Abstract
Type 2 diabetes is widespread and its prevalence is increasing rapidly. In the US alone, approximately 41 million individuals have prediabetes, placing them at high risk for the development of diabetes. The pathogenesis of type 2 diabetes involves inadequate insulin secretion and resistance to the action of insulin. Suggestive data link insulin resistance and accompanying hyperglycemia to an excess of abdominal adipose tissue, a link that appears to be mediated partially by adipocyte secretion of multiple adipokines that mediate inflammation, thrombosis, atherogenesis, hypertension, and insulin resistance. The adipokine adiponectin has reduced expression in obesity and appears to be protective against the development of type 2 diabetes. Current recommendations to prevent type 2 diabetes center on lifestyle modifications, such as diet and exercise. Clinical trials have established the efficacy of lifestyle intervention, as well as pharmacologic interventions that target glycemic control or fat metabolism. However, diabetes did develop in a substantial percentage of individuals who received intensive intervention in these trials. Thus there is an unmet need for additional strategies in high-risk individuals. Recent data suggest thiazolidinediones and blockade of the endocannabinoid system represent novel therapeutic approaches that may be used for the prevention of diabetes.
Burden of diabetes
Type 2 diabetes is the most common metabolic disorder worldwide (CitationGoldstein 2003), and its prevalence is growing at an alarming rate in both developed and developing countries (CitationWild et al 2004; CitationYach et al 2006). This growth has been related to the increased prevalence of obesity (defined as body mass index [BMI] ≥30 kg/m2), a primary driver in the development of type 2 diabetes, as well as an independent health problem (CitationCenters for Disease Control and Prevention 2005; CitationDiabetes Research Working Group 1999; CitationYach et al 2006). Moreover, an estimated 41 million people in the US currently have prediabetes, defined as impaired fasting glucose (IFG) or impaired glucose tolerance (IGT). These individuals have a high risk for the development of diabetes (CitationCenters for Disease Control and Prevention 2006).
Type 2 diabetes is associated with considerable morbidity and mortality, which can lead to substantial personal and societal costs (CitationYach et al 2006). In 2002, in the US alone, direct and indirect costs attributable to diabetes were estimated at US$132 billion by the American Diabetes Association (ADA) (CitationHogan et al 2003). This estimate does not include many intangible costs, such as pain and suffering. Cardiovascular disease (CVD) is the leading cause of death among diabetics, and is responsible for much of the increase in diabetes-related morbidity and mortality. CVD-related mortality is 2–4 times higher among diabetics (CitationCenters for Disease Control and Prevention 2005). Atherosclerosis, hypertension, and stroke are common problems affecting individuals with diabetes, all of which correlate highly with the presence of obesity (CitationCenters for Disease Control and Prevention 2005; CitationGlendening et al 2005).
A cluster of interrelated cardiometabolic risk factors is closely related to the development of type 2 diabetes and cardiovascular disease. Current views suggest that cardiometabolic risk factors represent a continuum of disease risks – not merely the presence or absence of a distinct disease entity (CitationEckel et al 2006). Obesity, hyperglycemia and insulin resistance, dyslipidemia, inflammation, and hypertension represent interrelated therapeutic targets in the battle against the increasing prevalence of type 2 diabetes (CitationEckel et al 2006).
Obesity, insulin resistance, and progression to diabetes
The classification and pathogenesis of type 2 diabetes involves abnormalities of glucose and lipid metabolism, including inadequate insulin secretion from pancreatic β cells and resistance to the action of insulin (ADA 2006; CitationGoldstein 2003). There is epidemiologic and physiologic evidence linking insulin resistance and hyperglycemia (which precedes and characterizes the development of type 2 diabetes) to the presence of abdominal obesity (CitationDiabetes Research Working Group 1999; CitationSharma 2006). An association between intra-abdominal adipose tissue and insulin resistance has been demonstrated in animal models and in human subjects (CitationRaz et al 2005), and increased abdominal adipose tissue greatly increases the risk of developing IGT and insulin resistance in individuals with normal glucose tolerance at baseline (CitationHayashi et al 2003).
The underlying mechanisms involve the increased flux of free fatty acids (FFAs) to the liver, pancreas, and other tissues, and subsequent deposition of triglycerides (TG) (CitationLewis et al 2002; CitationRaz et al 2005). This process is related to excessive release by adipose tissue of assorted bioactive substances known as adipokines (CitationChandran et al 2003), the combined actions of which trigger a chronic inflammatory state that contributes to the development of insulin resistance (CitationXu et al 2003). Elevated circulating FFA levels cause tissues to become resistant to the action of insulin. Hyperinsulinemia results as a compensatory mechanism to maintain glucose tolerance under these conditions, a situation that can lead to pancreatic β cell damage and the development or worsening of glucose tolerance and diabetes (CitationLewis et al 2002; CitationZraika et al 2002; CitationGoldstein 2003; CitationHaber et al 2003; CitationRaz et al 2005). In addition to adverse pancreatic effects, the excess glucose and fat in the blood can lead to additional organ and vascular damage, which underlies much of the morbidity and mortality associated with diabetes (CitationDeedwania and Fonseca 2005; CitationCenters for Disease Control and Prevention 2006).
The mechanisms by which abdominal obesity contribute to cardiometabolic risk appear to involve the endocrine activity of adipose tissue (CitationKershaw and Flier 2004). Adipose tissue and specifically abdominal adipose cells secrete a number of cytokines and adipokines that can have deleterious cardiometabolic effects. These include effects on glucose control, lipid profile, increased thrombotic risk, and increased inflammatory state (CitationLewis et al 2002; CitationGoldstein 2003). Secreted substances include (but are not limited to) C-reactive protein (CRP), a marker of inflammation and cardiovascular risk (CitationBerg and Scherer 2005; CitationNatali et al 2006), and the inflammatory cytokines interleukin-6 (IL-6) and tumor necrosis factor-alpha (TNF-α) (CitationMatsuzawa 2006; CitationNatali et al 2006; CitationSharma 2006). These cytokines in turn induce expression of the adipocyte-derived secretory protein resistin, which has been implicated in induction of the inflammatory cascade that contributes to the development of insulin resistance (CitationLehrke et al 2004). Additional adipokines that play a role in cardiometabolic risk include the thrombotic and fibrinolytic factors plasminogen-activator inhibitor type 1 (PAI-1) and fibrinogen (CitationMatsuzawa 2006; CitationNatali et al 2006; CitationSharma 2006), and components of the renin-angiotensin system (RAS) that are involved in the pathogenesis of hypertension, endothelial dysfunction, and the development of insulin resistance (CitationReaven et al 1996; CitationCaglayan et al 2005; CitationSharma 2006).
