Abstract
This retrospective database analysis compared the effectiveness of dihydropyridine calcium channel blockers (DHPs), angiotensin-converting enzyme (ACE) inhibitors, and angiotensin receptor blockers (ARBs) added to diuretics or β-blockers. Adults with hypertension treated with diuretic or β-blocker monotherapy between 1998 and 2001 were identified from a large US electronic medical records database of primary care practices. Patients were required to have a baseline blood pressure (BP) ≥140/90 mmHg (≥130/80 mmHg for diabetes mellitus) and recorded BP measurements within 6 months before and 1–12 months following index date. Patients were matched 1:1:1 by propensity score to correct for differences in baseline characteristics. 1875 patients met study criteria and 660 (220 in each cohort) were matched based on propensity scores. Matched cohorts had no significant differences in baseline characteristics. Mean changes in systolic/diastolic BP were −17.5/−8.8, −15.7/−6.3, and −13.0/−8.0 mmHg with DHPs, ACE inhibitors, and ARBs, respectively. Joint National Committee on the Prevention, Detection, Evaluation, and Treatment of High BP 6/7 goal attainment for each regimen was 47.3%, 40.0%, and 32.2%, respectively. DHPs, ACE inhibitors, and ARBs improved BP when added to patients’ β-blocker or diuretic therapy. The greatest benefits were observed with DHPs, followed by ACE inhibitors, then ARBs.
Introduction
Hypertension is a key independent risk factor for cardiovascular diseases (CVD), such as heart failure, stroke, coronary heart disease (CHD), and end-stage renal disease (CitationChobanian et al 2003).
Morbidity and mortality from hypertension-associated disease have been reduced in the US over the past three decades (CitationChobanian et al 2003). However, past progress has not been maintained. The prevalence of hypertension in the US has increased recently (CitationHajjar and Kotchen 2003). Death rates from CHD and stroke have failed to further improve, and end-stage renal disease is being diagnosed at increasing rates (CitationChobanian et al 2003). Importantly, more than two thirds of hypertensive adults in the US do not have their BP under control, manifesting BP levels ≥140/90 mmHg (CitationChobanian et al 2003; CitationHajjar and Kotchen 2003).
The Sixth Report of the Joint National Committee (JNC) on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure (JNC 6) recommended initiation of antihypertensive therapy using a diuretic or β-blocker for patients who have no specific indications for other drug classes (CitationJoint National Committee 1997). The subsequent JNC 7 guidelines recommended thiazide diuretics as the preferred initial agent (CitationChobanian et al 2003). However, approximately half of patients treated for hypertension do not respond to monotherapy (CitationMaterson et al 1993). Indeed, large landmark clinical trials have shown that patients often require up to four medications to achieve BP control (CitationHansson et al 1998; CitationALLHAT Collaborative Research Group 2002; CitationDahlöf et al 2002; CitationBlack et al 2003). It is now accepted that in order to achieve BP goals, most patients will require at least two antihypertensive agents, each from a different class, including diuretics, β-blockers, angiotensin-converting enzyme (ACE) inhibitors, angiotensin receptor blockers (ARBs), and dihydropyridine calcium channel blockers (DHPs) (CitationBakris 2001; CitationAmerican Diabetes Association 2002; CitationChobanian et al 2003; CitationGuidelines Committee 2003).
Despite support for the use of multiple therapies in treating hypertension, few studies have compared the effectiveness of different antihypertensive classes and agents as part of a multidrug regimen in real-world clinical practice. Many real-world issues, such as suboptimal patient adherence with medications, are often not accounted for in clinical trials (CitationMonane et al 1997; CitationBurnier et al 2001). The objective of this retrospective cohort analysis was to compare, within a physician office setting, the clinical effectiveness of DHPs, ACE inhibitors, and ARBs when added to diuretic or β-blocker therapy in patients who had previously received a diuretic or β-blocker, but had failed to achieve their BP goal. This study compared the effectiveness of different multiple antihypertensive regimens used in a way that mirrored the JNC 6 treatment recommendations that were in effect during the time period of the study cohort. Clinical effectiveness was measured by absolute BP reductions as well as by attainment of BP goals specified by key treatment guidelines, including both JNC 6 and 7.
