Abstract
Initially considered as a semipermeable barrier separating lumen from vessel wall, the endothelium is now recognised as a complex endocrine organ responsible for a variety of physiological processes vital for vascular homeostasis. These include the regulation of vascular tone, luminal diameter, and blood flow; hemostasis and thrombolysis; platelet and leucocyte vessel-wall interactions; the regulation of vascular permeability; and tissue growth and remodelling. The endothelium modulates arterial stiffness, which precedes overt atherosclerosis and is an independent predictor of cardiovascular events. Unsurprisingly, dysfunction of the endothelium may be considered as an early and potentially reversible step in the process of atherogenesis and numerous methods have been developed to assess endothelial status and large artery stiffness. Methodology includes flow-mediated dilatation of the brachial artery, assessment of coronary flow reserve, carotid intimamedia thickness, pulse wave analysis, pulse wave velocity, and plethysmography. This review outlines the various modalities, indications, and limitations of available methods to assess arterial dysfunction and vascular risk.
The vascular endothelium
The endothelium has an important role in maintaining vascular homeostasis. Although once considered simply as a semipermeable membrane, endothelial cells transduce a wide range of physiological stimuli, and in response, produce a variety of signalling molecules that exert autocrine and paracrine effects. The endothelium can therefore be considered as an important endocrine organ (CitationVanhoutte et al 1989; CitationVane et al 1990), and is responsible for maintaining vasomotor tone, hemostasis and thrombosis, inflammatory processes, platelet and leucocyte vessel-wall interactions, and controlling vascular permeability. The equilibrium between vasodilatation and vasoconstriction in regional vascular beds is largely controlled by the interaction between endothelium-derived vasoactive mediators and the vascular smooth muscle layer. Endothelial nitric oxide (NO), produced by constitutive activity of nitric oxide synthase (eNOS) (CitationSchini-Kerth 1999), is a potent vasodilator and one of the most important regulators of vascular tone. In addition, NO is antiatherogenic, inhibiting platelet aggregation, smooth muscle proliferation, expression of adhesion molecules, and neutrophil aggregation (CitationVanhoutte et al 1989; CitationVane et al 1990). Arterial endothelial dysfunction is a key, early, and potentially reversible, event in the process of atherogenesis and is characterised by impaired NO bioavailability (CitationHealy 1990; CitationRoss 1993; CitationBerliner et al 1995). Endothelial dysfunction causes impaired vasomotor responses to various neurohumoral stimuli which may contribute to transient myocardial ischemia, plaque rupture, thrombosis, and myocardial infarction (CitationMaseri et al 1978). Endothelial dysfunction has so far been described in association with many established cardiovascular risk factors such as active and passive smoking, hypertension, hypercholesterolemia, obesity, and type II diabetes (CitationMcVeigh et al 1992; CitationAnderson, Meredith, et al 1995; CitationTreasure et al 1995; CitationGoodfellow et al 1996; CitationWilliams et al 1996; CitationKoller 2002; CitationWilliams et al 2002). The extent of endothelial dysfunction and vasomotor responsiveness correlates with the rate of progression of atherosclerosis and cardiovascular events (CitationSchachinger et al 2000; CitationWidlansky et al 2003). As such, endothelial function has importance, not only in determining predisposition to atherosclerotic disease, but also in determining prognosis in clinically affected patients.
Clinical assessment of endothelial function
Endothelial function can be measured in a variety of ways using invasive and noninvasive techniques in the coronary and peripheral circulation. The clinical examination of endothelial function involves assessing the ability of the endothelium to release NO in response to various exogenous and endogenous stimuli. The quantity of NO released from endothelial cells determines the degree of vasodilatation detected in clinical studies, and thus arterial “health”. CitationLudmer and collegues (1986) initially tested this concept by infusing acetylcholine into coronary arteries at angiography and measuring subsequent changes in arterial diameter. In healthy arteries, infusion of acetylcholine caused vasodilation, whereas vasoconstriction occurred in the presence of a damaged endothelial lining. Further evidence that the observed vasodilation was secondary to NO release was derived from studies which blocked dilatation using inhibitors of the L-arginine-NO pathway (CitationHodgson and Marshall 1989; CitationLefroy et al 1993). Subsequent studies using vasoactive pharmacological and physiological agents have confirmed differences in dilatation and endothelial responsiveness between healthy vessels and atherosclerotic vessels (CitationGollino et al 1991; CitationYeung et al 1991).
Coronary angiography
Methods of assessment
Quantitative coronary artery angiography of the left anterior descending artery and intracoronary doppler techniques have been applied to measure coronary artery vaso-responsiveness in response to endothelium-dependent agonists such as bradykinin and mechanical stimuli such as increased flow. Quantitative angiography can assess coronary arterial luminal diameter following cardiac catheterization, whilst doppler probes evaluate blood flow velocity in response to infusion of vasoactive agents (CitationGroves et al 1995).
The integrity of coronary arteries has recently been evaluated angiographically via stimulation of the sympathetic nervous system using exercise and cold pressor tests. Sympathetic neuronal stimulation using cold pressor testing induces vasodilatation in healthy vasculature and vasoconstriction in proatherogenic disease states and atherosclerotic coronary arteries (CitationZeiher et al 1991; CitationAntony et al 1994; CitationNitenberg et al 1998).
