Abstract
Diabetes mellitus is associated with an increased risk of cardiovascular disease, even in the presence of intensive glycemic control. Substantial clinical and experimental evidence suggest that both diabetes and insulin resistance cause a combination of endothelial dysfunctions, which may diminish the anti-atherogenic role of the vascular endothelium. Both insulin resistance and endothelial dysfunction appear to precede the development of overt hyperglycemia in patients with type 2 diabetes. Therefore, in patients with diabetes or insulin resistance, endothelial dysfunction may be a critical early target for preventing atherosclerosis and cardiovascular disease. Microalbuminuria is now considered to be an atherosclerotic risk factor and predicts future cardiovascular disease risk in diabetic patients, in elderly patients, as well as in the general population. It has been implicated as an independent risk factor for cardiovascular disease and premature cardiovascular mortality for patients with type 1 and type 2 diabetes mellitus, as well as for patients with essential hypertension. A complete biochemical understanding of the mechanisms by which hyperglycemia causes vascular functional and structural changes associated with the diabetic milieu still eludes us. In recent years, the numerous biochemical and metabolic pathways postulated to have a causal role in the pathogenesis of diabetic vascular disease have been distilled into several unifying hypotheses. The role of chronic hyperglycemia in the development of diabetic microvascular complications and in neuropathy has been clearly established. However, the biochemical or cellular links between elevated blood glucose levels, and the vascular lesions remain incompletely understood. A number of trials have demonstrated that statins therapy as well as angiotensin converting enzyme inhibitors is associated with improvements in endothelial function in diabetes. Although antioxidants provide short-term improvement of endothelial function in humans, all studies of the effectiveness of preventive antioxidant therapy have been disappointing. Control of hyperglycemia thus remains the best way to improve endothelial function and to prevent atherosclerosis and other cardiovascular complications of diabetes. In the present review we provide the up to date details on this subject.
Introduction
Isolated diabetes mellitus is a frequent and increasing public health problem. Importantly, diabetes has a prevalence of 2%–5% in most Western countries, and is rapidly increasing in Asiatic countries due to changes in dietary habits during the last years (CitationContreras et al 2000).
Over the last two decades it has become evident that the endothelium is not an inert, single-cell lining covering the internal surface of blood vessels, but in fact plays a crucial role in regulating vascular tone and structure. Importantly, a healthy endothelium inhibits platelet and leukocyte adhesion to the vascular surface and maintains a balance of profibrinolytic and prothrombotic activity (CitationLibby 2002).
Endothelial dysfunction has received increasing attention as a potential contributor to the pathogenesis of vascular disease in diabetes mellitus. Under physiological conditions, there is a balanced release of endothelial-derived relaxing and contracting factors, but this delicate balance is altered in diabetes and atherosclerosis, thereby contributing to further progression of vascular and end-organ damage (CitationTan, Chow, Ai et al 2002).
Hyperglycemia is the major causal factor in the development of endothelial dysfunction in diabetes mellitus. Although the mechanisms underlying this phenomenon are likely to be multifactorial. Insulin resistance has been described in several diseases that increase cardiovascular risk and mortality, such as diabetes, obesity, hypertension, metabolic syndrome, and heart failure.
Increasing evidence suggests that the progression of insulin resistance to type 2 diabetes parallels the progression of endothelial dysfunction to atherosclerosis. Insulin resistance is closely linked with visceral adiposity, and early data suggested that free fatty acids were responsible for this association (CitationBoden and Shulman 2002). More recently, other plasma biomarkers produced by adipose tissue, including TNF and resistin, have been shown to have elevated levels during obesity and to mediate insulin resistance. Conversely, the expression and secretion of adiponectin, an adipocyte-specific protein that enhances insulin-mediated glucose uptake, is inversely correlated with fat mass (CitationLyon et al 2003). Several studies have demonstrated that nitric oxide (NO)-mediated vasodilation is abnormal in patients with type 2 diabetes (CitationWilliams et al 1996). Brachial artery responses were found to be abnormal to both endogenous and exogenous NO donors, suggesting that there was increased inactivation of NO, possibly caused by enhanced metabolism of NO or abnormal vascular smooth muscle cell (VSMC) responses to NO because of alterations in signal transduction in the guanylate cyclase pathway. Obese patients without frank type 2 diabetes have been shown also to have abnormal endothelial function (CitationSteinberg et al 1996; CitationPerticone et al 2001). Herein, we review the literature about endothelial dysfunction in diabetes mellitus with regards to its pathogenesis at molecular and clinical level, and possible available mode of therapy.
Normal endothelial cell (EC) function
The EC is no longer considered a simple barrier. In fact it is a complex organ, with paracrin and autocrin function, which provides a “first line” physiological defense against atherosclerosis. The EC lines the internal lumen of all the vasculature and serves as an interface between circulating blood and vascular smooth muscle cells (VSMC). In addition to serving as a physical barrier between the blood and tissues, the EC facilitates a complex array of functions in intimate interaction with the VSMC, as well as cells within the blood compartment (CitationVanhoutte 1995; CitationDe Meyer and Herman 1997; CitationHaller 1997; CitationMombouli 1997).
The last two decades of research have established unambiguously that the EC has a critical role in overall homeostasis whose functions are integrated by a complicated system of chemical mediators. This system exerts effects on both the surrounding VSMC and the cells in the blood that lead to one or more of the following alterations: (1) vasodilatation or vasoconstriction to regulate organ blood, (2) maintenance of fluidity of blood and avoidance of bleeding, (3) proinflammatory or anti-inflammatory changes, and (4) growth and/or changes in the phenotypic characteristics of VSMC (CitationWautier et al 1983, Citation1990, Citation1996; CitationConger 1994; CitationChappey 1996; CitationDe Meyer and Herman 1997).
During the last decade, a multitude of experimental arguments have led to the concept that NO is not only involved in the control of vasomotor tone but also in vascular homeostasis and neuronal and immunological functions. Endogenous NO is produced through the conversion of the amino acid, l-arginine to l-citrulline by the enzyme, NO-synthase (NOS) from which several isoforms have recently been isolated, purified, and cloned. NOS-type I (isolated from brain) and type III (isolated from ECs) are termed “constitutive-NOS” and produce picomolar levels of NO from which only a small fraction elicits physiological responses. NO produced by NOS type III in the endothelium diffuses to the vascular smooth muscle (VSM) where it activates the enzyme guanylate cyclase. The concomitant increase in cyclic GMP then induces relaxation of the VSM.
The EC produces mediators that induce vasoconstriction, including endothelin (CitationHaefliger et al 1992; CitationCacoub 1993; CitationLevin 1996), prostaglandins (CitationViberti 1989; CitationGoldin et al 1996) and angiotensin II (ANG-II) (CitationStuddy et al 1983; CitationHsueh and Anderson 1993; CitationRabelink and Bakris 1998; CitationMcFarlane 1999) and regulates vascular tone by maintaining a balance between vasodilation (NO production) and vasoconstriction (eg, A-II generation). ANG-II is produced in local tissues by the EC (Toop et al 1989; CitationMombouli 1997) and exerts regulatory effects upon several VSMC functional activities including contraction (ie, vasoconstriction), growth, proliferation, and differentiation. NOS also are regulated by local concentrations of bradykinin (CitationBusse et al 1993). This peptide acts with b2 receptors on the EC cell surface membrane, increasing the generation of NO via NOS activation. Interestingly, the local concentrations of bradykinin are regulated by the activity of angiotensin converting enzyme (ACE). ACE breaks down bradykinin into inactive peptides (CitationLuscher et al 1993; CitationMombouli 1997).
Furthermore the EC has a prominent role in maintaining blood fluidity and restoration of vessel wall integrity to avoid bleeding and plays a key role in the balance between the coagulation and fibrinolytic systems. In addition to its key role in growth and differentiation of the VSMC through the release of either promoters of growth and/or inhibitors of growth and differentiation and, as such, has an impact on vascular remodeling (CitationCowan and Langille 1996). However, strong evidence suggests that promotion of VSM growth is mediated by local production of platelet growth factor (PGF) and ANG-II (CitationWilliams 1998).
The EC is also involved in the production of specific molecules that have a regulatory role in inflammation such as leukocyte adhesion molecule (LAM), intracellular adhesion molecule (ICAM) and vascular cell adhesion molecule (VCAM). These molecules are denominated “adhesion molecules” and function to attract and “anchor” those cells involved in the inflammatory reaction. Very recently it has been demonstrated that the atherosclerotic process is associated with an increased blood level of inflammation (acute phase proteins) markers (CitationTracy 1997; CitationBiegelsen and Loscalzo 1999).
Endothelial dysfunction and microalbuminuria
Microalbuminuria is usually defined as a urinary albumin excretion rate of 30–300 mg in a 24 h urine collection, or as a urinary albumin excretion rate of 20–200 mg/min in a timed overnight urine collection, although microalbuminuria was demonstrated to be a predictor for cardiovascular events at levels below these conventional cut-off values. It is an independent risk factor for the development of cardiovascular disease and a predictor of cardiovascular mortality in the diabetic population. It is associated with insulin resistance, atherogenic dyslipidaemia, and central obesity, the absence of nocturnal drop in both systolic and diastolic pressures and is a part of the metabolic cardiovascular syndrome associated with hypertension. Because microalbuminuria is related to endothelial dysfunction and increased oxidative stress, it is not surprising that diabetic atherosclerosis parallels diabetic glomerulosclerosis and is a very powerful risk factor for coronary heart disease and stroke in diabetic persons. The impairment of endothelium and NO-dependent vasodilation in the human forearm microcirculation in type 1 diabetic patients is more severe in the presence of microalbuminuria (CitationDogra et al 2001). This defect was attributed to the presence of advanced glycosylation end products and/or increased generation of the superoxide anion in type 1 diabetic patients, both of which are known to effectively antagonize the biological activity of NO. Furthermore, basal NO-dependent vasodilatory tone has been found to be reduced in type 1 diabetic patients. Impaired NO biosynthesis has been demonstrated in the forearm vasculature of type 1 diabetic patients with microalbuminuria (CitationElliot 1993).
A cross-sectional association possibly exists between increased urinary albumin excretion and the presence of sub-clinical atherosclerosis (CitationJensen 2000), whether urinary albumin excretion increases before, during or after the development of morphological changes in the atherosclerotic process (in stage I, II or III), ie, whether microalbuminuria is a predictor of atherosclerosis or of atherosclerotic progression is not clear. Multiple markers of endothelial dysfunction have also been documented in normoalbuminuric subjects with type 2 diabetes, suggesting that the vasculopathy in type 2 diabetes occurs early and may even be operative before the development of microalbuminuria (CitationLim et al 1999).
Endothelial dysfunction and the metabolic syndrome
The metabolic syndrome is a highly prevalent multifaceted clinical entity produced through the interaction of genetic, hormonal and lifestyle factors. A distinctive constellation of abnormalities precedes and predicts the accelerated development of inflammation and coagulation represent emerging risk contributors associated with obesity and insulin resistance, central components of the metabolic syndrome, which act in concert with traditional abnormalities to increase cardiovascular risk. The initiation and progression of atherosclerosis may have its origins in impaired endothelial function that can be detected at the earliest stages of development of the syndrome. The basic elements of the metabolic syndrome and accelerated phase of atherogenesis are often silent partners that present many years before the onset of type 2 diabetes mellitus. The ability to detect and monitor sub clinical vascular disease, as a reflection of the multiple factors that contribute to impair arterial wall integrity, holds potential to further refine cardiovascular risk stratification (CitationMcVeigh and Cohn 2003).
Over time, insulin resistance is associated with more components of the metabolic syndrome () including, low high density lipoprotein (HDL) cholesterol level, hypertension, increased vascular production of reactive oxygen species, increased plasma PAI-1–mediated thrombotic tendency, hyperuricemia, high triglyceride levels and elevation of oxidation-prone small dense low-density lipoprotein (LDL) cholesterol levels. All are associated with endothelial dysfunction (CitationMcIntyre et al 1999; CitationToikka et al 1999; CitationKita et al 2001; CitationMatsuoka 2001). The incidence of the metabolic syndrome, as defined by the Adult Treatment Panel III report, increases with age. Carbohydrate intolerance occurs when the islet cells can no longer make enough insulin to overcome insulin resistance, and thus secreted insulin does not appropriately suppress hepatic glucose production. Free fatty acids may contribute to these changes, given that they can induce islet cell apoptosis and enhance liver gluconeogenesis (CitationArner 2003).
Table 1 Clinical identification of the metabolic syndrome
Free fatty acids and proinflammatory adipokines likely contribute to endothelial dysfunction early in the course of insulin resistance. Free fatty acids induce endothelial dysfunction, whereas several adipokines promote both inflammatory responses and insulin resistance (CitationSteinberg et al 1997). The role of tumor necrosis factor TNF- in vascular inflammation is well known, and a role for leptin is emerging (CitationFantuzzi and Faggioni 2000; CitationPlutzky 2001). Adiponectin attenuates vascular inflammatory changes, but its effects are reduced by its diminished expression in patients who are obese or have insulin resistance (CitationOuchi et al 2000, Citation2001; CitationYokota et al 2000). In the later stages of the metabolic syndrome, hyperglycemia contributes to the pathology by affecting signal transduction pathways, including those mediated through protein kinase C, in the endothelial cells (Tesfamariam et al 1999).
Insulin resistance in the natural history of type 2 diabetes
Insulin resistance, defined as the decreased ability of insulin to promote glucose uptake in skeletal muscle and adipose tissue and to suppress hepatic glucose output, may be present for many years before the development of any abnormality in plasma glucose levels (CitationKahn and Flier 2000; CitationHaffner 2003).
The insulin resistance syndrome encompasses more than a subnormal response to insulin-mediated glucose disposal. Patients with this syndrome also frequently display elevated blood pressure, hyperlipidemia and dysfibinolysis even without any clinically demonstrable alteration in plasma glucose concentrations. Of note, endothelial dysfunction also has been demonstrated in patients with hypertension (CitationLandin et al 1990; CitationLuscher 1990; CitationBonner 1994; CitationBriner and Luscher 1994; CitationKamide et al 1996; CitationLemne and de Faire 1996; CitationHedner and Sun 1997; CitationKhder et al 1998), which is one of the features of the insulin resistance syndrome. It is tempting to speculate that loss of endothelial-dependent vasodilation and increased vasoconstrictors might be etiological factors of hypertension. Moreover loss of activity and/or quantity of endothelium-bound protein lipase activity may contribute to hyperlipidemia, which is typical of the insulin resistance syndrome. A synergistic interaction and vicious cycle may exist in which endothelial dysfunction contributes to insulin resistance and vice versa ().
