Abstract
Bendamustine is an alkylating agent which also shows properties of a purine analog. Because of its unique mechanism of action it shows activity in relapsed indolent lymphomas which are resistant to alkylating agents, purine analogs, and rituximab. Bendamustine has a favorable toxicity profile causing no alopecia and only a moderate hematotoxicity and gastrointestinal toxicity. Combinations of bendamustine with mitoxantrone and rituximab and with rituximab alone have been shown to be highly active in relapsed/refractory indolent lymphomas and mantle cell lymphomas achieving long lasting complete remissions. Because of only moderate toxicity these combinations can be applied safely in elderly patients who can be treated in an outpatient setting.
Introduction
Indolent B-cell lymphomas are a heterogenous group of lymphoproliferative malignancies with a relatively good prognosis and a median survival of up to 10 years (CitationArmitage et al 1993). Standard first-line chemotherapy results in high response rates but unfortunately the disease relapses and second and further lines of chemotherapy lead to continously lower remission rates and shorter periods until the next anti-lymphoma therapy is necessary. Therefore new treatments that are highly active in the relapsed situation and result in long term remissions are urgently needed.
Development of bendamustine, mechanism of action, and metabolism
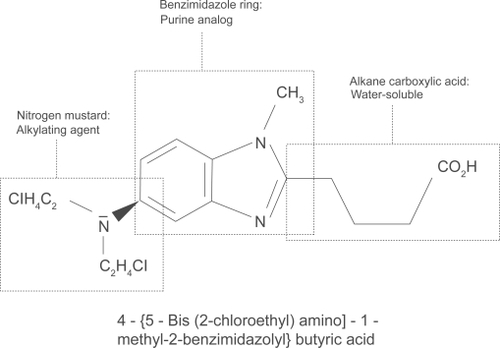
Bendamustine hydrochloride was first synthesized in 1963 by Ozegowski and Krebs in East Germany. It is a water soluble, white, microcrystalline powder with amphoteric properties due to a nitrogen mustard group and a butyric acid side chain. Chemically it is 4-{5-[bis(2-chloro-ethyl)amino]-1-methyl-2-benzimidazolyl}butyric acid (). It has a nitrogen mustard moiety, a benzimidazole ring, and an alkane carboxylic acid side chain, which all may be responsible for its cytotoxic activity (CitationOzegowski and Krebs 1963, Citation1971; CitationSchnabel et al 1967). Bendamustine acts as an alkylating agent causing intra-strand and inter-strand cross-links between DNA bases (CitationHartmann et al 1972). Compared with other alkylating agents, bendamustine causes more cross-links and importantly cross-linking seems to be more durable and more difficult to repair than those induced by carmustine and cyclophosphamide (CitationStrumberg et al 1996). Treatment with bendamustine also leads to disruption of the matrix function of DNA in DNA synthesis (CitationHesse et al 1981). The benzimidazole ring may be responsible for the purine analog activity of bendamustine (CitationStaib et al 1999), although this has not been proven definitely in vivo. It has been shown that bendamustine induces apoptosis in B-chronic lymphocytic leukemia cells (CitationSchwänen et al 2002). Very recently it has been demonstrated that bendamustine has a distinct mechanism of action unrelated to other alkylating agents by activation of DNA damage stress response and apoptosis, inhibition of mitotic checkpoints, and induction of mitotic catastrophe (CitationLeoni et al 2008). Compared with equitoxic concentrations of phosphoramide mustard and chlorambucil, the genes p21 (Cip1/Waf1) and Noxa which are responsible for apoptosis are induced much more strongly by bendamustine. Bendamustine also leads to a unique and marked phosphorylation of Ser15, which is one of the key events of p53-mediated apoptosis. It was shown also in SU-DHL-1 cells that bendamustine, but not phosphoramide or chlorambucil, causes an increase in the protein expression of Bax leading to p53 mediated apoptosis. Furthermore, bendamustine inhibits mitotic checkpoints and induces mitotic catastrophe by the inhibition of several mitosis-related genes like polo-like kinase 1, Aurora Kinase A, and Cyclin B1 (CitationLeoni et al 2008). After intravenous application bendamus-tine undergoes an extensive first-pass metabolism in the liver by cytochrome p450 (CitationPreiss et al 1985). A high percentage of the drug (>95%) is bound to protein, primarily albumin, but only free bendamustine is active (Haase et al 1991). Elimination is biphasic with a half-life of 6–10 minutes and a terminal half-life of approximately 30 minutes. Bendamustine is eliminated primarily by the renal route (CitationMatthias et al 1995). Interestingly it is not necessary to reduce the bendamustine dose in patients with impaired renal function. Bendamustine doses up to 120 mg/m2 on day 1 + 2 can be given safely even to patients on hemodialysis (W. Pönisch, pers comm and own unpublished observation).