Adiponectin, a serum protein synthesized exclusively by adipocytes, plays a role in cardiometabolic pathology (CitationScherer et al 1995; CitationHu et al 1996). This adipokine is a modulator of insulin sensitization, lipid metabolism, and inflammatory states (CitationChandran et al 2003; CitationKadowaki et al 2006; CitationMatsuzawa 2006). In contrast to many of the inflammatory adipokines related to atherogenesis, and induction of insulin resistance, adiponectin has reduced expression under conditions of abdominal obesity, type 2 diabetes, and insulin resistance (CitationWeyer et al 2001; CitationChandran et al 2003; CitationSchulze et al 2004; CitationSchulze et al 2005). Increased adiponectin levels are associated with lower hyperglycemia, dyslipidemia, and inflammation in diabetic individuals, and appear protective against the development of type 2 diabetes in individuals at risk (CitationLindsay et al 2002; CitationKrakoff et al 2003; CitationSpranger et al 2003). Low adiponectin levels are independently predictive of eventual type 2 diabetes even in apparently healthy (non-obese) individuals (CitationLindsay et al 2002; CitationSpranger et al 2003) and in patients with coronary artery disease and IFG (CitationKnobler et al 2006). Genetic variability is attributable to plasma adiponectin levels and may be an independent cardiovascular risk factor in diabetic individuals (CitationQi et al 2006). Although the mechanisms underlying the protective role of adiponectin are under investigation, several models have been proposed. These include adiponectin-mediated modification of the insulin receptor in skeletal muscle, leading to enhanced signaling; increased FFA oxidation in skeletal muscle and liver, leading to a decrease in FFA flux; and decreased vascular inflammation through adiponectin-mediated effects on monocyte adhesion and on vascular proliferation of smooth muscle cells (CitationChandran et al 2003). Abdominal obesity and resultant adipokine dysregulation may be potential therapeutic targets through lifestyle and/or pharmacologic approaches aimed at delaying or preventing the onset of type 2 diabetes in high-risk individuals.
Preventing the progression or onset of diabetes
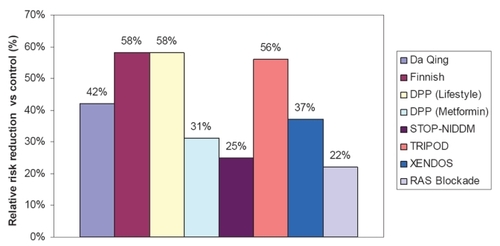
Prediabetes (or IGT) is a major risk factor for diabetes, as are obesity, physical inactivity, and insulin resistance. It is well established that the risk for development or progression of type 2 diabetes can be modified through lifestyle changes and/or pharmacotherapy. A number of well-designed clinical trials evaluating different strategies to prevent or delay type 2 diabetes have shown that lifestyle modifications and/or therapy with glucose-lowering agents used to treat this form of diabetes can significantly prevent or delay its onset in individuals with IGT, irrespective of obesity (CitationSherwin et al 2003; CitationKlein et al 2004). The results of major, randomized, controlled clinical studies on the prevention of type 2 diabetes are summarized in .
Figure 1 Summary of the relative risk reduction (%) of new-onset type 2 diabetes in randomized, controlled clinical trials of prevention. Studies shown are the Da Qing IGT and Diabetes Study, which evaluated diet and exercise (CitationPan et al 1997); the Finnish Diabetes Prevention Study, which evaluated diet and exercise (CitationTuomilehto et al 2001); the Diabetes Prevention Program (DPP) studies, which evaluated diet and exercise or metformin (CitationKnowler et al 2002); the Study To Prevent Non-Insulin-Dependent Diabetes Mellitus (STOP-NIDDM), which evaluated acarbose; Troglitazone in Prevention of Diabetes (TRIPOD), which evaluated Troglitazone; XENical in the Prevention of Diabetes in Obese Subjects (XENDOS), which evaluated the gastrointestinal lipase inhibitor orlistat (CitationTorgerson et al 2004); and a meta-analysis of 10 trials of RAS blockade with either ACE inhibitors or ARBs (CitationScheen 2004a). (See text for study details.)
Intensive lifestyle modification
The Da Qing IGT and Diabetes Study (CitationPan et al 1997) was an early long-term trial evaluating the impact of diet and/or exercise on the development of type 2 diabetes in more than 110,660 individuals with IGT. After 6 years, the cumulative incidence of diabetes was 68% in the control group, compared with 44% in the diet group, 41% in the exercise group, and 46% in the diet-plus-exercise group. The benefit of lifestyle modification was similar for the lean and overweight subgroups.
The Finnish study (CitationTuomilehto et al 2001) compared the impact of lifestyle modification involving intensive individualized diet counseling and increased physical activity (intervention group) with that of brief diet and exercise counseling (control group) in 522 obese males with IGT. After an average follow-up of 3.2 years, there was a 58% relative reduction in the incidence of diabetes in the intervention group compared with the control group. There was a clear correlation between diabetes risk reduction and the extent to which weight and activity goals were achieved. The impact of lifestyle intervention on insulin sensitivity and secretion, as measured using frequently sampled intravenous glucose tolerance testing, was evaluated after 4 years in a subset of these patients (CitationUusitupa et al 2003). There was a strong correlation between 4-year changes in insulin sensitivity and changes in weight. Insulin sensitivity improved by 64% among patients in the highest tertile of weight loss (a loss of −8% to −17%) and deteriorated by 24% among patients who gained weight (weight change of −1.4% to +10%). The acute insulin response declined significantly among patients in the control group (ie, no intensive lifestyle modification). Importantly, insulin secretion remained stable (ie, did not worsen) among patients with IGT at baseline who were able to lose weight.