Although the coronary angiography technique is undoubtedly a useful tool for assessing vascular risk, widespread use is not practical. Coronary angiography is invasive and unsuitable for studying early preclinical atherosclerosis in asymptomatic subjects, or for the serial evaluation of vascular physiology in response to potential antiatherogenic strategies. Furthermore, its use is limited as a consequence of serious adverse reactions reported following the intracoronary infusion of acetylcholine at angiography (CitationTio et al 2002).
Association with coronary artery disease and atherosclerotic risk factors
Impaired vascular reactivity in the coronary artery circulation is associated with traditional coronary risk factors such as type 2 diabetes, insulin resistance, hypertension, and dyslipidemia (CitationNitenberg et al 1998; CitationDagres et al 2004; CitationMokelke et al 2005), even in the absence of clinically overt atherosclerotic lesions. Impaired vascular reactivity may also serve as an index integrating the overall stress imposed by coronary risk factors (CitationVogel and Corretti 1998). Coronary endothelial vasodilator dysfunction persists after angiographically significant coronary atherosclerotic plaque is evident and has been shown to predict long-term disease progression and cardiovascular event rates in patients at risk of coronary disease (CitationSchachinger et al 2000). However, disease modifying agents which reduce cholesterol and exhibit antioxidant qualities improve coronary artery endothelium-dependent dilatation (CitationAnderson, Meredith, et al 1995; CitationTreasure et al 1995) and may reflect the cardioprotective qualities of these agents.
Flow-mediated dilatation
Method of assessment
A noninvasive technique using high-resolution ultrasound to overcome the practical constraints of invasive coronary artery testing has been developed to assess endothelial function in the peripheral circulation (CitationCelermajer et al 1992). Using this technique, changes in brachial artery diameter are measured by following the endothelium-dependent stimulus of increased blood flow and may be compared with changes in vessel diameter following the oral administration of endothelium-independent agonists such as glyceryl trinitrate (GTN) (CitationCelemajer et al 1992). Since endothelial dysfunction is a generalized systemic process, it occurs in both the coronary and systemic circulation (CitationAnderson, Gerhard, et al 1995). Indeed, a close relationship has been demonstrated between vasodilator responses in the brachial artery and those in the coronary circulation (CitationAnderson, Uehata, et al 1995; CitationMatsuo et al 2004). The sensitivity of the original technique developed by CitationCelermajer et al (1992) has been improved by using a validated computerized vessel wall tracking system (Vadirec Medical Systems® [CitationRamsey et al 1995]) to follow changes in brachial artery diameter throughout the cardiac cycle.
Many wall tracking systems have been developed to determine flow-mediated dilatation (FMD). One such system comprises an adapted duplex colour flow echo machine, giving high axial resolution (CitationRamsey et al 1995). With this technique, the brachial artery is identified using an ultrasound transducer with a stand-off device containing ultrasound coupling gel placed between the transducer and the arm to prevent compression of the anterior wall of the artery. Vessel wall movements are tracked using the stored radio frequency signals to produce displacement waveforms of the anterior and posterior walls together with the distension waveform (diameter change as a function of time [CitationHoeks et al 1990]). The distension waveform allows measurement of end-diastolic diameter for each beat, providing a theoretical resolution of 3 m. Forearm blood flow is measured throughout the study using a continuous wave doppler probe positioned over the brachial artery (CitationSmith et al 2002). Once baseline measurements of brachial artery diameter are established, a cuff placed at the wrist is inflated to suprasystolic pressure, causing relative hand ischemia. Release of the occluding cuff results in reactive hand hyperemia and an associated increase in blood flow through the brachial artery, which induces shear stress on the arterial wall and provides a stimulus for endothelium-dependent dilatation. Similar measurements can also be made using a NO donor, eg, glyceryl trinitrate (GTN) for an assessment of endothelial-independent vasodilatation (CitationCelermajer et al 1992).
A degree of investigator expertise is required to determine brachial artery vasodilation using ultrasonography and no consensus exists regarding the degree of vasodilation which should be expected in individuals with healthy endothelial function (CitationFaulx et al 2003). Significant changes in brachial artery reactivity have been reported within healthy subjects throughout the course of a day when measured by the same operators, suggesting that variability occurs between morning and evening measurements, in addition to variability between subjects examined on different days (CitationDe Roos et al 2003). However, this is disputed by others who have carefully controlled for confounding factors (Citationter Avest et al 2005). Despite this, FMD will continue to be an extensively used technique for assessing endothelial function. Improvements in available equipment and operator expertise will reduce variability in results.
Association with coronary artery disease and atherosclerotic risk factors
The FMD technique is now one of the most widely used noninvasive methods of assessing endothelial function and closely correlates with cardiovascular risk (CitationKuvin and Karas 2003). Impaired FMD is described in insulin resistant states and type 2 diabetes, dyslipidemia, hypertension, end stage renal disease, and smoking (CitationYildiz et al 2003; CitationEsen et al 2004; CitationHolay et al 2004; CitationThomas et al 2004). Subsequently, FMD has been used extensively to assess the potential antiatherogenic qualities of treatment options, and continues to be indispensable in determining endothelial integrity.
Carotid intimamedial thickness
Method of assessment
Another noninvasive method of assessing subclinical atherosclerosis involves measurements of carotid intimamedia thickness (IMT) with high resolution B-mode ultrasonography. This is a well established technique which has been extensively used to estimate coronary artery events and the extent of established atherosclerosis in central and peripheral vasculature (CitationBots et al 1993), with early increases in IMT possibly reflecting adaptation to elevated intravascular shear stress (CitationBots et al 1997). As a noninvasive imaging technique, quantitative carotid IMT is versatile for use in large populations with minimal risk to subjects (CitationBarth 2004). However, accurate measurements, particularly of the near wall, require a high level of technical expertise. Consequently, some authors suggest the administration of contrast media during the examination period (CitationMacioch et al 2004; CitationMartin and Lekaris 2004).
