Abstract
Cardiovascular disease is a major complication of diabetes mellitus, especially for patients with diabetic nephropathy. The underlying factor or pathogenic mechanism that links diabetic nephropathy with cardiovascular disease is not known. The endothelial cell adhesion molecules, intercellular adhesion molecule-1 or vascular cell adhesion molecule-1, play a crucial role in the initiation of atherosclerosis. Levels of both cell adhesion molecules are raised by the diabetic and kidney disease states. This review focuses on these important cell adhesion molecules and their role in the pathogenesis of cardiovascular disease in diabetes and diabetic nephropathy.
Keywords:
Introduction
Diabetes mellitus (diabetes) affects approximately 100 million people worldwide (CitationAmos et al 1997). Cardiovascular disease is a major chronic complication of both type 1 and type 2 diabetes and people with diabetes have an approximately 2–4-fold increased risk of cardiovascular events, as compared with control populations (CitationKannel and McGee 1979; CitationPanzram 1987). In addition to cardiovascular disease, people with diabetes are also at high risk of developing microvascular complications, the most clinically important being end-stage kidney disease or diabetic nephropathy. Importantly, the combination of diabetes and nephropathy increases cardiovascular disease risk by 20–40-fold (CitationMattock et al 1992; CitationAlzaid 1996).
Different stages of kidney disease versus cardiovascular disease risk
Diabetic nephropathy can be classified on its severity. Diabetics initially have no kidney disease at all. The earliest detectable level of kidney disease is microalbuminuria, where there is a minute amount of protein that is excreted in the urine (not detectable by urine dipstick). The next stage is proteinuria, which is defined as easily measurable levels of protein in the urine, but without disturbance of measures that generally mark renal failure (creatinine and urea). Lastly, the disease process may develop into renal failure, otherwise known as uremia (CitationWilliams et al 1988; CitationIseki et al 2003).
Patients who eventually develop end-stage diabetic renal failure will have passed through the stages of normal renal function, microalbuminuria, and proteinuria before reaching uremia. It has long been standard practise to use microalbuminuria as a target for treatment in the prevention of diabetic nephropathy (Citationde Zeeuw et al 2004). Less clear, until recently, is the role of microalbuminuria as a marker and therapeutic target in vascular disease (CitationAnavekar et al 2004).
Albuminuria as a marker for cardiovascular disease
In the normal population, cardiovascular risk increases in a continuous fashion along with progression from normal to overt proteinuria levels (CitationHillege et al 2001, Citation2002; CitationRomundstad et al 2003; CitationHunsicker et al 2004). Shown in a prospective 5-year survey of more than 20 000 subjects in the United Kingdom, microalbuminuria and proteinuria were independently associated with risk of cardiovascular disease and death (CitationRomundstad et al 2003). This relationship is also true for people with diabetes, with post-hoc analyses of three recent large clinical trials showing that albuminuria not only determines renal outcomes, but also cardiovascular outcomes (CitationUKPDS 1998; CitationAnavekar et al 2004; Citationde Zeeuw et al 2004). In one of these three studies, the reduction of albuminuria with therapeutic interventions resulted in protection against cardiovascular disease as well as the development of progressive renal impairment (CitationUKPDS 1998).
Albuminuria leading to vascular inflammation
There are many physiological abnormalities that are attendant in end-stage kidney disease that has led to the identification of mechanisms that may link cardiovascular disease and renal failure (CitationYuyen et al 2004). High on the list of possible mechanisms are factors such as: hypertension; anemia (CitationRebelink 2004); dyslipidemia (CitationRebelink 2004); activation of the renin-angiotensin system (CitationStevens and Levin 2003); medial calcification of the vascular tree (CitationBrewster et al 2003); malnutrition and inflammation (CitationBrewster et al 2003).
However, while these factors are present in end-stage nephropathy, not all of them are universally present in the early stages of albuminuria. Inflammation is associated with the microalbuminuric state, with albuminuria now recognized to reflect generalized vascular damage (CitationHillege et al 2001). Importantly, inflammation underlies all stages of atherosclerotic lesion formation, including early atherogenesis where inflammatory cells adhere and infiltrate the subendothelium (CitationLiu et al 2004). Critical proteins expressed by endothelial cells that bind the inflammatory cells are the cell adhesion molecules (see ).