Intensive lifestyle modification and/or pharmacologic intervention with glucose-lowering agents
The Diabetes Prevention Program (DPP) is one of the largest and most extensive ongoing clinical trials evaluating this issue (CitationKnowler et al 2002). Intensive nutrition and exercise counseling, metformin therapy, and placebo were compared among 3234 obese individuals with IGT in a randomized, controlled format. The latter 2 interventions were combined with standard diet and exercise recommendations. Following the 2.8-year follow-up, there was a 58% relative reduction in the progression to diabetes with lifestyle modification (compared with controls), and a 31% relative reduction in progression in the metformin group.
Pharmacologic intervention with glucose-lowering agents
Thiazolinedione (troglitazone) also has been evaluated as a preventive agent. The TRIPOD study monitored 236 Hispanic women with a history of previous gestational diabetes who were randomized to receive either troglitazone or placebo (CitationBuchanan et al 2002). After the median follow-up of 30 months, a 56% relative reduction in progression to diabetes in the troglitazone group was noted. Protection from diabetes was associated with a preservation of pancreatic β cell compensation for insulin resistance, as measured by acute insulin response to intravenous glucose administration and whole-body insulin sensitivity. The DPP group conducted a long-term comparison of treatment with metformin, troglitazone, placebo, or intensive lifestyle intervention in 2343 patients with IGT (CitationKnowler et al 2005). During the study, concerns arose over the potential liver toxicity of troglitazone, leading to discontinuation of this study arm and the withdrawal of troglitazone from clinical use. Prior to troglitazone discontinuation (mean time of 0.9 years), the incidence of diabetes was lower (3.0 cases per 100 person-years) than that observed for individuals receiving placebo, metformin, or intensive lifestyle intervention (12.0, 6.7, and 5.1 cases per 100 person-years, respectively). This lower incidence was statistically significant for the troglitazone-treated group versus both the placebo and metformin groups, but was not significant in comparison with lifestyle intervention (p < 0.001, p = 0.02, and p = 0.18, respectively). This protective effect observed in the troglitazone group persisted for 8 months after discontinuation of the study drug.
The Study To Prevent Non-Insulin-Dependent Diabetes Mellitus (STOP-NIDDM) was a randomized, placebo-controlled trial designed to evaluate the α-glucosidase inhibitor acarbose in the prevention or delay of type 2 diabetes in 1368 individuals with IGT (CitationChiasson et al 2002). All patients were instructed to follow a weight-reducing or maintaining diet and were encouraged to exercise regularly. After the mean follow-up period of 3.3 years, diabetes had developed in 32% of patients treated with acarbose and in 42% of placebo subjects, yielding a relative hazard rate of 0.75 with acarbose treatment (p = 0.0015). Acarbose also significantly increased reversion of IGT to normal glucose tolerance (p < 0.0001). This treatment generally was well tolerated; the most common adverse events that occurred during acarbose treatment were gastrointestinal effects such as flatulence and diarrhea.
The DREAM (Diabetes REduction Assessment with ramipril and rosiglitazone Medication) trial prospectively assessed whether treatment with the thiazolidinedione rosiglitazone could reduce the frequency of diabetes in 5269 individuals with IGT, IFG, or both (CitationGerstein et al 2006). All participants were given information on diet and lifestyle modifications to delay or prevent diabetes. After the median follow-up of 3 years, diabetes or death was the outcome for 11.6% of rosiglitazone recipients and 26.0% of placebo subjects (p < 0.0001). The incidence of regression to normoglycemia (defined as 2-hour and fasting plasma glucose concentrations of <7.8 mmol/L and <6.1 mmol/L, respectively) was significantly greater in the rosiglitazone group (p < 0.0001 vs placebo).
Pharmacologic intervention with lipase inhibitor
The XENical in the Prevention of Diabetes in Obese Subjects (XENDOS) trial was a 4-year, randomized, double-blind, placebo-controlled study conducted in 3,305 obese individuals to evaluate the efficacy of lifestyle changes in conjunction with either the gastrointestinal lipase inhibitor orlistat or placebo in preventing or delaying type 2 diabetes (CitationTorgerson et al 2004). Only 21% of patients had IGT at the time of study entry. After 4 years of treatment, a 37% reduction in the risk of developing diabetes was noted for the orlistat group (cumulative incidence: 6% and 9% with orlistat and placebo, respectively; p = 0.0032). This risk reduction was accompanied by a significantly greater mean weight loss in the orlistat group compared with placebo (5.8 vs 3.0 kg, respectively; p < 0.001). Further analysis suggested that the reduced risk of developing diabetes could be explained by an effect on the group with IGT at baseline.
Underlying mechanisms of prevention
A number of studies have identified mechanistic bases for the benefits of lifestyle and/or pharmacologic intervention in the delay or prevention of diabetes. As expected, the benefits appear to be mediated by effects on multiple potentially causative emerging risk factors related to inflammation, adipokine dysregulation, fibrinolysis, insulin resistance, and glucose metabolism. For example, lifestyle intervention in subjects participating in the Finnish Diabetes Prevention Study was associated with decreased expression of PAI-1 and fibrinogen, both mediators of fibrinolysis (CitationHamalainen et al 2005).
The thiazolidinediones troglitazone, rosiglitazone, and pioglitazone (CitationGhanim et al 2006; CitationSamaha et al 2006; CitationSzapary et al 2006) have early anti-inflammatory effects, which are associated with decreased lipolysis and FFA flux, improved insulin signaling and sensitization, increased adiponectin expression, and improved lipid profiles (eg, elevated high-density lipoprotein [HDL] cholesterol levels and favorable changes in lipoprotein particle size). These beneficial effects of thiazolidinediones on cardiometabolic risk factors have been observed in obese and non-obese patients with type 2 diabetes (CitationChiquette et al 2004; CitationGhanim et al 2006) and in nondiabetic patients with metabolic syndrome (CitationSamaha et al 2006; CitationSzapary et al 2006). This interrelationship of factors confirms the concept of metabolic risk being a continuum of disease processes and not merely the absence or presence of one or all of these cardiometabolic risk factors.