A variety of techniques have been used in the determination of carotid IMT. Measurements of the common carotid, internal carotid, and carotid bifurcation are all technically acceptable, including combination measurements of 12 carotid arterial sites, eg, using Meijer's Arch (CitationBots et al 2003). In view of the diversity and lack of uniformity in determining carotid IMT, meta-analysis suggests that circumferential scanning of the carotid artery and calculation of the mean maximum carotid IMT provides a more accurate measurement of carotid atherosclerosis (CitationBots et al 2003). However, all sites of carotid IMT measurement appear to have equivalent value in predicting future coronary artery events (CitationIglesias del Sol et al 2002).
Association with coronary artery disease and atherosclerotic risk factors
Carotid IMT correlates with cardiovascular risk factors such as the ‘metabolic syndrome’ (CitationMcNeill et al 2004), insulin resistance in type 1 and 2 diabetics (CitationFujiwara et al 2003; CitationSingh 2003), microalbuminuria (CitationJadhav and Kadam 2002), hypercholesterolemia (CitationWendelhag et al 1992), and atherogenesis (CitationSalonen and Salonen 1993).
Carotid IMT and the progression of IMT correlates well with cardiovascular and cerebrovascular end-points (CitationBots et al 1997; CitationHodis et al 1998; CitationO'Leary et al 1999). However, although extensive data supports the use of carotid IMT as a predictor of cardiovascular risk, endothelial dysfunction manifesting as impaired brachial artery reactivity may be an earlier predictor of coronary artery disease, with increased carotid IMT being evident at a later stage in the process of atherogenesis (CitationFurumoto et al 2002).
Cardiovascular risk and vascular stiffness
Large artery stiffness
Arteriosclerosis is an integral part of the aging process (CitationPearson et al 1994) and is now also recognised as an important and independent risk factor for cardiovascular disease (CitationArnett et al 1994). As a result of vascular stiffening, the diastolic blood pressure decreases and pulse pressure widens, as occurs with advancing age (CitationFranklin et al 1997). Consequently, brachial artery pulse pressure is a surrogate marker of vascular stiffness and is used to determine cardiovascular risk in normotensive and hypertensive subjects (CitationBenetos et al 1997, Citation1998; CitationFranklin et al 1999), having a higher predictive value of cardiovascular risk than mean arterial blood pressure (CitationDomanski et al 1999; CitationMiller et al 1999). Isolated systolic hypertension and elevated pulse pressure have also been identified as a major cardiovascular risk factor in the Systolic Hypertension in the Elderly Programme and the Systolic Hypertension in Europe trial (CitationFrishman 2000).
Confirming the association between pulse pressure and cardiovascular risk, CitationPhilippe et al (2002) demonstrated a direct correlation between aortic pulse pressure, measured with intra-aortic balloons at coronary angiography, and the extent of atherosclerotic disease. Wave reflection within the vascular tree leads to a higher pulse pressure in central vessels than in the periphery (CitationPauca et al 1992; CitationNichols and O'Rourke 1998, Citation2005). The resulting increase in left ventricular after-load increases myocardial oxygen consumption and promotes left ventricular hypertrophy. In addition, increasing systolic pressure elevates arterial wall circumferential stress and predisposes to atherosclerotic plaque generation. Left ventricular hypertrophy that arises from increased aortic systolic pressure (CitationLakatta 1991) predisposes to coronary artery disease (CitationMacMahon et al 1990), cerebrovascular events (CitationKannel et al 1981), and is an independent predictor of cardiovascular mortality (CitationLevy et al 1990). Furthermore, increased arterial stiffening has also been demonstrated in subjects with increased cardiovascular risk including diabetes mellitus (CitationWahlqvist et al 1988, CitationSalomaa et al 1995), hypertension (CitationMcVeigh et al 1991, CitationArmentano et al 1991), hypercholesterolemia (CitationDart et al 1991, CitationGiannattasio et al 1996), and end stage renal disease (CitationBlacher et al 2002).
Regulation of large artery stiffness
Elastin and collagen are the major determinants of large artery stiffness, with smooth muscle originally thought to play a minor role (CitationWilkinson and McEniery 2004). Advancing age causes gradual destruction in arterial wall elasticity, with increasing demands placed on the collagenous element (CitationO'Rourke 1976; CitationAvolio et al 1983). This redistribution of the heterogeneous element in the vascular wall can be triggered by endothelial dysfunction (CitationNili et al 2002). However, recent work has highlighted the importance of smooth muscle in determining vessel stiffening. Vasoconstrictors such as noradrenaline can increase vascular stiffness and dilators such as hydrallazine and sodium nitroprusside have the opposite effect (CitationNichols and O'Rourke 2005). Such vasoactive pharmacological agents can alter vessel diameter by up to 30%, independent of changes in peripheral resistance or blood pressure (CitationLatson et al 1988), demonstrating the important dynamic contribution of vascular smooth muscle to large vessel stiffness.
Whilst NO profoundly alters basal arterial tone, its effect on arterial stiffness remains unclear. However, the acute administration of a NO donor such as GTN produces changes in the peripheral pressure pulse that are consistent with a reduction in arterial stiffness (CitationCockcroft et al 1997). β-adrenergic drugs, in particular albuterol, act via the L-arginine-NO pathway to stimulate NO release and cause vasodilatation in resistance arteries (CitationCardillo et al 1997; CitationDawes et al 1997) via their action on β2-adrenoreceptors. β2-agonists have therefore been used to evaluate endothelial integrity in healthy controls (CitationHayward et al 2002).