Methods
Data source
This retrospective database analysis used encrypted data extracted from the GE Medical Quality Improvement Consortium Electronic Medical Records (EMR) database. At the time of this analysis, the database contained longitudinal data for approximately 370,000 patients who were receiving treatment from primary care physicians across the US. Data collected from patient records included demographics and diagnoses, prescribed medications and procedures, cardiac risk factors, test results, and patient functional status. Physicians were from large practices in Oregon, Arizona, Texas, Massachusetts, Iowa, Virginia, New Hampshire, and Maine who had been using the EMR database for at least 1 year at study initiation.
Study population
Patients aged ≥20 years who visited a physician’s office during a 4-year period (1998 through 2001), had a documented diagnosis of hypertension (ICD-9-CM: 401.xx) and/or “hypertension/high BP” documented in the problem list, and initiated add-on treatment with any ACE inhibitor, ARB, or DHP were identified for the study. Add-on therapy was operationally defined as patients already receiving β-blocker or diuretic therapy at the time the ACE, ARB, or DHP was initiated; therefore, all study patients were required to be receiving prior treatment with a β-blocker or diuretic. Those patients receiving ACE inhibitor/diuretic or ARB/diuretic fixed-dose combinations were included only if they previously used a diuretic and had discontinued the diuretic at the time the fixed-dose combination was initiated.
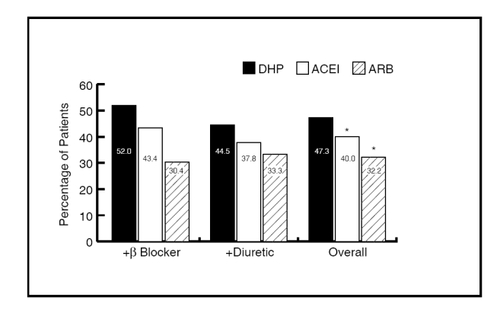
At least two valid BP readings (pre- and post-index) were required for each patient. The pre-index (or baseline) BP reading, defined as the most recent measurement within 6 months before the initiation of ACE inhibitor, ARB, or DHP therapy, was required to be ≥140/90 mmHg for patients who did not have diabetes and ≥130/80 mmHg for patients with diabetes mellitus. The post-index measurement was the final BP reading between 1 to 12 months following the index date and must have been taken before the earliest of the following events: discontinuation of the ACE inhibitor, ARB, or DHP; initiation of any other antihypertensive agent; or 12 months after initiation of the ACE inhibitor, ARB, or DHP. Consequently, patients who initiated another antihypertensive agent on the same day or within the first month of initiating the index ACE inhibitor, ARB, or DHP were excluded, as were patients who discontinued their index product within 1 month of its initiation. Patients also were excluded if they had a recorded diagnosis of congestive heart failure or previous treatment with any other antihypertensive agent. The time frame for the study is depicted in .
Figure 1 Study time frame. Pre-index BP was defined as the most recent BP reading from the date of therapy initiation to 6 months prior to the initiation of therapy. Post-index BP was defined as the final BP reading within 30 to 60 days from the index date.
Data collection
Patient demographics at baseline included age, sex, and weight. During the study period, a number of data were collected to enable comparison of disease severity between patient groups. These data included patients’ age, comorbid hyperlipidemia, diabetes, coronary artery disease and/or, end-stage renal disease, baseline SBP and DBP, and JNC 6 BP stage, the number of BP measurements during the 6 months prior to ACE inhibitor, ARB, or DHP initiation, month/year of ACE inhibitor, ARB, or DHP initiation, prior therapy (β-blocker versus diuretic), and interval between baseline BP measurement and the date of ACE inhibitor, ARB, or DHP initiation. Additionally, Charlson’s comorbidity index, a single score based on the sum of a weighted ranking of comorbid conditions, was calculated from patient data at baseline in order to compare the overall health status of patient groups (CitationCharlson et al 1987). The calculations were based on ICD-9 codes, using the methods described by CitationRomano et al (1993).
As data were analyzed for patients receiving treatment during the period 1998 through 2001, BP goal attainment was defined by JNC 6 (CitationJoint National Committee 1997), the JNC 6 goals were incorporated into the newer JNC 7 guidelines after the study period (CitationChobanian et al 2003). Therefore, JNC 6/7 BP goal attainment was calculated as the proportion of patients with a final BP reading <140/90 mmHg. Attainment of the American Diabetes Association (ADA) goal for hypertension was also calculated, and was defined as the proportion of patients with BP <130/80 mmHg (CitationAmerican Diabetes Association 2002).