Early clinical studies in East Germany
Until 1990 bendamustine was available only in East Germany, the former German Democratic Republic. There it was used for the treatment of different tumors. East German investigators showed that it has considerable cytotoxic activity in chronic lymphocytic leukemia (CLL) (CitationAnger et al 1975), Hodgkin’s disease (CitationHerold et al 1992), non-Hodgkin’s lymphoma (CitationRuffert et al 1989; CitationBrockmann 1992), multiple myeloma (CitationAnger et al 1967, Citation1969), and lung cancer (CitationAnger et al 1975).
Bendamustine monotherapy
Apart from case reports, only a few studies have been published that examined the efficacy of bendamustine as a monotherapy in relapsed indolent lymphomas. The first is the study by CitationHeider and Niederle (2001) who treated 58 patients in the relapsed situation with bendamustine 120 mg/m2 day 1 + 2 of a 3-week cycle. The treatment was repeated until complete remission (CR) or partial remission (PR) or stable disease (SD) was confirmed on two consecutive cycles. Fifty-two patients were evaluable for response and toxicity. They reported a CR of 11% and a PR of 62%. SD was seen in 10% and progressive disease (PD) in 17% of the patients. The median duration of remission was 16 months. The main toxicities were a reversible grade 1–4 hematotoxicity and a grade 1 or 2 gastrointestinal toxicity. The second study was reported by CitationBremer in 2002, who treated 102 relapsed patients with different indolent lymphomas (CLL: 15, immunocytic: 46, multiple myeloma: 25, others: 16). The bendamustine dose was 60 mg/m2, days 1–5 every 4–6 weeks. A median of 4 cycles (1–11) were applied. The main toxicity observed was a grade 3 or 4 hematotoxicity with anemia in 7%, thrombocytopenia in 12%, and leukocytopenia in 25% of the patients treated. Nonhematological toxicity grade 3 or 4 was seen in less than 5% of the patients. Grade 1 or 2 nausea and vomiting was reported in more than 20% of the patients (CitationBremer 2002). He reported an overall response rate (ORR) of CR + PR of 77% with 20% stable disease and only 4% of patients with progressive disease. Median duration of response in the patients with indolent lymphoma was 39 months (CitationBremer 2002). Recently, a study examined the efficacy of bendamustine in relapsed patients with rituximab-refractory disease and demonstrated an ORR of 84% (29% CR, 3% CR unconfirmed, and 53% PR) with a bendamustine dose of 120 mg/m2 on day 1 + 2 of a 3-week cycle for 6 cycles (CitationKahl et al 2007). This study was confirmed by another trial in patients with rituximab resistant disease, in which 20% of the patients had transformed indolent lymphomas (CitationFriedberg et al 2008). In this study, 76 patients were treated with a bendamustine dose of 120 mg/m2 on day 1 + 2 of a 3-week cycle for 6 cycles. The authors reported an ORR of 77% (15% CR, 19% unconfirmed CR, and 43% PR). The median duration of response was 6.7 months with 36% of the responses exceeding 1 year. In this study a grade 3 or 4 hematologic toxcicity included neutropenia (54%), throm-bocytopenia (25%), and anemia (12%).
