCR5 and used candidate drug antagonism of radiolabelled MIP-1β binding as the basis of the screen resulting in hits UK-107,543 and UK-179,645.
Following intensive structure-activity relationship (SAR) studies and numerous structural modifications via modern medicinal chemistry, UK-427,587, or 4,4’-difluoro-N-[(1S)-3-[(3-exo)-3-[3-methyl-5-(1-methylethyl)-4H-1,2,4-triazol-4-yl]-8-azabicyclo[3.2.1] oct-8-yl]-1-phenylpropyl]cyclohexanecarboxamid, became the lead analogue (see ). With its ability to block CCR5 binding and signaling at nanomalor concentrations plus no problematic cytochrome P450 D2 interaction or cardiac ion channel binding, and favorable permeability characteristics, further investigation began of this potent inhibitor of laboratory optimized HIV-1 isolates (mean inhibitory concentration of 90% of isolates or IC90 of 2.0 nM).
Additional work demonstrated encouraging pharmacokinetic data, and high selectivity for the CCR5 receptor compared to other pertinent receptors, eg similar chemokine receptors. The antiretroviral activity of UK-427,587 proved potent against primary HIV-1 isolates from a number of clades, as well as drug-sensitive and drug-resistance clinical isolates of HIV-1 both as monotherapy and in concert with additional antiretrovirals. UK-427,587’s mechanism of action was also confirmed to be strictly attributable to CCR5 blockade and no other antiviral means, eg, cell lysis.
Measurements made in first-in-man studies closely matched expectations derived preclinically (CitationDorr et al 2005; CitationWood and Armour 2005). Single doses were tolerable up to 900 mg, multiple doses to 600 mg daily, and twice daily doses of 100 mg of maraviroc continuously maintained plasma exposure above the IC90. No worrisome laboratory or electrocardiographic findings were observed and phase IIa efforts with 10 days of maraviroc monotherapy in the HIV-1 infected commenced shortly thereafter.
These two studies (A4001007 and A4001015) were combined for analysis and reported in November 2005 (CitationFätkenheuer et al 2005). Investigators randomized 82 CCR5-positive subjects to receive 10 days of treatment with maraviroc (25 mg, 100 mg or 300 mg once daily or 50 mg, 100 mg, 150 mg [fed and fasted] or 300 mg twice daily) or placebo. Baseline subject characteristics were similar across treatment groups and barring one subject inadvertently enrolled with D/M infection, subjects receiving 100 mg twice daily or more demonstrated robust HIV-1 suppression. Maximum viral load reductions averaged −1.68 (range −2.10 to −1.37) for the 100 mg twice daily group and peaked at −1.84 (range −2.42 to −1.49) for 300 mg twice daily. These values frequently occurred after day 11 and likely reflect the prolonged occupancy of the CCR5 receptor by maraviroc, a phenomenon also reported for other CCR5 antagonists (CitationLalezari et al 2005; CitationSchurman et al 2007). Three subjects were excluded from analysis; the aforementioned subject inadvertently enrolled with D/M infection, a subject who withdrew consent, and a subject who discontinued treatment prior to day 3 secondary to a moderate headache felt to be unrelated to their 100 mg once daily dose. Maraviroc was generally well tolerated, except for one case of severe diarrhea in the 150 mg twice daily (fed) group which started on day 1 and resolved after 11 days without intervention. The most common mild or moderate side effects were headache, asthenia, dizziness, gingivitis, and nausea. Overall these results were one of the first to demonstrate the viability of targeting the CCR5 receptor in the treatment of HIV-1 infection.
Late phase efforts in maraviroc’s development have targeted both treatment-naïve and treatment-experienced patients. Among treatment-naïve patients, maraviroc is being investigated in the MERIT study. This ongoing phase IIb/III study had interim 48-week data presented at the 4th IAS Conference on HIV Pathogenesis, Treatment and Prevention held July, 2007 (CitationSaag et al 2007). This study tests the hypothesis that maraviroc is not inferior to EFV when used in combination with AZT/3TC (provided as fixed dose Combivir) in CCR5-tropic patients without resistance to AZT, 3TC or EFV. Subjects were stratified at entry by HIV-1 viral load (> or <100,000 copies/mL) and also geographic location (Northern vs Southern Hemisphere). Of note, in an effort to minimize discontinuance due to medication intolerance, especially AZT, subjects who experienced toxicity were allowed to substitute an alternative nucleoside reverse transcriptase inhibitor. The primary endpoint was the proportion of patients who achieved a viral load <50 copies/mL through 48 weeks, which proved important to the investigators’ conclusions.
Initially planned with three treatment groups, maraviroc 300 mg once or twice daily or EFV, the data safety and monitoring board closed the once-daily maraviroc arm early because of inadequate response rates. The remaining study arms recruited 721 subjects with a mean age of 37 years, 79% men/21% women, roughly 50% white/35% black, and roughly 400 from the Northern Hemisphere vs 300 from the Southern Hemisphere. At baseline, subject characteristics were similar between the EFV and maraviroc groups: median CD4 counts of 241 and 254 cells/mm3, respectively, and mean viral load of roughly 4.9 log copies/mL each.
