Abstract
Background
The beneficial effects of statins were unequivocally demonstrated in the Scandinavian Simvastatin Survival Study (4S) in 1994, leading to an increase in the use of lipid-lowering drugs. However, to what extent this translates into serum cholesterol levels in a real-life setting has not been systematically investigated.
Objective
To estimate secular trends from 1994 to 2002 in blood lipid levels among unselected younger patients after a first acute myocardial infarction (AMI).
Method
Descriptive single centre study using consecutive data collection in 781 patients (aged <65 years) hospitalized with a first AMI during the period 1994–2002.
Results
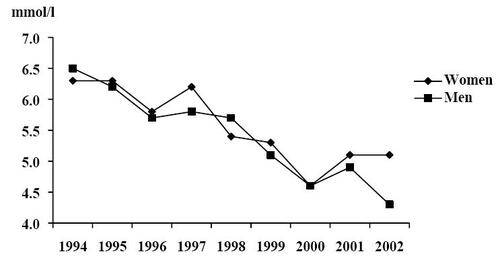
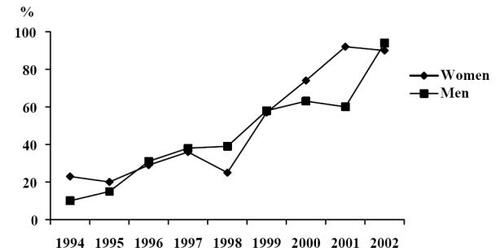
From 1994–2002, the use of lipid-lowering drugs increased from 10% to 94% for men and from 23% to 90% for women. In 1994, the mean serum cholesterol levels were 6.53 mmol/l in men and 6.32 mmol/l in women, decreasing to 4.31 mmol/l and 5.13 mmol/l in men and women, respectively, in 2002. Still, only 56% of the men and 35% of the women had total serum cholesterol levels <4.5 mmol/l in 2002.
Conclusion
Despite a marked increase in lipid-lowering drug treatment in which there was an increase from about 10% in 1994 to more than 90% in 2002, current target levels of <4.5 mmol/l for serum cholesterol were not achieved in a significant proportion of post-AMI patients.
Introduction
Cardiovascular risk factors and prevention
Low-density lipoprotein cholesterol (LDL) concentration in serum is well established as one of the most important risk factors of coronary heart disease (CHD) and much research has been devoted to lipid-lowering therapies and diet modifications (CitationAnonymous 1975, Citation1984a, Citation1984b; CitationBrensike et al 1984). The relation between serum cholesterol levels and CHD is strong and curvilinear with no obvious lower threshold (CitationShekelle et al 1981; CitationPekkanen et al 1990; CitationLaw and Wald 1994). Even relatively small changes in serum cholesterol are closely related to CHD incidence and mortality. Lowering serum cholesterol by 0.6 mmol/l (10%) has been estimated to decrease the risk of CHD by 50% at the age of 40, and by 20% at 70 years. The full effect in risk reduction of decreasing serum cholesterol concentration is reported to be achieved within 5 years (CitationLaw et al 1994a, Citation1994b).
After the publication of several secondary prevention studies (CitationAnonymous 1975, Citation1980, 1984, Citation1984a, Citation1984b, 1987; CitationLevy et al 1984; CitationBrensike et al 1984; CitationBlankenhorn et al 1987; CitationBuchwald et al 1990; CitationWatts et al 1992), lipid lowering by pharmacological agents is now standard therapy after an acute myocardial infarction (AMI). The Scandinavian Simvastatin Survival Study (4S) (CitationAnonymous 1994) was the first, however, to demonstrate unequivocally the beneficial effects of lipid-lowering drugs in patients with CHD. Yet, how this has influenced lipid levels in unselected post-AMI patients has not been systematically explored. Therefore, the aim of this single-centre study was to describe among younger men and women with a first AMI changes in pharmacological treatment with lipid-lowering drugs between 1994 and 2002, to quantify ensuing changes in mean serum concentrations of cholesterol and triglycerides, and to estimate the proportion of patients who meet current European target levels for serum total cholesterol (CitationDe Backer et al 2003).