Figure 1 Progression of endothelial dysfunction in relation the progression of insulin resistance (CitationHsueh et al 2004).
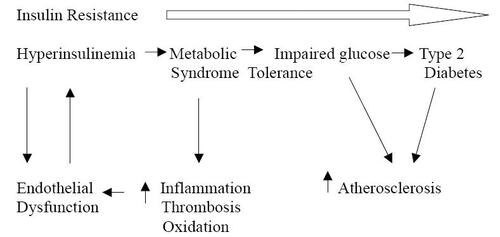
Insulin resistance has a well-known but not completely defined genetic influence, frequently transmitted along generations in any given family. Endothelial dysfunction has been demonstrated in insulin-resistant states in animals and humans and may represent an important early event in the development of atherosclerosis. Insulin resistance may be linked to endothelial dysfunction by a number of mechanisms, including disturbances of sub cellular signaling pathways common to both insulin action and NO production. Other potential unifying links include the roles of oxidant stress, endothelin, the renin angiotensin system and the secretion of hormones and cytokines by adipose tissue. Individuals who advance toward the development of type 2 diabetes experience progressive deterioration of glucose tolerance over time. In addition, obesity, which also has an important genetic component, invariably exacerbates any degree of insulin resistance (CitationKahn and Flier 2000). Thus, obesity and insulin resistance are usually present for many years before the appearance of other abnormalities such as hypertension, dyslipidemia, type 2 diabetes and cardiovascular disease. In certain individuals, obesity and insulin resistance may be present during childhood and adolescence (CitationGoran et al 2003).
Increasing evidence suggest that hyperinsulinaemia is linked with the development of atherosclerosis in patients with diabetes. Whether hyperinsulinaemia directly affects neutrophil transendothelial migration and surface expression of related endothelial adhesion molecules were studied on healthy volunteers and from patients with non-insulin-dependent diabetes mellitus across human umbilical vein. Endothelial cells cultured in insulin-rich medium using cell-culture inserts high insulin (over 50 microU/ml for 24 h) enhanced neutrophil transendothelial migration in a dose-dependent manner. This was associated with increased expression of platelet endothelial cell adhesion molecule-1 (PECAM-1) but not of intercellular adhesion molecule-1 (ICAM-1), P-selectin or E-selectin (CitationOkouchi et al 2002).
Mechanisms of endothelial dysfunction in insulin resistance
Multiple, interrelated mechanisms contribute to endothelial cell dysfunction in insulin resistance. The exact mechanism by which dyslipidemia contributes to endothelial dysfunction is unknown. It is known that endothelial NOS infiltrates into caveolae, which are cholesterol-rich invaginations present in endothelial cells and VSMC that decrease vasoconstrictive responses to angiotensin II, endothelin and constitutive endothelial NOS activity in animals (CitationRizzo 1998). Addition of oxidized LDL to cultured endothelial cells disrupts the caveolae complex and is thought to be associated with decreased endothelial NOS activity and endothelial dysfunction (CitationBlair et al 1999; CitationDrab et al 2001). HDL cholesterol can prevent the oxidized LDL–mediated decrease in cholesterol in caveolae, prevent the translocation of endothelial NOS and caveol in from caveolae, and prevent the decrease in responsiveness to acetylcholine (CitationUittenbogaard et al 2000). These effects occur because HDL cholesterol donates cholesterol to the caveolae complex. These cellular events are consistent with the proatherogenic effects of LDL cholesterol and oxidized LDL cholesterol and the protective effects of HDL cholesterol.
The presence of hypertension and other atherosclerotic risk factors is associated with increased vascular angiotensin II generation and activity (CitationDzau 2001). Because angiotensin II and insulin activate a common signaling pathway, increased sensitivity to angiotensin II may occur in the hyperinsulinemic, insulin-resistant state (CitationGaboury et al 1994). In addition, angiotensin II stimulates intracellular adhesion molecule–1 and monocyte chemo-attractant protein–1 through the MAPK pathway in endothelial cells and VSMC (CitationChen et al 1998; CitationTummala et al 1999; CitationXi et al 1999). It is likely that many of the components of the metabolic syndrome directly alter endothelial vasoreactivity. However, these factors may decrease NO activity through oxidation pathways; the role of oxygen free radical is discussed bellow in Oxidative stress and endothelial cell dysfunction.
Role of hyperglycemia in diabetic endothelial dysfunction
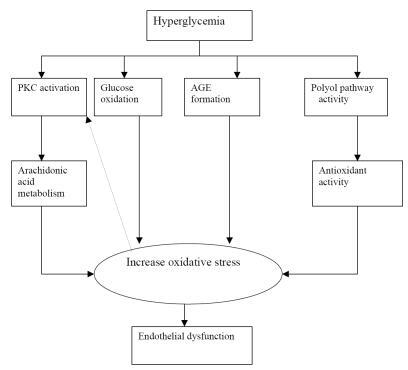
Hyperglycemia is the major causal factor in the development of endothelial dysfunction in patients with diabetes mellitus (). Clinical trials have identified hyperglycemia as the key determinant in the development of chronic diabetic complications. The formation of advanced glycation end products (AGEs) is an important biochemical abnormality accompanying diabetes mellitus and, likely inflammation in general. Although the mechanisms underlying this phenomenon are likely to be multi-factorial, recent in-vivo and in- vitro studies have indicated a crucial role of the diacylglycerol (DAG)-protein kinase C (PKC) pathway in mediating this phenomenon. PKC may have multiple adverse effects on vascular function, including the activation of superoxide-producing enzymes such as the nicotinamide adenine dinicleotide phosphate (NADPH) oxidase as well as increased expression of a dysfunctional, superoxide-producing, uncoupled endothelial nitric oxide synthase (NOS III). PKC-mediated superoxide production may inactivate NO derived from endothelial NOS III, and may inhibit the activity and/or expression of the NO downstream target, the soluble guanylyl cyclase. The effects of AGEs on vessel wall homeostasis may account for the rapidly progressive atherosclerosis associated with diabetes. Driven by hyperglycemia and oxidant stress, AGEs form to a greatly accelerated degree in diabetes. Within the vessel wall, collagen-linked AGEs may “trap” plasma proteins, quench NO activity and interact with specific receptors to modulate a large number of cellular properties. On plasma low density lipoproteins (LDL), AGEs initiate oxidative reactions that promote the formation of oxidized LDL. The interaction of AGEs with endothelial, as well as with other cells accumulating within the atherosclerotic plaque, such as mononuclear phagocytes and smooth muscle cells, provides a mechanism to augment vascular dysfunction. Specifically, the interaction of AGEs with vessel wall component increases vascular permeability, the expression of procoagulant activity and the generation of reactive oxygen species, resulting in increased endothelial expression of endothelial leukocyte adhesion molecules (CitationWen et al 2002; CitationHink et al 2003; CitationBasta et al 2004; CitationFarhangkhoee et al 2006), while acute hyperglycemia and hyperinsulinemia induced vasodilatation is not accompanied by changes in microvascular permeability or endothelial markers (CitationOomen et al 2002).
The effects of acute glycemia on plasma nitric oxide (NO; nitrite plus nitrate) levels, Cu-Zn Superoxide dismutase (Cu-Zn SOD) activity and thiobarbituric acid-reactive substances (TBARS) levels were studied in age-matched female subjects before and two hours after glucose loading. Plasma NO levels were significantly higher in subjects with diabetic glucose tolerance (DGT) than in subjects with normal glucose tolerance (p < 0.001) and impaired glucose tolerance (IGT) (p < 0.05) at baseline. TBARS levels were significantly elevated in subjects with DGT and IGT (p < 0.001 and p < 0.001). Cu-Zn SOD activities were significantly increased in subjects with NGT, and were significantly decreased in subjects with IGT and DGT (p < 0.001 and p < 0.001) after glucose loading; suggest that NO availability was decreased when the blood glucose levels were only moderately elevated above normal levels. This might be related with the enhanced oxidative stress (CitationKonukoglu et al 2003).
Other studies examined the effect of acute hyperglycemia on endothelium-dependent vasodilation in patients with DM or impaired glucose metabolism in- vivo by plethysmography. The vasodilatory response to acetylcholine at infusion rates of 7.5, 15, and 30 microg/min was studied in the fasting state and at two levels of hyperglycemia, which were achieved by the infusion of glucose, insulin and somatostatin. The vasodilatory response to acetylcholine was measured by calculating the forearm blood flow ratio (FBFR), defined as the measured forearm blood flow at a specific acetylcholine infusion rate divided by the baseline forearm blood flow without acetylcholine infusion. The induction of hyperglycemia resulted in a significant reduction in FBFR for all rates of acetylcholine infusion and suggests the importance of hyperglycemia in the development of endothelial dysfunction observed in patients with DM or impaired glucose metabolism (CitationBhargava et al 2003; CitationKim et al 2003).
Oxidative stress and endothelial cell dysfunction
Diabetic endothelium produces an increase in both O2 and H2O2 leading to enhanced intracellular production of OH. Thus, OH is implicated in diabetes-induced endothelial dysfunction (CitationTesfamariam et al 1992; CitationPieper et al 1997). Reactive oxygen species (ROS) are generated at sites of inflammation and injury. ROS at low concentrations can function as signaling molecules participating as signaling intermediates in the regulation of fundamental cell activities such as cell growth and cell adaptation responses, whereas at higher concentrations, ROS can cause cellular injury and death. The vascular endothelium, which regulates the passage of macromolecules and circulating cells from blood to tissues, is a major target of oxidative stress, playing a critical role in the pathophysiology of several vascular diseases and disorders. Specifically, oxidative stress increases vascular endothelial permeability and promotes leukocyte adhesion, which is coupled with alterations in endothelial signal transduction and redox-regulated transcription factors (CitationHazel et al 2001). Decreased endothelium-dependent vasodilation in diabetic subjects is associated with the impaired action of NO secondary to its inactivation resulting from increased oxidative stress, rather than decreased NO production from vascular endothelium, and that abnormal NO metabolism is related to advanced diabetic microvascular complications (CitationMaejima et al 2001).
Since ROS generation is increased in various disease states including DM and a direct reaction between NO and superoxide anion has been demonstrated, so a hypothesis suggest that inhibition of ROS will restore coronary microvascular responses to ACh in a dog model of DM and topical application of superoxide dismutase (SOD) (250 U/ml) and catalase (250 U/ml) restored to normal ACh induced coronary microvascular responses in DM while having no affect in normal animals (CitationAmmar et al 2000).
How is endothelial function assessed?
Endothelium-dependent vasodilatation can be assessed in the coronary and peripheral circulations. The most relevant methodological issues in the research on endothelial function and dysfunction have recently been published (CitationDeanfield et al 2005; CitationHadi et al 2005). We provide a summary of the available modalities of testing:
In coronary circulation, non-invasive tests for assessment of coronary endothelial function include Doppler echocardiography, positron emission tomography and phase-contrast magnetic resonance imaging were described. However, the gold-standard test for the evaluation of coronary endothelial function requires invasive coronary angiography; quantitative coronary angiography can be used to examine the changes in diameter in response to intracoronary infusions of endothelium-dependent vasodilators such as acetylcholine. Endothelial function of the coronary microvasculature can be assessed with intracoronary doppler techniques to measure coronary blood flow in response to pharmacological or physiological stimuli (CitationAnderson 1999; CitationAl Suwaidi 2001; CitationFarouque and Meredith 2001). Diagnostic coronary angiography is first performed with a standard femoral percutaneous approach. No nitroglycerin given before the diagnostic approach. Vasomotor responses to acetylcholine and adenosine then assessed (CitationAl Suwaidi et al 2001). After control coronary angiograms had been obtained, a 0.014- Inc Doppler guide wire is introduced through an 8F-guiding catheter into the left anterior descending coronary artery (LAD). Once baseline flow velocity data are obtained at the position (when a stable doppler signal was obtained), a bolus of intracoronary adenosine (24–36 μg, from a solution of 6 mg adenosine in 1 L of saline) is administered. Then selective intra coronary infusion of increasing concentration of acetylcholine (10−6, 10−5, and 10−4mol/L) is performed for a total 3 minutes through a 2.2 F Ultrafuse coronary infusion catheter. Symptoms, hemodynamic data, electrocardiographic and doppler velocities are recorded at the end of each infusion or bolus injection, followed by selective coronary angiogram. Coronary blood flow is calculated using the formula D2×APV, where D represents the coronary diameter and APV equals the average peak velocity from Doppler tracing.
In Peripheral Circulation, Brachial artery ultrasound is a widely used non-invasive measure of endothelial function. Upper-arm occlusion for 5 minutes results in reactive hyperemia after the cuff is released; this increase in shear stress results in endothelium-dependent flow-mediated vasodilatation. Importantly, endothelial dysfunction assessed by this technique correlates with measures of coronary endothelial dysfunction (CitationAnderson et al 1995). Peripheral vascular endothelial function can be assessed by straingauge venous impedance plethysmography. This technique examines the change in forearm blood flow in response to direct intra-arterial (brachial artery) administration of agonists. Non-invasive measures of arterial compliance and waveform morphology provide a marker of vascular health (CitationDeanfield et al 2005).
Molecular and cellular basis of endothelial dysfunction in diabetes
Hyperglycemia may lead to intracellular changes in the redox state resulting in depletion of the cellular NADPH pool. Accumulation of AGEs, whose formation is closely linked to oxidative stress, and resultant endothelial dysfunction may start early in the course of type 1 diabetes (CitationTsukahara et al 2003). Diminished capacity of nitric NOS to generate NO has been demonstrated experimentally when endothelial cells (ECs) were exposed either in-vitro or in-vivo to a diabetic environment (CitationArbogast et al 1982; CitationAanderud et al 1985; CitationKoh et al 1985; CitationLorenziet al 1986; CitationHattori et al 1991; CitationNordt et al 1993; CitationAvogaro et al 1999; CitationCipolla 1999; Salvolini et al 1999).
Over expression of growth factors has also been implicated as a link between diabetes and proliferation of both endothelial cells and vascular smooth muscle, possibly promoting neovascularization. Chronic hyperglycemia leads to non-enzymatic glycation of proteins and macromolecules (CitationJorge et al 2001). Insulin appears to regulate shedding or clearance of vascular adhesion protein-1 VAP-1, and an increase in sVAP-1. Therefore; absolute or relative insulin deficiency may be directly involved in the pathogenesis of diabetic angiopathy (CitationSalmi et al 2002).