Clinical assessment of arterial stiffness
Pulse wave analysis and pulse wave velocity
Method of assessment
The peripheral pressure waveform can be useful in determining cardiovascular risk. However, an adequate assessment of central arterial pressure waveforms cannot be determined from peripheral pulse wave analysis (PWA) because changes in vessel stiffening throughout the vascular tree causes location-dependent changes in the pressure waveform. In addition, central arterial waveforms will be influenced by the reflective wave phenomenon as described by CitationNichols and O'Rourke (2005). The systolic waveform leaves the aortic root and travels to the periphery, where smaller arterioles provide multiple points of reflection. A resulting ‘reflective’ wave is generated and returns to central arteries (CitationO'Rourke and Kelly 1993). In individuals with healthy compliant arteries, the reflective wave will return to the central vasculature in diastole and augment diastolic coronary arterial blood flow. The speed of the advancing wave is termed pulse wave velocity (PWV) (CitationLehmann et al 1997). With age, a combination of increased reflective capacity at peripheral sites and faster PWV within stiffened vessels causes premature augmentation of the systolic waveform, forming a ‘late systolic peak’ on waveform analysis (). This explains the differences between the brachial and aortic pressure waveforms, which may be as high as 20 mmHg (CitationPauca et al 1992). The central pressure waveform is important in view of determining left ventricular workload, which is relatively independent of the brachial pressure.
Figure 1 Representation of central arterial waveform.
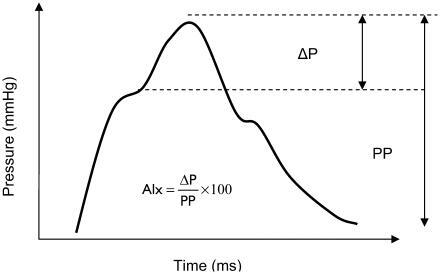
In view of the above observations, a technique has been derived by CitationO'Rourke and Gallagher (1996), which is able to noninvasively record the peripheral pulse pressure wave and generate a corresponding central arterial waveform. The technique involves the use of an applanation tonometer to record the radial pulse wave. Applanation tonometry causes partial flattening of the arterial wall and equilibration of intra-arterial circumferential pressure. The accuracy of arterial tonometry in recording peripheral waveforms has been described by previous investigators who evaluated waveforms derived from noninvasive tonometry and direct arterial puncture (CitationCohn et al 1995). The central arterial waveform can subsequently be derived from the peripheral waveform using a validated generalized transfer factor (CitationKaramanoglu et al 1993; CitationChen et al 1997; CitationTakazawa et al 1998; CitationFetics et al 1999). This is then expressed in terms of an Augmentation Index (AIx) which can be used to assess vascular stiffness and cardiovascular risk between study groups.
Pulse wave analysis has more recently been used as a noninvasive tool to assess endothelial function (CitationWilkinson, Hall, et al 2002). Administration of β-agonist therapy induces repeatable reductions in the AIx, which are inhibited by infusion of L-NG-monomethyl arginine (L-NMMA), suggesting that observed differences are endothelial- and NO-dependent (CitationWilkinson, Hall, et al 2002). Nitroglycerin administration induces further reductions in the AIx which are unaffected by L-NMMA and thus endothelial-independent (CitationWilkinson, Hall, et al 2002). Furthermore, the technique has been shown to correlate with FMD in healthy and type 2 diabetic subjects (CitationWilson et al 2004).
The analysis of PWV uses a similar system that calculates pulse wave propagation velocity between two sites, commonly the carotid and femoral pulses, or carotid and radial (CitationOliver and Webb 2003), although brachial-ankle PWV has been assessed by some (CitationKatayama et al 2004; CitationIgarashi et al 2005). Pulse wave velocity is inversely proportional to vessel stiffness and distensibility (CitationNichols and O'Rourke 2005). Waveform data is recorded from two sites using noninvasive tonometry and stored electronically. Following documentation of the distance between the two recording sites, determination of the pulse transit time allows calculation of PWV. In order to assess pulse transit time a correlation point is identified within the pressure waveform, which may be the foot of the pressure wave (using SphygmoCor system) or the point of maximal upstroke (using Complior system) (CitationMillasseau et al 2005). If the two pressure waveforms are not recorded simultaneously, an R wave on the electrocardiograph can be used to calculate wave transit time. Elevation of PWV leads to augmentation of the ascending aortic systolic waveform as previously outlined, resulting in higher left ventricular afterload and amplification of pulse pressure (CitationNichols 2005).
Pulse wave analysis and PWV are both noninvasive simple techniques that can be used to assess vascular stiffness in research and clinical settings (CitationO’Rourke and Gallagher 1996; CitationHayward et al 2002; CitationSutton-Tyrrell et al 2005). Both techniques are influenced by factors that may confound data. For example, elevation in pulse rate will lower the AIx as a result of a reduction in reflective wave amplitude, and does not represent a change in vascular stiffness (CitationWilkinson, Mohammed, et al 2002). Consequently, a correction factor has been suggested to standardize for variation in heart rate (CitationWilkinson et al 2000). In addition, an inverse relationship between AIx, PWV, and height has been described, which may result from shorter reflective wave propagation time in individuals with short stature (CitationMcGrath et al 2001). While some investigators consider this a confounding variable in data analysis, it may explain the elevation in cardiovascular risk observed in short individuals (CitationKannam et al 1994). Despite the lack of data to confirm correlation between noninvasive and invasive measurements of PWV (CitationChiu et al 1991; CitationDavies and Struthers 2003), the evidence that tonometer-derived PWV is an important determinant of cardiovascular risk is difficult to dispute.