By 48 weeks, 65.3% of the maraviroc arm and 69.3% of the EFV arm achieved a viral load <50 copies/mL. This margin of difference failed to meet the preselected criteria for noninferiority as the lower bound of the 97.5% confidence interval was less than −10% (observed noninferiority margin −10.9%). Using an endpoint of <400 copies/mL at 48 weeks, twice daily maraviroc met noninferiority criteria as 70.6% of subjects in the maraviroc arm and 73.1% of the EFV arm achieved the endpoint. Also by 48 weeks, a greater increase in mean CD4 cell count was observed in the maraviroc treated subjects than in the EFV treated (170 cells/mm3 vs 144 cells/mm3) though this difference likely has little clinical relevance.
Two subgroup analyses are of particular note. Among subjects with baseline viral loads <100,000 copies/mL EFV and maraviroc had similar rates of suppression to <50 copies/mL (71.6% vs 69.6% respectively). However, EFV was superior to maraviroc when baseline viral load was >100,000 copies (proportion with viral loads <50 copies/mL, 66.6% vs 59.6%). The two geographic regions also demonstrated a difference in response. Higher rates of response were observed with EFV in subjects from the Southern hemisphere (proportion with viral loads <50 copies/mL, 71.0% vs 62.1%) while similar rates of response were observed in subjects from the Northern Hemisphere. No underlying mechanism(s) has been clearly identified for this difference though clade variation between hemispheres may play a role.
Rates of study drug discontinuation were similar in the two groups (26.9% for maraviroc and 25.2% for EFV) though reasons did differ. Subjects receiving EFV were more likely to stop due to adverse events (13.6% vs 4.2%; typically neuropsychiatric side effects such as abnormal dreams and dizziness) while subjects receiving maraviroc experienced higher rates of virologic failure (11.9% vs 4.2% in the EFV arm). Subjects taking maraviroc had fairly more frequent cases of bronchitis, and nose and throat infections.
Further safety analyses demonstrated similar proportions of severe adverse events as well as severe (grade 3 or 4) liver enzyme disturbances, which were infrequent in both groups but nevertheless helped prompt an FDA “black box” warning regarding potential hepatotoxicity. Rates of new malignancies also did not differ between the treatment groups, which is a reassuring finding after initial concerns regard increased risk of malignancy with vicriviroc and potentially all CCR5 antagonists. Overall, maraviroc performed very well in the MERIT study but fell just short of rivaling EFV, an agent considered by some to be a standard worth embracing (CitationDeeks 2006).
Two identical studies, MOTIVATE 1 and MOTIVATE 2, are investigating maraviroc in treatment-experienced CCR5-tropic HIV-1 positive patients (CitationLalezari et al 2007; CitationNelson et al 2007). Identical in design, these phase IIb/III studies included subjects with: resistance to and/or ≥6 months experience with at least one antiretroviral agent from each of the three approved oral drug classes (at least 2 agents for protease inhibitors), HIV-1 viral load of ≥5,000 copies/mL and either off treatment or on a stable but failing antiretroviral regimen for at least four weeks. Subjects were stratified by enfurvitide use as well as viral load > or <100,000 copies/mL. Applying genotypic and phenotypic test results, subjects were randomized to receive OBT plus placebo, maraviroc once daily or maraviroc twice daily (subjects receiving a PI other than tipranavir and/or delavirdine in their OBT received 150 mg while remaining subjects received 300 mg) in a 1:2:2 ratio.
Interim results from planned 24-week analyses of both trials were very similar (see ). MOTIVATE 1 enrolled 601 subjects mainly from North America, while MOTIVATE 2 enrolled 475 individuals mainly from Europe and Australia. In each study the vast majority of subjects were male (84%–91%) and predominately white (81%–87%). Baseline characteristics were similar across treatment groups in both studies. Median baseline CD4+ cell counts ranged from 150 to 182 cells/mm3, median baseline viral loads from 4.84 to 4.89 log10 copies/mL, enfuvirtide (T-20, Fuzeon) use from 37% to 46% of subjects, and the majority of subjects had 2 or fewer active agents in their OBT (66%–76% and 62%–66% in MOTIVATE 1 and 2, respectively).
Table 1 24-week results of phase III maraviroc studies in CCR5-tropic subjects (CitationLalezari et al 2007; CitationNelson et al 2007)
Maraviroc arms in both studies demonstrated highly statistically significant virologic and immunologic benefits compared with the placebo groups. Maraviroc was very well tolerated, with no differences observed in the rate of study discontinuation or grade 3/4 adverse events across treatment arms. Importantly, no excess of cancer diagnoses or liver function abnormalities were observed in the maraviroc groups compared to placebo.