Renin-angiotensin blockade
Large randomized clinical trials have demonstrated that blockade of the RAS with angiotensin-converting enzyme (ACE) inhibition or angiotensin receptor blockers (ARBs) can reduce the incidence of new-onset type 2 diabetes. A recent meta-analysis of 10 randomized clinical trials involving more than 76,000 patients assessed the potential prevention of diabetes through RAS blockade (CitationScheen 2004a), including 5 trials of ACE inhibitors (enalapril, lisinopril, captopril, and ramipril) and 4 of ARBs (losartan, candesartan, and valsartan). Among all these trials, new cases of type 2 diabetes were found in 7.4% of patients treated with an ACE inhibitor or ARB, compared with 9.6% of control patients. This corresponded to a 22% relative risk reduction of developing type 2 diabetes (p < 0.00001). Despite these positive findings on the preventive effects of ACE inhibitors, it was recently reported that ramipril (included as a treatment arm in the DREAM study) failed to reduce the incidence of the primary outcome (diabetes or death) among participants with IFG or IGT over the median 3-year treatment period (CitationBosch et al 2006). However, individuals receiving ramipril in this study were more likely to have normal fasting glucose levels or glucose tolerance at study endpoint than those receiving placebo. This suggests that the study may not have had adequate power to discern a difference; a longer or larger study might be required for detecting an effect of the ACE inhibitor on the incidence of diabetes.
The mechanisms involved in the actions of ACE inhibitors and ARBs in diabetes prevention are not fully understood. The multiple physiologic actions of angiotensin II may in part explain this complexity (CitationDeedwania and Fonseca 2005). It is likely that the beneficial actions of RAS blockade involve improvement in both insulin sensitivity and insulin secretion through the impact of multiple mediators on insulin action and receptor signaling, muscle pancreatic islet blood flow, sympathetic nervous activity, adipokine production, and lipid metabolism (CitationScheen 2004b). For example, it was recently shown that losartan improves insulin sensitivity by increasing adiponectin production and decreasing TNF-α production (CitationPark et al 2006). There is also evidence that elevated angiotensin II produced by large insulin-resistant adipocytes may inhibit the recruitment of pre-adipocytes, resulting in increased lipid storage in muscle and decreased insulin sensitivity (CitationSharma et al 2002).
Impact of dietary choice
Both large randomized trials (The Finnish and DPP studies) and many smaller ones have demonstrated a significant impact of intensive lifestyle modification using conventional dietary recommendations for overweight or obese persons at risk for the development of diabetes; such diets are low in saturated fats and total fat intake, and rich in complex carbohydrates (CitationKnowler et al 2002; CitationTuomilehto et al 2001; CitationKlein et al 2004). However, there has been growing interest in low-carbohydrate diets as therapy for obesity. Overall, recent prospective trials indicate similar weight-loss efficacy over the long term with low-fat and carbohydrate-restricted diets (CitationSamaha 2005). The combined results of 5 recent randomized controlled trials indicate that subjects receiving a low-carbohydrate, high-fat diet achieved greater short- but not long-term weight loss than those receiving a conventional diet (CitationKlein et al 2004). However, some data suggest that high-fat diets, while having similar effects on weight, may have more favorable effects on lipid profile and glycemic status in obese patients. In a 6-month study in 79 severely obese patients with a high prevalence of metabolic syndrome or diabetes, a carbohydrate-restricted diet was associated with relative improvement in insulin sensitivity and TG levels compared with a low-fat diet (CitationSamaha et al 2003). A carbohydrate-restricted diet also was associated with more favorable effects on lipoprotein subfractions and on inflammation as measured by CRP levels in these patients (CitationSeshadri et al 2004). In a 1-year follow-up of the latter study, weight loss was still similar for the 2 groups, and effects on atherogenic dyslipidemia and glycemia had remained more favorable in the group on a low-carbohydrate diet (CitationStern et al 2004). Although these findings are compelling, outcomes studies evaluating the impact of carbohydrate-restricted diet on diabetes development and other cardiovascular outcomes are needed before recommendations regarding such a diet are warranted.
Drugs with potential application to prevention
Pharmacologic intervention enhancing incretin action
The incretin hormone glucagon-like peptide-1 (GLP-1) has demonstrated a variety of antidiabetic effects, including stimulation of insulin secretion, inhibition of glucagon secretion, delay of gastric emptying, suppression of appetite, promotion of β cell proliferation, and inhibition of β cell apoptosis (CitationDrucker 2006). Native GLP-1 has limited clinical use because it is rapidly inactivated by the enzyme dipeptidyl peptidase-4 (DPP-4), resulting in a half-life of <2 minutes. To overcome this obstacle, GLP-1 analogues have been developed with low affinity for DPP-4 as well as inhibitors of DPP-4. The GLP-1 mimetic exenatide and the DPP-4 inhibitor sitagliptin are now available for clinical use. Preclinical evidence suggests that exenatide may delay onset or prevent development of diabetes (CitationWang and Brubaker 2002; CitationStoffers et al 2003), although these findings need confirmation in clinical studies.
Exenatide has demonstrated efficacy in randomized controlled studies when used as adjunct therapy in patients with type 2 diabetes and inadequate glycemic control while receiving metformin (n = 336) (CitationDeFronzo et al 2005), a sulfonylurea (n = 377) (CitationBuse et al 2004), or metformin/sulfonylurea (n = 733) (CitationKendall et al 2005). The recommended dosages are 5 or 10 µg subcutaneously, twice daily. In addition to improving glycemic control, treatment with exenatide for 30 weeks reduced body weight by 0.9–1.6 kg with the lower dose and by 1.6–2.8 kg with the higher dose, compared with reductions of 0.3–0.9 kg in placebo recipients (CitationBuse et al 2004; CitationDeFronzo et al 2005; CitationKendall et al 2005). In each study, dose-related nausea was the most common adverse event in exenatide-treated patients (low dose, 36%–39%; high dose, 45%–51%). No correlation between change in body weight and nausea was observed in any of the studies.