Figure 1 Cell adhesion molecules and early atherosclerotic plaque formation. Cell adhesion molecules, including VCAM-1 and ICAM-1, are expressed on the surface of endothelial cells in response to inflammatory stimuli. Monocytes and other leukocytes bind to the cell adhesion molecules via their own specific cell adhesion molecules called integrins. Integrin leukocyte function antigen-1 (LFA-1) binds ICAM-1 and very-late antigen-4 (VLA-4) binds VCAM-1 (insert). The binding of the monocytes to endothelial cells subsequently triggers the tethering, rolling, and subsequent migration of the monocytes into the subintima.
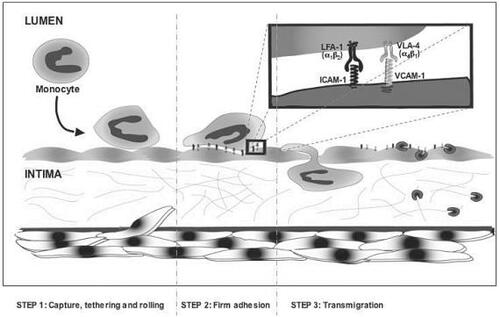
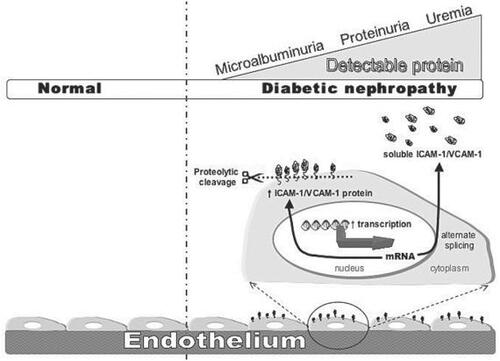
Figure 2 sVCAM-1 and sICAM-1. VCAM-1 and ICAM-1 are expressed on the cell surface of cells. Soluble forms of VCAM-1 and ICAM-1 are measurable in plasma. Several theories for the formation of the soluble forms exist, including alternate splicing, increased transcription, and proteolytic cleavage of the membrane protein (favored). There is an increase in sVCAM-1 and ICAM-1 in plasma of diabetic patients associated with an increase in the severity of kidney disease.
Cell adhesion molecules, inflammation, and atherosclerosis
Two important cell adhesion molecules expressed by endothelial cells that play a major role in the pathogenesis of atherosclerosis are vascular cell adhesion molecule-1 (VCAM-1) and intercellular cell adhesion molecule-1 (ICAM-1). Expression of both ICAM-1 and VCAM-1 have been demonstrated in atherosclerotic plaques (CitationPoston et al 1992; CitationDavies et al 1993; CitationJohnson-Tidey et al 1994; CitationO'Brien et al 1996; CitationDeGraba et al 1998; CitationBlankenberg et al 2003) with focal expression evident at lesion prone areas (CitationO'Brien et al 1996; CitationNakashima et al 1998) and at the borders of atherosclerotic lesions (CitationNakashima et al 1998; CitationIiyama et al 1999). There have been many in vitro studies showing high glucose milieus increase both ICAM-1 and VCAM-1 endothelial cell expression at both the protein (CitationKim et al 1994; CitationBaumgartner-Parzer et al 1995; CitationTaki et al 1996; CitationTakami et al 1998; CitationManduteanu et al 1999; CitationEsposito et al 2001; CitationKado et al 2001; CitationHoffman et al 2002; CitationOmi et al 2002; CitationItoh et al 2003) and messenger ribonucleic acid (mRNA) (CitationKim et al 1994; CitationChettab et al 2002; CitationItoh et al 2003; CitationAltannavch et al 2004) levels, via a cell signaling mechanism related to activation of protein kinase C-β (CitationQuagliaro et al 2005). Additionally, human endothelial cells exposed to the serum of nephropathic patients (none of whom had diabetes) had high cell surface ICAM-1 and VCAM-1 expression, correlating with increased mRNA levels (CitationSerradell et al 2002). Our own laboratory has recently shown that exposure of cultured human endothelial cells to serum from diabetic patients with advancing stages of diabetic nephropathy (microalbuminuria progressing to uremia) have a stepwise increase in the expression of both VCAM-1 and ICAM-1, as measured at the levels of gene transcription, mRNA, and protein (CitationWu et al 2004). This suggests that diabetic/microalbuminuric patients already have underlying pathological signaling that increases key early steps in atherosclerosis using in vitro measures.