Statistical analyses
To reduce the potential influence of confounding variables, a statistical matching technique was utilized. Propensity scores (CitationD’Agostino 1998) were calculated as the probability of being in the DHP and ACE inhibitor cohorts using a multinomial logistic regression model. Patients across the three study cohorts (ACE inhibitor, ARB, DHP) were matched using propensity scores at a 1:1:1 ratio. A set of three matches was identified as the first three patients selected in random order who matched on the likelihood of being in the DHP and ACE inhibitor groups within one-fourth standard deviation of the respective propensity scores. This matching process continued until there were no more sets of three matching patients. One of the advantages of this technique over the use of Cox proportional hazard models is that it removes differences between the groups where attributes of one treatment group may be completely absent in other treatment groups. In retrospective data where treatment assignment is very systematic, these differences can impact the regression model and cause under/over correction for data within the common sample subjects, due to the influence of an unlike group in one arm.
The main study outcomes were incremental mean change in SBP and DBP from pre- to post-index BP reading and the percentage of patients reaching BP goals according to JNC 6/7. Categoric variables were presented as the sum and percentage of patients, and continuous variables as the mean and standard deviation. Baseline characteristics and treatment outcomes were compared using a chi-square test and analysis of variance (ANOVA) for categorical and continuous variables, respectively. Baseline characteristics were tested despite the scoring matching technique used, because matching was based on the p-score, and not each individual characteristic that was used to generate the p-score. Therefore, it was still possible that some differences could exist between the groups with respect to some characteristics. This process also served to test how successful the propensity matching had been. No corrections were applied to p-values for multiple comparisons. Analyses were performed using SAS version 8.2 (SAS Institute, SAS Procedures Guide, Version 8.2, 2002; SAS Institute, Cary, NC, USA).
Results
Baseline characteristics
A total of 1875 patients met the original inclusion criteria for the study; after applying propensity score matching, a total of 660 (220 for each cohort) were included in the final analysis (). There were no statistically significant differences between the DHP, ACE inhibitor, and ARB groups at baseline for mean age, percentage of male patients, and pre-index SBP or DBP. Within medication classes, the most commonly used agents were: DHP (amlodipine besylate [81%]); ACE inhibitor (lisinopril [52%]); ARB (valsartan [50%]). The mean intervals between starting and ending BP measurements were 256 days (DHP), 261 days (ACE inhibitor), and 265 days (ARB). There were no statistically significant differences between the cohorts with respect to the measurement intervals.
Table 1 Propensity score matching – baseline characteristics
Blood pressure outcomes
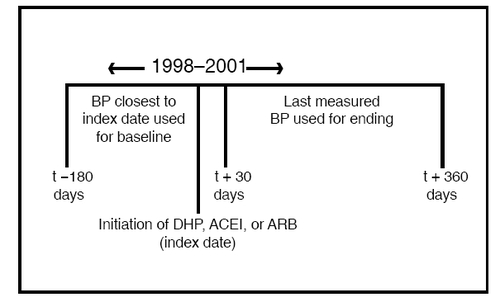
As shown in , mean (SD) SBP reductions in the overall sample were −17.5 (21.0) mmHg for patients receiving add on DHP therapy, −15.7 (20.2) mmHg for those receiving ACE inhibitors as add-on therapy, and −13.0 (21.4) mmHg among patients that received add-on treatment with an ARB. The reductions in SBP were slightly greater when DHP or ACE inhibitors were added on to patients receiving β-blockers in comparison to when they were used as additional therapy in those receiving diuretics as initial therapy, whereas the converse was true for ARBs.
Figure 2 Incremental systolic blood pressure reduction. *p < 0.05 versus DHP.
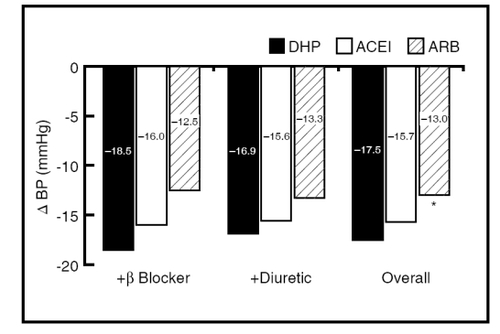
shows that overall mean (SD) reductions in DBP in patients who received DHP as add-on therapy were −8.8 (12.7) mmHg in comparison with −6.3 (11.4) mmHg for those receiving add-on ACE inhibitor therapy, and −8.0 (12.2) mmHg in those that received add-on ARBs. Reductions in DBP were slightly greater when ACE inhibitors or ARBs were added on to patients receiving initial therapy with diuretics versus those receiving β-blockers as initial therapy. In contrast to this, reductions in DBP with DHP add-on therapy were greater in those on initial therapy with β-blockers versus diuretics.