The diabetic state is typified by an increased tendency for oxidative stress and high levels of oxidized lipoproteins, especially the so-called small dense low density lipoprotein (LDL-C). High levels of fatty acids and hyperglycemia have both been shown to induce an increased level of oxidation of phospholipids as well as proteins. The diabetic state in humans is associated with a prothrombotic tendency as well as increased platelet aggregation; furthermore TNF has been implicated as a link between insulin resistance, diabetes and endothelial dysfunction. The hypothesis has been advanced in recent years that insulin and/or insulin precursors may be atherogenic (CitationJorge et al 2001). Recent study suggests that E-selectin may enhance CAD prediction beyond traditional risk factors or markers of oxidative stress in Type 1 diabetes (CitationCostacou et al 2005). Furthermore elevated circulating asymmetric dimethylarginine ADMA may contribute to the excess cardiovascular morbidity and mortality in early diabetic nephropathy (CitationTarnow et al 2004). In addition adverse metabolic stress factors in type 1 diabetes are associated with reduced angiogenicity, endothelial progenitor cells EPC numbers and function (by 44%) compared with age and sex matched control subjects (P < 0.001). This reduction was inversely related to levels of HbA (1c) (R = −0.68, P = 0.01) using an in-vitro angiogenesis assay (CitationLoomans et al 2004).
Role of adhesion molecules has been clarified in the last few years. Elevated level of slCAM-1 in young diabetic patients correlates with metabolic compensation and positive family history of cardiovascular diseases. sVCAM-1 level in diabetic children correlates significantly positively with body mass index (BMI). Evaluation of adhesion molecules levels can be useful tool in the observation of the dynamic development of early phases of atherosclerotic process in young patients with type 1 diabetes (CitationGlowinska et al 2003).
We have reviewed all experimental and clinical studies from 1982–2006 that evaluated endothelial dysfunction in diabetic patients; most of which were prospective studies. Most of these studies in human indicate that endothelial dysfunction is closely associated to microangiopathy and atherosclerosis in diabetic patients.
Endothelial dysfunction in IDDM
The association between diabetes and endothelial dysfunction is particularly true in patients with type 1 diabetes who have either early (microalbuminuria) or late (macroalbuminuria) nephropathy. A variety of markers indicate endothelial dysfunction including: poor EC-dependent vasodilation, increased blood levels of von Willebrand factor (vWF), thrombomodulin, selectin, PAI-1, type IV collagen and t-PA were demonstrated in this patients population (CitationYaqoob et al 1993; CitationDosquet et al 1994; CitationMyrup et al 1994; CitationMakimattila et al 1996; Huszka et al 1997; Cosentino and Luscher 1998; Elhadd et al 1998; Malamitsi et al 1998; CitationHuvers et al 1999). Endothelial dysfunction was an early manifestation of vascular disease in type 2 diabetes but late in the course of type 1 diabetes (CitationClarkson et al 1996), furthermore studies have shown that the levels of cVCAM-1 were more markedly elevated in type 1 diabetes patients with diabetic retinopathy than in those patients with micro- or macroalbuminuria, whereas no difference in cICAM-1 and cELAM-1 levels was apparent regarding the clinical status of diabetic microangiopathy (CitationFasching et al 1996). In diabetic subjects, endothelium-dependent vasodilation correlated inversely with serum insulin concentration but not with glucose concentration, glycosylated hemoglobin, or duration of diabetes (CitationJohnston et al 1993). In a 10 year prospective study of 209 insulin-dependent diabetic patients with normal urinary albumin excretion has demonstrated coincidence of microalbuminuria and decreasing high density lipoprotein cholesterol, but no coincidence between onset of microalbuminuria and endothelial dysfunction assessed by von Willebrand factor (CitationMyrup et al 1994; CitationHadi et al 2005). Little is known about the formation and accumulation of AGEs in young patients with type 1 diabetes. Patients with microalbuminuria (> or = 15 mg/g Cr) showed significantly higher levels of pentosidine and pyrraline, and markers of oxidative stress, 8-hydroxy-2’-deoxyguanosine (8-OHdG) and acrolein-lysine than did normoalbuminuric patients and control. Of these four markers, urinary concentrations of pentosidine, 8-OHdG, and acrolein-lysine were significantly higher in the patients with diabetes than in the healthy control subjects (CitationTsukahara et al 2003).
In another study a significantly raised mean concentration of a free N-terminal fibronectin 30-kDa domain was found in plasma of diabetic patients with proliferative retinopathy as compared with healthy persons, and a positive correlation was observed between free N-terminal fibronectin and vWF and the degree of albuminuria. No relationship was found between fibronectin and the degree of control of diabetes (CitationSkrha et al 1990). In Participants from the Epidemiology of Diabetes Complications (EDC) cohort, a 10-year prospective study of childhood-onset Type 1 diabetes. Mean age at baseline was 28 years, and diabetes duration was 19 years. It has been found cellular adhesion molecules E-selectin may enhance CAD prediction beyond traditional risk factors or markers of oxidative stress in Type 1 diabetes (CitationCostacou et al 2005).
Impaired FMD response is a common manifestation in children with type 1 diabetes and is associated with increased carotid artery intimae media thickness (IMT). Which may predispose them to the development of early atherosclerosis (Jarvisalo et al 2005). Although small dense LDL and oxidized LDL are features of type 2 diabetes and predict the development of coronary artery disease, their role in type 1 diabetes is less clear. One study has suggested, but do not prove, that LDL particle size and LDL vitamin E may be determinants of conduit and resistance vessel endothelial vasodilator function in type 1 diabetes. Further work will be required to prove cause and effect (CitationSkyrme-Jones et al 2001).
It is well known that pregnant women with diabetes mellitus have a higher incidence of adverse pregnancy outcomes. This issue has been assessed in a study which has found that the arteries obtained from the diabetic pregnant women did not demonstrate any difference in either endothelial or smooth muscle function when compared with non-diabetic pregnant women. The contribution of NO to endothelium-dependent relaxation was approximately 20% in the pregnant women regardless of whether they were diabetic, and approximately 11% in the non-pregnant women (CitationAng et al 2002). In contrary in another small study the result of which need further confirmation has found that although pregnancy enhances microvascular function, but in women with diabetes, such improvements are insufficient to attain responses seen in healthy non pregnant women. And a persistent vascular defect in young women with type 1 diabetes that may contribute to adverse pregnancy outcome (CitationRamsay et al 2003).
Endothelial dysfunction, as estimated by plasma vWF concentration, but not fibrinogen, precedes and may predict the development of microalbuminuria in IDDM (CitationStehouwer et al 1995; CitationVerrotti et al 2003). The presence of endothelial dysfunction in normoalbuminuric diabetic patients suggests it could precede microalbuminuria as an early risk marker for cardiovascular disease (CitationDogra et al 2001). Recently a small study shows the vasomotor endothelial function in patients with diabetes mellitus (DM) type 1 at different stages of diabetic nephropathy (DN). ie, without renal affection, stage of microalbuminuria (MAU), proteinuria (PU), and chronic renal failure (CRF).in 26 patients with DM type 1 (11 males and 15 females, mean age 25.9 +/− 4.3 years, mean history of DM 12.9 +/− 3.4 years) and 7 healthy volunteers as control group. Endothelium-dependent vasodilation (EDVD) was assessed using test with reactive hyperemia provoked by 4−5 min occlusion of the brachial artery by pneumocollar and subsequent assessment of arterial diameter changes after decompression using high-resolution ultrasound dopplerography conclude that at the earliest stage of diabetic nephropathy (stage MAU), EDVD is not affected as maximal vasodilation of the brachial artery and endothelial sensitivity to shift tension do not differ from the control values. This means that the stage of MAU is reversible in early treatment, but proteinuria and chronic renal failure are not reversible stages associated with depletion of endothelial cells and loss of sensitivity to changing hemodynamic conditions (CitationShestakova et al 2003). The role of endothelial dysfunction in the development and progression of cardio-renal syndrome in 93 patients with type 1 diabetes mellitus were studied by same investigator and analyzed endothelial flow-mediated dilation of the brachial artery, levels of endothelin-1, von Willerbrand factor, C-reactive protein, renal:albumin and protein excretion rates, glomerular filtration rate (GFR), and cardiovascular functions (ECG, echocardiography, blood pressure monitoring). GFR correlated positively with the coefficient of sensitivity of endothelium to shear stress. Found a positive correlation between BP, permeability of glomerular filter and endothelial dysfunction markers and negative correlation with the coefficient of sensitivity of endothelium to shear stress and GFR. Left ventricle mass correlated with markers of endothelial dysfunction and stage of renal disease (CitationShestakova et al 2005b).
More severe diabetic nephropathy was associated with higher prevalence of cardiac pathology. Frequency of ischemic heart disease was 13%, 33% and 53%, frequency of left ventricular concentric hypertrophy and remodeling 33%, 40% and 60% among patients with microalbuminuria, proteinuria and chronic renal failure, respectively. Abnormalities of 24-hour blood pressure rhythm as well as signs of endothelial dysfunction were more pronounced in patients with more severe nephropathy. Correlation analysis revealed significant relationships between markers of endothelial dysfunction, parameters of renal function, blood pressure level and mass of left ventricular myocardium. (CitationShestakova et al 2005a). Low plasma levels of active TGF-beta are associated with an impaired endothelial response and this may provide a useful tool for identifying Type 1 diabetic patients at a greater risk of coronary artery disease (CitationMeeking et al 1999).
It is the general consensus that the occurrence of endothelial cell dysfunction in type 1 diabetes signifies a very high risk of micro- and macroangiopathy and although the diabetic state predisposes to endothelial cell dysfunction in this disease, is not sufficient to cause it. More likely, other agents (genes, environment) are likely to play a role in determining those patients that will develop aggressive angiopathy and hence endothelial cell dysfunction. Irrespective of whether endothelial cell dysfunction is a cause or a consequence of vascular injury in type 1 diabetes, therapeutic efforts aimed at restoring endothelial cell to normal will more likely have an affect on the natural history of vasculopathy in type 1 diabetes (CitationJorge et al 2001).
Plasma homocysteine levels in type 1 diabetes and endothelial dysfunction
Although the findings are inconsistent, moderate hyperhomocysteinaemia (15–30 μmol/l) has been observed in some studies of patients with type 1 diabetes. Adolescent patients with no microvascular complications have lower (CitationChiarelli et al 2000; CitationCotellessa 2001; CitationWiltshire et al 2001) or similar (CitationPavia et al 2000) homocysteine levels compared with non-diabetic controls. Studies in adult patients have demonstrated similar (CitationHultberg et al 1991; CitationChico et al 1998; CitationVaccaro et al 2000), lower (CitationRobillon et al 1994; CitationCronin et al 1998) and higher (CitationHofmann 1998; CitationTargher et al 2000) plasma homocysteine levels compared with non-diabetic controls. The homocysteine levels are independent of vitamin status and reflect the heterogeneous nature of the patients studied, including patients with poor glycaemic control, variable duration of diabetes and a variety of microvascular and macrovascular complications. It would appear that certain subgroups are more likely to be associated with hyperhomocysteinaemia; several factors have suggested: General factors; include genetic, nutrition, increasing age, male gender and renal failure. Factors specific to type 1 diabetes such as a lower age of onset of diabetes, poor glycaemic control, renal hyperfiltration and diabetic nephropathy. The interpretation of the result of these studies should be taken cautiously and further extensive work is needed to finalize this issue.
Endothelial dysfunction in NIDDM
The role of endothelial dysfunction in type 2 diabetes is more complicated than that for type 1. The effects of ageing, hyperlipidemia, hypertension and other factors add to the complexity of the problem. In contrast to patients with type 1 diabetes, endothelial dysfunction can also occur in patients with type 2 diabetes even when the patients have normal urinary albumin excretion. In fact, markers of endothelial dysfunction are often elevated years before any evidence of microangiopathy becomes evident (CitationJanka 1985; CitationHsueh and Anderson 1992; CitationBloomgarden 1998; CitationDe Mattia et al 1998; CitationNeri et al 1998; CitationWatts and Playford 1998; CitationGazis et al 1999). The insulin resistance syndrome encompasses a subnormal response to insulin-mediated glucose disposal and frequently elevated blood pressure, hyperlipidemia and dysfibinolysis, even without any clinically demonstrable alteration in plasma glucose concentrations (CitationSteinberg et al 1994). There is a growing body of evidence to suggest the coexistence of insulin resistance and endothelial dysfunction. Insulin-induced vasodilation, which is partially mediated by NO release, is impaired in obese individuals who do not have type 2 diabetes but whom display insulin resistance (CitationSteinberg et al 1994; Ferri et al 1997; CitationCleland et al 2000). Moreover, the obese state, a model of human insulin resistance, is associated with high levels of endothelin in plasma. Also blood concentrations of PAI-1 are high in patients with otherwise uncomplicated obesity (CitationCalles et al 1996). Endothelial activation and acute-phase reaction correlate with insulin resistance and obesity in type 2 diabetic patients (CitationLeinonen et al 2003).
Abnormalities in vascular reactivity and biochemical markers of endothelial cell activation are present early in individuals at risk of developing type 2 diabetes. The vasodilatory responses to acetylcholine were reduced in healthy normoglycemic subjects who have first degree diabetic relatives. The plasma levels of endothelin-1 were significantly higher in subjects with impaired glucose tolerance and patients with type 2 diabetes without vascular complications compared with healthy normoglycemic subjects with no history of type 2 diabetes in a first-degree relative (CitationCaballero et al 1999). In addition there is a significant association between endothelial dysfunction and insulin resistance in young first degree relatives of DM subjects independent of the classic cardiovascular risk factors (CitationBalletshofer et al 2000).