Soluble cell adhesion molecules
Although the cell adhesion molecules are firmly anchored on the cell membranes of endothelial cells, cell adhesion molecules may be broken off into the circulation forming soluble VCAM-1 (sVCAM-1) and soluble ICAM-1 (sICAM-1). The underlying physiologic pathway leading to the formation of soluble cell adhesion molecules and their subsequent physiologic function remains unclear. Possible explanations have been proposed, including an increased synthesis of soluble forms via increased gene transcription, altered mRNA stability, and/or the existence of alternate splice variants. However, the favored hypothesis is that enhanced proteolytic cleavage of the cell adhesion molecules from the cell surface leads to soluble cell adhesion molecules, measurable in plasma. This implies that there is a relationship between the degree of cellular expression of cell adhesion molecules and plasma soluble cell adhesion molecule levels. This is yet to be proven. Soluble cell adhesion molecules are easily measurable in plasma and much work has been done in the last 10 years on whether sICAM-1 and sVCAM-1 are useful markers for cardiovascular disease in patients with diabetes and diabetic nephropathy.
Soluble cell adhesion molecules and diabetic kidney disease
There appears to be a strong relationship between sICAM-1/VCAM-1 and diabetic nephropathy. A number of studies have found a general increasing trend in both sICAM-1 and sVCAM-1 with increasing levels of diabetic kidney disease in diabetics (CitationClausen et al 2000; CitationGuler et al 2002; CitationWu et al 2004). Importantly, sVCAM-1 and sICAM-1 have been found to be significantly associated with microalbuminuria in type 2 diabetics as compared with controls (CitationFasching et al 1996; CitationSchmidt et al 1996; CitationGasic et al 1999; CitationKado and Nagata 1999; CitationLim et al 1999; CitationJager et al 2000; CitationMurakami et al 2001). This has suggested the potential usefulness of plasma sVCAM-1 as a marker of vascular perturbation (CitationSchmidt et al 1996).
Soluble cell adhesion molecules and diabetic cardiovascular disease
Soluble ICAM-1 and/or sVCAM-1 show good correlation with cardiovascular disease in diabetic subjects. In a recent study, type 2 diabetics showed high sICAM-1 levels, independent of known cardiovascular risks, and predicted all cause as well as cardiovascular mortality over 10 years (CitationBecker et al 2002). Increased levels of sVCAM-1 were also associated with increased risk of mortality in type 2 diabetes, as seen in the Hoorn study (CitationJager et al 2000). In the Hoorn study, 631 type 2 diabetic and control subjects with higher sVCAM-1 levels at the beginning of the study period had increased risk of cardiovascular death during 8 years of follow-up even after adjustment for age, sex, glucose tolerance, hypertension, cardiovascular disease, high density lipoproteins, low density lipoproteins, homocysteine, microalbuminuria, von Willebrand factor, C-reactive protein, and glomerular filtration rate. The effect was magnified in type 2 diabetics, thus indicating that sVCAM-1 is independently associated with the risk of cardiovascular mortality (CitationJager et al 2000). In another study, CitationStehouwer et al (2002) also showed that high sVCAM-1 levels were independently associated with increased mortality in type 2 diabetics followed for a mean of 9 years.
These findings are well supported by a number of crosssectional studies. Both sICAM-1 and sVCAM-1 levels were higher in elderly type 2 diabetics with known cerebrovascular disease (CitationKawamura et al 1998); and sVCAM-1 levels were higher in type 2 diabetic patients with symptomatic cardiovascular disease as compared with those with no known cardiovascular disease (CitationOtsuki et al 1997). However, one very recent study did not demonstrate any correlation between sICAM-1, sVCAM-1, and known cardiovascular disease, nor with degree of intimamedia thickening (CitationLeinonen et al 2003). It is important to keep in mind that this last survey was smaller than the longitudinal studies outlined above. Overall, sICAM-1 and sVCAM-1 levels have been demonstrated to be predictive for the future development of cardiovascular disease and mortality in diabetic subjects.