Figure 3 Incremental diastolic blood pressure reduction. *p < 0.05 versus DHP.
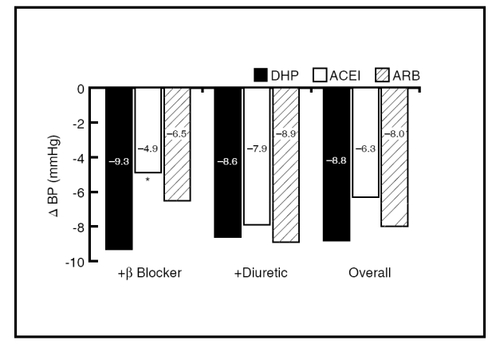
Blood pressure goal attainment is illustrated in . As shown, 47.3% of study patients in the overall DHP-cohort achieved the JNC 6/7 BP goals during the year following treatment initiation, in comparison with 40.0% in the ACE inhibitor group and 32.2% of those receiving add-on therapy with β-blockers. Much of this difference appeared due to improved performance among the cohort initially receiving β-blockers, for whom goal attainment with the addition of DHPs was 52.0% and with the addition of ACE inhibitors it was 43.4% versus 30.4% for ARBs.
Discussion
This “real-world” analysis supports the use of combinations of antihypertensive drugs in order to reduce SBP and DBP and to enable patients to achieve JNC 6/7 BP goals. The addition of an ACE inhibitor, ARB, or DHP to existing β-blocker or diuretic treatment for up to 12 months resulted in significant reductions in SBP and DBP compared with baseline values. These results are in agreement with findings from clinical trials showing that more than one antihypertensive drug is often required to reduce BP and achieve BP control (CitationHansson et al 1998; CitationALLHAT Collaborative Research Group 2002; CitationDahlöf et al 2002; CitationBlack et al 2003). The mean reduction in BP during the study period reported here ranged from 13.0 mmHg to 17.5 mmHg for SBP, and from 6.3 mmHg to 8.8 mmHg for DBP. Sustained BP reductions of this magnitude in patients with hypertension are likely to represent a clinically meaningful treatment effect (CitationStaessen et al 2003; CitationTurnbull et al 2005).
When comparing the effects of three different antihypertensive drug classes as add-ons to β-blocker or diuretic therapy, DHPs were associated with the greatest improvements in BP, followed by ACE inhibitors and then ARBs. We observed that SBP was reduced to a statistically greater extent by DHPs compared with ARBs. Large-scale clinical trials have confirmed that DHP-based treatment regimens are associated with reduced cardiovascular events compared with β-blocker-based therapy (CitationDahlöf et al 2005) and similar reductions to ARB-based antihypertensive regimens (CitationJulius et al 2004). The benefits of ACE inhibitor or DHP combination therapy on SBP is significant, given the importance of SBP as a major risk factor for CVD and the difficulty of achieving improvement in this measure (CitationIzzo et al 2000; CitationChobanian et al 2003). When given in combination with β-blockers or diuretics, DHPs also resulted in a significantly greater reduction in DBP compared with that achieved with ACE inhibitors.
Overall, JNC 6/7 BP goal was achieved by up to 47% of patients taking combination therapy in this analysis. However, a greater proportion of patients attained BP goal when either a DHP (47.3%) or an ACE inhibitor (40.0%) was added to pre-existing β-blocker or diuretic therapy, compared with patients receiving an ARB (32.2%) as add-on therapy. Our study used a standard definition of hypertension control based on the JNC 6 guidelines, as these were applicable during the period for which the data were analyzed (1998 through 2001). The recommendations of JNC 6 have been incorporated into JNC 7; thus, the outcomes of this study continue to be relevant. Nevertheless, 50% of patients in this study had not achieved their BP goal with two agents, suggesting that either the dose of these agents should have been increased further or that additional agents should have been added. Indeed, the Irbesartan type II Diabetic Neuropathy Trials showed more than three antihypertensive agents were required to control BP (CitationLewis et al 2001).