Combined analysis of the two studies was performed to assess maraviroc’s contribution to viral suppression. As expected, with an increasing number of active agents in the OBT, the greater the likelihood of reaching an undetectable viral load. Subjects in the maraviroc arms achieved a much higher proportion of complete viral suppression when two or fewer active agents were present in the OBT in comparison with the placebo arm. This is consistent with numerous prior studies demonstrating that two active agents are keys to a successful salvage regimen.
More recent combined 24-week analyses demonstrated results similar to the individual studies (see ; CitationGulick et al 2007d). While the studies were not designed for a formal comparison of once daily and twice daily maraviroc dosing, higher rates of virologic suppression were observed with twice-daily maraviroc than with once-daily maraviroc in several important subgroups: subjects with viral loads ≥100,000 copies/mL at screening, and also subjects with baseline CD4 counts <50 cells/mm3. With such robust data, the makers of maraviroc requested and received accelerated approval by the FDA for treatment-experienced patients with inadequate control of multidrug resistant, CCR5-tropic HIV-1. In conjunction with maraviroc’s approval, the single-cycle recombinant virus tropism assay (Trofile®, Monogram Biosciences South San Francisco, CA, USA) also began its commercial availability (CitationCoakley et al 2005).
Table 2 Contribution of maraviroc at 24 weeks to viral suppression based on overall susceptibility score of phase III maraviroc studies (CitationGulick et al 2007d)
While the approval of maraviroc is for the treatment of patients with CCR5-tropic virus, its potential in patients with D/M-tropic virus has also been evaluated. Pfizer study A4001029 is a double-blind placebo controlled study in subjects with D/M-tropic virus who were randomized to OBT including at least one sensitive drug, plus either maraviroc once daily, maraviroc twice daily, or placebo (CitationGoodrich et al 2007). 186 subjects with D/M virus and advanced immunodeficiency, approximate median CD4 cell count of 42 cells/mm3 and HIV viral load of 5.1 log copies/mL within each cohort, were enrolled across the study.
After 48 weeks, the mean viral load decreases were 0.62 log copies/mL in the once-daily maraviroc group, 1.11 log copies/mL in the twice-daily group, and 0.84 log copies/mL in the placebo group. These differences were not statistically significant and there was also no substantial difference across study cohorts in the proportion of subjects who achieved an undetectable viral load. However, despite a lack of antiretroviral benefit, CD4 cell counts did rise in both maraviroc cohorts, by 65 cells/mm3 in the once daily arm and 78 cells/mm3 in the twice daily arm, whereas the placebo cohort CD4 cell count increase was only 51 cells/mm3. This finding has generated interest in the possibility that maraviroc, or CCR5 antagonists in general, may have an effect on elevating CD4 cell counts independent of antiviral activity.
Similar rates of adverse effects and deaths were observed, while no cases of lymphoma or adenocarcinoma occurred. Thus, in addition to further reassurance of maraviroc’s safety profile, the lack of HIV progression in the D/M group was quite significant and deserves additional investigation as concerns linger regarding the impact of X4-tropic virus.
Consequences of CCR5 antagonist treatment
A number of concerns, some unique and others general, are germane to the potential use of CCR5 antagonists in patients. As previously discussed, targeting CCR5 leaves a patient without the role of the CCR5 receptor in innate immunity. However, the natural example of the Δ32 CCR5 allele and the redundancy of chemokine receptor function provide significant reassurance that blockade should be tolerable. Whether untoward consequences of the iatrogenic loss of the CCR5 receptor’s function, including an undue number of severe West Nile virus infections in WNV endemic areas, is a central question that will prove important to CCR5 antagonist use.
Also, just as with all antiretrovirals to date, the issue of viral escape has attended the development of CCR5 antagonists. This concern takes on more substance with CCR5 antagonists than other agents as failure of HAART using a CCR5 antagonist may result in co-receptor switching to CXCR4. Whether de novo or through promotion of minor D/M or CXCR4 using variants already present within the patient, co-receptor switching would be a troubling outcome as D/M and CXCR4 tropic viruses have historically, but not uniformly, been associated with accelerated CD4 cell loss and progression to AIDS (CitationPhilpott 2003; CitationDaar et al 2007; CitationGoetz et al 2007). Nevertheless it remains possible that emergence of CXCR4 using virus is a consequence and not a cause of severe immunodeficiency.
Some data addressing co-receptor switching in the setting of CCR5 antagonist use have been reported. Analysis of co-receptor switching during early studies of maraviroc suggests that emergent D/M and CXCR4 tropic viruses result from a pre-treatment reservoir not detected by screening tropism assays (CitationWestby et al 2006). During MOTIVATE 1 and 2, maraviroc’s phase III trials, 63 of 751 MVC treated subjects failed with D/M or X4-tropic virus compared to 35 R5-tropic subjects failing with R5-tropic virus. Reassuringly, patients failing a maraviroc regimen with D/M or X4-tropic virus had higher mean increases in CD4 count vs placebo at time of failure (range +37 to +56 cells/μl vs +14 cells/μl respectively). Approximately two thirds of these subjects had their D/M or X4 virus return to R5 tropism prior to going off study (median = 203 days), and there was no association between CXCR4-using virus and AIDS-defining events. Time to failure with a D/M or X4-tropic virus was also shorter than for failure with a CCR5-tropic virus. Overall, these results are consistent with the selective and reversible suppression of R5 virus during maraviroc therapy (Citationvan der Ryst et al 2007).
