Abstract
Background
Acute descending thoracic aortic dissection is a life-threatening emergency. It is not often considered as the initial diagnosis in patients presenting with epigastric pain and could easily be missed in a busy casualty department.
Aim
This case report is aimed to highlight the feasibility of the technique and the need for long-term surveillance following endovascular repair of acute thoracic aortic dissection.
Results
The patient presented with epigastric pain radiating to the interscapular region with a stable hemodynamic status. A computerized tomography (CT) scan demonstrated type B thoracic aortic dissection of the proximal descending thoracic aorta. A successful endovascular repair was carried out with uneventful recovery and follow-up CT scan six years after stent-grafting shows satisfactory position of the stent-graft, patent false lumen in the abdominal aorta perfusing the right kidney, and progressively enlarging diameter of the abdominal aorta.
Conclusion
Thoracic aortic dissection should be considered as a differential diagnosis in patients presenting with epigastric and interscapular chest pain. Emergency endovascular repair of acute thoracic aortic dissection is feasible and relatively safe. Regular follow-up with CT scan is required to evaluate the long-term efficacy and identify the need for re-intervention.
Keywords:
Introduction
Aortic dissection was first described by the personal physician to King George II in 1796 (CitationRoss 1999). Early diagnosis of aortic dissection remains a challenge and in 30%–40% of cases, there is a delay in the initial diagnosis (CitationSpittel et al 1993). The overall mortality for acute descending thoracic aortic dissection (ADTAD) with conservative antihypertensive treatment is reported to be 1.6% with a sharp increase in mortality to 31.5% for open surgical repair (CitationTefera et al 2007). However, the endovascular repair for emergency thoracic aortic dissection is associated with a lower mortality of 12% according to the data from the combined EUROSTAR and United Kingdom Thoracic Endograft registries (CitationLeurs et al 2004).
Intensive antihypertensive treatment is effective in preventing early mortality after ADTAD (CitationTefera et al 2007). The current standard therapy consists of treatment with a β blocker, followed by a vasodilator such as nitroprusside in order to reduce the systemic arterial pressure and heart rate along with analgesia.
In this report, we present a case of acute thoracic aortic Stanford type B dissection, successfully treated with endovascular stenting, followed by a review of recent literature to highlight the feasibility of the technique and the need for long-term surveillance following endovascular repair of thoracic aortic dissection.
Case report
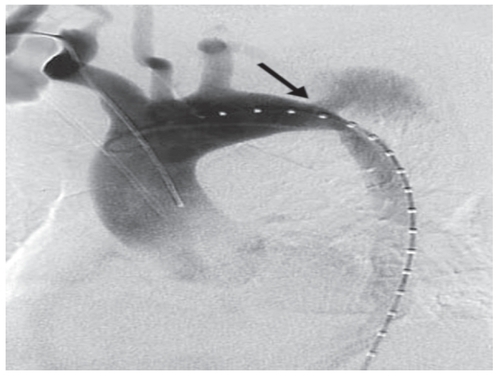
A 57-year-old female sociology student presented to the emergency department with 5–6 days history of persistent epigastric pain radiating to the interscapular region. She had past history of poorly controlled hypertension with no history of a collagen vascular disorder. Previously she had burr-hole evacuation of a traumatic acute subdural hematoma in 1998, with good recovery. Her hemodynamic parameters were stable on admission with a blood pressure of 145/70 mmHg in the right arm and 146/70 in the left. Air entry was reduced in the left lung base. Her hemoglobin was 9.8 gm/dl with a serum creatinine of 61 mmol/L and lactate of 1.2 mmol/L. Both the femoral pulses were palpable and there was no evidence of myocardial ischemia on electrocardiogram. Chest radiograph showed left basal fluid and an urgent computer tomography (CT) scan identified a type B dissection of the thoracic aorta extending down to the abdominal aorta with an exit point of dissection in the right external iliac artery (EIA). Blood flow was seen in both the true and false lumens () with the right kidney being perfused by the false lumen. A decision to stent-graft the thoracic dissection was made in view of her persistent chest pain. Despite her relatively young age, the option of open surgical repair was not considered because of the higher mortality associated with surgery.