Methods
Patients for this study were consecutively included among patients discharged from the Coronary Care Unit (CCU) or step-down unit at the Sahlgrenska University Hospital/Östra, Sweden. The catchment’s area of the Sahlgrenska University Hospital/Östra is the northern and eastern parts of Göteborg, with a population of 250,000. Since 1994, all patients under 65 years of age with a first AMI were scheduled for a structured nurse-led follow-up visit 3 months after discharge. During the period 1994 to 2002, 952 patients were discharged alive from hospital with a discharge diagnosis of a first myocardial infarction defined as typical symptoms and either typical ECG changes and/or increased levels of creatin-kinaseMB subunit mass concentration (1994–2001 > 15 μg/l, from 2002 > 10 μg/l). Four patients died before they could be investigated, the medical condition of 8 patients precluded the follow-up visit and 16 patients had their visit in another area. One hundred forty-three patients were either not admitted to the coronary care unit and were therefore not scheduled for routine follow-up, or had a late follow-up with no systematic collection of data and were thus excluded. After these exclusions, 781 patients (607 men, 174 women) were available for the present investigation. All patients were routinely offered dietary counseling by nurses and dieticians in group sessions using essentially the same methods throughout the study period. At the 3-month follow-up, anthropometric measurements, including blood samples, were performed and information on previous diabetes, hypertension and smoking were recorded in a standardized protocol. The study protocol was approved by the Ethics committee of Göteborg University.
Follow-up visit
At follow-up 3 months after the myocardial infarction, blood samples for serum cholesterol and serum triglycerides were drawn after an overnight fast. Use of any lipid-lowering drug and dosage was recorded, as were data on smoking, diabetes and hypertension. Body weight was measured on a lever balance to the nearest 0.1 kg while the patient was wearing indoor clothing. Height was recorded to the nearest centimetre. Body mass index (BMI, weight in kg/height in m2) was used as an index of relative weight and overweight/obesity.
Definitions
Hypertension was defined as diagnosed by a physician before hospitalization. Diabetes was defined as diagnosed by a physician before or during hospitalization. Data on smoking habits at the time of hospitalization and at the follow-up visit were self-reported and/or from hospital records. Total cholesterol concentration and serum triglyceride concentration were measured at the 3-month follow-up or at a later visit (maximum 6 months after the AMI). Blood samples were drawn from an antecubital vein and fasting serum cholesterol and triglyceride measurements were determined according to standard laboratory procedures. Since 1993, serum cholesterol has been analyzed according to Boehringer Mannheim (cat. no. 701912). This method is the standard method of the Laboratory of Clinical Chemistry (certified laboratory) at Göteborg University and remained constant through the study period. Target levels for total serum cholesterol were defined as <4.5 mmol/l according to the current European Society of Cardiology (ESC) guidelines (CitationDe Backer et al 2003).
Statistical methods
The SPSS statistical package (version 11.0) was used for all statistical analyses. Background data were divided into three 3-year periods: 1994–1996, 1997–1999, and 2000–2002. The results are shown as means and standard deviations (SD) for serum cholesterol, serum triglycerides and percentage treated with lipid-lowering drugs each 3-year period from 1994–2002. EpiInfo was used for statistical analysis of linear trends over the years 1994–2002. p-values < 0.05 were considered significant.
Results
Risk factors at baseline
Patient characteristics are shown in . Mean age for men was 54.0 (SD 7.65) years and for women 55.7 (SD 7.29) years. Fifty-six and 59% of the men and women, respectively, were smokers before their AMI. At follow-up, 24% of the men and 27% of the women were still smoking. One in five patients had diabetes, with no gender differences. More women than men had a previous diagnosis of hypertension (43% and 25% in women and men, respectively). More than half of the women and two thirds of the men were overweight or obese.
Table 1 Baseline characteristics for 781 patients, 607 (78%) men and 174 (22%) women, with a first myocardial infarction
Lipid-lowering drugs and lipid levels
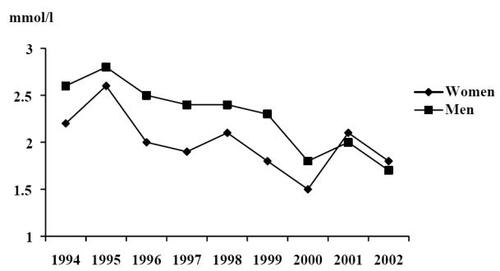
The proportion treated with lipid-lowering drugs increased substantially during the investigated period in both genders (). In 1994, 10% of all men and 23% of all women were treated with lipid-lowering drugs. In 2002, the proportion of patients treated with lipid-lowering drugs had increased to approximately 90% in both men and women. The linear trend over the period was significant in both men and women (p < 0.0001). In 1994, the mean total serum cholesterol was 6.53 (SD 1.27) and 6.32 mmol/l (SD 1.34) in men and women, respectively. During the study period, the mean serum cholesterol levels decreased steadily and, in 2002, the mean serum cholesterol in men and women, respectively, was 4.31 (SD 1.16) and 5.13 mmol/l (SD 1.47) (). The linear trend was significant for both genders (p < 0.0001). Mean serum triglycerides also decreased during the years 1994 to 2002. In 1994, the mean serum triglyceride levels were 2.55 mmol/l (SD 1.58) in men and 2.16 mmol/l (SD 1.11) in women, and in 2002 1.72 mmol/l (SD 0.81) and 1.77 mmol/l (SD 1.13) in men and women, respectively () (p for linear trend over time was <0.0001 in men and <0.05 in women). In 2002, 65% of the men and 50% of the women had total serum cholesterol levels <5.0 mmol/l. If target levels for serum total cholesterol instead were defined as <4.5 mmmol/l), these levels were achieved in 56% of the cases in men and 35% in women.