Association with coronary artery disease and atherosclerotic risk factors
Pulse wave analysis has revealed accelerated large artery stiffening and endothelial dysfunction in association with several well established cardiovascular risk factors such as obesity (CitationSuh et al 2005), end-stage renal failure (CitationCovic et al 2003), and hypercholesterolemia (CitationWilkinson, Prasad, et al 2002). Similarly, PWV is increased in microalbuminuria (CitationSmith et al 2005), renal dysfunction (CitationHaydar et al 2004), type 2 diabetes (CitationTsuchiya et al 2004), and insulin resistance (CitationSengstock et al 2005).
Using PWA and PWV, vascular stiffness has been assessed and identified as an independent risk marker for cardiovascular mortality (CitationLaurent et al 2001; CitationMeaume et al 2001) and cerebrovascular events (CitationLaurent and Boutouyrie 2005), and has a prognostic value equivalent to currently available biomarkers.
Elevations of central systolic pressure and consequent proatherosclerotic effects can be modified by vasodilatory compounds which reduce PWV in peripheral vessels without altering brachial blood pressure. Such reductions in augmentation of central pressure may underlie the observed benefits of cardiovascular drugs which are not currently attributed to blood pressure modification (CitationNichols 2005). Vascular stiffness has consequently gained increasing importance as a therapeutic target.
Photophlesymographic assessment of pulse wave reflection
Method of assessment
Photophlethysmography involves measuring the digital volume pulse via infrared light transmission through the finger. Previous investigators have demonstrated that the digital volume pulse resembles the carotid pressure wave and alters in a similar way to vasoactive mediators (CitationTakazawa et al 1998). Reflected peripheral waveforms cause a second peak in the digital volume pulse (DVP) in a similar fashion to that seen in the peripheral pressure waveform, as measured using PWA (CitationChowienczyk et al 1999). With this technique, the point at which the reflective wave meets the systolic waveform is termed the inflection point (IP). When suprasystolic pressure is applied to both lower limbs at thigh level, the reflective wave returns sooner and causes an expected elevation of the IP (CitationChowienczyk et al 1999). In a similar way to the peripheral pressure wave, the DVP undergoes changes in response to exogenous NO donors such as GTN (CitationMorikawa 1967; CitationLund 1986), which is independent of changes in heart rate (CitationChowienczyk et al 1999). Using both techniques, the major change seen is a reduction in the diastolic component of the waveform and the preceding IP (CitationChowienczyk et al 1999). This has been demonstrated recently in vivo, where acetylcholine-induced endothelial-derived NO release resulted in lowering of the IP in the photophlethysmographic waveform recorded in cholesterol-fed rabbits. This response is diminished in cholesterol-fed rabbits when compared with healthy rabbits and antagonised by NOS inhibitors (CitationKlemsdal et al 1994). As with PWA, pharmacological preparations which induce NO release, such as β-adrenergic drugs, will also cause a reduction in the IP of the pulse volume waveform (CitationChowienczyk et al 1999). Such effects are blunted by L-NMMA administration which suggests that this effect involves the L-arginine-NO pathway (CitationChowienczyk et al 1999).
Association with coronary artery disease and atherosclerotic risk factors
With evidence supporting the use of this technique to assess both endothelial-dependent and endothelial-independent vasodilatation, investigators have studied patient groups who are known to demonstrate marked endothelial dysfunction. Photophlethysmographic examination of type 2 diabetics has shown impairment of albuterol-induced responses with preservation of the endothelial-independent vasodilatation seen with GTN (CitationChowienczyk et al 1999). Vascular stiffness using this technique has also been described in cases of impaired glucose tolerance (CitationOhshita et al 2004) and hypertension in aging individuals, although some authors believe the technique to be inferior to PWV (CitationBortolotto et al 2000). However, this noninvasive technique provides a useful method of assessing vascular stiffening, in which both endothelial-dependent and independent responses can be determined (CitationMillasseau et al 2002).
Biomarkers of endothelial function
As outlined previously, the antiatherogenic functions of the endothelium are complex. Several biochemical markers have been identified that correlate with coronary artery disease and conventional cardiovascular risk factors (CitationSzmitko et al 2003). Further investigation of the inflammatory and thrombotic processes involved in atherogenesis will allow the assessment of potential biomarkers which may be incorporated into current cardiovascular risk stratification models. Such biomarkers include, oxidized low-density lipoprotein (oxLDL), high sensitivity C-reactive protein (CRP), endothelial progenitor cells (EPC), prothrombotic factors such as von Willebrand factor (VWF), and inflammatory markers including tumor necrosis factor-α (TNF-α), interleukin-6 (IL-6), and intracellular adhesion molecule-1 (ICAM-1) (CitationRidker et al 2001; CitationSzmitko et al 2003). The clinical use of many of the biomarkers is restricted due to lack of end-point data (CitationTsimikas and Witztum 2001), with the exception of CRP which may correlate to a greater extent than traditional risk factors such as LDL-cholesterol (CitationRidker et al 2005). In consequence, CRP has already been incorporated into some risk stratification models.