In vitro studies have also demonstrated that viral escape may be a consequence of viral adaptation to the conformational change in CCR5 caused by CCR5 antagonist binding. Laboratory isolates of HIV-1 have demonstrated the ability to generate mutations in the V3 region of gp120 that allow cell entry via vicriviroc- or maraviroc-bound CCR5 (CitationPugach et al 2007; CitationWestby et al 2007). Emerging data demonstrate multiple pathways and significant complexity to CCR5 resistance. Preliminarily it appears these mutations are not as stereotypical as those for other antiretroviral agents but rather specific to the env background of the individual virus (CitationMori et al 2007; CitationTsibris et al 2007).
Role in HIV-1 therapy and conclusions
Evidenced by the FDA and European Medicines Agency’s (EMEA) recent approval of maraviroc (as Selzentry® in the USA and Celsentri® in the EU), CCR5 antagonists are a welcome addition to the care of treatment-experienced patients with CCR5-tropic virus. Their potential role in treatment-naïve patients is unsupported at this time, considering the shortfalls of both maraviroc and vicriviroc based regimens against an EFV based regimen. This is unfortunate, as it may be better to use CCR5 antagonists early in the course of HIV-1 infection treatment when CCR5-tropic virus predominates. Whether patients with D/M virus may derive immunologic benefit from a CCR5 antagonist without significant consequence also remains to be seen in large studies.
Additional questions that remain to be answered that will help guide the use of CCR5 antagonists include whether the agents are cross-resistant, synergistic with each other or other agents, and, should CXCR4 antagonists be developed, whether combination X4/R5 inhibitor therapy would have merit. Clearly the addition of another distinct antiretroviral class should be met with celebration, particularly since it is only 10 years after target identification. However further experience and study are needed to clearly define the risks, benefits, and roles that CCR5 antagonists will have in the care of HIV-infected patients.
References
- AndersonJAkkinaRComplete knockdown of CCR5 by lentiviral vector-expressed siRNAs and protection of transgenic macrophages against HIV-1 infectionGene Ther20071412879717597795
- BabaMNishimuraOKanzakiNA small-molecule, nonpeptide CCR5 antagonist with highly potent and selective anti-HIV-1 activityProc Natl Acad Sci USA199996569870310318947
- BabaMTakashimaKMiyakeHTAK-652 inhibits CCR5-mediated human immunodeficiency virus type 1 infection in vitro and has favorable pharmacokinetics in humansAntimicrob Agents Chemother20054945849116251299
- BartlettJADeMasiRQuinnJOverview of the effectiveness of triple combination therapy in antiretroviral-naive HIV-1-1-1 infected adultsAIDS20011513697711504958
- BlanpainCMigeotteILeeBCCR5 binds multiple CC-chemokines: MCP-3 acts as a natural antagonistBlood199994189990510477718
- BrummeZLGoodrichJMayerHBMolecular and clinical epidemiology of CXCR4-using HIV-1 in a large population of antiretroviral-naïve individualsJ Infect Dis20051924667415995960
- ChanDCFassDBergerJMCore structure of gp41 from the HIV envelope glycoproteinCell199789263739108481
- ChanDCKimPSHIV entry and its inhibitionCell19989368149630213
- CoakleyEPetropoulosCJWhitcombJMAssessing chemokine co-receptor usage in HIVCurr Opin Infect Dis20051891515647694
- CocchiFDeVicoALGarzino-DemoAIdentification of RANTES, MIP-1 alpha, and MIP-1 beta as the major HIV-suppressive factors produced by CD8+ T cellsScience19952701811158525373
- ConnorRISheridanKECeradiniDChange in coreceptor use correlates with disease progression in HIV-1 infected individualsJ Exp Med199718562189034141
- CooperDGatellJRockstrohJResults from BENCHMRK-1, a phase III study evaluating the efficacy and safety of MK-0518, a novel HIV-1integrase inhibitor, in patients with triple-class resistant virus2007Program and abstracts of the 14th Conference on Retroviruses and Opportunistic InfectionsLos Angeles, CA Abstract 105aLB
- CrabbCGlaxoSmithKline ends aplaviroc trialsAIDS20062064116514292
- DaarESKeslerKLPetropoulosCJHemophilia Growth and Development Study. Baseline HIV type 1 coreceptor tropism predicts disease progressionClin Infect Dis200745643917683002
- DalgleishAGBeverleyPCClaphamPRThe CD4 (T4) antigen is an essential component of the receptor for the AIDS retrovirusNature198431276376096719