Although our analysis does not report results for specific antihypertensive agents, patient drug therapies were reported. The majority of patients taking DHPs (81%) in the study received amlodipine besylate, and approximately half the patients taking ACE inhibitors and ARBs took lisinopril and valsartan, respectively. We recently performed a retrospective database analysis that specifically assessed the clinical effectiveness of amlodipine given as monotherapy or in combination with other antihypertensive drugs in reducing BP and attaining BP goals (CitationBisognano et al 2004). There were substantial reductions in BP when amlodipine was added to antihypertensive regimens. The benefits occurred regardless of the number of antihypertensive drugs that patients were taking upon initiation of amlodipine (CitationBisognano et al 2004). The observations from the present study corroborate those from our earlier study.
The study reported here has some limitations. Firstly, the results are based on patient samples from several large US general physician practices and may not be generalizable to other populations treated by other physicians. Results may not be applicable to practices without electronic medical records. Secondly, patient adherence to medication regimens was not documented. Low rates of adherence or patient discontinuation of therapy may affect outcomes with medications, and the impact of this effect cannot be taken into account in this analysis. However, discontinuations and lack of adherence are realities of real-world treatment, and while they may limit evaluation of pure efficacy from the study, incorporation of these factors may better reflect real-world effectiveness. Thirdly, JNC 6 states that if a diuretic is not used as the initial antihypertensive it is usually indicated as the second agent because its addition will enhance the effects of other agents. Therefore, the use of DHPs, ACE inhibitors, and ARBs of add-on therapy in patients receiving β-blockers as initial therapy suggests poor compliance with this recommendation. Fourthly, sample sizes in the present study were small and did not allow analysis of results for key subpopulations (for example, the elderly and patients with diabetes mellitus). The propensity matching technique used also reduced the sample size. However, the intent was to compare similar cohorts (based on baseline characteristics) and this was thought more important than keeping all patients in the sample. Finally, the use of a single pre- and post-index measurement of BP is a limitation. The single pre- and post- index measurement was a prospectively defined end point for this analysis based on application of this end point in a prior study (CitationBisognano et al 2004). Alternative definitions may provide differing results, however we felt this definition was the most consistent measure between patients based on the structure of the database, and the fairest end point to compare across treatment groups.
Another potential limitation of this analysis is that channeling bias (CitationPetri and Urquhart 1991) may not be fully addressed, although propensity matching analyses (CitationD’Agostino 1998) were performed to address between-group differences in a number of baseline characteristics. Channeling bias may occur in observational studies because prescribing does not occur by random allocation in clinical practice, in contrast to randomized controlled trials where treatment assignment is random. As it was not known why the prescribing physicians decided upon the use of each antihypertensive agent, whether as initial or subsequent therapy, we cannot fully assess whether patient or prescriber factors systematically led to different treatment choices for different patient types. To the extent that these patient factors were collected and incorporated into the propensity score model, this effect is largely accounted for. However, these treatment choices may have been driven by unobserved factors, such as perceptions of or reaction to indications or formulary restrictions. However, collecting and correcting for such factors were beyond the scope of this study.
Although retrospective cohort analyses such as the study reported here have traditionally been considered to have limited use in comparing treatments, there is evidence that such observational studies and randomized controlled trials demonstrate similar treatment effects (CitationBenson and Hartz 2000; CitationConcato et al 2000). Therefore, despite limitations, most of which are inherent in observational studies, this report provides important results of treatment outcomes in a physician office setting.
In summary, our findings support the benefits of adding a second antihypertensive agent to a patient’s antihypertensive treatment regimen. The greatest benefits are observed when DHPs, followed by ACE inhibitors, and then ARBs are added as second-line therapy to patients already on β-blocker or diuretic therapies. Naturally, if patients have specific indications for specific drug treatment (such as proteinuria or diabetes), such indications must be followed. These findings suggest that appropriate and early integration of an additional antihypertensive drug into patients’ therapeutic regimens, particularly a DHP, together with the appropriate dose titration may lead to improved BP outcomes in real- world clinical practice.
Conflict of interest
Funding for this study was provided by the Pfizer Inc, Outcomes Research Group. Editorial assistance was provided by Jon Edwards of Envision Pharma and funded by Pfizer Inc.
Conflicts of Interest at the time the paper was written, Dr Trent McLaughlin was a paid employee of NDC Health; a firm that received funding from Pfizer Inc to conduct the analysis described in this paper. Drs Roberts and Tang are employees of Pfizer Inc, Dr Bisognano is on the Pfizer speaker’s bureau and received consultancy fees from Pfizer.