Oxidized LDL
Oxidation of LDL occurs within the subendothelial cells of the vascular tissue which promotes the binding and transformation of monocytes to foam cells (CitationParhami et al 1993; CitationWatson et al 1997). Mechanisms include enhancing chemotaxis and monocyte adhesion, upregulation of inflammatory genes and growth factors, causing endothelial cell dysfunction and apoptosis, enhancing platelet aggregation with thrombus formation, and inducing plaque destabilisation (CitationBerliner et al 1995; CitationAikawa et al 1998; CitationNorata et al 2002). Consequently, oxLDL levels are increased in cases of acute coronary syndrome and myocardial infarction (CitationTsimikas et al 2003).
Prothrombotic factors
The prerequisites for thrombogenesis in atheromatous plaques include activation of the coagulation cascade and platelet activation (CitationSmith et al 2003). As such, prothrombotic factors are often evaluated in studies aimed at assessing cardiovascular risk. von Willebrand factor is a multimeric glycoprotein that is synthesised in endothelial cells and released following endothelial damage (CitationMannucci 1998). As such, levels can be indicative of the degree of endothelial injury and subsequent atherosclerotic potential (CitationMannucci 1998). Prospective trials suggest that elevated VWF may predict future cardiovascular events in patients with established coronary atherosclerosis (CitationJansson et al 1991; CitationThompson et al 1995), which may be a reflection of the role of VWF in initiating platelet aggregation and thrombus formation (CitationMannucci 1998). von Willebrand factor also has a role in stabilising factor VIII and the latter, together with fibrinogen, have been incorporated into cardiovascular risk profiles in numerous studies (CitationWilhelmsen et al 1984; CitationFolsom et al 1999; CitationChambless et al 2003; CitationChaves et al 2004).
Endothelial progenitor cells
Endothelial progenitor cells have also gained importance as a potential surrogate marker of endothelial health (CitationSchmidt-Lucke et al 2005). These are essentially stem cells which are recruited to sites of endothelial injury in order to perform a therapeutic function by differentiating into mature endothelial cells (CitationSzmitko et al 2003). Depletion of circulating EPCs with impaired adhesion to vasculature may reflect repeated and enhanced demand for EPC mobilization from bone marrow, and indicate a state of endothelial dysfunction predisposing to enhanced cardiovascular risk (CitationHill et al 2003). In support of this, reduced EPC levels with impaired activity have been demonstrated in subjects known to have impaired endothelial function, such as hypertension and ischemic heart disease (CitationVasa et al 2001) and their use for therapeutic intervention of vascular dysfunction continues to be evaluated (CitationSilva et al 2005).
Inflammatory markers
Several inflammatory markers have been described in association with cardiovascular risk, including TNF-α, IL-6, ICAM-1, and CRP, of which CRP has greatest prognostic value (CitationRidker et al 2001; CitationRidker 2002). CRP is not only a marker of cardiovascular risk, but may itself function as a proatherogenic molecule (CitationSzmitko et al 2003). The acute phase reactant has been demonstrated to enhance proinflammatory cytokines, such as IL-6, TNF-α, and monocyte chemoattractant protein-1 (MCP-1), promoting chemotaxis and lipid accumulation (CitationVerma, Li, et al 2002; CitationLi and Fang 2004). In addition, CRP may interfere with NO synthesis, inhibit angiogenesis, and influence vascular remodelling (CitationVerma, Wang, et al 2002; CitationWang et al 2003). Although CRP correlates well with atherogenesis, it is feasible that elevation reflects the impact of traditional risk factors on inflammatory processes, as opposed to the direct influence of CRP on endothelial function (CitationVita et al 2004; CitationVerma et al 2004).
Summary
As the number of individuals suffering from the ‘metabolic syndrome’ escalates, the cardiovascular morbidity and mortality rates of future generations may continue to rise despite advances in pharmaceutical interventions. Disruption of endothelial function is multifactorial and complex, and precedes clinically apparent coronary and cerebrovascular disease.
Therefore, the evaluation of reproducible, noninvasive techniques for assessing endothelial function should enable screening of large populations and may guide interventions designed specifically to reduce the individual's vascular risk.