Bendamustine in combination with other cytotoxic substances
Bendamustine has been combined with different cyto-toxic substances in the past. However, these studies are all small phase I/II studies with 14–82 patients each and no consistent response evaluation (). The combination with vincristine and prednisone was tested in 4 small trials with a total of 157 patients. The ORR ranged from 66% to 90% with a CR rate of 22%–45% and a PR rate of 41%–52% (CitationRuffert et al 1989; CitationBlumenstengel et al 1998; CitationHerold et al 1999; CitationKath et al 2000). Mitoxantrone was combined with bendamustine in one study showed an ORR of 59% (7% CR, 52% PR) (CitationHeck et al 1998). Another study combined mitoxantrone/methotrexate/prednisone with bendamustine in 23 patients and reported an ORR of 48% (13% CR, 35% PR) (CitationKahl et al 1997). In a small study 14 patients were treated with a combination of bendamustine/idarubicine/dexamethasone with a reported ORR of 79% (29% CR, 50% PR) (CitationKönig et al 1999). Bendamustine was also combined with oral etoposide in 38 patients with a high ORR of 97% (67% CR, 30% PR) (CitationRuffert 1999). Most extensively the combination of bendamustin/vincristine/prednisone has been studied by the OSHO group. In a phase III study the BOP regimen (bendamustine 60 mg/m2 days 1–5, vincristine 2 mg on day 1, and prednisolone 100 mg/m2 days 1–5) has been directly compared with the COP (cyclophosphamide, vincristine, and prednisone) regimen. No significant differences were seen for ORR, remission duration, and overall survival, although BOP caused less toxicity. BOP caused significantly less leukocytopenia (19% versus 34%) and alopecia (4% versus 48%) compared with COP (CitationHerold et al 2006).
Table 1 Bendamustine in combination with other cytotoxic substances
In vitro studies suggest that especially combinations of bendamustine with purine analogs could lead to a synergistic cytotoxicity (CitationChow et al 2001). So far only one phase I/II trial has been published by the OSHO group combining bendamustine with fludarabine. They treated 29 patients with relapsed indolent lymphomas with different dose levels and found a maximal tolerated dose of bendamustine 30 mg/m2 on days 1–3 and fludarabine 30 mg/m2 on days 1–3 when these drugs were combined. The reported ORR rate was 77% with 8 of 15 responders relapsing after a median time of 14 months. Unfortunately, a significant grade 3 or 4 hematotoxicity was observed, and 1 patient died of febrile neutropenia (CitationKönigsmann et al 2004).
Bendamustine in combination with rituximab
In 1999, we treated a patient with stage IV indolent lymphoma resistant to alkylating agents, anthracyclines, fludarabine, and rituximab with a combination of bendamustine plus mitoxantrone and rituximab (BMR) as fifth-line therapy. The disease went into CR after the first cycle and remains at CR until today (9+ years). This experience led to a small pilot study, which confirmed the efficacy of the BMR regimen in relapsed/refractory indolent lymphomas and B-cell chronic lymphocytic leukemia (B-CLL) (CitationWeide et al 1999). BMR was applied as follows: bendamustine 90 mg/m2 day 1 + 2, mitoxantrone 10 mg/m2 on day 1, and rituximab 375 mg/m2 on days 8, 15, 22, 29. BM was repeated on day 36 for 3–5 more cycles every 28 days (1 × BMR followed by 3–5 × BM). The pilot phase of BMR was continued and showed a consistent high anti-lymphoma activity with long lasting complete remissions (CitationWeide et al 2002). An ORR of 96% with 41% CR and 55% PR was observed. Importantly the time to next anti-lymphoma therapy was markedly prolonged and a significant proportion of the study population is still in ongoing CR up to more than 9 years after BMR. Interestingly, 46% of the patients received one cycle of BMR only, which means just 5 weeks of cytotoxic therapy, underscoring the potency of this chemoimmunotherapy (CitationWeide et al 2004). The experience of our single center pilot study led to a multicenter phase II trial, which confirmed the efficacy of BMR in rituximab pretreated, relapsed, or refractory indolent lymphomas or mantle cell lymphomas. BMR consisted of bendamustine 90 mg/m2 on day 1 + 2, mitoxantrone 10 mg/m2 on day 1, and rituximab 