In a case-cohort study, using the Monitoring of Trends and Determinants in Cardiovascular Disease (MONICA)/Cooperative Research, men and women with elevated levels of sE-selectin had a significantly increased risk of type 2 diabetes after multivariable adjustment. Hazard ratios (95% CIs) comparing tertile extremes of sE-selectin were 2.63 (1.79–3.88) and 1.71 (1.07–2.75) for men and women, respectively. Elevated levels of sICAM-1 were also associated with an increased risk of type 2 diabetes; however, the association was not independent of other diabetes risk factors including E-selectin, while vWF was not associated with risk of type 2 diabetes (CitationThorand et al 2006). A prospective, nested case-control study within the Nurses’ Health Study, has found elevated E-selectin and ICAM-1 levels can predict incident diabetes in logistic regression models conditioned on matching criteria and adjusted for body mass index (BMI), family history of diabetes, smoking, diet score, alcohol intake, activity index and postmenopausal hormone use. Adjustment for waist circumference instead of BMI or further adjustment for baseline levels of C-reactive protein, fasting insulin, and HbA1c or exclusion of cases diagnosed during the first 4 years of follow-up did not alter these associations (CitationMeigs et al 2004).
In diabetes, glycation, tissue oxidation and endothelial function are all abnormal and predisposing to microvascular complications but interrelationships are complex with glycation appearing most direct (CitationWen et al 2002). The patients with microalbuminuria, unlike those without it, are characterized by longer course of diabetes, more pronounced lipid exchange disorder, more variable arterial pressure, higher pressure load index, elevated activity of lipid peroxidation (LP) processes and prominent disorder of NO-producing endothelial function. All improve with treatment (CitationAmetov et al 2005). The Endothelium-dependent vasodilation was impaired in the microalbuminuric patients compared with the normoalbuminuria patients and the healthy controls. Plasma PAI-1 and vWF levels increased in the microalbuminuric patients compared with the levels in the normoalbuminuric patients and in the healthy controls (CitationYu et al 2004).
In type 2 diabetes mellitus as in type 1, increased calpain (calcium-dependent protease) activity in response to hyperglycemia may play a role in diabetic cardiovascular disease. Immunoprecipitation studies revealed that glucose induces loss of NO via a calpain-dependent decrease in the association of hsp90 with endothelial NOS. In addition, inhibition of calpain activity decreased endothelial cell surface expression of the pro-inflammatory adhesion molecules ICAM-1 and VCAM-1 during hyperglycemia (CitationStalker et al 2003). Furthermore inhibition of PKC activity reduces leukocyte-endothelium interactions by suppressing surface expression of endothelial cell adhesion molecules in response to increased oxidative stress (CitationBooth et al 2002).
In diabetes associated with diabetic microangiopathy, compared with non diabetics, asymmetric dimethylarginine [ADMA]; an endogenous inhibitor of NOS, serum TNF-alpha and soluble TNF receptor I (sTNFR-I) has been assessed in a study which concludes that the serum sTNFR-I and VEGF levels were significantly increased, but no difference in the serum TNF-alpha, sTNFR-II, and ADMA levels between uncomplicated diabetic patients and in non diabetics (CitationMakino et al 2005).
Increased levels of vWF antigen, t-PA antigen and PAI-1 activity were seen in impaired glucose tolerance (IGT) and diabetics compared with the normal glucose tolerance (NGT). Tissue factor pathway inhibitor TFPI activity and thrombomodulin levels were increased in all elderly subjects, with positive association between HbA (1c), TFPI activity and vWF antigen. Fasting blood glucose levels correlated with vWF antigen, t-PA antigen and PAI-1 activity, whereas urine albumin excretion correlated with TFPI activity, vWF antigen and PAI-1 activity. Serum insulin levels correlated strongly not only with vWF antigen and t-PA antigen but also with PAI-1 activity. This correlation did not change after further adjustment for serum glucose and HbA(1c), which may suggest that in the elderly subjects, impaired fibrinolysis is probably associated with insulin resistance (CitationLeurs et al 2002). The above reflect a prothrombotic state associated with an insulin resistance state, an increased vWF release, raised sP-Sel and TNFalpha levels and, may be, low NO bioavailability, which could lead to a higher risk of development of thrombotic events in hypertensive diabetic patients (CitationOuvina et al 2001).
NADPH oxidase gene expression is increased in circulating lymphomonocytes from patients with DM, and this increased gene expression is dependent upon metabolic control. Hyperglycemia can mediate its adverse effects through the activation of protein kinase C. Recent study has shown an increase in membrane-associated PKC beta 2 activity in monocytes from patients with DM. This activity was reduced by 40% in the euglycemic condition (CitationAvogaro et al 2006). Further more patients with Type 2 diabetes with good residual C-peptide secretion are better protected from endothelial dysfunction that those with poor C-peptide secretion (CitationManzella et al 2003).
Endothelial dysfunction may have deleterious effect cardiovascular pathology in diabetic patients. Recent study found a significant association between an abnormal SPECT result, left ventricular diastolic dysfunction and impaired post-ischaemic dilatation of the brachial artery. No association was found between the SPECT result, systolic function and left ventricular hypertrophy, however, an abnormal SPECT result was significantly associated with left ventricular diastolic dysfunction and the deterioration of post-ischaemic dilatation of the brachial artery in asymptomatic patients with type 2 diabetes (CitationCharvat et al 2005). Myocardial blood flow (MBF) measured with positron emission tomography and 13N-ammonia to characterize coronary circulatory function in states of insulin resistance without carbohydrate intolerance (IR), impaired glucose tolerance (IGT), normotensive and hypertensive type 2 diabetes mellitus (DM) compared with insulin-sensitive (IS) individuals shows that endothelium-dependent coronary vasomotion was significantly diminished in IR (–56%), as well as in IGT and normotensive and hypertensive diabetic patients (−85%, −91%, and −120%, respectively). Total vasodilator capacity was similar in normoglycemic individuals (IS, IR, and IGT), whereas it was significantly decreased in normotensive (−17%) and diabetic, hypertensive (–34%) patients (CitationPrior et al 2005).
The phospho-Akt (Thr308) level in arteries from diabetic patients was reduced to about one-half of the level in non diabetic patients, suggesting impaired insulin signaling in human diabetic vascular tissue. Augmented vasoconstriction was observed in diabetic arteries, due in part to deficiency of basal and stimulated NO production. This correlated with decreased endothelial NOS expression and activity in diabetic vessels (CitationOkon et al 2005). The evaluation of enzymes implicated in the evolution of endothelial dysfunction associated with type 2 diabetes [lipoprotein-associated phospholipase A2, meloperoxidase (MPO) and paraoxonase (PON) activities] , may improve early diagnosis of CVD in asymptomatic patients with type 2 diabetes and can help to evaluate accelerated atherosclerosis and microvascular disease (CitationMoldoveanu et al 2006). A study recently, using high-resolution ultrasound, measured brachial artery responses to flow-mediated vasodilatation; (endothelium-dependent vasodilatation) and nitroglycerine-induced vasodilatation; (endothelium-independent vasodilatation), compares non-traditional risk factors, such as endothelial function, plasma levels of CRP and adiponectin were measured by ELISA in Type 2 diabetic and non-diabetic patients following acute myocardial infarction. Twenty Type 2 diabetic patients were compared with 25 non-diabetic patients at baseline (1–3 days from the onset of chest pain) and at 60 days follow-up after an AMI. At 60 days follow-up, there were significant differences in FMD (1.5 compared with 4.1%; P < 0.02), CRP (4.23 compared with 1.46 mg/ml; P < 0.01) and adiponectin (3.3 compared with 5.3 ng/ml; P < 0.05) levels between Type 2 diabetic and non-diabetic patients. These findings may, in part explain, the poor outcome in coronary artery disease seen in Type 2 diabetes (CitationNystrom et al 2005). Type 2 diabetes is independently associated with impaired flow mediated dilatation (FMD). Hyperglycemia and hyperinsulinemia contribute minimally to this association. Impaired FMD may therefore, in part, explains the increased cardiovascular disease risk in DM2, whereas the normal FMD in impaired glucose metabolism (IGM) suggests that other forms of endothelial dysfunction are important in explaining the increased cardiovascular disease risk in IGM (CitationHenry et al 2004). On the other side, acute hyperinsulinaemia, both with and without concomitant hyperglycaemia, does not increase skin microvascular permeability, haemodynamics or parameters of endothelial dysfunction in Type 2 diabetic patients (CitationOomen et al 2004).
Patients with diabetes or hypertension have elevated ET-1 levels, but do not exhibit positive correlations between ET-1 levels and blood pressure, which was observed in healthy controls. Increased ET-1 levels do not induce hypertension in diabetes, but were lower in diabetic patients taking ACE inhibitors compared to those without ACE inhibitors. There is no significant association between ET-1 levels and vascular complications. These findings suggest that the plasma ET-1 level is not a marker of endothelial dysfunction but changes in plasma ET-1 levels may precede vascular complications associated with hypertension and diabetes (CitationSchneider et al 2002). The same author studied plasma endothelin-1 (ET-1) levels in patients with diabetes mellitus or hypertension with healthy controls, and investigates whether ET-1 levels are correlated with glycemic control, metabolic parameters and vascular complications on 103 patients with type 1 diabetes, 124 patients with type 2 diabetes, 35 hypertensive patients without diabetes mellitus and 99 controls. Patients with diabetes or hypertension have elevated ET-1 levels, but do not exhibit positive correlations between ET-1 levels and BP, which was observed in healthy controls. Increased ET-1 levels do not induce hypertension in diabetes, but were lower in diabetic patients taking ACE inhibitors compared to those without ACE inhibitors. There is no significant association between ET-1 levels and vascular complications (Schneider et al 2005). Furthermore the activity of endogenous ET-1 on ET (A) receptors is enhanced in the resistance vessels of patients with diabetes, whereas their sensitivity to exogenous ET-1 is blunted (CitationCardillo et al 2002).
Well-controlled type 2 diabetic patients free of clinical macrovascular complications have elevated plasma markers of cardiovascular risk without having increased intima-media thickness (IMT). The elevation of plasma markers of endothelial cell activation (sE-selectin and s-ICAM-1) or inflammation (CRP) and oxidative stress (8-isoprostane) in diabetics vs. controls is distinct from and cannot be explained simply by differences in the burden of atherosclerosis as assessed by carotid intima-media thickness (CitationMoussavi et al 2004). Activation of poly (ADP-ribose) polymerase (PARP) is an important factor in the pathogenesis of endothelial dysfunction in diabetes. Destruction of islet cells with streptozotocin in mice induced hyperglycemia, intravascular oxidant production, DNA strand breakage, PARP activation and a selective loss of endothelium-dependent vasodilation. Treatment with a novel potent PARP inhibitor, starting after the time of islet destruction, maintained normal vascular responsiveness, despite the persistence of severe hyperglycemia (CitationGarcia Soriano et al 2001).
Possible available therapy
Several therapeutic interventions have been tested in clinical trials aimed at improving endothelial function in patients with diabetes (). Insulin sensitizers may have a beneficial effect in the short term, but the virtual absence of trials with cardiovascular end-points precludes any definitive conclusion. Two trials offer optimism that treatment with angiotensin converting enzyme inhibitors may have a positive impact on the progression of atherosclerosis (CitationO’Driscoll et al 1997, CitationMullen et al 1998; CitationPrasad et al 2000; CitationHornig et al 2001), although widely used, the effect of hypolipidemic agents on endothelial function in diabetes is not clear (CitationEvans et al 2000). The role of antioxidant therapy is controversial.
Table 2A Role of various modalities of therapy on endothelial dysfunction
Chronic cigarette smoking has a deleterious effect on plasma cICAM-1 levels in young type 1 diabetic patients, which further supports the clinical importance of discouraging the initiation of smoking and promoting its cessation in people with type 1 diabetes (CitationZoppini et al 1999).
Children with type 1 diabetes have early endothelial dysfunction. Better folate status is associated with better endothelial function, as measured by higher FMD, higher FMD:GTN ratio, and lower thrombomodulin. Folate may therefore protect against endothelial dysfunction in children with diabetes (CitationWiltshire et al 2002).
Elevation in blood glucose and total glycosylated hemoglobin in diabetic animals was normalized after islet transplantation. Furthermore, islet transplantation completely restored the defective endothelium-dependent relaxation to acetylcholine in diabetic (CitationPieper et al 1995, Citation1996). Post-prandial state is accompanied by endothelial dysfunction in Type 2 diabetic patients and that insulin aspart improved endothelial function (CitationCeriello et al 2004). Few studies have shown the beneficial effect of insulin on endothelial dysfunction (). Long-term treatment with hydroxymethyl starch conjugated-deferoxamine had no effect on relaxation to nitroglycerin but completely prevented the impaired relaxation to acetylcholine in diabetic rats (CitationPieper and Siebeneich 1997).
Inhibition of rennin angiotensin pathway ()
Angiotensin II has several pro-oxidative effects on the vasculature, decreasing NO bioavailability and resulting in vascular injury. ACE inhibitors are known to improve endothelial dysfunction, but the ability of angiotensin receptor blockers to improve endothelial dysfunction is less clear (CitationMancini et al 1996; CitationTaddei et al 2002). Both drug classes consistently prevent coronary artery (particularly in the case of ACE inhibitors), stroke, and diabetic microvascular complications of nephropathy and retinopathy (CitationMcFarlane et al 2003). Inhibition of the renin-angiotensin system is associated with reduced incidence of new-onset diabetes. In the Heart Outcomes Prevention Evaluation (HOPE) study (CitationYusuf et al 2001), the incidence of diabetes was 32% lower in the ramipril-treated group than in the placebo group. In the Losartan Intervention for Endpoint reduction in hypertension (LIFE) study (CitationDahlof et al 2002), losartan was associated with 25% less new-onset diabetes compared with atenolol. The mechanisms responsible for the reduced incidence of diabetes observed during these trials are unknown, although possible mechanisms include increased plasma bradykinin levels, which improves insulin-mediated glucose uptake (CitationDuka et al 2001), improved endothelial function, increased vascular NO activity and reduced vascular inflammation. More recent study in Chinese investigates the relationship between angiotensin converting enzyme (ACE) gene and endothelial dysfunction, concludes that, ACE DD genotype is related to endothelium-dependent arterial dilation in the early stage of type 2 diabetes mellitus and in healthy individuals (CitationXiang et al 2004). Which may hope for gene therapy in the future?
Thiazolidinediones ()
Thiazolidinediones enhances insulin-mediated glucose uptake into insulin target tissues, through activation of peroxisome proliferator-activated receptor (PPAR) (CitationMudaliar et al 2001). They have direct effects on adipose tissue by suppression TNF and, possibly, leptin expression; suppress lipolysis and thus decrease plasma free fatty acid concentrations and increase plasma adiponectin levels (CitationHauner et al 2001, Citation2002) and exert direct effects on insulin-mediated glucose transport in skeletal muscle and the heart (CitationBishop-Bailey et al 2000; CitationLoviscach et al 2000).