Correlations with novel risk factors for atherosclerosis
The cell adhesion molecules are just one of a number of emerging markers for cardiovascular risk factors (). Additional to cell adhesion molecules, one of the most exciting novel risk factors sparking a lot of research interest is C-reactive protein. The significance of C-reactive protein and inflammation has become increasingly evident recently, and it now appears that C-reactive protein actively contributes to atherosclerotic plaque formation and thrombotic events. Additionally, C-reactive protein is associated with the inflammatory states of not only renal failure, but also microalbuminuria. In a recent study, C-reactive protein was found to be associated with cardiovascular mortality risk rate in patients with end-stage kidney disease, and traditional risk factors including left ventricular hypertrophy showed higher associations (CitationShlipak et al 2005). Similarly, in cell adhesion molecules, recent data reported a linear association between the level of albuminuria and elevations of C-reactive protein. Specific monitoring has been proposed (CitationBakris 2004). C-reactive protein studies remain in their infancy and prognostic values remain on a case-by-case basis (CitationMcCullough 2004). Both sICAM-1 (CitationRidker et al 1998) and sVCAM-1 (CitationSchalkwijk et al 1999; CitationJager et al 2000) levels have been shown to significantly correlate with C-reactive protein in the diabetic setting.
Table 1 Association of kidney disease with risk factors for cardiovascular disease
The soluble cell adhesion molecules also associate with other prominent novel cardiovascular risk factors including carotid intimamedia thickness (CitationOtsuki et al 1997; CitationKawamura et al 1998; CitationMatsumoto et al 2002; CitationTakeuchi et al 2002), advanced glycation end-points (CitationSmulders et al 1998; CitationVlassara et al 2003; CitationLieuw et al 2004), plasma von Willebrand factor and homocysteine (CitationRidker et al 1998; CitationJager et al 2000; CitationTargher et al 2001), fibrinogen, and tissuetype plasminogen-activator antigen (CitationRidker et al 1998), thereby justifying their consideration as a novel risk marker for cardiovascular disease, especially in diabetic patients.
The effect of treatments on sICAM-1 and sVCAM-1
The effect of glucose control on sICAM-1 and sVCAM-1 is not consistent between studies, with only a minority showing decreasing soluble cell adhesion molecule levels with normalization of glucose (CitationAlbertinin et al 1998; CitationMarfella et al 2000). However, diet and dietary supplements can influence soluble cell adhesion molecule levels; eg, ingestion of antioxidants vitamins E and C immediately after a meal can significantly suppress the rapid rise in sICAM-1 and sVCAM-1 seen with a high fat meal (CitationNappo et al 2002). Additionally, diabetics given RRR-alphatocopheol therapy for 3 months showed a significant fall in sVCAM-1 and sICAM-1 (CitationDevaraj and Jialal 2000). Other antioxidants have also been shown to decrease cell adhesion molecules in type 2 diabetics, such as N-acetyl-L-cysteine which decreased sVCAM-1 (CitationDe Mattia et al 1998) and glutathione which decreased sICAM-1 (CitationCeriello et al 1998).
Pharmacologic treatments can also effect soluble cell adhesion molecule levels; eg, hypertension is a common problem in diabetics and blockade of the renin-angiotensin system is a common method to achieve control of blood pressure. The angiotensin-converting enzyme inhibitor, fosinopril, administered for 12 weeks to microalbuminuric type 2 diabetics, decreased sVCAM-1 to control levels, but did not change sICAM-1 levels (CitationGasic et al 1999). In a crossover trial in type 2 diabetics, angiotensin-converting enzyme inhibitor, enalapril, and angiotensin receptor II blocker, losartan, both decreased sVCAM-1, but not sICAM-1 (CitationAndersen et al 2000). Even though both decreased blood pressure and urine albumin excretion by the same amount, the enalapril was found to be more effective than losartan in decreasing the level of sVCAM-1 (CitationAndersen et al 2000). In another example, management of dyslipidemia with hydroxymethyl glutaroyl coenzyme A (HMG-coA) reductase inhibitors (statins) is also common in diabetes. Three months of simvastatin therapy was able to significantly decrease both sICAM-1 and sVCAM-1 levels (CitationCeriello et al 2004). In addition, simvastatin was able to significantly suppress the acute rise in sICAM-1 and sVCAM-1 seen after a glucose load and/or high-fat oral load (CitationCeriello et al 2004). A similar drug, atorvastatin, significantly decreased sVCAM-1 in type 2 diabetics as compared with placebo (CitationDalla Nora et al 2003). Cardiovascular patients are often treated with antiplatelet agents, including aspirin and sarpogrelate. Both these drugs have been found to decrease serum sICAM-1 levels (CitationShouzu et al 2000; CitationMateos-Careres et al 2002). Lastly, hormone replacement therapy is often used by older women to control the symptoms of menopause and until recently, was thought to have cardioprotective benefit, although this is now very controversial (CitationPrentice et al 2005). Hormone replacement therapy, whether oestrogen only (CitationKoh et al 2001), or combined oestrogen-progestin based (CitationManning et al 2002), did not have any effect on sICAM-1 or sVCAM-1 levels in post-menopausal type 2 diabetic women.