- DeanMCarringtonMWinklerCGenetic restriction of HIV-1 infection and progression to AIDS by a deletion allele of the CKR5 structural gene: Hemophilia Growth and Development Study, Multi-center AIDS Cohort Study, Multicenter Hemophilia Cohort Study, San Francisco City Cohort, ALIVE StudyScience19962731856628791590
- DeeksSGChallenges of developing R5 inhibitors in antiretroviral naive HIV-infected patientsLancet2006367711316517257
- DorrPWestbyMDobbsSMaraviroc (UK-427,857), a potent, orally bioavailable, and selective small-molecule inhibitor of chemokine receptor CCR5 with broad-spectrum anti-human immunodeficiency virus type 1 activityAntimicrob Agents Chemother20054947213216251317
- DragicTLitwinVAllawayGPHIV-1 entry into CD4+ cells is mediated by the chemokine receptor CC-CKR-5Nature1996381667738649512
- DragicTTrkolaAThompsonDAA binding pocket for a small molecule inhibitor of HIV-1 entry within the transmembrane helices of CCR5Proc Natl Acad Sci USA20009756394410779565
- EckertDMKimPSMechanisms of viral membrane fusion and its inhibitionAnnu Rev Biochem20017077781011395423
- FätkenheuerGPozniakALJohnsonMAEfficacy of short-term monotherapy with maraviroc, a new CCR5 antagonist, in patients infected with HIV-1Nat Med2005111170216205738
- FischerederMLuckowBHocherBCC chemokine receptor 5 and renal-tranplant survivalLancet200135717586111403814
- GalvaniAPSlatkinMEvaluating plague and smallpox as historical selective pressures for the CCR5-Δ32 HIV-resistance alleleProc Natl Acad Sci USA200310015276914645720
- GlassWGMcDermottDHLimJKCCR5 deficiency increases risk of symptomatic West Nile virus infectionJ Exp Med2006203354016418398
- GoetzMBLeducRKostmanJRPrediction of disease progression by HIV coreceptor tropism in persons with untreated chronic HIV infection2007Program and abstracts of the 47th Interscience Conference on Antimicrobial Agents and ChemotherapyChicago, Ill Abstract H-1027
- GoodrichJMSaagMvan der RystE48-week safety and efficacy of maraviroc, a novel ccr5 antagonist, in combination with optimized background therapy (OBT) for the treatment of antiretroviral-experienced patients infected with dual/mixed-tropic HIV-12007Program and abstracts of the 45th Annual Infectious Diseases Society of AmericaSan Diego, CA Abstract LB-2
- GreavesWLandovitzRFätkenheuerGLate Virologic breakthrough in treatment-naive patients on a regimen of combivir + vicriviroc2006Program and abstracts of the 13th Conference on Retroviruses and Opportunistic InfectionsDenver, CO Abstract 161LB
- GulickRSuZFlexnerCPhase II study of the safety and efficacy of vicriviroc in HIV-infected treatment-experienced subjects: ACTG 5211J Infect Dis2007a1963041217570119
- GulickRSuZFlexnerCfor the ACTG 5211 TeamACTG 5211: phase II study of the safety and efficacy of vicriviroc (VCV) in HIV-infected treatment-experienced subjects: 48 week results2007bProgram and abstracts of the 4th International AIDS Society Conference on HIV Pathogenesis, Treatment and PreventionSydney, Australia Abstract TUAB102
- GulickRHaasDCollierATwo-year follow-up of treatment-experienced patients on vicriviroc (VCV)2007cProgram and abstracts of the 47th Interscience Conference on Antimicrobial Agents and ChemotherapyChicago, IL Abstract H-1030
- GulickRMvan der RystELampirisHEfficacy and safety of once-daily (QD) compared with twice-daily (BID) maraviroc plus optimized background therapy (OBT) in treatment-experienced patients infected with CCR5-tropic-HIV-1: 24-week combined analysis of the MOTIVATE 1 and 2 studies2007dProgram and abstracts of the 4th IAS Conference on HIV Pathogenesis, Treatment and Prevention Abstract WEPEB116LB
- GuoQHoHTDickerIBiochemical and genetic characterizations of a novel human immunodeficiency virus type 1 inhibitor that blocks gp120-CD4 interactionsJ Virol200377105283612970437
- HammerSMSaagMSSchechterMInternational AIDS Society-USA panel. Treatment for adult HIV-1 infection: 2006 recommendations of the International AIDS Society-USA panelJAMA20062968274316905788
- HartleyOGaertnerHWilkenJMedicinal chemistry applied to a synthetic protein: development of highly potent HIV entry inhibitorsProc Natl Acad Sci USA200410116460515545608
- HolmbergSDHamburgerEMMoormanACFactors associated with maintenance of long-term plasma human immunodeficiency virus RNA suppressionClin Infect Dis200337702712942404