Thiazolidinedione administration reverses insulin resistance and many components of the metabolic syndrome. Treatment is generally associated with increased HDL cholesterol levels; decreased blood pressure, plasma triglyceride levels, small dense LDL cholesterol particles, PAI-1 levels and albumin excretion rates; in addition to decreased glucose levels and reduced hemoglobin A1C levels (CitationDay 1999; CitationKruszynska et al 2000; CitationLebovitz et al 2001; CitationFreed et al 2002).
PPAR ligands also improve endothelial function (CitationDandona and Aljada 2004). Several studies have demonstrated improvements in brachial artery reactivity in patients with diabetes. (CitationAvena et al 1998; CitationCaballero et al 2003). Troglitazone (CitationWatanabe et al 2000) and Rosiglitazone, improves coronary artery endothelial function in patients with insulin resistances who have no traditional risk factors for atherosclerosis as well as no impaired glucose tolerance or diabetes (CitationQuiñones et al 2002). With an increase in insulin sensitivity and a drop in fasting insulin and free fatty acid levels, thiazolidinediones in combination with hormone therapy (HT) in postmenopausal women is, however, have shown in study to attenuates endothelial function (CitationHonisett et al 2004).
The mechanisms by which thiazolidinediones improve endothelial-dependent blood flow are unknown, but likely involve several effects. First, as described above; it has an important anti-inflammatory effects that involve decreasing circulating adipokines levels (eg, TNF, PAI-1, leptin), which are reflected by reduced high-sensitivity C-reactive protein levels; increasing adiponectin levels; decreasing vascular expression of adhesion molecules (CitationWakino et al 2002). Second, insulin is a vasodilator stimulating expression of eNOS through the phosphatidylinositol 3-kinase (PI3K) pathway (CitationZeng et al 2000). This effect of insulin is blunted in patients with insulin resistance (CitationKuboki et al 2000). PPAR- is expressed in endothelial cells, and its ligands have been reported to enhance NO production, possibly by stimulating the PI3K pathway and hence expression of eNOS (CitationKim et al 2002). Third, PPAR- ligands improve several components of the metabolic syndrome that could adversely affect endothelial function, including low HDL cholesterol levels, high triglyceride and free fatty acid levels, hypertension and carbohydrate intolerance. PPAR- ligands also decrease oxidative stress and thus are able to improve the vascular balance between NO and vasoconstrictors (CitationBagi et al 2004). Rosiglitazone administration for 12 weeks was shown to improve insulin sensitivity and decrease asymmetric dimethylarginine levels. An endogenous inhibitor of NOS, is associated with reduced NO–mediated vasodilation and enhanced adherence of mononuclear cells to the endothelium (CitationChan et al 2000; CitationStuhlinger et al 2002). In recently performed a double-blind crossover trial of 12 patients with recently diagnosed type 2 diabetes concludes that insulin resistance is a major contributor toward endothelial dysfunction in type 2 diabetes; both endothelial dysfunction and insulin resistance are amenable to treatment by rosiglitazone (CitationPistrosch et al 2004). Recently studies have shown that Rosiglitazone ameliorated glomerular hyperfiltration in early type 2 diabetes, improved NO bioavailability and lessened renal end-organ damage in type 2 diabetes with microalbuminuria (CitationPistrosch et al 2005) and Pioglitazone improves endothelial dysfunction independently from the observed benefits on insulin sensitivity and beta-cell function in patients with newly diagnosed type 2 diabetes and CAD.and may exerts additional effects on endothelial function beyond metabolic control (CitationForst et al 2005; CitationSourij et al 2006). Furthermore the GATE study may provide the rationale and impetus for the aggressive treatment of insulin-resistant patients with glitazone therapy (CitationHubacek et al 2004).
Other antidiabetic
Repaglinide administration, through good control of postprandial glucose levels, improves brachial reactivity and declines oxidative stress indexes (CitationManzella et al 2005). While Nateglinide an oral antidiabetic insulinotropic agent neither improved nor impaired myocardial blood flow in Type 2 diabetic patients (CitationBengel et al 2005). Metformin; an antidiabetic agent that improves insulin sensitivity, treatment improved both insulin resistance and endothelial function, in animal and human (CitationKatakam et al 2000; CitationMather et al 2001).
Statin and endothelial dysfunction ()
Several clinical trials have demonstrated that statin treatment not only reduces serum cholesterol levels in hypercholesterolemic patients, but also substantially decreases the risk of cardiovascular disease (CitationShepherd et al 1995). In current clinical use, statins can reduce LDL cholesterol levels by an average of 20%–35%, with a corresponding 30%–35% reduction in major cardiovascular outcomes. Decreases in serum cholesterol levels could account for the observed risk reduction, since LDL cholesterol has a strong, well-documented association with cardiovascular risk, and since plasma LDL apheresis has been shown to improve both endothelium-dependent vasodilation and cardiovascular risk in hypercholesterolemic patients (CitationThompson et al 1995; CitationTamai et al 1997). Several studies, however, have shown that improvements in endothelial function can occur before reductions in serum cholesterol levels. For example, cerivastatin has been shown to improve endothelial function in elderly diabetic patients within 3 days, while, even more strikingly, healthy normocholesterolemic subjects have demonstrated markedly improved endothelial vasoreactivity after 3 hours (CitationTsunekawa et al 2001; CitationOmori et al 2002). These acute effects are in agreement with other studies that have reported improvements in endothelial function after statin administration that do not correlate with reductions in serum LDL cholesterol levels (Kureishi et al 2000). Statins decrease high-sensitivity C-reactive protein levels by 30%–40%, independent of their cholesterol lowering capacities (CitationAnsell et al 2003). Recent evidence also suggests that statins can improve insulin sensitivity. Cerivastatin has been shown to improve insulin sensitivity, as determined by hyperinsulinemic-euglycemic clamp, in patients with type 2 diabetes after 3 months of treatment (CitationPaniagua et al 2002). A similar study, in which patients with impaired fasting glucose levels were treated with atorvastatin for 16 weeks, noted a trend towards improved insulin sensitivity in the treatment group, as determined by oral glucose tolerance test, but this trend failed to reach significance (CitationCosta et al 2003). Statin treatment did not, however, reduce the incidence of diabetes in at least one large prospective trial that addressed this question (CitationKeech et al 2003).
Table 2B Role of various modalities of therapy on endothelial dysfunction
Insulin therapy is it of help? ()
Low and high physiological hyperinsulinemia abolished endothelium-dependent vasodilation, whereas endothelium-independent vasodilation was unaffected. Vitamin C fully restored insulin-impaired endothelial function without affecting endothelium-independent vasodilation (CitationArcaro 2002). Other investigators concluded that insulin therapy partly restores insulin-stimulated endothelial function in patients with type 2 diabetes and ischemic heart disease (Rask et al 2001). Another studies investigate long-term effects of insulin glargine on vascular function in patients with type 2 diabetes, the result supports the idea that long-term insulin therapy has beneficial rather than harmful effects on vascular function in type 2 diabetes (CitationPaolisso and Giugliano 1996; Vehkavaara et al 2001).
Other modalities of therapy ()
Few sporadic studies has raised the Role of vitamins, the benefit of L-arginine , antioxidant , and hydroxyethyl starch conjugated-deferoxamine aerobic exercise training and Pancreatic cell transplantation, the benefit which need to clarified in more extensive studies.
Table 2C Role of various modalities of therapy on endothelial dysfunction
Where we are from endothelial dysfunction in diabetes mellitus?
We think that we still far from the core pathological process in endothelial dysfunction, extensive research together with randomized trial are needed in this entity especially in molecular biology and genetic engineering for more exploration of hidden aspect of iceberg. The future will witness increasing interest in finding reliable methods of testing endothelial function. As the measures of endothelial dysfunction become clinically applicable, this may translate into improved methods of risk assessment that help in predicting, preventing and treating cardiovascular disease. Inflammatory markers, such as CRP, will probably find their way into risk assessment; several therapeutic strategies aimed at improving endothelial function in diabetes mellitus states are under investigation. The future may holds great promise.
References
- AanderudSKraneHNordoyAInfluence of glucose, insulin and sera from diabetic patients on the prostacyclin synthesis in vitro in cultured human endothelial cellsDiabetologia19852864143905474
- Al SuwaidiJHiganoSTHolmesDRObesity is an independent predictor of coronary endothelial dysfunction in patients with normal or mildly diseased coronary arteriesJ Am Coll Cardiol200137152311345360
- AmetovASDemidovaTIuKosykhSANO synthesis in the vascular endothelium of patients with type II diabetesKlin Med (Mosk)200583862816218368
- AmmarRFJrGuttermanDDBrooksLAFree radicals mediate endothelial dysfunction of coronary arterioles in diabetesCardiovasc Res20004759560110963732
- AndersonTJAssessment and treatment of endothelial dysfunction in humansJ Am Coll Cardiol199934631810483941
- AndersonTJElsteinEHaberHComparative study of ACE-inhibition, angiotensin II antagonism, and calcium channel blockade on flow-mediated vasodilation in patients with coronary disease (BANFF study)J Am Coll Cardiol20003560610636260
- AndersonTJUehataAGerhardMDClose relation of endothelial function in the human coronary and peripheral circulationsJ Am Coll Cardiol1995261235417594037
- AngCHillierCJohnstonFEndothelial function is preserved in pregnant women with well-controlled type 1 diabetesBJOG200210969970712118651
- AnsellBJWatsonKEWeissREhsCRP and HDL Effects of Statins Trial (CHEST): rapid effect of statin therapy on C-reactive protein and high-density lipoprotein levels. A clinical investigationHeart Dis200352712549983
- ArbogastBWLeeGMRaymondTLIn vitro injury of porcine aortic endothelial cells by very-low-density lipoproteins from diabetic rat serumDiabetes19823159396819172
- ArcaroGCrettiABalzanoSInsulin causes endothelial dysfunction in humans: sites and mechanismsCirculation20021055768211827922
- ArcaroGZenereBMSaggianiFACE inhibitors improve endothelial function in type 1 diabetic patients with normal arterial pressure and microalbuminuriaDiabetes Care19992215364210480522
- ArnerPThe adipocyte in insulin resistance: key molecules and impact of the thiazolidinedionesTrends Endocrinol Metab2003141374512670740
- AvenaRMitchellMENylenESInsulinaction enhancement normalizes brachial artery vasoactivity in patients with peripheral vascular disease and occult diabetesJ VascSurg199828102432
- AvogaroACaloLPiarulliFEffect of acute ketosis on the endothelial function of type 1 diabetic patients: the role of nitric oxideDiabetes199948391710334319
- AvogaroAFadiniGPGalloAEndothelial dysfunction in type 2 diabetes mellitusNutr Metab Cardiovasc Dis200616Suppl 1S394516530129
- AvogaroAMiolaMFavaroAGemfibrozil improves insulin sensitivity and flow-mediated vasodilatation in type 2 diabetic patientsEur J Clin Invest200131603911454015
- BagiZKollerAKaleyGPeroxisome proliferator-activated receptor activation increases NO bioavailability in coronary arterioles in type 2 diabetes by reducing oxidative stressAm J Physiol HeartCirc Physiol2004286H7428
- BalletshoferBMRittigKEnderleMDEndothelial dysfunction is detectable in young normotensive first-degree relatives of subjects with type 2 diabetes in association with insulin resistanceCirculation20001011780410769277
- BastaGDel TurcoSDe CaterinaRAdvanced glycation endproducts: implications for accelerated atherosclerosis in diabetesRecenti Prog Med200495678015072391
- BeishuizenEDTamsmaJTJukemaJWThe effect of statin therapy on endothelial function in type 2 diabetes without manifest cardiovascular diseaseDiabetes Care20052816687415983318
- BengelFMAbletshauserCNeverveJEffects of nateglinide on myocardial microvascular reactivity in Type 2 diabetes mellitus – a randomized study using positron emission tomographyDiabet Med2005221586315660732
- BhargavaKHansaGBansalMEndothelium-dependent brachial artery flow mediated vasodilatation in patients with diabetes mellitus with and without coronary artery diseaseJ Assoc Physicians India200351355812723648
- BiegelsenESLoscalzoJEndothelial function and atherosclerosisCoron Artery Dis1999102415610376203
- BijlstraPJSmitsPLuttermanJAEffect of long-term angiotensin-converting enzyme inhibition on endothelial function in patients with the insulin-resistance syndromeJ Cardiovasc Pharmacol199525658647596136
- BilsboroughWO’DriscollGStantonKEffect of lowering tumour necrosis factor-alpha on vascular endothelial function in Type II diabetesClin Sci (Lond)2002103163912149108
- Bishop-BaileyDPeroxisome proliferator-activated receptors in the cardiovascular systemBr J Pharmacol20001298233410696077
- BlairAShaulPWYuhannaISOxidized low-density lipoprotein displaces endothelial nitric-oxide synthase (eNOS) from plasmalemmal caveolae and impairs eNOS activationJ Biol Chem1999274325121910542298