375 mg/m2 on day 8 every 4 weeks times 4 (4 × BMR). In this trial the ORR was 89% with 35% CR and 54% PR. The main toxicity of BMR was a reversible hematotoxicity grade 3 or 4 (10% anemia, 78% leukocytopenia, 46% granulocytopenia, 16% thrombocytopenia). However, hospitalizations due to therapy were necessary after 4% of BMR applications only (CitationWeide et al 2007). Due to the observed hematotoxicity in pretreated patients, we have reduced the mitoxantrone dose in clinical practice to 6 mg/m2 which results in a significant reduced hematotoxicity without reducing the activity of BMR (unpublished observation). Parallel to the development of BMR, CitationRummel et al (2002) developed the bendamustine-rituximab regimen (BR). In in vitro studies they could demonstrate in their cell line assay a synergistic cytotoxic effect when they applied bendamustine together with rituximab, leading to a markedly increased cell killing rate (CitationChow et al 2002; Rummel et al 2002). This led to a multicenter phase II trial in which they could demonstrate a high anti-lymphoma activity of BR in indolent lymphomas and mantle cell lymphomas with an ORR of 90% with a CR rate of 60%. Interestingly they found a remarkably low hematotoxicity grade 3 or 4 (16% leukocytopenia, 3% thrombocytopenia [CitationRummel et al 2005]). BR consisted of bendamustine 90 mg/m2 days 8 + 9, 36 + 37, 64 + 65, 92 + 93. Rituximab (375 mg/m2) was given on days 1, 7, 35, 63, 91, 120. These results have been confirmed by other groups (CitationRobinson et al 2005; CitationVan der Jagt et al 2006). In a subsequent randomized phase III study the STIL-group (Study Group Indolent Lymphoma, Germany) were able to demonstrate that 6 × BR (bendamustine 90 mg/m2 on day 1 + 2, rituximab 375mg/m2 on day 1) is equally effective concerning overall response rate compared with 6 × R-CHOP in the first-line therapy of indolent lymphomas and mantle cell lymphomas (CitationRummel et al 2007). Bendamustine has been combined with fludarabine and rituximab (BFR) in the treatment of relapsed indolent lymphomas. In this study bendamustine was applied at a dose of 50 mg/m2 on days 1–3, fludarabine at a dose of 25 mg/m2 days 1–3 and rituximab (375 mg/m2) was given on days 8, 15, 22, 29. The chemotherapy part (bendamustine plus fludarabine) was repeated on day 57 for 4 cycles. BFR proved to be effective with an ORR of 76% (28% CR, 48% PR) (CitationKirchner et al 2001). Unfortunately, the study could not be continued due to a significant hematotoxicity and a high rate of serious infections (Kirchner et al pers comm). The results of the studies combining bendamustine with rituximab in patients with relapsed or refractory indolent lymphomas are summarized in . Future directions of bendamustine development could be the sequential application of a chemoimmunotherapy with bendamustine (BMR or BR) followed by radioimmu-notherapy. We have treated so far 10 patients with relapsed or refractory indolent lymphoma and mantle cell lymphoma with 3 × BMR followed by 90Y-ibritumomab tiuxetan (ZEVALINTM) with a high response rate (6 CR, 3 PR, 1 PD) with durable complete remissions in 5 patients. The main toxicity was a reversible grade 3 or 4 hematotoxicity after ZEVALINTM. No blood or platelet transfusions or hospital admissions were necessary. No severe infections were observed (unpublished observation). Other directions could be the combination of bendamustine with bortezomib, thalidomide or revlimide, antiangiogenesis agents like bevacizumab, or new anti-B-cell-antibodies.
Table 2 Bendamustine in combination with rituximab
Conclusions
Bendamustine has enriched our armamentarium against relapsed indolent lymphomas remarkably due to its unique mechanism of action. Especially because of its activity in lymphomas resistant to alkylating agents, purine analogs, and rituximab, it opens up an opportunity for patients who are normally very difficult to treat. Of utmost importance are combinations of bendamustine with rituximab, which have shown to be highly active in achieving long lasting remissions Due to a positive toxicity profile these combinations are especially suitable for the treatment of elderly patients.
Disclosures
The author has declared no conflicts of interest.