- HuangYPaxtonWAWolinskySMThe role of a mutant CCR5 allele in HIV-1 transmission and disease progressionNat Med19962124038898752
- JacobsonJMIsraelRJLowyITreatment of advanced human immunodeficiency virus type 1 disease with the viral entry inhibitor PRO 542Antimicrob Agents Chemother200448423914742190
- JacobsonJMThompsonMSaagMSAntiretroviral Activity and Pharmacodynamics of PRO 140, a CCR5 Monoclonal Antibody, in HIV-Infected Individuals2007Program and abstracts of the 47th Annual Interscience Conference on Antimicrobial Agents and ChemotherapyChicago, IL Abstract H-716
- JiCZhangJDioszegiMCCR5 small-molecule antagonists and monoclonal antibodies exert potent synergistic antiviral effects by cobinding to the receptorMol Pharmacol200772182817392523
- JouvenotYPerezEUrnovFDTowards Gene Knock Out Therapy for AIDS/HIV: Targeted Disruption of CCR5 Using Engineered Zinc Finger Protein Nucleases (ZFNs)2005Program and abstracts of the 45th Annual Interscience Conference on Antimicrobial Agents and ChemotherapyWashington, DC Abstract H-1084
- KadowJWangHGLinPFSmall-molecule HIV-1 gp120 inhibitors to prevent HIV-1 entry: an emerging opportunity for drug developmentCurr Opin Investig Drugs200677216
- KootMKeetIPVosAHPrognostic value of HIV-1 syncytium-inducing phenotype for rate of CD4+ cell depletion and progression to AIDSAnn Intern Med199311868188096374
- KuhmannSEPugachPKunstmanKJGenetic and phenotypic analyses of human immunodeficiency virus type 1 escape from a small-molecule CCR5 inhibitorJ Virol2004782790807 Erratum in: J Virol, 2005 78:670614990699
- KwongPDWyattRRobinsonJStructure of an HIV gp120 envelope glycoprotein in complex with the CD4 receptor and a neutralizing human antibodyNature1998393648599641677
- LalezariJThompsonMKumarPAntiviral activity and safety of 873140, a novel CCR5 antagonist, during short-term monotherapy in HIV-infected adultsAIDS2005191443816135896
- LalezariJLedermanMYadavalliGA phase 1, dose-escalation, placebo-controlled study of a fully human monoclonal antibody (CCR5mAb004) against CCR5 in patients with CCR5-tropic HIV-1 infection2006Program and abstracts of the 46th Interscience Conference on Antimicrobial Agents and ChemotherapySan Francisco, CA Abstract H-1668
- LalezariJGoodrichJDeJesusEMOTIVATE 1. USA and Canada. Efficacy and safety of maraviroc plus optimized background therapy in viremic, ART-experienced patients infected with CCR5-tropic HIV-1: 24-week results of phase 2b/3 studies2007Program and abstracts of the 14th Conference on Retroviruses and Opportunistic InfectionsLos Angeles, CA Abstract 104bLB
- LapidotTMechanism of human stem cell migration and repopulation of NOD/SCID and B2mnull NOD/SCID mice. The role of SDF-1/CXCR4 interactionsAnn NY Acad Sci2001938839511458529
- LiuRPaxtonWAChoeSHomozygous defect in HIV-1 coreceptor accounts for resistance of some multiply-exposed individuals to HIV-1 infectionCell199686367778756719
- LutherSACysterJGChemokines as regulators of T cell differentiationNat Immunol20012102711175801
- MaedaKYoshimuraKShibayamaSNovel low molecular weight spirodiketopiperazine derivatives potently inhibit R5 HIV-1 infection through their antagonistic effects on CCR5J Biol Chem20012763519420011454872
- MaedaKNakataHKohYSpirodiketopiperazine-based CCR5 inhibitor which preserves CC-chemokine/CCR5 interactions and exerts potent activity against R5 human immunodeficiency virus type 1 in vitroJ Virol20047886546215280474
- ManiMKandavelouKDyFJDesign, engineering, and characterization of zinc finger nucleasesBiochem Biophys Res Commun20053354475716084494
- MarkowitzMMohriHMehandruSInfection with multidrug resistant, dual-tropic HIV-1and rapid progression to AIDS: a case reportLancet20053651031815781098
- MarozsanAJKuhmannSEMorganTGeneration and properties of a human immunodeficiency virus type 1 isolate resistant to the small molecule CCR5 inhibitor, SCH-417690 (SCH-D)Virology20053381829915935415
- MelbyTDespiritoMDemasiRHIV-1 coreceptor use in triple-class treatment-experienced patients: baseline prevalence, correlates, and relationship to enfuvirtide responseJ Infect Dis20061942384616779731
- MocroftAPhillipsANFriis-MollerNResponse to antiretroviral therapy among patients exposed to three classes of antiretrovirals: results from the EuroSIDA StudyAntivir Ther20021213012008784