Sitagliptin was recently approved as monotherapy, or in combination with metformin or a peroxisome proliferator-activated receptor gamma agonist, to improve glycemic control in patients with type 2 diabetes. The recommended oral dosage of sitagliptin is 100 mg once daily, with dosage adjustments required for patients with moderate or severe end-stage renal disease. Pharmacokinetic studies support once-daily dosing and show a lack of interaction between sitagliptin and metformin (CitationBergman et al 2006; CitationHerman et al 2005, Citation2006). Based on prescribing information, treatment with sitagliptin improves glycemic control (CitationJanuvia™ prescribing information 2006). No significant effects on body weight were reported, although the duration of treatment (up to 24 weeks) was shorter than that for exenatide. The most common adverse events were nasopharyngitis (5%) in patients receiving sitagliptin alone, and upper respiratory tract infection (6%) and headache (5%) in patients receiving sitagliptin/pioglitazone (CitationJanuvia™ prescribing information 2006).
Pharmacologic intervention inhibiting serotonin and norepinephrine reuptake
Numerous clinical studies have been conducted with the serotonin and norepinephrine reuptake inhibitor sibutramine, which is thought to induce weight loss by increasing satiety and possibly energy expenditure (CitationPoston and Foreyt 2004). Sibutramine is indicated for the management of obesity in conjunction with a reduced-calorie diet. It is administered orally at dosages of 5–15 mg once daily. The effects of sibutramine on body weight are well established, as described below. However, no study has assessed whether this agent can delay or prevent the development of type 2 diabetes.
In a large systematic review involving 29 randomized controlled trials of obese patients who were healthy (n = 3604) or who had type 2 diabetes (n = 654), hyperlipidemia (n = 341), hypertension (n = 340), or obstructive sleep apnea (n = 40), sibutramine 10–20 mg/day was associated with a placebo-subtracted mean weight loss of 2.8 kg in 8- to 12-week studies, 5.16 kg in 16- to 24-week studies, and 4.5 kg in 44- to 54-week studies (CitationArterburn et al 2004). No dose-response was observed. Body-weight reductions were consistent across the different study populations. A recent meta-analysis of 8 randomized, double-blind, placebo-controlled trials, which was restricted to obese patients with type 2 diabetes (n = 1093), yielded similar benefits with regard to body-weight reductions (CitationVettor et al 2005). In both analyses, cardiovascular and metabolic findings were more modest and included increases in heart rate and blood pressure, improvements in triglyceride and HDL cholesterol levels and, among patients with type 2 diabetes, improvements in glycemic control (CitationArterburn et al 2004; CitationVettor et al 2005). The cardiovascular effects of sibutramine necessitate monitoring of blood pressure and heart rate prior to initiating therapy and at regular intervals during therapy; sibutramine should not be used in patients with a history of coronary artery disease, congestive heart failure, arrhythmias, or stroke (Meridia® prescribing information 2006).
Blockade of the endocannabinoid (EC) system
Blockade of the EC system represents a novel therapeutic modality that targets intra-abdominal obesity, glycemic regulation, and related cardiometabolic risk factors. Animal studies have shown that this system plays a role in energy intake and homeostasis as well as excessive food intake (CitationDe Petrocellis et al 2004; CitationDi Marzo et al 2004). The EC system is overactivated in obesity (CitationDi Marzo et al 2001), and there is growing evidence that its activity may impact a number of cardiometabolic parameters associated with obesity (CitationDespres et al 2006; CitationJohn et al 2006).
Promising preclinical findings have led to the development of selective CB1 antagonists for clinical use. Several are currently in development, with one (rimonabant) now in Phase III testing (CitationAntel et al 2006). The efficacy and safety of CB1 blockade have been investigated in patients with obesity, with or without co-morbidities, in a clinical development program (Rimonabant in Obesity; RIO) (CitationLebovitz et al 2006) involving 4 large trials; the results of 3 trials have been published in full (CitationDespres et al 2005; CitationVan Gaal et al 2005; CitationPi-Sunyer et al 2006; CitationScheen et al 2006).
Treatment with rimonabant 20 mg for 1 year induced a consistent reduction in waist circumference and weight in all 4 trials (CitationDespres et al 2005; CitationVan Gaal et al 2005; CitationPi-Sunyer et al 2006; CitationScheen et al 2006). Improvements in HDL and TG levels also were observed and, as in the animal studies, much of this effect (approximately 50%) was not attributable to the weight decrease. These benefits were maintained throughout the second year of follow-up.
The potential benefit of rimonabant therapy on glycemic and other cardiometabolic parameters has been investigated in RIO-Diabetes (CitationScheen et al 2006), which involved 1045 patients with type 2 diabetes. In addition to the significant reduction in weight and waist circumference observed in all RIO studies, rimonabant 20 mg/day for 1 year produced a 0.7% reduction in hemoglobin A1c (HbA1C) versus placebo, with 43% of patients achieving HbA1C levels below 6.5%. Again, much of this effect was independent of weight change. Consistent with the other RIO trials, improvements from baseline in cardiometabolic parameters also were noted, including beneficial effects on HDL cholesterol and TG.
To explore the association between abdominal obesity and the development of diabetes, pooled data from RIO-Europe, RIO-North America, and RIO-Lipids were used to assess the effects of rimonabant on the development of diabetes in obese individuals who were classified with prediabetes at study enrolment (CitationRosenstock 2005). Prediabetes, or IFG, was defined as fasting glucose levels >5.6 mmol/L (100 mg/dL) and <7 mmol/L (126 mg/dL). This analysis involved 1290 patients participating in the 3 studies. Significant reductions were observed for fasting insulin levels (−2.7 MIU/mL; p < 0.001 vs placebo) and for homeostasis model assessment of insulin resistance (HOMA-IR) (−0.8%; p = 0.002 vs placebo). A trend toward halting or delaying the progression of IFG was suggested by the greater percentage of patients whose fasting glucose level became normal (46% vs 39% for rimonabant 20 mg vs placebo, respectively). In addition, a smaller percentage of rimonabant recipients progressed to type 2 diabetes (3.6% vs 4.9% for rimonabant 20 mg vs placebo, respectively); however, statistical analyses of these comparisons were not provided. The potential of rimonabant to delay or prevent the onset of type 2 diabetes is undergoing more extensive study in a clinical trial of patients with prediabetes (CitationUS National Institutes of Health 2006).