- BloomgardenZTEndothelial dysfunction, neuropathy and the diabetic foot, diabetic mastopathy, and erectile dysfunctionDiabetes Care19982118399538990
- BodenGShulmanGIFree fatty acids in obesity and type 2 diabetes: defining their role in the development of insulin resistance and beta celldysfunctionEur J Clin Invest200232Suppl 3142312028371
- BonnerGHyperinsulinemia, insulin resistance, and hypertensionJ Cardiovasc Pharmacol199424Suppl 2S39497898093
- BoothGStalkerTJLeferAMMechanisms of amelioration of glucose-induced endothelial dysfunction following inhibition of protein kinase C in vivoDiabetes20025115566411978656
- BrinerVALuscherTFRole of vascular endothelial abnormalities in clinical medicine: atherosclerosis, hypertension, diabetes, and endotoxemiaAdv Intern Med1994391228140952
- BusseRFlemingIHeckerMSignal transduction in endothelium-dependent vasodilatationEur Heart J199314Suppl I298293777
- CaballeroAEAroraSSaouafRMicrovascular and macrovascular reactivity is reduced in subjects at risk for type 2 diabetesDiabetes19994818566210480619
- CaballeroAESaouafRLimSCThe effects of troglitazone, an insulin-sensitizing agent, on the endothelial function in early and late type 2 diabetes: a placebo-controlled randomized clinical trialMetabolism2003521738012601628
- CacoubPCarayonADorentREndothelin: the vasoconstrictor of the 1990’s?Rev Med Interne199314229328378653
- Calles-EscandonJBallorDHarvey-BerinoJAmelioration of the inhibition of fibrinolysis in elderly, obese subjects by moderate energy intake restrictionAm J Clin Nutr1996647118669417
- CardilloCCampiaUBryantMBIncreased activity of endogenous endothelin in patients with type II diabetes mellitusCirculation20021061783712356630
- CerielloACavarapeAMartinelliLThe post-prandial state in Type 2 diabetes and endothelial dysfunction: effects of insulin aspartDiabet Med200421171514984453
- ChanJRBogerRHBode-BogerSMAsymmetric dimethylarginine increases mononuclear cell adhesiveness in hypercholesterolemic humansArterioscler Thromb Vasc Biol2000201040610764670
- ChappeyOWautierMPBovalBEndothelial cells in culture: an experimental model for the study of vascular dysfunctionsCell Biol Toxicol1996121992059034609
- CharvatJMichalovaKChlumskyJThe association between left ventricle diastolic dysfunction and endothelial dysfunction and the results of stress myocardial SPECT in asymptomatic patients with type 2 diabetesJ Int Med Res2005334738216222880
- ChaturvediNFullerJHPokrasFCirculating plasma vascular endothelial growth factor and microvascular complications of type 1 diabetes mellitus: the influence of ACE inhibitionDiabet Med2001182889411437859
- CheethamCO’DriscollGStantonKLosartan, an angiotensin type I receptor antagonist, improves conduit vessel endothelial function in Type II diabetesClin Sci (Lond)2001100131711115412
- CheethamsCCollisJO’DriscollGLosartan, an angiotensin type 1 receptor antagonist, improves endothelial function in non-insulin-dependent diabetesJ Am Coll Cardiol2000361461611079643
- ChenX-LTummalaPEOlbrychMTAngiotensin II induces monocyte chemoattractant protein-1 gene expression in rat vascular smooth muscle cellsCirc Res19988395299797345
- ChiarelliFPomilioMMohnAHomocysteine levels during fasting and after methionine loading in adolescents with diabetic retinopathy and nephropathyJ Pediatr20001373869210969265
- ChicoAPerezACordobaAPlasma homocysteine is related to albumin excretion rate in patients with diabetes mellitus: a new link between diabetic nephropathy and cardiovascular disease?Diabetologia199841684939662051
- ChowienczykPJBrettSEGopaulNKOral treatment with an antioxidant (raxofelast) reduces oxidative stress and improves endothelial function in men with type II diabetesDiabetologia200043974710990073
- CipollaMJElevated glucose potentiates contraction of isolated rat resistance arteries and augments protein kinase C-induced intracellular calcium releaseMetabolism19994810152210459567
- ClarksonPCelermajerDSDonaldAEImpaired vascular reactivity in insulin-dependent diabetes mellitus is related to disease duration and low density lipoprotein cholesterol levelsJ Am Coll Cardiol19962857398772741
- ClelandSJPetrieJRSmallMInsulin action is associated with endothelial function in hypertension and type 2 diabetesHypertension2000351 Pt 25071110642350
- ClemensAKlevesathMSHofmannMOctreotide (somatostatin analog) treatment reduces endothelial cell dysfunction in patients with diabetes mellitusMetabolism19994812364010535384
- CongerJDEndothelial regulation of vascular toneHosp Pract19942911726 (Off Ed)
- ContrerasFDiabetes and hypertension physiopathology and therapeuticsJ Hum Hypertens200014S263110854077
- CostaACasamitjanaRCasalsEEffects of atorvastatin on glucose homeostasis, postprandial triglyceride response and C-reactive protein in subjects with impaired fasting glucoseDiabet Med200320743512925055
- CostacouTLopes-VirellaMFZgiborJCMarkers of endothelial dysfunction in the prediction of coronary artery disease in type 1 diabetes. The Pittsburgh Epidemiology of Diabetes Complications StudyJ Diabetes Complications2005191839315993351
- CotellessaMMinnitiGCeroneRLow total plasma homocysteine concentrations in patients with type 1 diabetesDiabetes Care2001249697111347774
- CowanDBLangilleBLCellular and molecular biology of vascular remodelingCurr Opin Lipidol19967941008743902
- CroninCCMcPartlinJMBarryDGPlasma homocysteine concentrations in patients with type 1 diabetesDiabetes Care199821184379802731
- DahlofBDevereuxRBKjeldsenSECardiovascular morbidity and mortality in the Losartan Intervention For Endpoint reduction in hypertension study (LIFE): a randomised trial against atenololLancet2002359995100311937178
- Dalla NoraEPassaroAZamboniPFAtorvastatin improves metabolic control and endothelial function in type 2 diabetic patients: a placebo-controlled studyJ Endocrinol Invest20032673812602538
- DandonaPAljadaAEndothelial dysfunction in patients with type 2 diabetes and the effects of thiazolidinedione antidiabetic agentsJ Diabetes Complications2004189110215120703
- DarkoDDornhorstAKellyFJLack of effect of oral vitamin C on blood pressure, oxidative stress and endothelial function in Type II diabetesClin Sci (Lond)20021033394412241530
- DayCThiazolidinediones: a new class of antidiabetic drugsDiabet Med1999161799210227562
- De CobelliFFiorinaPPerseghinGL-arginine-induced vasodilation of the renal vasculature is preserved in uremic type 1 diabetic patients after kidney and pancreas but not after kidney-alone transplantationDiabetes Care2004279475415047654
- De MattiaGBraviMCLaurentiOReduction of oxidative stress by oral N-acetyl-L-cysteine treatment decreases plasma soluble vascular cell adhesion molecule-1 concentrations in non-obese, non-dyslipidaemic, normotensive, patients with non-insulin-dependent diabetesDiabetologia199841139269833950
- De MattiaGLaurentiOFavaDDiabetic endothelial dysfunction: effect of free radical scavenging in Type 2 diabetic patientsJ Diabetes Complication2003172 Suppl305
- De MeyerGRHermanAGVascular endothelial dysfunctionProg Cardiovasc Dis199739325429050818
- De VrieseASVerbeurenTJde VoordeJVEndothelial dysfunction in diabetesBritish Journal of Pharmacology20001309637410882379
- DeanfieldJDonaldAFerriCEndothelial function and dysfunction. Part I: Methodological issues for assessment in the different vascular beds: A statement by the Working Group on Endothelin and Endothelial Factors of the European Society of HypertensionJ Hypertens20052371715643116
- DheinSKabatAOlbrichAEffect of chronic treatment with vitamin E on endothelial dysfunction in a type I in vivo diabetes mellitus model and in vitroJ Pharmacol Exp Ther20033051142212649359
- DograGRichLStantonKEndothelium-dependent and independent vasodilation studies at normoglycaemia in type I diabetes mellitus with and without microalbuminuriaDiabetologia20014459360111380077
- DosquetCWautierMPGuillausseauPJMonokines and endothelial cell proliferation in patients with diabetes mellitusDiabete Metab19942037428056134
- DrabMVerkadePElgerMLoss of caveolae, vascular dysfunction, and pulmonary defects in caveolin-1 gene-disrupted miceScience200129324495211498544
- DukaIShenoudaSJohnsCRole of the B(2) receptor of bradykinin in insulin sensitivityHypertension20013813556011751717
- DumontASHyndmanMEDumontRJImprovement of endothelial function in insulin-resistant carotid arteries treated with pravastatinJ Neurosurg2001954667111565869
- DzauVJTissue angiotensin and pathobiology of vascular disease: a unifying hypothesisHypertension20013710475211304501
- ElliotTGCockcroftJRGroopPHInhibition of nitric oxide synthesis in forearm vasculature of insulin-dependentdiabetic patients: blunted vasosonstriction on patients with microalbuminuriaClin Sci (Lond)199385687938287660
- EvansMAndersonRAGrahamJCiprofibrate therapy improves endothelial function and reduces postprandial lipemia and oxidative stress in type 2 diabetes mellitusCirculation20001011773910769276
- EvansMAndersonRASmithJCEffects of insulin lispro and chronic vitamin C therapy on postprandial lipaemia, oxidative stress and endothelial function in patients with type 2 diabetes mellitusEur J Clin Invest200333231812641541
- FantuzziGFaggioniRLeptin in the regulation of immunity, inflammation, and hematopoiesisJ Leukoc Biol2000684374611037963
- FarhangkhoeeHKhanZAKaurHVascular endothelial dysfunction in diabetic cardiomyopathy: Pathogenesis and potential treatment targetsPharmacol Ther20061113849916343639
- FarouqueHMMeredithITThe assessment of endothelial function in humansCoron Artery Dis2001124455411696683
- FaschingPVeitlMRohacMElevated concentrations of circulating adhesion molecules and their association with microvascular complications in insulin-dependent diabetes mellitusJ Clin Endocrinol Metab1996814313178954033
- FeganPGShoreACMawsonDMicrovascular endothelial function in subjects with Type 2 diabetes and the effect of lipid-lowering therapyDiabet Med2005221670616401310
- ForstTLubbenGHohbergCInfluence of glucose control and improvement of insulin resistance on microvascular blood flow and endothelial function in patients with diabetes mellitus type 2Microcirculation2005125435016207627
- FreedMIRatnerRMarcovinaSMEffects of rosiglitazone alone and in combination with atorvastatin on the metabolic abnormalities in type 2 diabetes mellitusAm J Cardiol2002909475212398960
- Fuchsjager-MayrlGPleinerJWiesingerGFExercise training improves vascular endothelial function in patients with type 1 diabetesDiabetes Care200225179580112351480
- GabouryCLSimonsonDCSeelyEWRelation of pressor responsiveness to angiotensin II and insulin resistance in hypertensionJ Clin Invest19949422953007989585
- GaenzerHNeumayrGMarschangPEffect of insulin therapy on endothelium-dependent dilation in type 2 diabetes mellitusAm J Cardiol200289431411835925
- Garcia SorianoFViragLJagtapPDiabetic endothelial dysfunction: the role of poly(ADP-ribose) polymerase activationNat Med200171081311135624
- GasicSWagnerOFFaschingPFosinopril decreases levels of soluble vascular cell adhesion molecule-1 in borderline hypertensive type II diabetic patients with microalbuminuriaAm J Hypertens1999122 Pt 12172210090351
- GazisAWhiteDJPageSREffect of oral vitamin E (α-tocopherol) supplementation on vascular endothelial function in type 2 diabetes mellitusDiabet Med1999163041110220204
- GlowinskaBUrbanMPeczynskaJSelected adhesion molecules: sICAM-1 and sVCAM-1 as markers of endothelial dysfunction in diabetic children and adolescencePol Merkuriusz Lek2003142059
- GoldinECasadevallMMourelleMRole of prostaglandins and nitric oxide in gastrointestinal hyperemia of diabetic ratsAm J Physiol1996270G684908928799
- GoranMIBallGDCruzMLObesity and risk of type 2 diabetes and cardiovascular disease in children and adolescentsJ Clin Endocrinol Metab20038814172712679416
- HaefligerIOFlammerJLuscherTFNitric oxide and endothelin-1 are important regulators of human ophthalmic arteryInvest Ophthalmol Vis Sci199233234031607246
- HadiARHCarrCSAl SuwaidiJEndothelial dysfunction: cardiovascular risk factors, therapy and outcomeVascular Health and Risk Management200511839817319104
- HaffnerSMPre-diabetes, insulin resistance, inflammation and CVD riskDiabetes Res Clinc Pract200361Suppl 1S918
- HallerHEndothelial function. General considerationsDrugs199753Suppl 11109034750
- HattoriYKasaiKNakamuraTEffect of glucose and insulin on immunoreactive endothelin-1 release from cultured porcine aortic endothelial cellsMetabolism19914016591988773
- HaunerHThe mode of action of thiazolidinedionesDiabetes Metab Res Rev200218Suppl 2S101511921433
- HaunerHTakahashiMFunahashiTPPAR_ ligands increase expression and plasma concentrations of adiponectin, an adipose derived proteinDiabetes2001502094911522676
- HazelLKennethARoebuckOOxidant stress and endothelial cell dysfunctionAm J Physiol Cell Physio2001280C71941
- HednerTSunXMeasures of endothelial function as an endpoint in hypertension?Blood Press Suppl1997258669495629
- HenryRMFerreiraIKostensePJType 2 diabetes is associated with impaired endothelium-dependent, flow-mediated dilation, but impaired glucose metabolismis not; The Hoorn StudyAtherosclerosis2004174495615135250
- HermannTSLiWDominguezHQuinapril treatment increases insulin-stimulated endothelial function and adiponectin gene expression in patients with type 2 diabetesJ Clin Endocrinol Metab2006911001816352688
- HinkUTsilimingasNWendtMMechanisms underlying endothelial dysfunction in diabetes mellitus: therapeutic implicationsEndocrinol20032293304
- HofmannMAKohlBZumbachMSHyperhomocyst(e)inemia and endothelial dysfunction in IDDMDiabetes Care19982184189589252
- HonisettSYStojanovskaLSudhirKHormone therapy impairs endothelial function in postmenopausal women with type 2 diabetes mellitus treated with rosiglitazoneJ Clin Endocrinol Metab2004894615915356071
- HornigBLandmesserUKohlerCComparative effect of ACE inhibition and angiotensin II type 1 receptor antagonism on bioavailability of nitric oxide in patients with coronary artery disease: role of superoxide dismutaseCirculation200110379980511171786