Figure 1 Computerized tomography scan showing a type B dissection of the descending thoracic aorta with true and false lumens (arrow).
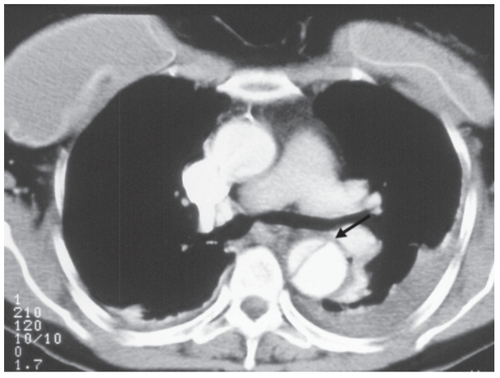
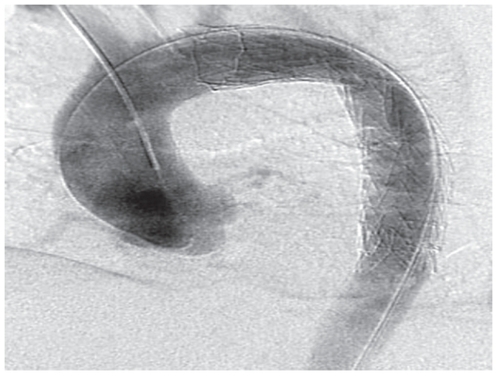
An arch angiogram showed the proximal entry tear into the false lumen (). The right femoral artery was explored and a single thoracic stent-graft measuring 37 mm by 15 cm (Gore Tag®, WL Gore and Associates, Inc., Flagstaff, Arizona, USA) was successfully deployed in the descending thoracic aorta to seal off the entry tear, without covering the ostium of the left subclavian artery (). The stent-graft was oversized by 15% for the thoracic aortic diameter. Repeat angiogram showed that the entry tear was closed and the right renal artery remained patent and perfused by the false lumen with flow entering into the re-entry site within the right EIA. Two further stents were placed in the right EIA to seal off the exit site of dissection. However, the dissection flap was torn proximally into the distal abdominal aorta with persistent flow into the false lumen perfusing the right kidney. A decision was made to leave and monitor the re-entry tear with serial CT scans. The right femoral artery was closed and a drain was placed in the groin wound for three days.
Figure 3 Successful deployment of a thoracic stent in the aortic arch and proximal descending thoracic aorta, sealing off the entry tear.
Her post-operative recovery was uneventful without evidence of visceral, renal or spinal cord ischaemia and she was discharged home on the fifth day following endovascular repair. An initial follow up CT scan at six weeks and six months showed satisfactory position of the thoracic and right external iliac stents with obliteration of the false lumen in the thoracic aorta and patent left subclavian artery.
She has been followed-up for six years since her thoracic stenting in April 2001. Her postoperative serum creatinine measured 64 mmol/L and has remained stable during the entire duration of follow-up with a recent isotope renal scan suggesting good bilateral renal function (Right kidney 45% and left kidney 55%). A recent CT scan in July 2007 shows that the thoracic stent-graft remains in good position. The false lumen is thrombosed within the thoracic aorta but remains patent below the level of diaphragm and is supplied by the true lumen through the re-entry tear perfusing the right kidney. Although the false lumen has slightly decreased in size, there is an overall increase in the diameter of infrarenal aorta from an initial size of 2.9 cm to 4.8 cm. At present, she is being closely monitored with a possibility of intervention for her abdominal aortic aneurysm.
Discussion
Acute dissection of descending thoracic aorta is a challenging emergency and most patients could be treated with intensive medical therapy as hypertension is the commonest predisposing factor. Collagen vascular disease is a relatively uncommon cause of ADTAD (CitationSandridge and Kern 2005). Medical treatment remains the mainstay of treatment in uncomplicated cases of ADTAD. However, at times intervention is required, in addition to medical treatment, to deal with the complications associated with dissection. Indications for intervention in ADTAD include persistent back or chest pain (as in the current case), pseudoaneurysm >4 cm in diameter, uncontrolled hypertension, distal malperfusion with end organ ischemia, progression of dissection and rupture (CitationSong et al 2006). Distal malperfusion can manifest in the form of intestinal, renal, or leg ischemia depending upon the vessels involved in the dissection process and would merit urgent intervention.