Conclusion
Although lifestyle intervention has proven successful in clinical trials, there are barriers to its long-term success for many individuals, such as cost, communication with healthcare providers, and the difficulty in maintaining substantial lifestyle changes long term (CitationVijan et al 2005). In the DPP studies, 49% and 74% of lifestyle participants met their weight loss and activity goals, respectively, at the end of 6 months; however, the success rates declined to 37% and 67%, respectively, over the 3.2-year follow-up period (CitationWing et al 2004). Despite the reduced risk that accompanies even modest weight loss (eg, 5% of body weight) (CitationKlein et al 2004), diabetes developed in a substantial number of patients with active intervention in the randomized clinical trials (). There is a current medical need for additional preventive intervention strategies in overweight and obese patients, particularly those at high risk for the development of type 2 diabetes.
Current guidelines do not advocate specific preventive pharmacologic therapy for prediabetes, although aggressive therapy for patients with cardiovascular risk factors (eg, hypertension) is recommended and has been beneficial in preventing type 2 diabetes in these patients. More aggressive preventive therapy, the adoption of novel therapeutic approaches, and possibly modification of current treatment guidelines in patients at high risk should be considered as strategies to reduce the growing burden of type 2 diabetes.
Acknowledgements
Funding for editorial support was provided by Sanofi-Aventis US.
References
- American Diabetes AssociationStandards of medical care in diabetes- – 2006Diabetes Care200629Suppl 1S442
- AntelJGregoryPCNordheimUCB1 cannabinoid receptor antagonists for treatment of obesity and prevention of comorbid metabolic disordersJ Med Chem20064940081616821760
- ArterburnDECranePKVeenstraDLThe efficacy and safety of sibutramine for weight loss: a systematic reviewArch Intern Med2004164994100315136309
- BergAHSchererPEAdipose tissue, inflammation, and cardiovascular diseaseCirc Res2005969394915890981
- BergmanAJStevensCZhouYPharmacokinetic and pharmacodynamic properties of multiple oral doses of sitagliptin, a dipeptidyl peptidase-IV inhibitor: a double-blind, randomized, placebo-controlled study in healthy male volunteersClin Ther200628557216490580
- BoschJYusufSGersteinHCEffect of ramipril on the incidence of diabetesN Engl J Med200635515516216980380
- BuchananTAXiangAHPetersRKPreservation of pancreatic beta-cell function and prevention of type 2 diabetes by pharmacological treatment of insulin resistance in high-risk hispanic womenDiabetes200251279680312196473
- BuseJBHenryRRHanJEffects of exenatide (exendin-4) on glycemic control over 30 weeks in sulfonylurea-treated patients with type 2 diabetesDiabetes Care20042726283515504997
- CaglayanEBlaschkeFTakataYMetabolic syndrome-interdependence of the cardiovascular and metabolic pathwaysCurr Opin Pharmacol200551354215780821
- Centers for Disease Control and PreventionNational diabetes fact sheet: general information and national estimates on diabetes in the United States, 20052005Atlanta, GAU.S. Department of Health and Human Services, Centers for Disease Control and Prevention
- Centers for Disease Control and PreventionDiabetes: Disabling, deadly, and on the rise2006U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, Coordinating Center for Health Promotion
- ChandranMPhillipsSACiaraldiTAdiponectin: more than just another fat cell hormone?Diabetes Care20032624425012882876
- ChiassonJLJosseRGGomisRAcarbose for prevention of type 2 diabetes mellitus: the STOP-NIDDM randomised trialLancet20023592072712086760
- ChiquetteERamirezGDefronzoRA meta-analysis comparing the effect of thiazolidinediones on cardiovascular risk factorsArch Intern Med2004164209710415505122
- De PetrocellisLCascioMGDiMVThe endocannabinoid system: a general view and latest additionsBr J Pharmacol20041417657414744801
- DeedwaniaPCFonsecaVADiabetes, prediabetes, and cardiovascular risk: shifting the paradigmAm J Med20051189394716164876
- DeFronzoRARatnerREHanJEffects of exenatide (exendin-4) on glycemic control and weight over 30 weeks in metformin-treated patients with type 2 diabetesDiabetes Care200528109210015855572
- DespresJPGolayASjostromLEffects of rimonabant on metabolic risk factors in overweight patients with dyslipidemiaN Engl J Med200535321213416291982
- DespresJPLemieuxIAlmerasNContribution of CB1 blockade to the management of high-risk abdominal obesityInt J Obes (Lond)200630Suppl 1S44S5216570106
- Di MarzoVBifulcoMDe PetrocellisLThe endocannabinoid system and its therapeutic exploitationNat Rev Drug Discov200437718415340387
- Di MarzoVGoparajuSKWangLLeptin-regulated endocannabinoids are involved in maintaining food intakeNature2001410822511298451
- Diabetes Research Working GroupConquering diabetes. A strategic plan for the 21st century1999NIH Publication No. 99–4398. National Institutes of Health
- DruckerDJThe biology of incretin hormonesCell Metab200631536516517403
- EckelRHKahnRRobertsonRMPreventing cardiovascular disease and diabetes: a call to action from the American Diabetes Association and the American Heart AssociationCirculation20061132943616801475
- GersteinHCYusufSBoschJEffect of rosiglitazone on the frequency of diabetes in patients with impaired glucose tolerance or impaired fasting glucose: a randomised controlled trialLancet2006368109610516997664