Figure 1 Percent of men and women with lipid-lowering medication at 3-months follow-up after hospitalization for first myocardial infarction during 1994–2002.
Discussion
The results from the 4S study, the first study to demonstrate unequivocally the benefits of statin therapy in CHD patients, were presented in 1994 (CitationAnonymous 1994). In response to the results of the study and other, ensuing lipid-lowering secondary prevention trials treatment with statins in order to improve patient outcome is now standard practice in CHD patients. The present study provided an opportunity to investigate the implementation of this landmark study. Over the 9-year period between 1994 and 2002, the use of lipid-lowering medication (eg, statins) increased from a low to a markedly high level in younger patients with a first AMI, with a concomitant decrease in lipid levels. Despite the huge increase in lipid-lowering drug treatment, in which there was an increase from about 10% in 1994 to 90% in 2002, current target levels of <4.5 mmol/l for serum cholesterol were not achieved in a significant proportion of these patients. The results from the study correspond with those from the Swedish centre (Malmö) in the Euroaspire II study (CitationAnonymous 2001) except for the higher percentage treated with a statin in our study (90% compared with 74% in CHD patients in Euroaspire II). In the Euroaspire II survey 65% of the patients reached target levels (≤5 mmol/l) for serum total cholesterol; in our study 62% reached these same target levels.
In 2002, the Heart Protection Study (HPS) (CitationHPSCG 2002) established that lowering cholesterol with 40 mg simvastatin daily substantially reduced the incidence of major vascular events in high-risk individuals, irrespective of initial cholesterol level. Following the results in the trial, patients are now routinely treated with 40 mg simvastatin, regardless of initial cholesterol concentrations. Among the 98 patients discharged in 2002, 8.1% (n = 8), however, had no lipid-lowering treatment due to side-effects (n = 2), liver disease (n = 4) or unknown reasons (n = 2).
In the 4S trial 20 mg simvastatin daily lowered total serum cholesterol, on average, with 25% to 28% and LDL with 35% to 38% (1994). The HPS study (CitationHPSCG 2002) showed a reduction in cardiovascular disease by 25% in individuals allocated to 40 mg simvastatin daily in comparison with the placebo group. Because one-sixth of the patients in the statin group in the HPS (CitationHPSCG 2002) trial terminated their statin therapy, the potential reduction is probably underestimated. The average reduction in LDL cholesterol was 1.0 mmol/l, but this difference should probably also have been greater and has been estimated at 1.5 mmol/l (CitationHPSCG 2002). Among the patients in the present study mean serum cholesterol decreased from about 6 mmol/l in both men and women to 4.31 and 5.13 mmol/l in men and women, respectively, corresponding to what might have been expected in the men, but less than that in women. However, the decrease in total serum cholesterol may also partly be attributed to population trends, with decreasing total serum cholesterol in the Göteborg population (CitationWilhelmsen et al 1997; CitationBerg et al 2005) and elsewhere (CitationEvans et al 2001). This decrease is probably partly attributable to diet changes in the population (CitationBecker and Pearson 2002), which include less saturated fat and more fruit and vegetables. Women with a first AMI had higher mean levels of total serum cholesterol at the end of the study. This finding is explained by the fact that a higher proportion of women had less than the recommended dose of statin. In our study 20% (n = 20) of all patients had less than 40 mg simvastatin in the last year of the study; 18% of all men and 30% of all women.