References
- ALLHAT Collaborative Research GroupMajor outcomes in high-risk hypertensive patients randomized to angiotensin-converting enzyme inhibitor or calcium channel blocker vs diuretic: the Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial (ALLHAT)JAMA200228829819712479763
- American Diabetes AssociationTreatment of hypertension in adults with diabetesDiabetes Care20022519920111772916
- BakrisGLA practical approach to achieving recommended blood pressure goals in diabetic patientsArch Intern Med20011612661711732930
- BensonKHartzAJA comparison of observational studies and randomized, controlled trialsAm J Ophthalmol200013068811078861
- BisognanoJMcLaughlinTRobertsCSIncremental effectiveness of amlodipine besylate in the treatment of hypertension with single and multiple medication regimensAm J Hypertens2004176768315323063
- BlackHRElliottWJGranditsGPrincipal results of the Controlled ONset Verapamil INvestigation of Cardiovascular Endpoints (CONVINCE) trialJAMA200328920738212709465
- BurnierMSchneiderMPChioleroAElectronic compliance monitoring in resistant hypertension: the basis for rational therapeutic decisionsJ Hypertens2001193354111212978
- CharlsonMEPompeiPAlesKLA new method of classifying prognostic comorbidity in longitudinal studies: development and validationJ Chronic Dis198740373833558716
- ChobanianAVBakrisGLBlackHRSeventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood PressureHypertension20034212065214656957
- ConcatoJShahNHorwitzRIRandomized, controlled trials, observational studies, and the hierarchy of research designsN Engl J Med200034218879210861325
- D’AgostinoRBJrPropensity score methods for bias reduction in the comparison of a treatment to a non-randomized control groupStat Med1998172265819802183
- DahlöfBDevereuxRBKjeldsenSECardiovascular morbidity and mortality in the Losartan Intervention For Endpoint reduction in hypertension study (LIFE): a randomised trial against atenololLancet2002359995100311937178
- DahlöfBSeverPSPoulterNRPrevention of cardiovascular events with an antihypertensive regimen of amlodipine adding perindopril as required versus atenolol adding bendroflumethiazide as required, in the Anglo-Scandinavian Cardiac Outcomes Trial-Blood Pressure Lowering Arm (ASCOT-BPLA): a multicentre randomised controlled trialLancet200536689590616154016
- Guidelines CommitteeEuropean Society of Hypertension-European Society of Cardiology guidelines for the management of arterial hypertensionJ Hypertens20032110115312777938
- HajjarIKotchenTATrends in prevalence, awareness, treatment, and control of hypertension in the United States 1988–2000JAMA200329019920612851274
- HanssonLZanchettiACarruthersSGEffects of intensive blood-pressure lowering and low-dose aspirin in patients with hypertension: principal results of the Hypertension Optimal Treatment (HOT) randomised trial. HOT Study GroupLancet19983511755629635947
- IzzoJLJrLevyDBlackHRClinical Advisory Statement. Importance of systolic blood pressure in older AmericansHypertension2000351021410818056
- Joint National Committee on, Detection, Evaluation, and Treatment of High Blood PressureThe Sixth Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood PressureArch Intern Med19971572413469385294
- JuliusSKjeldsenSEWeberMOutcomes in hypertensive patients at high cardiovascular risk treated with regimens based on valsartan or amlodipine: the VALUE randomised trialLancet200436320223115207952
- LewisEJHunsickerLGClarkeWRRenoprotective effect of the angiotensin-receptor antagonist irbesartan in patients with nephropathy due to type 2 diabetesN Engl J Med20013458516011565517
- MatersonBJRedaDJCushmanWCSingle-drug therapy for hypertension in men: a comparison of six antihypertensive agents with placebo. The Department of Veterans Affairs Cooperative Study Group on Antihypertensive AgentsN Engl J Med1993328914218446138
- MonaneMBohnRLGurwitzJHThe effects of initial drug choice and comorbidity on antihypertensive therapy compliance: results from a population-based study in the elderlyAm J Hypertens1997106977049234822
- PetriHUrquhartJChanneling bias in the interpretation of drug effectsStat Med199110577812057656
- RomanoPSRoosLLJollisJGAdapting a clinical comorbidity index for use with ICD-9-CM administrative data: differing perspectivesJ Clin Epidemiol1993461075978410092
- StaessenJAWangJGThijsLCardiovascular prevention and blood pressure reduction: a quantitative overview updated until 1 March 2003J Hypertens20032110557612777939
- TurnbullFNealBAlgertCEffects of different blood pressure-lowering regimens on major cardiovascular events in individuals with and without diabetes mellitus: results of prospectively designed overviews of randomized trialsArch Intern Med200516514101915983291