References
- AikawaMRabkinEOkadaYLipid lowering by diet reduces matrix metalloproteinase activity and increases collagen content of rabbit atheroma: a potential mechanism of lesion stabilisationCirculation1998972433449641696
- AndersonTJMeredithITYeungACThe effect of cholesterol-lowering and antioxidant therapy on endothelium-dependent coronary vasomotionN Eng J Med199533248893
- AndersonTJGerhardMDMeredithITSystemic nature of endothelial dysfunction in atherosclerosisAm J Cardiol19957571B74B7801869
- AndersonTJUehataAGerhardMDClose relation of endothelial function in the human coronary and peripheral circulationJ Am Coll Cardiol1995261235417594037
- AntonyIAptecarELereboursGCoronary artery constriction caused by the cold pressor test in human hypertensionHypertension199424212198039846
- ArmentanoRSimonALevensonJMechanical pressure versus intrinsic effects of hypertension on large arteries in humansHypertension199118657641937668
- ArnettDKEvansGWRileyWAArterial stiffness: a new cardiovascular risk factorAm J Epidemiol1994140669827942769
- AvolioAPChenSGWangRPEffects of ageing on changing arterial compliance and left ventricular load in a northern Chinese urban communityCirculation1983685086851054
- BarthJDCarotid intima media thickness and beyondCurr Drug Targets Cardiovasc Hematol Disord2004412945
- BenetosARudnichiASafarMPulse pressure and cardiovascular mortality in normotensive and hypertensive subjectsHypertension19983256049740626
- BenetosASafarMRudnichiAPulse pressure: a predictor of long-term cardiovascular mortality in a French male populationHypertension1997301410159403561
- BerlinerJNavabMFogelmanAAtherosclerosis: basic mechanismsCirculation1995912488967729036
- BlacherJSafarMEPannierBPrognostic significance of arterial stiffness measurements in end-stage renal disease patientsCurr Opin Nephrol Hypertens2002116293412394609
- BortolottoLABlacherJKondoTAssessment of vascular aging and atherosclerosis in hypertensive subjects: second derivative of photophlethysmogram versus pulse wave velocityAm J Hypertens2000131657110701816
- BotsMLEvansGWRileyWACarotid intima-media thickness measurements in intervention studies: design options, progression rates, and sample size considerations; a point of viewStroke20033429859414615619
- BotsMLHoesAWKoudstaalPJCommon carotid intimamedia thickness and risk of stroke and myocardial infarction: the Rotterdam studyCirculation199796143279315528
- BotsMLWittemanJCGrobbeeDECarotid intima-media wall thickness in elderly women with and without atherosclerosis of the abdominal aortaAtherosclerosis1993102991058257458
- CardilloCKilcoyneCMQuyyumiAADecreased vasodilator response to isoproterenol during nitric oxide inhibition in humansHypertension199730918219336393
- CelermajerDSSorensenKEGoochVNon-invasive detection of endothelial dysfunction in children and adults at risk of atherosclerosisLancet19923401111151359209
- ChamblessLEFolsomARSharrettARCoronary heart disease risk prediction in the Atherosclerosis Risk in Communities (ARIC) studyJ Clin Epidemiol2003568809014505774
- ChavesPHKullerLHO'LearyDHSubclinical cardiovascular disease on older adults: insights from the Cardiovascular Health StudyAm J Geriatr Cardiol2004131375115133417
- ChenCHNevoEFeticsBEstimation of central aortic pressure waveform by mathematical transformation of radial tonometry pressureCirculation1997951827369107170
- ChiuYCArandPWShroffSGDetermination of pulse wave velocities with computerised algorithmsAm Heart J19911211460702017978
- ChowienczykPKellyRMacCallumHPhotophlesymographic assessment of pulse wave reflection: blunted response to endothelium-dependent beta2-adrenergic vasodilation in type II diabetes mellitusJ Am Coll Cardiol19993420071410588217
- CockcroftJRWilkinsonIBWebbDJThe Trevor Howell Lecture. Age, arterial stiffness and the endotheliumAge Ageing199726Suppl 453609506434
- CohnJFinkelsteinSMcVeighGNon-invasive pulse wave analysis for the early detection of vascular diseaseHypertension19952650387649589
- CovicAGoldsmithDJGusbeth-TatomirPSuccessful renal transplantation decreases aortic stiffness and increases vascular reactivity in dialysis patientsTransplantation2003761573714702526
- DagresNSallerBHaudeMInsulin sensitivity and coronary vasoreactivity: insulin sensitivity relates to adenosine-stimulated coronary flow response in human subjectsClin Endocrinol (Oxf)2004617243115579187
- DartAMLancombeFYeohJKAortic distensibility in patients with isolated hypercholesterolaemia, coronary artery disease, or cardiac transplantationLancet199133827031677109
- DaviesJIStruthersAPulse wave analysis and pulse wave velocity: a critical review of their strengths and weaknessesJ Hypertens2003214637212640232
- DawesMChowienczykPJRitterJMEffects of inhibition of the L-arginine/nitric oxide pathway on vasodilation caused by beta-adrenergic agonists in human forearmCirculation199795229379142007
- De RoosNMBotsMLSchoutenEWithin subject variability of flow mediated vasodilation of the brachial artery in healthy men and women: implications for experimental studiesUltrasound Med Biol200329401612706191
- DomanskiMJDavisBRPfefferMAIsolated systolic hypertension: prognostic information provided by pulse pressureHypertension1999343758010489379
- EsenAMBarutcuIAcarMEffect of smoking on endothelial function and wall thickness of brachial arteryCirc Res20046811236
- FaulxMDWrightATHoitBDDetection of endothelial dysfunction with brachial artery ultrasound scanningAm Heart J20031459435112796748
- FeticsBNevoEChenCHParametric model derivation of transfer function for non-invasive estimation of aortic pressure by radial tonometryIEEE Trans Biomed Eng19994669870610356876
- FolsomARRosamondWDShaharEProspective study of markers of hemostatic function with risk of ischaemic stroke. The Atherosclerosis Risk in Communities (ARIC) Study InvestigatorsCirculation19991007364210449696
- FranklinSSKhanSAWongNDIs pulse pressure useful in predicting risk for coronary heart disease? The Framingham Heart StudyCirculation19991003546010421594