A decrease in mean serum triglycerides was also observed (from 2.55 and 2.16 mmol/l in 1994 to 1.72 and 1.77 mmol/l in 2002 in men and women, respectively). Although there is no target level for serum triglycerides in the current European guidelines (CitationDe Backer et al 2003), it is known to be an important risk factor, particularly in women (CitationSharrett et al 2001). In the definition from the US National Cholesterol Education program serum triglycerides > 1.7 mmol/l are one of the criteria for the metabolic syndrome. Even though the target for lipid-lowering treatment is serum LDL cholesterol concentrations, triglyceride levels are also affected by statin treatment (CitationAnonymous 1994). The increasing use of lipid-lowering drugs probably explains why serum triglycerides have decreased despite increasing BMI levels. In our population about two thirds of the men and women with a first AMI were overweight.
Despite widespread treatment with statins, a substantial proportion of the patients did not reach target levels for serum cholesterol. Target levels for total serum cholesterol (<4.5 mmol/l) were met in 54% of the men and in 35% of the women. Of the 98 patients discharged after a first AMI in 2002, 79 had simvastatin, 10 had atorvastatin, fluvastatin, or pravastatin. Cholestipol hydrochloride was used in one patient. No patients took nicotinic acid or fibrates. Eight patients had no lipid-lowering medication at all. Of those treated with simvastatin, 13 had 20 mg daily. Fiftyfive per cent of patients on the recommended dosage (40 mg daily) according to the HPS study (CitationHPSCG 2002) (36/66 patients) reached the desired levels of <4.5 mmol/l for total serum cholesterol.
During the last decades both CHD mortality and incidence rate of first myocardial infarction have decreased (CitationAbildstrom et al 2003). The decrease started before this study and continued through and after the study period. However, the use of statins has probably influenced this according to evidence given in prior trials (CitationAnonymous 1994; CitationHPSCG 2002). We have not investigated to which extent in this survey.
Limitations
There are several limitations of the present study. First, it is a single-centre study and thus data may not be representative. However, data from the Swedish National Register of Information and Knowledge about Heart Intensive Care Admission (RIKS-HIA) show that there has been a similar increase in usage of lipid-lowering drugs in patients below the age of 80 years from 12% in 1995 to 82% in 2004. The data in this register derive not only from university (teaching) and regional hospitals but also from smaller hospitals, an observation that may explain the slightly higher proportion of patients treated with statins in our hospital. In addition, our study only included younger patients (ie, less than 65 years of age). Accordingly, our population is probably representative of Swedish AMI patients at large. Second, although dieticians and nurses routinely offered dietary counselling to all patients, systematic information regarding participation and compliance was not collected, and hence dietary factors on possible influences of serum lipids cannot be gauged. Third, there is only information on total cholesterol and not LDL cholesterol because high-density lipoprotein cholesterol (HDL) measurements were not done for most of the study period. Fourth, the study was limited to patients discharged from the CCU and step-down unit, and accordingly, we have no information for those patients treated in other units. Presumably, this subset of patients had less severe manifestations of AMI, but to which extent the inclusion of these subjects would have affected the overall results is not known.
Conclusions
Since the results of the 4S study were presented in 1994 until the end of 2002, there has been an increasing use of lipid-lowering medication in AMI patients, with over 80% nationwide now being treated. Almost all patients in the present study under 65 years of age with a first AMI were treated with lipid-lowering drugs by the end of the study period. Despite this, target levels for serum cholesterol were not met in a substantial proportion of patients. These results imply that a standard dose of a statin may not be sufficient and that younger men and women with AMI should be targeted for more intense lifestyle intervention. Moreover, additional medication may be needed.
Acknowledgements
The study was supported by FOU-rådet in Göteborg and Södra Bohuslän, Västra Götalandsregionen and Merck, Sharp and Dohme. Conduct of the study and preparation of the manuscript were funded by an unrestricted grant from Merck, Sharp and Dohme. The company had no role in the interpretation of the data or preparation, review or approval of the manuscript. Conflicts of interest: A Rosengren has received consulting fees and lecture fees from Astrazeneca, as well as lecture fees from Pfizer, Merck, Sharp and Dohme, and Novartis but has no relevant financial interest in the manuscript.