References
- AngerGHessePKöhlerP1967Erste klinische Erfahrungen mit einem neuen ZytostatikumDeutsch Gesundheitswes22107984
- AngerGHessePBaufeldH1969Behandlung des multiplen Myeloms mit einem neuen ZytostatikumDtsch Med Wochenschr4824955004903552
- AngerGFinkRFleischerJ1975Vergleichsuntersuchungen zwischen Cytostasan und Cyclophosphamid bei der chronischen Lymphadenose, dem Plasmozytom, der Lymphogranulomatose und dem BronchialkarzinomDeutsch Gesundheitswes3012805
- ArmitageJ1993Treatment of non-Hodgkin’s lymphomaN Engl J Med3281023308450856
- BlumenstengelKFrickeHJKathR1998Bendamustine (B), vincristine (O), prednisone (P) in relapsed and refractory low grade non-Hodgkin’s lymphoma (NHL) [abstract]Ann Hematol77Suppl 11S149
- BremerK2002High rates of long lasting remissions after 5-day bendamustine chemotherapy cycles in pre-treated low-grade non-Hodgkin’s lymphomasJ Cancer Res Clin Oncol128603912458340
- BrockmannB1992Therapy of the recurrence of malignant lymphomaZ Aerztl Fortbild (Jena)86843
- ChowKUBoehrerSGeduldigK2001In vitro studies of apoptosis of neoplastic cells in low-grade non-Hodgkin’s lymphomas using combinations of established cytotoxic drugs with bendamustineHaematologica864859311410411
- ChowKUSommerladWDBoehrerS2002Anti-CD20 antibody (IDEC-C2B8, rituximab) enhances efficacy of cytotoxic drugs on neoplastic lymphocytes in vitro: role of cytokines, complement, and caspasesHaematologica87334311801463
- FriedbergJWCohenPChenL2008Bendamustine in patients with rituximab-refractory indolent and transformed non-Hodgkin’s lymphoma: results from a phase II multicenter, single agent studyJ Clin Oncol262041018182663
- HaaseDPreissRSohrR1990Untersuchungen zur Plasmaei-weißbindung von Bendamustin (Cytostasan) und AmbazoneZ Klin Med45126771
- HartmannMZimmerCH1972Investigation of cross-link formation in DNA by the alkylating cytostatica IMET 3106, 3393 and 3943Biochim Biophys Acta28738694629776
- HeckHKPreissJMSchmidtP1998Bendamustine (B) and mitoxantrone (M) in the treatment of low grade non-Hodgkin’s lymphoma (NHL) [abstract]J Cancer Res Clin Oncol124SupplR147
- HeiderANiederleN2001Efficacy and toxicity of bendamustine in patients with relapsed low – grade non-Hodgkin’s lymphomasAnticancer Drugs12725911593053
- HeroldMKeinertKAngerG1992Risk-adapted combined radio-therapy and chemotherapy for Hodgkin’s disease – results of a pilot studyOnkologie155015
- HeroldMSchulzeAMantovaniL1999BOP versus COP in advanced low-grade non-Hodgkin’s lymphoma – results of a randomized multicenter trial [abstract]Ann Oncol10Suppl 312510076735
- HeroldMSchulzeANiederwieserD2006Bendamustine, vincristine and prednisone (BOP) versus cyclophosphamide, vincristine and prednisone (COP) in advanced indolent non-Hodgkin’s lymphoma and mantle cell lymphoma: results of a randomised phase III trial (OSHO# 19)J Cancer Res Clin Oncol1321051216088404
- HesseGSchulzeWWachtelE1981Zur Methodik der Bestimmung alkylierender Aktivitäten von N-Losten mit Nitrobezylpyridin (NBP) in biologischem MaterialPharmazie36609127301901
- KahlCHeroldMHöffkesH1997Bendamustine, methotrexate, mitoxantrone and prednisone (BMMP) for the treatment of high grade non-Hodgkin’s lymphomaOnkologie204068
- KahlBBartlettNLLeonardJP2007Bendamustine is safe and effective in patients with rituximab-refractory, indolent B-cell non-Hodgkin’s lymphoma [abstract]Blood1101351
- KathRHöffkenKMerkleK2000Prevention of immunological complications in bendamustine treatment [abstract]Onkologie23171
- KirchnerHHGaedeBSteinhauerEU2001Chemoimmuno-therapy with Fludarabine, Bendamustine and Rituximab for relapsed low grade malignant non-Hodgkin’s lymphoma [abstract]Blood98568
- KönigUJunghassCDeckerS1999Response of refractory and relapsed low grade non-Hodgkin’s lymphoma and chronic lymphocytic leukemia to Dexa-BID, a bendamustine hydrochloride-containing regimen [abstract]Ann Oncol10Suppl 3132
- KönigsmannMKnaufWHeroldM2004Fludarabine and bendamustine in refractory and relapsed indolent lymphoma – a multicenter phase I/II trial of the east german society of hematology and oncology (OSHO)Leuk Lymphoma451821715223642