Following endovascular stenting for ADTAD the false lumen is thrombosed completely in the portion of the aorta covered by the stent-graft in over 88% of patients by the end of first year, with 60% having thrombosed the entire length of dissection (CitationSong et al 2006). CitationShimono and colleagues (2002) have reported a 58% rate of complete regression of the false lumen following endovascular stenting. These figures suggest that a significant minority would have a patent false lumen as in our case, which is related to the retrograde filling from the true lumen at the site of distal tear.
The risk of spinal cord ischemia and paraplegia is low following endovascular stenting for thoracic aortic dissection even in patients in whom spinal segment T9–L1, which is usually the origin of the anterior spinal artery, had been covered by the endoprosthesis. Consequently, fewer spinal drains are required. Perioperative hypotension, length of aortic stents and previous or simultaneous repair of abdominal aortic aneurysm increase the risk of cord ischemia and paraplegia (CitationChiesa et al 2005).
The combined data from EUROSTAR and United Kingdom Thoracic Endograft registries report a high technical success rate of 88.6% for endovascular stenting in ADTAD. The complication rates remain low with a reported incidence of paraplegia and stroke at 0.8 and 1.5% respectively (CitationLeurs et al 2007). CitationSong and colleagues (2006) has recently reported a 60% rate of re-intervention following endovascular stenting for ADTAD, the indications being proximal or junctional endoleaks, distal reperfusion, stent obstruction and conversion to open repair. The reported 30-day mortality in most series is 7%–9% (CitationLeurs et al 2004; CitationSong et al 2006). Aortic fenestration is a rare procedure that is required in case of a distal malperfusion and end-organ ischemia (CitationPanneton et al 2000) as a result of enlargement of false lumen with compression of the true lumen.
Despite its feasibility, relative safety, and encouraging early results, the long-term outcome of endovascular approach is still under question. Although the approach looks simple, it does however, require the expertise of an experienced and dedicated endovascular team.
Conclusion
Thoracic aortic dissection should be considered as a differential diagnosis in patients presenting with acute onset of epigastric or interscapular pain. Emergency endovascular repair of acute thoracic aortic dissection is feasible and relatively safe. Regular follow-up with CT scan is required to evaluate the long-term efficacy and identify the need for re-intervention.
References
- ChiesaRMalissanoGMarrocco-TrischittaMMSpinal cord ischaemia after elective stent-graft repair of the thoracic aortaJ Vasc Surg20054211716012446
- LeursLJBellRDegrieckYEndovascular treatment of thoracic aortic diseases: combined experience from the EUROSTAR and United Kingdom Thoracic Endograft registriesJ Vasc Surg2004406708015472593
- PannetonJMTehSHCherryKJJrAortic fenestration for acute or chronic aortic dissection: an uncommon but effective procedureJ Vasc Surg2000327112111013035
- RossJKThe death of King George II, with a biographical note on Dr. Frank Nicholls, physician to the kingJ Med Biogr199972283311624084
- SandridgeLKernJAAcute descending aortic dissections: management of visceral, spinal cord, and extremity malperfusionSemin Thorac Cardiovasc Surg2005172566116253830
- ShimonoTKatoNYasudaFTransluminal stent-graft placements for the treatments of acute onset and chronic aortic dissectionsCirculation2002106suppl I24147
- SongTKDonayreCEWalotIEndograft exclusion of acute and chronic descending thoracic aortic dissectionsJ Vasc Surg2006432475816476595
- SpittelPCSpittellJAJrJoyceJWClinical features and differential diagnosis of aortic dissection: experience with 236 cases (1980 through 1990)Mayo Clin Proc199368642518350637
- TeferaGAcherCWHochJREffectiveness of intensive medical therapy in type B aortic dissection: A single-center experienceJ Vasc Surg2007451114917543672