In summary, dietary interventions and some medications lower sVCAM-1 and sICAM-1 levels. Therefore cell adhesion molecules could be considered adjunctive factors to monitor, especially in diabetic and diabetic nephropathy patients, as a dual measure of cardiovascular and kidney disease risk.
Summary
The prevalence of cardiovascular disease in diabetic nephropathy patients is high and is a major cause of morbidity and mortality. The cell adhesion molecules, ICAM-1 and VCAM-1, are raised in both cardiovascular disease and diabetic nephropathy, with levels increasing in stepwise fashion with increasing kidney disease. Importantly, sICAM-1 and sVCAM-1 levels are raised even in the earliest stage of diabetic kidney disease; microalbuminuria. They are good predictors of atherosclerotic disease and cardiovascular mortality, and they correlate well with other conventional and nonconventional risk factors. sICAM-1 and sVCAM-1 are lowered by some dietary supplements and pharmacologic agents and therefore represent factors that can be measured to correlate with decreased cardiovascular risk, although more prospective correlative studies would be required for their use as a primary strategy. As early detection of renal impairment and cardiovascular disease in the type 2 diabetic remains a global health priority, soluble cell adhesion molecules may represent a marker of vascular disease, associated closely with early diabetic kidney disease, which if monitored could allow patients to have significant benefit from both renoand cardioprotective treatment.
References
- AlbertininJValensiPLormeuaBElevated concentrations of soluble E-selectin and vascular cell adhesion molecule-1 in NIDDM. Effect of intensive insulin treatmentDiabetes Care1998211008139614623
- AltannavchTSRoubalovaKKuceraPEffect of high glucose concentrations on expression of ELAM-1, VCAM-1 and ICAM-1 in HUVEC with and without cytokine activationPhysiol Res20043778214984317
- AlzaidAAMicroalbuminuria in patients with NIDDM: an overviewDiabetes Care19961979898720542
- AmosAFMcCartyDJZimmetPThe rising global burden of diabetes and its complications: estimates and projections to the year 2010Diabet Med199714Suppl 5S1859450510
- AnavekarNSGansDJBerlTPredictors of cardiovascular events in patients with type 2 diabetic nephropathy and hypertension: A case for albuminuriaKidney Int200466505
- AndersenSSchalkwijkCGStehouwerCDAngiotensin II blockade is associated with decreased plasma leukocyte adhesion molecule levels in diabetic nephropathyDiabetes Care2000231031210895868
- BakrisGLClinical importance of microalbuminuria in diabetes and hypertensionCurr Hypertens Rep20046352615341686
- Baumgartner-ParzerSMWagnerLPettermannMModulation by high glucose of adhesion molecule expression in cultured endothelial cellsDiabetologia1995381367708582548
- BeckerAvan HinsberghVWJagerAEur J Clin Invest2002321811851720
- BlankenbergSBarbauxSTiretLAdhesion molecules and atherosclerosisAtherosclerosis2003170191314612198
- BrewsterUCSetaroJFPerazellaMAThe renin-angiotensinaldosterone system: cardiorenal effects and implications for renal and cardiovascular disease statesAm J Med Sci2003326152412861121
- CerielloAFalletiEMotzEHyperglycemia-induced circulating ICAM-1 increase in diabetes mellitus: the possible role of oxidative stressHorm Metab Res19983014699566857
- CerielloAQuagliaroLPiconiLEffect of postprandial hypertriglyceridemia and hyperglycemia on circulating adhesion molecules and oxidative stress generation and the possible role of simvastatin treatmentDiabetes2004537011014988255
- ChettabKZibaraKBelaibaSRAcute hyperglycaemia induces changes in the transcription levels of 4 major genes in human endothelial cells: macroarrays-based expression analysisThromb Haemost200287141811848444
- ClausenPJacobsenPRossingKPlasma concentrations of VCAM-1 and ICAM-1 are elevated in patients with type 1 diabetes mellitus with microalbuminuria and overt nephropathyDiabet Med200017644911051283
- Dalla NoraEPassaroAZamboniPFAtorvastatin improves metabolic control and endothelial function in type 2 diabetic patients: a placebo-controlled studyJ Endocrinol Invest20032673812602538