- GhanimHDhindsaSAljadaALow-dose rosiglitazone exerts an antiinflammatory effect with an increase in adiponectin independently of free fatty acid fall and insulin sensitization in obese type 2 diabeticsJ Clin Endocrinol Metab2006913553816804037
- GlendeningPNHearneSASegalLMF as in fat: How obesity policies are failing in America. Trust for America’s Health2005 Available at: http://healthyamericans.org/reports/obesity2005/Obesity2005Report.pdf
- GoldsteinBJInsulin resistance: from benign to type 2 diabetes mellitusRev Cardiovasc Med20034Suppl 6S31014668698
- HaberEPXimenesHMProcopioJPleiotropic effects of fatty acids on pancreatic beta-cellsJ Cell Physiol200319411212447984
- HamalainenHRonnemaaTVirtanenAImproved fibrinolysis by an intensive lifestyle intervention in subjects with impaired glucose tolerance. The Finnish Diabetes Prevention StudyDiabetologia20054822485316205886
- HayashiTBoykoEJLeonettiDLVisceral adiposity and the risk of impaired glucose tolerance: a prospective study among Japanese AmericansDiabetes Care200326650512610016
- HermanGABergmanAYiBTolerability and pharmacokinetics of metformin and the dipeptidyl peptidase-4 inhibitor sitagliptin when co-administered in patients with type 2 diabetesCurr Med Res Opin20062219394717022853
- HermanGAStevensCVan DyckKPharmacokinetics and pharmacodynamics of sitagliptin, an inhibitor of dipeptidyl peptidase IV, in healthy subjects: results from two randomized, double-blind, placebo-controlled studies with single oral dosesClin Pharmacol Ther2005786758816338283
- HoganPDallTNikolovPEconomic costs of diabetes in the US in 2002Diabetes Care2003269173212610059
- HuELiangPSpiegelmanBMAdipoQ is a novel adipose-specific gene dysregulated in obesityJ Biol Chem1996271106977038631877
- Januvia™Januvia™ (sitagliptin) prescribing information. Merck & Co. Inc [online]2006 URL: http://www.merck.com/product/usa/pi_circulars/j/januvia/januvia_pi.pdf
- JohnBJIrukullaSAbulafiAMSystematic review: adipose tissue, obesity and gastrointestinal diseasesAliment Pharmacol Ther20062315112316696799
- KadowakiTYamauchiTKubotaNAdiponectin and adiponectin receptors in insulin resistance, diabetes, and the metabolic syndromeJ Clin Invest200611617849216823476
- KendallDMRiddleMCRosenstockJEffects of exenatide (exendin-4) on glycemic control over 30 weeks in patients with type 2 diabetes treated with metformin and a sulfonylureaDiabetes Care20052810839115855571
- KershawEEFlierJSAdipose tissue as an endocrine organJ Clin Endocrinol Metab20048925485615181022
- KleinSSheardNFPi-SunyerXWeight management through lifestyle modification for the prevention and management of type 2 diabetes: rationale and strategies: a statement of the American Diabetes Association, the North American Association for the Study of Obesity, and the American Society for Clinical NutritionDiabetes Care20042720677315277443
- KnoblerHBenderlyMBoykoVAdiponectin and the development of diabetes in patients with coronary artery disease and impaired fasting glucoseEur J Endocrinol2006154879216381996
- KnowlerWCBarrett-ConnorEFowlerSEReduction in the incidence of type 2 diabetes with lifestyle intervention or metforminN Engl J Med200234639340311832527
- KnowlerWCHammanRFEdelsteinSLPrevention of type 2 diabetes with troglitazone in the Diabetes Prevention ProgramDiabetes2005541150615793255
- KrakoffJFunahashiTStehouwerCDInflammatory markers, adiponectin, and risk of type 2 diabetes in the Pima IndianDiabetes Care20032617455112766104
- LebovitzHEAustinMMBlondeLACE/AACE consensus conference on the implementation of outpatient management of diabetes mellitus: consensus conference recommendationsEndocr Pract200612Suppl 161216627372
- LehrkeMReillyMPMillingtonSCAn inflammatory cascade leading to hyperresistinemia in humansPLoS Med200411618
- LewisGFCarpentierAAdeliKDisordered fat storage and mobilization in the pathogenesis of insulin resistance and type 2 diabetesEndocr Rev2002232012911943743
- LindsayRSFunahashiTHansonRLAdiponectin and development of type 2 diabetes in the Pima Indian populationLancet200236057812114044
- MatsuzawaYTherapy Insight: adipocytokines in metabolic syndrome and related cardiovascular diseaseNat Clin Pract Cardiovasc Med20063354216391616
- Meridia®Meridia® (sibutramine hydrochloride monohydrate) prescribing information. Abbott Laboratories [online]2006 URL: http://rxabbott.com/pdf/meridia.pdf
- NataliAToschiEBaldewegSClustering of insulin resistance with vascular dysfunction and low-grade inflammation in type 2 diabetesDiabetes20065511334016567539
- PanXRLiGWHuYHEffects of diet and exercise in preventing NIDDM in people with impaired glucose tolerance. The Da Qing IGT and Diabetes StudyDiabetes Care199720537449096977
- ParkHHasegawaGObayashiHRelationship between insulin resistance and inflammatory markers and anti-inflammatory effect of losartan in patients with type 2 diabetes and hypertensionClin Chim Acta20063741293416857181
- Pi-SunyerFXAronneLJHeshmatiHMEffect of rimonabant, a cannabinoid-1 receptor blocker, on weight and cardiometabolic risk factors in overweight or obese patients: RIO-North America: a randomized controlled trialJAMA20062957617516478899
- PostonWSForeytJPSibutramine and the management of obesityExpert Opin Pharmacother200456334215013931
- QiLDoriaAMansonJEAdiponectin genetic variability, plasma adiponectin, and cardiovascular risk in patients with type 2 diabetesDiabetes2006551512616644713
- RazIEldorRCerneaSDiabetes: insulin resistance and derangements in lipid metabolism. Cure through intervention in fat transport and storageDiabetes Metab Res Rev20052131415386813