- MoriJMosleyMLewisMCharacterization of maraviroc resistance in patients failing treatment with CCR5-tropic virus in MOTIVATE 1 and MOTIVATE 22007Program and abstracts of the 16th International HIV Drug Resistance WorkshopBarbados, West Indies Abstract 10
- MosleyMSmith-BurchnellCMoriJResistance to the CCR5 antagonist maraviroc is characterized by dose-response curves that display a reduction in maximal inhibition2006Program and abstracts of the 13th Conference on Retroviruses and Opportunistic InfectionsDenver, Colorado Abstract 598
- MoyleGJWildfireAMandaliaSEpidemiology and predictive factors for chemokine receptor use in HIV-1 infectionJ Infect Dis20051918667215717260
- MoyleGJDeJesusEBoffitoMCXCR4 antagonism: proof of activity with AMD110702007Program and abstracts of the 14th Conference on Retroviruses and Opportunistic InfectionsLos Angeles, CA Abstract 511
- MurgaJDFrantiMPevearDCPotent antiviral synergy between monoclonal antibody and small-molecule CCR5 inhibitors of human immunodeficiency virus type 1Antimicrob Agents Chemother20065032899617005807
- NakataHMaedaKMiyakawaTPotent anti-R5 human immunodeficiency virus type 1 effects of a CCR5 antagonist, AK602/ONO4128/GW873140, in a novel human peripheral blood mononuclear cell nonobese diabetic-SCID, interleukin-2 receptor gamma-chain-knocked-out AIDS mouse modelJ Virol20057920879615681411
- NelsonMFatkenheuerGKonourinaIMOTIVATE 2. Europe, Australia and USA. Efficacy and safety of maraviroc plus optimized background therapy in viremic, ART-experienced patients infected with CCR5-tropic HIV-1: 24-week results of phase 2b/3 studies2007Program and abstracts of the 14th Conference on Retroviruses and Opportunistic InfectionsLos Angeles, CA Abstract 104aLB
- OldfieldVKeatingGMPloskerGEnfuvirtide: a review of its use in the management of HIV infectionDrugs20056511396015907147
- OlsonWCRabutGENagashimaKADifferential inhibition of human immunodeficiency virus type 1 fusion, gp120 binding, and CC-chemokine activity by monoclonal antibodies to CCR5J Virol199973541455510196311
- OppermannMChemokine receptor CCR5: insights into structure, function, and regulationCell Signal20041612011015337520
- PalellaFJJrDelaneyKMMoormanACDeclining morbidity and mortality among patients with advanced human immunodeficiency virus infection. HIV-1 Outpatient Study InvestigatorsN Engl J Med1998338853609516219
- PastoreCNedellecRRamosAHuman immunodeficiency virus type 1 coreceptor switching: V1/V2 gain-of-fitness mutations compensate for V3 loss-of-fitness mutationsJ Virol200680750816378977
- PhilpottSMHIV-1 coreceptor usage, transmission, and disease progressionCurr HIV Res200312172715043204
- PrahaladSNegative association between the chemokine receptor CCR5-[Delta]32 polymorphism and rheumatoid arthritis: a meta-analysisGenes Immun20067264816541097
- PugachPMarozsanAJKetasTJHIV-1 clones resistant to a small molecule CCR5 inhibitor use the inhibitor-bound form of CCR5 for entryVirology20073612122817166540
- QinXFAnDSChenISInhibiting HIV-1 infection in human T cells by lentiviral-mediated delivery of small interfering RNA against CCR5Proc Natl Acad Sci USA2003100183812518064
- ReynesJRouzierRKanouniT SCH C:Safety and antiviral effects of a CCR5 receptor antagonist in HIV-1-infected subjects2002Program and abstracts of the 9th Conference on Retroviruses and Opportunistic InfectionsSeattle, WA Abstract 1
- RoschkeVClarkSBrancoLCharacterization of a panel of novel human monoclonal antibodies that specifically antagonize CCR5 and Block HIV-1 entry2004Program and abstracts of the 44th Interscience Conference on Antimicrobial Agents and ChemotherapyWashington, D.C. Abstract #2871
- RuffingNSullivanNSharmeenLCCR5 has an expanded ligand-binding repertoire and is the primary receptor used by MCP-2 on activated T cellsCell Immunol199818916089790730
- SaagMIvePHeeraJA multicenter, randomized, double-blind, comparative trial of a novel CCR5 antagonist, maraviroc versus efavirenz, both in combination with Combivir (zidovudine [ZDV]/lamivudine [3TC]), for the treatment of antiretroviral naive patients infected with R5 HIV 1: Week 48 results of the MERIT study2007Program and abstracts of the 4th IAS Conference on HIV Pathogenesis, Treatment and PreventionSydney, Australia Abstract WESS104
- SabetiPCWalshESchaffnerSFThe case for selection at CCR5-Delta32PLoS Biol20053e37816248677
- SamsonMLibertFDoranzBJResistance to HIV-1 infection in Caucasian individuals bearing mutant alleles of the CCR-5 chemokine receptor geneNature199638272258751444