- DaviesMJGordonJLGearingAJThe expression of the adhesion molecules ICAM-1, VCAM-1, PECAM, and E-selectin in human atherosclerosisJ Pathol199317122397506307
- DeGrabaTJSirenALPenixLIncreased endothelial expression of intercellular adhesion molecule-1 in symptomatic versus asymptomatic human carotid atherosclerotic plaqueStroke1998291405109660396
- De MattiaGBraviMCLaurentiOReduction of oxidative stress by oral N-acetyl-L-cysteine treatment decreases plasma soluble vascular cell adhesion molecule-1 concentrations in non-obese, nondyslipidaemic, normotensive, patients with non-insulin-dependent diabetesDiabetologia199841139269833950
- DevarajSJialalILow-density lipoprotein post-secretory modification, monocyte function, and circulating adhesion molecules in type 2 diabetic patients with and without macrovascular complications: the effect of alpha-tocopherol supplementationCirculation2000102191610889130
- de ZeeuwDRemuzziGParvingAlbuminuria, a therapeutic target for cardiovascular protection in type 2 diabetic patients with nephropathyCirculation2004110921715302780
- EspositoCFasoliGPlatiARLong-term exposure to high glucose up-regulates VCAM-induced endothelial cell adhesiveness to PBMCKidney Int2001591842911318955
- FaschingPVeitlMRohacMElevated concentrations of circulating adhesion molecules and their association with microvascular complications in insulin-dependent diabetes mellitusJ Clin Endocrinol Metabol199681431317
- GasicSWagnerOFFaschingPFosinopril decreases levels of soluble vascular cell adhesion molecule-1 in borderline hypertensive type II diabetic patients with microalbuminuriaAm J Hypertens1999122172210090351
- GulerSCakirBDemirbasBPlasma soluble intercellular adhesion molecule 1 levels are increased in type 2 diabetic patients with nephropathyHorm Res200258677012207164
- HillegeHLFidlerVDiercksGFHUrinary albumin excretion predicts cardiovascular and noncardiovascular mortality in general populationCirculation200210617778212356629
- HillegeHLJanssenWMBakAAMicroalbuminuria is common, also in nondiabetic, nonhypertensive population, and an independent indicator of cardiovascular risk factors and cardiovascsular morbidityJ Intern Med20012495192611422658
- HoffmanWHChengCPassmoreGGAcetoacetate increases expression of intercellular adhesion molecule-1 (ICAM-1) in human brain microvascular endothelial cellsNeurosci Lett200233471412435474
- HunsickerLAtkinsRLewisJImpact of irbesartan, blood pressure control, and proteinuria on renal outcomes in the Irbesartan Diabetic Nephropathy TrialKidney Int200466S99101
- IiyamaKHajraLIiyamaMPatterns of vascular cell adhesion molecule-1 and intercellular adhesion molecule-1 expression in rabbit and mouse atherosclerotic lesions and at sites predisposed to lesion formationCirc Res19998519920710417402
- IsekiKIkemiyaYIsekiGProteinuria and the risk of developing end-stage renal diseaseKidney Int20036314687412631363
- ItohMOmiHOkouchiMThe mechanisms of inhibitory actions of gliclazide on neutrophils-endothelial cells adhesion and surface expression of endothelial adhesion molecules mediated by a high glucose concentrationJ Diabetes Complications20031722612505752
- JagerAvan HinsberghVWKostensePJIncreased levels of soluble vascular cell adhesion molecule 1 are associated with risk of cardiovascular mortality in type 2 diabetes: the Hoorn studyDiabetes2000494859110868972
- Johnson-TideyRRMcGregorJLTaylorPRIncrease in the adhesion molecule P-selectin in endothelium overlying atherosclerotic plaques. Coexpression with intercellular adhesion molecule-1Am J Pathol1994144952617513951
- KadoSNagataNCirculating intercellular adhesion molecule-1, vascular cell adhesion molecule-1, and E-selectin in patients with type 2 diabetes mellitusDiabetes Res Clin Pract199946143810724093
- KadoSWakatsukiTYamamotoMExpression of intercellular adhesion molecule-1 induced by high glucose concentrations in human aortic endothelial cellsLife Sci2001687273711205865
- KannelWBMcGeeDLDiabetes and cardiovascular disease: the Framingham studyJAMA197924120358430798
- KawamuraTUmemuraTKanaiAThe incidence and characteristics of silent cerebral infarction in elderly diabetic patients: association with serum-soluble adhesion moleculesDiabetologia199841911179726593