- HsuehWAAndersonPWHypertension, the endothelial cell, and the vascular complications of diabetes mellitus [clinical conference]Hypertension199220253631639468
- HsuehWAAndersonPWSystemic hypertension and the renin-angiotensin system in diabetic vascular complicationsAm J Cardiol19937214H21H8517422
- HsuehALyonJManuelJInsulin resistance and the endotheliumAm J Med20041171091715234647
- HubacekJVermaSShewchukLRationale and design of the Glitazones and the Endothelium (GATE) study: evaluation of rosiglitazone on endothelial function in patients with diabetesCan J Cardiol20042014495315614340
- HultbergBAgardhEAnderssonAIncreased levels of plasma homocysteine are associated with nephropathy, but not severe retinopathy in type 1 diabetes mellitusScand J Clin Lab Invest199151277821882179
- HuversFCDe LeeuwPWHoubenAJEndothelium-dependent vasodilatation, plasma markers of endothelial function, and adrenergic vasoconstrictor responses in type 1 diabetes under near-normoglycemic conditionsDiabetes1999481300710342820
- JankaHUPlatelet and endothelial function tests during metformin treatment in diabetes mellitusHorm Metab Res Suppl19851512022934311
- JarvisaloMJRaitakariMToikkaJOEndothelial dysfunction and increased arterial intima-media thickness in children with type 1 diabetesCirculation20041091750515023875
- JensenSMicroalbuminuria and risk of atherosclerosis. Clinical epidemiological and physiological investigatorsDan Med Bull200047637810822799
- JohnstoneMTCreagerSJScalesKMimpaired endothelium-dependent vasodilation in patients with insulin-dependent diabetes mellitusCirculation1993882510168080489
- JorgeC-EMarilynCDiabetes and endothelial dysfunction: a clinical perspectiveEndocrine Reviews200122365211159815
- JoyceMMooreKThompsonCHydroxy-methylglutaryl-coenzyme A reductase inhibition improves endothelial dysfunction in type-1 diabetesEur J Vasc Endovasc Surg200427432715015196
- KabatADheinSL-arginine supplementation prevents the development of endothelial dysfunction in hyperglycaemiaPharmacology2006761859116491042
- KahnBBFlierJSObesity and insulin resistanceJ Clin Invest20001064738110953022
- KamideKNaganoMNakanoNInsulin resistance and cardiovascular complications in patients with essential hypertensionAm J Hypertens199691165718972886
- KatakamPVUjhelyiMRHoenigMMetformin improves vascular function in insulin-resistant ratsHypertension2000351 Pt 11081210642283
- KeechAColquhounDBestJSecondary prevention of cardiovascular events with long-term pravastatin in patients with diabetes or impaired fasting glucose: results from the LIPID trialDiabetes Care20032627132114514569
- KhderYBrianconSPetermannRShear stress abnormalities contribute to endothelial dysfunction in hypertension but not in type II diabetesJ Hypertens1998161619259856362
- KimSHParkKWKimYSEffects of acute hyperglycemia on endothelium-dependent vasodilation in patients with diabetes mellitus or impaired glucose metabolismEndothelium200310657012791513
- KimY-BCiaraldiTPKongATroglitazone but not metformin restores insulin-stimulated phosphoinositide 3-kinase activity and increases p110_ protein levels in skeletal muscle of type 2 diabetic subjectsDiabetes200251443811812753
- KingHAubertREHermanWHGlobal burden of diabetes, 1995–2025: prevalence, numerical estimates and projectionsDiabetes Care1998211414319727886
- KitaTKumeNMinamiMRole of oxidized LDL in atherosclerosisAnn NY Acad Scie2001947199206
- KohMSMajewskiBBRhodesELDiabetic serum stimulates the proliferation of endothelial cells in cultureDiabetes Res1985228794075699
- KonukogluDDoganETurhanMSImpaired glucose tolerance: its relevance to early endothelial dysfunctionHorm Metab Res2003356071014605996
- KruszynskaYTYuJGOlefskyJMEffects of troglitazone on blood concentrations of plasminogen activator inhibitor 1 in patients with type 2 diabetes and in lean and obese normal subjectsDiabetes200049633910871202
- KubokiKJiangZYTakaharaNRegulation of endothelial constitutive nitric oxide synthase gene expression in endothelial cells and in vivo: a specific vascular action of insulinCirculation20001016768110673261
- LandinKTengbornLSmithUElevated fibrinogen and plasminogen activator inhibitor (PAI-1) in hypertension are related to metabolic risk factors for cardiovascular diseaseJ Intern Med199022727382182759
- LebovitzHEDoleJFPatwardhanRRosiglitazone monotherapy is effective in patients with type 2 diabetesJ Clin Endocrinol Metab200186280811232013
- LeinonenEHurt-CamejoEWiklundOInsulin resistance and adiposity correlate with acute-phase reaction and soluble cell adhesion molecules in type 2 diabetesAtherosclerosis20031663879412535753
- LemneCde FaireUElevation of plasminogen activator inhibitor 1 in borderline hypertension is linked to concomitant metabolic disturbancesEur J Clin Invest19962669278872066
- LeursPBStolkRPHamulyakKTissue factor pathway inhibitor and other endothelium-dependent hemostatic factors in elderly individuals with normal or impaired glucose tolerance and type 2 diabetesDiabetes Care2002251340512145232
- LevinEREndothelins as cardiovascular peptidesAmJ Nephrol199616246518739884
- LibbyPInflammation in atherosclerosisNature20024208687412490960
- LimACVasculopathy in type 2 diabetic individuals without microalbumuriaDiabetes Care19992218657010546021
- LoomansCJde KoningEJStaalFJEndothelial progenitor cell dysfunction: a novel concept in the pathogenesis of vascular complications of type 1 diabetesDiabetes200453195914693715
- LorenziMMontisanoDFToledoSHigh glucose induces DNA damage in cultured human endothelial cellsJ Clin Invest19867732253944257
- LoviscachMRehmanNCarterLDistribution of peroxisome proliferator-activated receptors (PPARs) in human skeletal muscle and adipose tissue: relation to insulin actionDiabetologia2000433041110768091
- LuscherTFThe endothelium. Target and promoter of hypertension?Hypertension19901548252110114
- LuscherTFTannerFCTschudiMREndothelial dysfunction in coronary artery diseaseAnnu Rev Med1993443954188476260
- LyonCJLawREHsuehWAMinireview: adiposity, inflammation, and atherogenesisEndocrinology2003144219520012746274
- MacKenzieKEWiltshireEJGentRFolate and vitamin B6 rapidly normalize endothelial dysfunction in children with type 1 diabetes mellitusPediatrics20061182425316818571
- MaejimaKNakanoSHimenoMIncreased basal levels of plasma nitric oxide in Type 2 diabetic subjects. Relationship to microvascular complicationsJ Diabetes Complications2001151354311358682
- MaioranaAO’DriscollGCheethamCThe effect of combined aerobic and resistance exercise training on vascular function in type 2 diabetesJ Am Coll Cardiol200138860611527646
- MakimattilaSVirkamakiAGroopPHChronic hyperglycemia impairs endothelial function and insulin sensitivity via different mechanisms in insulin-dependent diabetes mellitusCirculation1996941276828822980
- MakinoNMaedaTSuganoMHigh serum TNF-alpha level in Type 2 diabetic patients with microangiopathy is associated with eNOS down-regulation and apoptosis in endothelial cellsJ Diabetes Complications2005193475516260352
- ManciniGBHenryGCMacayaCAngiotensin-converting enzyme inhibition with quinapril improves endothelial vasomotor dysfunction in patients with coronary artery disease. The TREND (Trial on Reversing ENdothelial Dysfunction) StudyCirculation199694258658759064
- ManzellaDGrellaRAbbatecolaAMRepaglinide administration improves brachial reactivity in type 2 diabetic patientsDiabetes Care2005283667115677794
- ManzellaDRagnoEAbbatecolaAMResidual C-peptide secretion and endothelial function in patients with Type II diabetesClin Sci (Lond)20031051131812608890
- MatherKJVermaSAndersonTJImproved endothelial function with metformin in type 2 diabetes mellitusJ Am Coll Cardiol20013713445011300445
- MatsuokaHEndothelial dysfunction associated with oxidative stress in humanDiabetes Res Clin Practice200154SupplS6572
- McFarlaneSIKumarASowersJRMechanisms by which angiotensin-converting enzyme inhibitors prevent diabetes and cardiovasculardiseaseAm J Cardiol20039130H37H
- McFarlaneRMcCredieRJBonneyMAAngiotensin converting enzyme inhibition and arterial endothelial function in adults with type 1 diabetes mellitusDiabet Med19991662610229295
- McIntyreMBohrDFDominiczakAFEndothelial function hypertension: the role of superoxide anionHypertension1999345394510523323
- McSorleyPTBellPMYoungISEndothelial function, insulin action and cardiovascular risk factors in young healthy adult offspring of parents with Type 2 diabetes: effect of vitamin E in a randomized double-blind, controlled clinical trialDiabet Med2005227031015910620
- McVeighGECohnJNEndothelial dysfunction and the metabolic syndromeCurr Diab Rep20033879212643151
- MeekingDRCummingsMHThorneSEndothelial dysfunction in Type 2 diabetic subjects with and without microalbuminuriaDiabet Med199916841710547211
- MeigsJBHuFBRifaiNBiomarkers of endothelial dysfunction and risk of type 2 diabetes mellitusJAMA200429119788615113816
- MoldoveanuETanaseanuCTanaseanuSPlasma markers of endothelial dysfunction in type 2 diabeticsEur J Intern Med200617384216378884
- MombouliJVACE inhibition, endothelial function and coronary artery lesions. Role of kinins and nitric oxideDrugs199754Suppl 512229429841
- MombouliJVVanhouttePMKinins and endothelial control of vascular smooth muscleAnnu Rev Pharmacol Toxicol1995356797057598512
- MoussaviNRenierGRoussinALack of concordance between plasma markers of cardiovascular risk and intima-media thickness in patients with type 2 diabetesDiabetes Obes Metab20046697714686966
- MudaliarSHenryRRNew oral therapies for type 2 diabetesmellitus: the glitazones or insulin sensitizersAnnu Rev Med2001522395711160777
- MullenMJClarksonRDonaldAEEffect of enalapril on endothelial function in young insulin-dependent diabetic patients: A randomized, double blind studyJ Am Coll Cardiol199831133059581728
- MyrupBMathiesenERRonnBEndothelial function and serum lipids in the course of developing microalbuminuria in insulin-dependent diabetes mellitusDiabetes Res1994263397664535
- NeriSBrunoCMLeottaCEarly endothelial alterations in non-insulin-dependent diabetes mellitusInt J Clin Lab Res19982810039689551
- NielsenFSRossingPGallMALisinopril improves endothelial dysfunction in hypertensive NIDDM subjects with diabetic nephropathyScand J Clin Lab Invest199757427349279969
- NordtTKKlassenKJSchneiderDJAugmentation of synthesis of plasminogen activator inhibitor type-1 in arterial endothelial cells by glucose and its implications for local fibrinolysisArterioscler Thromb199313182288241103
- NystromTNygrenASjoholmAPersistent endothelial dysfunction is related to elevated C-reactive protein (CRP) levels in Type II diabetic patients after acute myocardial infarctionClin Sci (Lond)2005108121815504106
- O’DriscollGGreenDMaioranaAImprovement in endothelial function by angiotensin-converting enzyme inhibition in non-insulin-dependent diabetes mellitusJ Am Coll Cardiol19993315061110334415
- O’DriscollGGreenDRankinJImprovement in endothelial function by angiotensin converting enzyme inhibition in insulin-dependent diabetes mellitusJ Clin Invest1997100678849239416
- O’DriscollGGreenDTaylorRRSimvastatin, an HMG-coenzyme A reductase inhibitor, improves endothelial function within 1 monthCirculation1997951126319054840
- OkonEBChungAWRauniyarPCompromised arterial function in human type 2 diabetic patientsDiabetes20055424152316046309
- OkouchiMOkayamaNImaiSHigh insulin enhances neutrophil transendothelial migration through increasing surface expression of platelet endothelial cell adhesion molecule-1 via activation of mitogen activated protein kinaseDiabetologia20024514495612378388
- OmoriHNagashimaHTsurumiYDirect in vivo evidence of a vascular statin: a single dose of cerivastatin rapidly increases vascular endothelial responsiveness in healthy normocholesterolaemic subjectsBr J Clin Pharmacol200254395912392587
- OomenPHKantGDDullaartRPAcute hyperglycemia and hyperinsulinemia enhance vasodilatation in Type 1 diabetes mellitus without increasing capillary permeability and inducing endothelial dysfunctionMicrovasc Res2002631911749067
- OomenPHKantGDDullaartRPNo effects of acute hyperglycaemia and hyperinsulinaemia on skin microcirculation and endothelial markers in Type II diabetes mellitusScand J Clin Lab Invest2004641192715115249
- OuchiNKiharaSAritaYAdiponectin, an adipocyte-derived plasma protein, inhibits endothelial NF-kappaB signaling through a cAMP-dependent pathwayCirculation2000102129630110982546
- OuchiNKiharaSAritaYAdipocyte-derived plasma protein, adiponectin, suppresses lipid accumulation and class A scavenger receptor expression in human monocyte-derived macrophagesCirculation200110310576311222466
- OuvinaSMLa GrecaRDZanaroNLEndothelial dysfunction, nitric oxide and platelet activation in hypertensive and diabetic type II patientsThromb Res20011021071411323020
- PaniaguaJALopez-MirandaJEscribanoACerivastatin improves insulin sensitivity and insulin secretion in early-state obese type 2 diabetesDiabetes200251259660312145176
- PaolissoGGiuglianoDOxidative stress and insulin action: is there a relationship?Diabetologia199639357638721784
- PaviaCFerrerIVallsCTotal homo-cysteine in patients with type 1 diabetesDiabetes Care20002384710857974
- PenaASWiltshireEGentRFolic acid improves endothelial function in children and adolescents with type 1 diabetesJ Pediatr2004144500415069400
- PerticoneFCeravoloRCandigliotaMObesity and body fat distribution induce endothelial dysfunction by oxidative stress: protective effect of vitamin CDiabetes2001501596511147782
- PieperGMJordanMAdamsMBRestoration of vascular endothelial function in diabetesDiabetes Res Clin Pract199631SupplS157628864654
- PieperGMJordanMAdamsMBSyngeneic pancreatic islet transplantation reverses endothelial dysfunction in experimental diabetesDiabetes1995441106137657036
- PieperGMLangenstroerPSiebeneichWDiabetic-induced endothelial dysfunction in rat aorta: role of hydroxyl radicalsCardiovasc Res199734145569217884