- SchooleyRTMellorsJWNo cure yet for HIV-1-1, but therapeutic research presses onJ Infect Dis2007195770217299705
- SchurmannDFätkenheuerGReynesJAntiviral activity, pharmacokinetics and safety of vicriviroc, an oral CCR5 antagonist, during 14-day monotherapy in HIV-infected adultsAIDS2007211293917545705
- ShetABerryLMohriHTracking the prevalence of transmitted antiretroviral drug-resistant HIV-1-1: a decade of experienceJ Acquir Immune Defic Syndr2006414394616652051
- SignoretNHewlettLWavreSAgonist-induced endocytosis of CC chemokine receptor 5 is clathrin dependentMol Biol Cell2005169021715591129
- SimmonsGClaphamPRPicardLPotent inhibition of HIV-1 infectivity in macrophages and lymphocytes by a novel CCR5 antagonistScience199727627699092481
- Starr-SpiresLDCollmanRGHIV-1 entry and entry inhibitors as therapeutic agentsClin Lab Med20022268170112244592
- SteigbigelRKumarPEronJResults from BENCHMRK-2, a phase III study evaluating the efficacy and safety of MK-0518, a novel HIV-1integrase inhibitor, in patients with triple-class resistant virus2007Program and abstracts of the 14th Conference on Retroviruses and Opportunistic InfectionsLos Angeles, CA Abstract 105bLB
- StephensJCReichDEGoldsteinDBDating the origin of the CCR5-Delta32 AIDS-resistance allele by the coalescence of haplotypesAm J Hum Genet1998621507159585595
- StrizkiJMXuSWagnerNESCH-C (SCH 351125), an orally bioavailable, small molecule antagonist of the chemokine receptor CCR5, is a potent inhibitor of HIV-1 infection in vitro and in vivoProc Natl Acad Sci USA200198127182311606733
- StrizkiJMTremblayCXuSDiscovery and characterization of vicriviroc (SCH 417690), a CCR5 antagonist with potent activity against human immunodeficiency virus type 1Antimicrob Agents Chemother2005494911916304152
- TakashimaKMiyakeHKanzakiNHighly potent inhibition of human immunodeficiency virus type 1 replication by TAK-220, an orally bioavailable small-molecule CCR5 antagonistAntimicrob Agents Chemother20054934748216048963
- ThioCLAstemborskiJBashirovaAGenetic protection against hepatitis B virus conferred by CCR5Delta32: Evidence that CCR5 contributes to viral persistenceJ Virol200781441517079285
- TsamisFGavrilovSKajumoFAnalysis of the mechanism by which the small-molecule CCR5 antagonists SCH-351125 and SCH-350581 inhibit human immunodeficiency virus type 1 entryJ Virol2003775201812692222
- TsibrisAMNGulickRMSuZIn vivo emergence of HIV-1 resistance to the CCR5 antagonist vicriviroc: findings from ACTG A52112007Program and abstracts of the 16th International HIV Drug Resistance WorkshopBarbados, West Indies Abstract 13
- UnutmazDKewalRamaniVNLittmanDRG protein-coupled receptors in HIV and SIV entry: new perspectives on lentivirus-host interactions an on the utility of animal modelsSemin Immunol199810225369653049
- van der RystEWestbyMChanges in HIV-1 co-receptor tropism for patients participating in the maraviroc Motivate 1 and 2 clinical trials2007Program and abstracts of the 47th Interscience Conference on Antimicrobial Agents and ChemotherapyChicago, IL Abstract H-715
- WalenskyRPPaltielADLosinaEThe survival benefits of AIDS treatment in the United StatesJ Infect Dis200619411916741877
- WestbyMLewisMWhitcombJEmergence of CXCR4-using human immunodeficiency virus type 1 (HIV-1) variants in a minority of HIV-1-infected patients following treatment with the CCR5 antagonist maraviroc is from a pretreatment CXCR4-using virus reservoirJ Virol20068049092016641282
- WestbyMSmith-BurchnellCMoriJReduced maximal inhibition in phenotypic susceptibility assays indicates that viral strains resistant to the CCR5 antagonist maraviroc utilize inhibitor-bound receptor for entryJ Virol20078123597117182681
- WilkinTJSuZKuritzkesDRHIV type 1 chemokine coreceptor use among antiretroviral-experienced patients screened for a clinical trial of a CCR5 inhibitor: AIDS Clinical Trial Group A5211J Infect Dis2007445915
- WongMMFishENChemokines: attractive mediators of the immune responseSemin Immunol20031551412495636
- WoodAArmourDThe discovery of the CCR5 receptor antagonist, UK-427,857, a new agent for the treatment of HIV infection and AIDSProg Med Chem2005432397115850827
- ZhaoJMaLWuYLChemokine receptor CCR5 functionally couples to inhibitory G proteins and undergoes desensitizationJ Cell Biochem19987136459736452