- KimJBerlinerJNatarajanREvidence that glucose increases monocyte binding to human aortic endothelial cellsDiabetes199443110377520876
- KohKKKangMHJinDKVascular effects of estrogen in type II diabetic postmenopausal womenJ Am Coll Cardiol20013814091511691516
- LeinonenEHurt-CamejoEWiklundOInsulin resistance and adiposity correlate with acute-phase reaction and soluble cell adhesion molecules in type 2 diabetesAtherosclerosis20031663879412535753
- LieuwAFMLvan HinsbergVWTeerlinkTIncreased levels of N (epsilon)-(carboxymethyl)lysine and N(epsilon)-(carboxyethyl) lysine in type 1 diabetic patients with impaired renal function: correlation with markers of endothelial dysfunctionNephrol Dial Transplant200419631614767019
- LimSCCaballeroAESmakowskiPSoluble intercellular adhesion molecule, vascular cell adhesion molecule, and impaired microvascular reactivity are early markers of vasculopathy in type 2 diabetic individuals without microalbuminuriaDiabetes Care19992218657010546021
- LiuYCoreshJEustaceJAAssociation between cholesterol level and mortality in dialysis patients: role of inflammation and malnutritionJAMA2004291451914747502
- ManduteanuIVoineaMSerbanGHigh glucose induces enhanced monocyte adhesion to valvular endothelial cells via a mechanism involving ICAM-1, VCAM-1 and CD18Endothelium199963152410475094
- ManningPJSutherlandWHAllumAREffect of hormone replacement therapy on inflammation-sensitive proteins in postmenopausal women with Type 2 diabetesDiabet Med2002198475212358873
- MarfellaREspositoKGiuntaRCirculating adhesion molecules in humans: role of hyperglycemia and hyperinsulinemiaCirculation200010122475110811590
- Mateos-CareresPJGarcia-MendezAFarreJPrior aspirin use in unstable angina patients with modified plasma inflammatory markers and endothelial nitric oxide synthase in neutrophilsEur J Clin Invest20023289590012534448
- MatsumotoKSeraYNakamuraHSerum concentrations of soluble adhesion molecules are related to degree of hyperglycemia and insulin resistance in patients with type 2 diabetes mellitusDiabetes Res Clin Pract200255131811796179
- MattockMBMorrishNJVibertiGProspective study of microalbuminuria as predictor of mortality in NIDDMDiabetes199241736411587400
- McCulloughPACardiovascular disease in chronic kidney disease from a cardiologist's perspectiveCurr Opin Nephrol Hypertens20041359160015483448
- MurakamiHTamasawaNMatsuiJPlasma levels of soluble vascular adhesion molecule-1 and cholesterol oxidation product in type 2 diabetic patients with nephropathyJ Atheroscler Thromb2001821411686311
- NakashimaYRainesEWPlumpASUpregulation of VCAM-1 and ICAM-1 at atherosclerotic-prone sites on the endothelium in the ApoE-deficient mouseArterioscler Thromb Vasc Biol199818842519598845
- NappoFEspositoKCioffiMPostprandial endothelial activation in healthy subjects and in type 2 diabetic patients: role of fat and carbohydrate mealsJ Am Coll Cardiol20023911455011923038
- O'BrienKDMcDonaldTOChaitANeovascular expression of E-selectin, intercellular adhesion molecule-1, and vascular cell adhesion molecule-1 in human atherosclerosis and their relation to intimal leukocyte contentCirculation199693672828640995
- OmiHOkayamaNShimizuMParticipation of high glucose concentrations in neutrophil adhesion and surface expression of adhesion molecules on cultured human endothelial cells: effect of antidiabetic medicinesJ Diabetes Complications200216201812015189
- OtsukiMHashimotoKMorimotoYCirculating vascular cell adhesion molecule-1 (VCAM-1) in atherosclerotic NIDDM patientsDiabetes19974620961019392502
- PanzramGMortality and survival in type 2 (non-insulin-dependent) diabetes mellitusDiabetologia198730123313556287
- PrenticeRInvited commentary: ethics and sample size – another viewAm J Epidemiol20051611111215632259
- PostonRNHaskardDOCoucherJRExpression of intercellular adhesion molecule-1 in atherosclerotic plaquesAm J Pathol1992140665731372160
- QuagliaroLPiconiLAssaloniRIntermittent high glucose enhances ICAM-1, VCAM-1 and E-selectin expression in human umbilical vein endothelial cells in culture: The distinct role of protein kinase C and mitochondrial superoxide productionAtherosclerosis2005In press