References
- Clofibrate and niacin in coronary heart diseaseJAMA1975231360811088963
- W.H.O. cooperative trial on primary prevention of ischaemic heart disease using clofibrate to lower serum cholesterol: mortality follow-up. Report of the Committee of Principal InvestigatorsLancet19802379856105515
- The Lipid Research Clinics Coronary Primary Prevention Trial results. Reduction in incidence of coronary heart diseaseJAMA1984a25135164
- The Lipid Research Clinics Coronary Primary Prevention Trial results. II. The relationship of reduction in incidence of coronary heart disease to cholesterol loweringJAMA1984b25136574
- Randomised trial of cholesterol lowering in 4444 patients with coronary heart disease: the Scandinavian Simvastatin Survival Study (4S)Lancet1994344138397968073
- Lifestyle and risk factor management and use of drug therapies in coronary patients from 15 countries; principal results from EUROASPIRE II Euro Heart Survey ProgrammeEur Heart J2001225547211259143
- AbildstromSZRasmussenSRosenMTrends in incidence and case fatality rates of acute myocardial infarction in Denmark and SwedenHeart2003895071112695453
- BeckerWPearsonMRiksmaten 1997–98, kostvanor och näringsintag i Sverige, metod-och resultatrapport (Dierary habits and nutrient intake in Sweden 1997–98)2002UppsalaInformation and Nutrition Department, Swedish National Food Administration
- BergCMLissnerLAiresNTrends in blood lipid levels, blood pressure, alcohol and smoking habits from 1985 to 2002: results from INTERGENE and GOT-MONICAEur J Cardiovasc Prev Rehab20051211525
- BlankenhornDHNessimSAJohnsonRLBeneficial effects of combined colestipol-niacin therapy on coronary atherosclerosis and coronary venous bypass graftsJAMA19872573233403295315
- BrensikeJFLevyRIKelseySFEffects of therapy with cholestyramine on progression of coronary arteriosclerosis: results of the NHLBI Type II Coronary Intervention StudyCirculation198469313246360414
- BuchwaldHVarcoRLMattsJPEffect of partial ileal bypass surgery on mortality and morbidity from coronary heart disease in patients with hypercholesterolemia. Report of the Program on the Surgical Control of the Hyperlipidemias (POSCH)N Engl J Med1990323946552205799
- De BackerGAmbrosioniEBorch-JohnsenEuropean guidelines on cardiovascular disease prevention in clinical practice. Third Joint Task Force of European and Other Societies on Cardiovascular Disease Prevention in Clinical PracticeEur Heart J20032416011012964575
- EvansATolonenHHenseHWTrends in coronary risk factors in the WHO MONICA projectInt J Epidemiol200130Suppl 1354011171847
- [HPSCG] Heart Protection Collaborative GroupMRC/BHF Heart Protection Study of cholesterol lowering with simvastatin in 20536 high-risk individuals: a randomised placebo-controlled trialLancet200236072212114036
- LawMRWaldNJAn ecological study of serum cholesterol and ischaemic heart disease between 1950 and 1990Eur J Clin Nutr199448305258055847
- LawMRWaldNJThompsonSGBy how much and how quickly does reduction in serum cholesterol concentration lower risk of ischaemic heart disease?BMJ1994a308367728043072
- LawMRWaldNJWuTSystematic underestimation of association between serum cholesterol concentration and ischaemic heart disease in observational studies: data from the BUPA studyBMJ1994b30836368124143
- LevyRIBrensikeJFEpsteinSEThe influence of changes in lipid values induced by cholestyramine and diet on progression of coronary artery disease: results of NHLBI Type II Coronary Intervention StudyCirculation198469325376360415
- PekkanenJLinnSHeissGTen-year mortality from cardiovascular disease in relation to cholesterol level among men with and without preexisting cardiovascular diseaseN Engl J Med1990322170072342536
- SharrettARBallantyneCMCoadySACoronary heart disease prediction from lipoprotein cholesterol levels, triglycerides, lipoprotein(a), apolipoproteins A-I and B, and HDL density subfractions: The Atherosclerosis Risk in Communities (ARIC) StudyCirculation200110411081311535564
- ShekelleRBShyrockAMPaulODiet, serum cholesterol, and death from coronary heart disease. The Western Electric studyN Engl J Med198130465707442730
- WattsGFLewisBBruntJNLewisESEffects on coronary artery disease of lipid-lowering diet, or diet plus cholestyramine, in the St Thomas’ Atherosclerosis Regression Study (STARS)Lancet199233956391347091
- WilhelmsenLJohanssonSRosengrenARisk factors for cardiovascular disease during the period 1985–1995 in Goteborg, Sweden. The GOT-MONICA ProjectJ Intern Med19972421992119350164