- LeoniLMBaileyBReifertJ2008Bendamustine (Treanda) displays a distinct pattern of cytotoxicity and unique mechanistic features compared with other alkylating agentsClin Cancer Res143091718172283
- MatthiasMPreissRSohrR1995Pharmacokinetics of bendamustine in patients with malignant tumors [abstract]Proc Am Soc Clin Oncol141476
- OzegowskiWKrebsD1963w-[bis-(chlorethyl)-amino-benzimidazolyl-(2)]-propionic or butyric acids as potential cytostatic agentsJ Prakt Chem2017886
- OzegowskiWKrebsD1971IMET 3393, gamma-(1-methyl-5-bis-(ß-chloräthyl)-amino-benzimidazolyl(2)-buttersäure-hydrochlorid, ein neues Zytostatikum aus der Reihe der Benzimidazol-LosteZbl Pharm110101319
- PreissRSohrRMatthiasM1985The pharmacokinetics of bendamustine (Cytostasan) in humansPharmazie4078244095129
- RobinsonKSWilliamsMECohenP2005Bendamustine HCl (TREANDATM) treatment in combination with rituximab results in objective responses in patients with refractory/relapsed indolent B-cell and mantle cell non-Hodgkin’s lymphoma: Results from phase II multicenter study (SDX-105–02) [abstract]Blood106923
- RuffertKJannHSyrbeG1989Cytostasan (bendamustine) as an alternative therapeutic approach to treat malignant non-Hodgkin’s lymphomaZ Klin Med446714
- RuffertK1999Therapy of low grade non-Hodgkin’s lymphoma (NHL) with bendamustine and oral etoposide [abstract]Ann Oncol10Suppl 312510076735
- RummelMJChowKUHölzerD2002In vitro studies with bendamustine: enhanced activity in combination with rituximabSemin Oncol294 Suppl 13121412170426
- RummelMJAl-BatranSEKimSZ2005Bendamustine plus rituximab is effective and has a favorable toxicity profile in the treatment of mantle cell and low – grade non Hodgkin’s lymphomaJ Clin Oncol233383915908650
- RummelMJvon GrünhagenUNiederleN2007Bendamustine plus rituximab versus CHOP plus rituximab in the first line treatment of patients with indolent and mantle cell lymphomas – first interim results of a randomized phase III study of the StiL (Study Group Indolent Lymphomas, Germany) [abstract]Blood110385
- SchnabelRJungstandWGutscheW1967Comparative studies on the cystostatic activity of the new nitrogen mustard derivative IMET 3393 and endoxan in three experimental mouse tumours (Ehrlich-ascites-carcinoma, sarcoma 180 solid, leukaemia LAJ 1)Acta Biol Med1953458
- SchwänenCHeckerTHübingerG2002In vitro evaluation of bendamustine induced apoptosis in B-chronic lymphocytic leukemiaLeukemia16209610512357363
- StaibPSchinkotheTDimskiT1999In vitro modulation of ara-CTP accumulation in fresh AML cells by bendamustine in comparison with fludarabine, 2-CDA and gemcitabine [abstract]Blood9463
- StrumbergDHarstrickADollK1996Bendamustine hydrochloride activity against doxorubicine-resistant human breast cancer cell linesAnticancer Drugs7415218826610
- Van der JagtRHCohenPChesonBD2006Phase II Results of bendamustine in combination with rituximab in relapsed indolent and mantle-cell non-Hodgkin’s lymphoma [abstract]Blood1082710
- WeideRHeymannsJKöpplerH1999Successful treatment of alkylating agent resistant low grade B-cell non Hodgkin’s lymphomas with bendamustine/mitoxantrone/rituximab (BMR) [abstract]Onkologie22Suppl 1644
- WeideRHeymannsJGoresA2002Bendamustine, mitoxantrone and rituximab (BMR): A new effective regimen for refractory or relapsed indolent lymphomasLeuk Lymphoma433273111999564
- WeideRPandorfAHeymannsJ2004Bendamustine/Mitoxantrone/ Rituximab (BMR): A very effective, well tolerated outpatient chemoimmunotherapy for relapsed and refractory CD20-positive indolent malignancies. Final results of a pilot studyLeuk Lymphoma452445244915621757
- WeideRHessGKöpplerH2007High anti – lymphoma activity of bendamustine/mitoxantrone/rituximab in rituximab pretreated relapsed or refractory indolent lymphomas and mantle cell lymphomas. A mul-ticenter phase II study of the German Low Grade Lymphoma Study Group (GLSG)Leuk Lymphoma48129930617613757