- RebelinkTJCardiovascular risk in patients with renal disease: treating the risk of treating the risk factor?Nephrol Dial Transplant20041923614671033
- RidkerPHennekensCRoitman-JohnsonBPlasma concetration of soluble intercellular adhesion molecule 1 and risks of future myocardial infarction in apparently healthy menLancet199835188929439492
- RomundstadSHolmenJKvenildKMicroalbuminuria and all-cause mortality in 2089 apparently healthy individuals: a 4.4-year follow up study. The Nord-Trondelag Health Study (HUNT), NorwayAm J Kidney Dis2003424667312955674
- SchalkwijkCGPolandDCvan DijkWPlasma concentration of C-reactive protein is increased in type I diabetic patients without clinical macroangiopathy and correlates with markers of endothelial dysfunction: evidence for chronic inflammationDiabetologia1999423515710096789
- SchmidtACrandallJHoriOElevated plasma levels of vascular cell adhesion molecule-1 (VCAM-1) in diabetic patients with microalbuminuria: a marker of vascular dysfunction and progressive vascular diseaseBr J Haematol199692747508616048
- SerradellMDiaz-RicartMCasesAUremic medium causes expression, redistribution and shedding of adhesion molecules in cultured endothelial cellsHaematologica20028710536112368160
- ShlipakMGFriedLFCushmanMCardiovascular mortality risk in chronic kidney disease: comparison of traditional and novel risk factorsJAMA200529317374515827312
- ShouzuANomuraSHayakawaTEffect of sarpogrelate hydrochloride on platelet-derived microparticles and various soluble adhesion molecules in diabetes mellitusClin Appl Thromb Hemost200061394310898273
- SmuldersRAStehouwerCDSchalkwijkCGDistinct associations of HbA1c and the urinary excretion of pentosidine, an advanced glycosylation end-product, with markers of endothelial function in insulin-dependent diabetes mellitusThromb Haemost1998805279684785
- StehouwerCDGallMATwiskJWIncreased urinary albumin excretion, endothelial dysfunction, and chronic low-grade inflammation in type 2 diabetes: progressive, interrelated, and independently associated with risk of deathDiabetes20025111576511916939
- StevensLALevinAAnaemia, cardiovascular disease and kidney disease: integrating new knowledge in 2002Curr Opin Nephrol Hypertens200312133812589172
- TakamiSYamashitaSKiharaSHigh concentration of glucose induces the expression of intercellular adhesion molecule-1 in human umbilical vein endothelial cellsAtherosclerosis199813835419678769
- TakeuchiNKawamuraTKanaiAThe effect of cigarette smoking on soluble adhesion molecules in middle-aged patients with Type 2 diabetes mellitusDiabet Med200219576411869304
- TakiHKashiwagiATanakaYExpression of intercellular adhesion molecules 1 (ICAM-1) via and osmotic effect in human umbilical vein endothelial cells exposed to high glucose mediumLife Sci1996581713218637395
- TargherGZenarilLBertoliniLPlasma total homocysteine levels are associated with von Willebrand factor, soluble intercellular adhesion molecule-1 and soluble tumor necrosis factor-alpha receptors in young type 1 diabetic patients without clinical evidence of macrovascular complicationsDiabetes Care2001241496711473092
- [UKPDS] United Kingdom Prospective Diabetes Study GroupEffect of intensive blood glucose control with insulin and sulfonylureas on insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes (UKPDS 33)Lancet1998352837539742976
- WuTDeathAYueDMolecular and clinical measures of cell adhesion under the synergystic influence of diabetic nephropathy and high glucose [abstract]2004Meeting Proceedings: Annual Scientific Meeting of the Australian Diabetes Society62
- VlassaraHCaiWCrandallJInflammatory mediators are induced by dietary glycotoxins, a major risk factor for diabetic angiopathyProc Natl Acad Sci U S A20039915596601 Erratum: 2003. Proc Natl Acad Sci U S A, 100:76312429856
- WilliamsPSFassGBoneJMRenal pathology and proteinuria determine progression in untreated mild/moderate chronic renal failureQ J Med198867343543205906
- YuyunMFKhawKTLubenRMicroalbuminuria independently predicts all-cause and cardiovascular mortality in a British population: The European Prospective Investigation into Cancer in Norfolk (EPIC-Norfolk) population studyInt J Epidemiol2004331899815075168