- ReavenGMLithellHLandsbergLHypertension and associated metabolic abnormalities--the role of insulin resistance and the sympathoadrenal systemN Engl J Med1996334374818538710
- RosenstockJThe potential of rimonabant in prediabetes: Pooled 1-year results from the RIO-Lipids, RIO-Europe and RIO-North American studies [abstract]2005Presented at the 65th Annual Meeting of the American Diabetes Association Abstract 13-LB
- SamahaFFEffect of very high-fat diets on body weight, lipoproteins, and glycemic status in the obeseCurr Atheroscler Rep200574122016255998
- SamahaFFIqbalNSeshadriPA low-carbohydrate as compared with a low-fat diet in severe obesityN Engl J Med200334820748112761364
- SamahaFFSzaparyPOIqbalNEffects of rosiglitazone on lipids, adipokines, and inflammatory markers in nondiabetic patients with low high-density lipoprotein cholesterol and metabolic syndromeArterioscler Thromb Vasc Biol2006266243016357312
- ScheenAFinerNHollanderPRimonabant improves cardiometabolic risk factors in overweight/obese patients with type 2 diabetes irrespective of background oral antidiabetic therapy (metformin or sulfonylureas) [abstract]Diabetes200655Suppl 1A1334 Abstract 560-P
- ScheenAJRenin-angiotensin system inhibition prevents type 2 diabetes mellitus. Part 1. A meta-analysis of randomised clinical trialsDiabetes Metab2004a304879615671918
- ScheenAJRenin-angiotensin system inhibition prevents type 2 diabetes mellitus. Part 2. Overview of physiological and biochemical mechanismsDiabetes Metab2004b3049850515671919
- SchererPEWilliamsSFoglianoMA novel serum protein similar to C1q, produced exclusively in adipocytesJ Biol Chem19952702674697592907
- SchulzeMBRimmEBShaiIRelationship between adiponectin and glycemic control, blood lipids, and inflammatory markers in men with type 2 diabetesDiabetes Care2004271680715220246
- SchulzeMBShaiIRimmEBAdiponectin and future coronary heart disease events among men with type 2 diabetesDiabetes200554534915677512
- SeshadriPIqbalNSternLA randomized study comparing the effects of a low-carbohydrate diet and a conventional diet on lipoprotein subfractions and C-reactive protein levels in patients with severe obesityAm J Med200411739840515380496
- SharmaAMThe obese patient with diabetes mellitus: from research targets to treatment optionsAm J Med2006119S172316563943
- SharmaAMJankeJGorzelniakKAngiotensin blockade prevents type 2 diabetes by formation of fat cellsHypertension2002406091112411451
- SherwinRSAndersonRMBuseJBThe prevention or delay of type 2 diabetesDiabetes Care200326Suppl 1S62912502620
- SprangerJKrokeAMohligMAdiponectin and protection against type 2 diabetes mellitusLancet2003361226812547549
- SternLIqbalNSeshadriPThe effects of low-carbohydrate versus conventional weight loss diets in severely obese adults: one-year follow-up of a randomized trialAnn Intern Med20041407788515148064
- StoffersDADesaiBMDeLeonDDNeonatal exendin-4 prevents the development of diabetes in the intrauterine growth retarded ratDiabetes2003527344012606515
- SzaparyPOBloedonLTSamahaFFEffects of pioglitazone on lipoproteins, inflammatory markers, and adipokines in nondiabetic patients with metabolic syndromeArterioscler Thromb Vasc Biol200626182816284192
- TorgersonJSHauptmanJBoldrinMNXENical in the prevention of diabetes in obese subjects (XENDOS) study: a randomized study of orlistat as an adjunct to lifestyle changes for the prevention of type 2 diabetes in obese patientsDiabetes Care2004271556114693982
- TuomilehtoJLindstromJErikssonJGPrevention of type 2 diabetes mellitus by changes in lifestyle among subjects with impaired glucose toleranceN Engl J Med200134413435011333990
- US National Institutes of HealthClinicalTrials.gov. 2006. [online] Accessed 17 October 2006. URL: http://www.clinicaltrials.gov/ct/show/NCT00325650;jsessionid=DE34C9537828718F3BB395432F702959?order=4
- UusitupaMLindiVLouherantaALong-term improvement in insulin sensitivity by changing lifestyles of people with impaired glucose tolerance: 4-year results from the Finnish Diabetes Prevention StudyDiabetes2003522532814514637
- Van GaalLFRissanenAMScheenAJEffects of the cannabinoid-1 receptor blocker rimonabant on weight reduction and cardiovascular risk factors in overweight patients: 1-year experience from the RIO-Europe studyLancet200536513899715836887
- VettorRSerraRFabrisREffect of sibutramine on weight management and metabolic control in type 2 diabetes: a meta-analysis of clinical studiesDiabetes Care200528942915793204
- VijanSStuartNSFitzgeraldJTBarriers to following dietary recommendations in Type 2 diabetesDiabet Med20052232815606688
- WangQBrubakerPLGlucagon-like peptide-1 treatment delays the onset of diabetes in 8 week-old db/db miceDiabetologia20024512637312242459
- WeyerCFunahashiTTanakaSHypoadiponectinemia in obesity and type 2 diabetes: close association with insulin resistance and hyperinsulinemiaJ Clin Endocrinol Metab2001861930511344187
- WildSRoglicGGreenAGlobal prevalence of diabetes: estimates for the year 2000 and projections for 2030Diabetes Care20042710475315111519
- WingRRHammanRFBrayGAAchieving weight and activity goals among diabetes prevention program lifestyle participantsObes Res20041214263415483207
- XuHBarnesGTYangQChronic inflammation in fat plays a crucial role in the development of obesity-related insulin resistanceJ Clin Invest200311218213014679177
- YachDStucklerDBrownellKDEpidemiologic and economic consequences of the global epidemics of obesity and diabetesNat Med20061262616397571
- ZraikaSDunlopMProiettoJEffects of free fatty acids on insulin secretion in obesityObes Rev200231031212120417