- PieperGMSiebeneichWDiabetes-induced endothelial dysfunction is prevented by long-term treatment with the modified iron chelator, hydroxyethyl starch conjugated-deferoxamineJ Cardiovasc Pharmacol19973073489436811
- PieperGMSiebeneichWTemocapril, an angiotensin converting enzyme inhibitor, protects against diabetes-induced endothelial dysfunctionEur J Pharmacol20004031293210969153
- PinkneyJHDownsLHoptonMEndothelial dysfunction in Type 1 diabetes mellitus: relationship with LDL oxidation and the effects of vitamin EDiabet Med199916993910656227
- PistroschFHerbrigKKindelBRosiglitazone improves glomerular hyperfiltration, renal endothelial dysfunction, and microalbuminuria of incipient diabetic nephropathy in patientsDiabete200554220611
- PistroschFPassauerJFischerSIn type 2 diabetes, rosiglitazone therapy for insulin resistance ameliorates endothelial dysfunction independent of glucose controlDiabetes Care2004274849014747233
- PlutzkyJInflammatory pathways in atherosclerosis and acute coronary syndromesAm J Cardiol200188101511423051
- PrasadATupas-HabibTSchenkeWHAcute and chronic angiotensin-1 receptor antagonism reverses endothelial dysfunction in atherosclerosisCirculation200010123495410821809
- PriorJOQuinonesMJHernandez-PampaloniMCoronary circulatory dysfunction in insulin resistance, impaired glucose tolerance, and type 2 diabetes mellitusCirculation20051112291815851590
- QianLBWangHPQiuWLInterleukin-2 protects against endothelial dysfunction induced by high glucose levels in ratsVascul Pharmacol2006453748216837248
- QuinÜonesMJHernandez-PampaloniMChonYImprovement of coronary artery endothelial dysfunction in insulin resistant patients after treatment with insulin-sensitizing thiazolidinedionesDiabetes200251A172
- RabelinkTJBakrisGLThe renin-angiotensin system in diabetic nephropathy: the endothelial connectionMiner Electrolyte Metab19982438189930377
- RamsayJESimmsRJFerrellWREnhancement of endothelial function by pregnancy: inadequate response in women with type 1 diabetesDiabetes Care200326475912547884
- Rask-MadsenNIhlemannTKrarupEInsulin therapy improves insulin-stimulated endothelial function in patients with type 2 diabetes and ischemic heart diseaseDiabetes20015026111811679442
- RegensteinerJGPopylisenSBauerTAOral L-arginine and vitamins E and C improve endothelial function in women with type 2 diabetesVasc Med200381697514989557
- RizzoVMcIntoshDPOhPIn situ flow activates endothelial nitric oxide synthase in luminal caveolae of endothelium with rapid caveolin dissociation and calmodulin associationJ Biol Chem19982733472499856995
- RobillonJCanivetBCanditoMType 1 diabetes mellitus and homocyst(e)ineDiabetes Metab1994204946
- SahachVFPrysiazhnaODTkachenkoMNEffect of L-arginine on the endothelium functional activity in experimental diabetes mellitusFiziol Zh20055137
- SalmiMStolenCJousilahtiPInsulin-regulated increase of soluble vascular adhesion protein-1 in diabetesAm J Pathol200216122556212466139
- SatoNKaseHKatoTEffect of angiotensin II type 1 receptor antagonist on oxidative stress markers in type 2 diabetic patients with hypertensionNippon Rinsho2003611245912877092
- SchneiderJGTillyNHierlTElevated plasma endothelin-1 levels in diabetes mellitusAm J Hypertens2002159677212441216
- ShemyakinABohmFWagnerHEnhanced endothelium-dependent vasodilatation by dual endothelin receptor blockade in individuals with insulin resistanceJ Cardiovasc Pharmacol2006473859016633080
- ShepherdJCobbeSMFordIPrevention of coronary heart disease with pravastatin in men with hypercholesterolemia. West of Scotland Coronary Prevention Study GroupN Engl J Med1995333130177566020
- ShestakovaMVIarek-MartynovIRIvanishinaNSAssessment of vasomotor endothelial function in patients with diabetes mellitus type 1 at different stages of diabetic nephropathyTer Arkh200375172112920953
- ShestakovaMVIarek-MartynovaIRIvanishinaNSCardiorenal syndrome in type 1 diabetes mellitus: the role of endothelial dysfunctionKardiologiia2005a45354116007033
- ShestakovaMVJarek-MartynowaIRIvanishinaNSRole of endothelial dysfunction in the development of cardiorenal syndrome in patients with type 1 DiabetesRes Clin Pract2005b68Suppl 1S6572
- SkrhaJVackovaIKvasnickaJPlasma-free N-terminal fibronectin 30-kDa domain as a marker of endothelial dysfunction in type 1 diabetes mellitusEur J Clin Invest19902017162112482
- Skyrme-JonesRAMeredithITSoluble adhesion molecules, endothelial function and vitamin E in type 1 diabetesCoron Artery Dis200112697511211168
- Skyrme-JonesRAO’BrienRCLuoMEndothelial vasodilator function is related to low-density lipoprotein particle size and low-density lipoprotein vitamin E content in type 1 diabetesJ Am Coll Cardiol200035292910676672
- SourijHZweikerRWascherTCEffects of pioglitazone on endothelial function, insulin sensitivity, and glucose control in subjects with coronary artery disease and new-onset type 2 diabetesDiabetes Care20062910394516644634
- StalkerTJSkvarkaCBScaliaRA novel role for calpains in the endothelial dysfunction of hyperglycemiaFASEB J20031715111312824289
- StehouwerCDFischerHRvan KuijkAWEndothelial dysfunction precedes development of microalbuminuria in IDDMDiabetes19954456147729616
- SteinbergHOBrechtelGJohnsonAInsulin-mediated skeletal muscle vasodilation is nitric oxide dependent. A novel action of insulin to increase nitric oxide releaseJ Clin Invest199494117298083357
- SteinbergHOChakerHLeamingRObesity/insulin resistance is associated with endothelial dysfunction: implications for the syndrome of insulin resistanceJ Clin Invest1996972601108647954
- SteinbergHOTarshobyMMonestelRElevated circulating free fatty acid levels impair endothelium-dependent vasodilationJ Clin Invest1997100123099276741
- StuddyPRLapworthRBirdRAngiotensin-converting enzyme and its clinical significance-a reviewJ Clin Pathol198336938476308066
- StuhlingerMCAbbasiFChuJWRelationship between insulin resistance and an endogenous nitric oxide synthase inhibitorJAMA20022871420611903029
- TamaiOMatsuokaHItabeHSingle LDL apheresis improves endothelium-dependent vasodilatation in hypercholesterolemic humansCirculation19979576828994420
- TanKCChowWSAiVHEffects of angiotensin II receptor antagonist on endothelial vasomotor function and urinary albumin excretion intype 2 diabetic patients with microalbuminuriaDiabetes Metab Res Rev20021871611921421
- TanKCChowWSTamSCAtorvastatin lowers C-reactive protein and improves endothelium-dependent vasodilation in type 2 diabetes mellitusJ Clin Endocrinol Metab200287563811836286
- TargherGBertoliniLZenariLCigarette smoking and plasma total homocysteine levels in young adults with type 1 diabetesDiabetes Care200023524810857946
- TarnowLHovindPTeerlinkTElevated plasma asymmetric dimethylarginine as a marker of cardiovascular morbidity in early diabetic nephropathy in type 1 diabetesDiabetes Care20043273765914988299
- TaddeiSVirdisAGhiadoniLEffects of antihypertensive drugs on endothelial dysfunction: clinical implicationsDrugs2002622658411817973
- TesfamariamBBrownMLCohenRAElevated glucose impairs endothelium-dependent relaxation by activating protein kinaseJ Clin Invest199187164382022734
- TesfamariamBCohenRAFree radicals mediate endothelial cell dysfunction caused by elevated glucoseAm J Physiol19922632 Pt 2H32161510128
- ThompsonGRMaherVMMatthewsSFamilial Hypercholesterolaemia Regression Study: a randomised trial of low-densitylipoprotein apheresisLance199534581116
- ThorandBBaumertJChamblessLMONICA/KORA Study GroupElevated markers of endothelial dysfunction predict type 2 diabetes mellitus in middle-aged men and women from the general populationArterioscler Thromb Vasc Bio20062639840516322530
- ToikkaJOAhotupaMViikariJSAConstantly low HDLcholesterol concentration relates to endothelial dysfunction and increased in vivo LDL-oxidation in healthy young menAtherosclerosis1999147133810525134
- ToopMJDallingerKJJenningsPEAngiotensin-converting enzyme (ACE): relationship to insulin-dependent diabetes and microangiopathyDiabet Med1986345573030621
- TracyRPLemaitreRNPsatyBMRelationship of C-reactive protein to risk of cardiovascular disease in the elderly. Results from the Cardiovascular Health Study and the Rural Health Promotion ProjectArterioscler Thromb Vasc Biol199717112179194763
- TsukaharaHSekineKUchiyamaMFormation of advanced glycosylation end products and oxidative stress in young patients with type 1 diabetesPediatr Res2003544192412761359
- TsunekawaTHayashiTKanoHCerivastatin, a hydroxymethylglutaryl coenzyme a reductase inhibitor, improves endothelial function in elderly diabetic patients within 3 daysCirculation2001104376911468195
- TsunekawaTHayashiTKanoHCerivastatin, a hydroxymethylglutaryl coenzyme a reductase inhibitor, improves endothelial function in elderly diabetic patients within 3 daysCirculation2001104376911468195
- TummalaPEChenX-LSundellCLAngiotensin II induces vascular cell adhesion molecule-1 expression in rat vasculature: a potential link between the reninangiotensin system and atherosclerosisCirculation19991001223910484544
- UittenbogaardAShaulPWYuhannaISHigh-density lipoprotein prevents oxidized low-density lipoprotein-induced inhibition of endothelial nitric-oxide synthase localization and activation in caveolaeJ Biol Chem2000275112788310753938
- VaccaroOPernaAFManciniFPPlasma homocysteine and microvascular complications in type 1 diabetesNutr Metab Cardiovasc Dis20001029730411302003
- Van de ReeMAHuismanMVDe ManFHImpaired endothelium-dependent vasodilation in type 2 diabetes mellitus and the lack of effect of simvastatinCardiovasc Res20015229930511684078
- Van EttenRWde KoningEJHoningMLIntensive lipid lowering by statin therapy does not improve vasoreactivity in patients with type 2 diabetesArterioscler Thromb Vasc Biol20022279980412006393
- Van VenrooijFVvan de ReeMABotsMLAtorvastatin Lipid Intervention (DALI) Study: a randomized, double-blind, placebo-controlled trialDiabetes Care20022512111612087021
- VehkavaaraSMakimattilaSSchlenzkaAInsulin therapy improves endothelial function in type 2 diabetesArterioscler Thromb Vasc Biol2000205455010669655
- VehkavaaraSYki-JarvinenH3.5 years of insulin therapy with insulin glargine improves in vivo endothelial function in type 2 diabetesArterioscler Thromb Vasc Biol2004243253014684428
- VerrottiAGrecoRBascianiFvon Willebrand factor and its propeptide in children with diabetes. Relation between endothelial dysfunction and microalbuminuriaPediatr Res200353382612595584
- VibertiGCBenigniABognettiEGlomerular hyperfiltration and urinary prostaglandins in type 1 diabetes mellitusDiabet Med19896219232523782
- WakinoSLawREHsuehWAVascular protective effects by activation of nuclear receptor PPARJ Diabetes Complications20021646911872366
- WatanabeYSunayamaSShimadaKTroglitazone improves endothelial dysfunction in patients with insulin resistanceJ Atheroscler Thromb200071596311480457
- WattsGFPlayfordDADyslipoproteinaemia and hyperoxidative stress in the pathogenesis of endothelial dysfunction in non-insulin dependent diabetes mellitus: a hypothesisAtherosclerosis199814117309863535
- WautierJLSetiadiHViletteDLeukocyte adhesion to endothelial cellsBiorheology199027425322261508
- WautierJLWautierMPPintignyDFactors involved in cell adhesion to vascular endotheliumBlood Cells19839221346198016
- WautierJLZoukourianCChappeyOReceptor mediated endothelial cell dysfunction in diabetic vasculopathy. Soluble receptor for advanced glycation end products blocks hyperpermeability in diabetic ratsJ Clin Invest199697238438550841
- WenYSkidmoreJCPorter-TurnerMMRelationship of glycation, antioxidant status and oxidative stress to vascular endothelial damage in diabetesDiabetes Obes Metab20024305812190993
- WilliamsBA potential role for angiotensin II-induced vascular endothelial growth factor expression in the pathogenesis of diabetic nephropathy?Miner Electrolyte Metab19982440059930379
- WilliamsSBCuscoJARoddyMAImpaired nitric oxide-mediated vasodilation in patients with non-insulin-dependent diabetes mellitusJ Am Coll Cardiol199627567748606266
- WiltshireEThomasDWBaghurstPReduced total plasma homocyst(e)ine in children and adolescents with type 1 diabetesJ Pediatr20011388889311391334
- WiltshireEJGentRHirteCPenaAEndothelial dysfunction relates to folate status in children and adolescents with type 1 diabetesDiabetes2002512282612086961
- XiXPGrafKGoetzeSCentral role of the MAPK pathway in ang II-mediated DNA synthesis and migration in rat vascular smooth muscle cellsArterioscler Thromb Vasc Biol19991973829888869
- XiangGDHeYSDaiXJAngiotensin-converting enzyme gene and the brachial artery endothelial dysfunction in type 2 diabetes without angiopathyZhonghua Yi Xue Yi Chuan Xue Za Zhi200421355915300633
- YaqoobMPatrickAWMcClellandPRelationship between markers of endothelial dysfunction, oxidant injury and tubular damage in patients with insulin-dependent diabetes mellitusClin Sci (Colch)199385557628287643
- YokotaTOritaniKTakahashiIAdiponectin, a new member of the family of soluble defense collagens, negatively regulates the growth of myelomonocytic progenitors and the functions of macrophagesBlood20009617233210961870
- YuYSuoLYuHInsulin resistance and endothelial dysfunction in type 2 diabetes patients with or without microalbuminuriaDiabetes Res Clin Pract2004659510415223221
- YusufSGersteinHHoogwerfBRamipril and the development of diabetesJAMA20012861882511597291
- ZengGNystromFHRavichandranLVRoles for insulin receptor, PI3-kinase, and Akt in insulin-signaling pathways related to production of nitric oxide in human vascular endothelial cellsCirculation200010115394510747347
- ZoppiniGTargherGCacciatoriVChronic cigarette smoking is associated with increased plasma circulating intercellular adhesion molecule 1 levels in young type 1 diabetic patientsDiabetes Care1999221871410546022
- ZoukourianCWautierMPChappeyOEndothelial cell dysfunction secondary to the adhesion of diabetic erythrocytes. Modulation by iloprostInt Angiol1996151952008971575