- FranklinSSGustinW4thWongNDHemodynamic patterns of age-related changes in blood pressure: The Framingham Heart StudyCirculation199796308159236450
- FrishmanWHIncreased vascular compliance/decreased cardiovascular risk: what the studies tell usHeart Dis20002384811728287
- FujiwaraSEmotoMKomatsuMArterial wall thickness is associated with insulin resistance in type 2 diabetic patientsJ Atheroscler Thromb2003102465214566088
- FurumotoTFujiiSSaitoNRelationships between brachial artery flow mediated dilation and carotid artery intima-media thickness in patients with suspected coronary artery diseaseJpn Heart J2002431172512025898
- GiannattasioCMangonicAAFaillaMImpaired radial artery compliance in normotensive subjects with familial hypercholesterolemiaAtherosclerosis1996124249608830937
- GollinoPPiscioneFWillersonJTDivergent effects of serotonin on coronary artery dimensions and blood flow in patients with coronary atherosclerosis and control patientsN Engl J Med199132464181994246
- GoodfellowJRamseyMWLuddingtonLAEndothelium and inelastic arteries: an early marker of vascular dysfunction in non-insulin dependent diabetesBr Med J199631274458605460
- GrovesPKurzSJustHRole of endogenous bradykinin in human coronary vasomotor controlCirculation1995923424308521563
- HaydarAACovicAColhounHCoronary artery calcification and aortic pulse wave velocity in chronic kidney disease patientsKidney Int2004651790415086918
- HaywardCSKraidlyMWebbCMAssessment of endothelial function using peripheral waveform analysis: a clinical applicationJ Am Coll Cardiol200240521812142121
- HealyBEndothelial cell dysfunction: an emerging endocrinopathy linked to coronary diseaseJ Am Coll Cardiol19901635782197313
- HillJMZalosGHalcoxJPCirculating endothelial progenitor cells, vascular function and cardiovascular riskN Eng J Med2003348593600
- HodgsonJMMarshallJJDirect vasoconstriction and endothelium-dependent vasodilation: mechanisms of acetylcholine effects on coronary flow and arterial diameter in patients with nonstenotic coronary arteriesCirculation1989791043512785440
- HodisHNMackWJLaBreeLThe role of carotid arterial intima-media thickness in predicting clinical coronary eventsAnn Intern Med199812826299471928
- HoeksABrandsPSmeetsFAssessment of the distensibility of superficial arteriesUltrasound Med Biol19901612182183458
- HolayMPPaunikarNPJoshiPPEffect of passive smoking on endothelial function in healthy adultsJ Assoc Physicians India2004521141715656044
- IgarashiYChikamoriTTomiyamaHDiagnostic value of simultaneous brachial and ankle blood pressure measurements for the extent and severity of coronary artery disease as assessed by myocardial perfusion imagingCirc J2005692374215671620
- Iglesias del SolABotsMLGrobbeeDECarotid intimamedia thickness at different sites: relation to incident myocardial infarction; The Rotterdam StudyEur Heart J2002239161812069441
- JadhavUMKadamNNAssociation of microalbuminuria with carotid intima-media thickness and coronary artery disease – a cross sectional study in Western India20025011249
- JanssonJHNilssonTKJohnsonOvon Willebrand factor in plasma: a novel risk factor for recurrent myocardial infarction and deathBr Heart J19916635151747294
- KannamJPLevyDLarsonMShort stature and risk for mortality and cardiovascular disease events. The Framingham Heart StudyCirculation199490224177955180
- KannellWBWolfPAMcGeeDLSystolic blood pressure, arterial rigidity, and risk of strokeJAMA1981245122597206111
- KaramanogluMO'RourkeMFAvolioAPAn analysis of the relationship between central aortic and peripheral upper limb pressure waves in manEur Heart J19931416078449191
- KatayamaYShigeHYamamotoAOral vitamin C ameliorates smoking-induced arterial wall stiffness in healthy volunteersJ Atheroscler Thromb200411354715644590
- KlemsdalTOAnderssonTLMatzJVitamin E restores endothelium dependent vasodilatation in cholesterol fed rabbits: in vivo measurements by photophlesymographyCardiovasc Res199428139714027954652
- KollerASignaling pathways of mechanotransduction in arteriolar endothelium and smooth muscle cells in hypertensionMicrocirculation200292779412152104
- KuvinJTKarasRHClinical utility of endothelial function testing: ready for prime time?Circulation20031073243712835407
- LakattaEGSimilar myocardial effects of aging and hypertensionEur Heart J19911129381981552
- LatsonTWHunterWCKatohNEffect of nitroglycerin on aortic impedance, diameter, and pulse-wave velocityCirc Res198862884903129207
- LaurentSBoutouyriePArterial stiffness and stroke in hypertension; therapeutic implications for stroke preventionCNS Drugs20051911115651901
- LaurentSBoutouyriePAsmarRAortic stiffness is an independent predictor of all-cause mortality in hypertensive patientsHypertension20013712364111358934
- LefroyDCCrakeTUrenNGEffect of inhibition of NO synthesis on epicardial coronary artery caliber and coronary blood flow in humansCirculation19938843548319355
- LehmannEDRileyWAClarksonPNon-invasive assessment of cardiovascular disease in diabetes mellitusLancet1997350Suppl 1SI14199250278
- LevyDGarrisonRSavageDDPrognostic implications of echocardiographically determined left ventricular mass in the Framingham Heart StudyN Engl J Med1990332156162139921
- LiJJFangCHC-reactive protein is not only an inflammatory marker but also a direct cause of cardiovascular diseasesMed Hypotheses20046249950615050096
- LudmerPLSelwynAPShookTLParadoxical vasoconstriction induced by acetylcholine in atherosclerotic coronary arteriesN Engl J Med19863151046513093861
- LundFDigital pulse plethysmography (DPG) in studies of the hemodynamic responses to nitrates – a survey of recording methods and principles of analysisActa Pharmacol Toxicol (Copenh)198659Suppl 679963538782
- MaciochJEKatsamakisCDRobinJEffect of contrast enhancement on measurement of carotid artery intimal medial thicknessVasc Med2004971215230482
- MacMahonSPetoRCutlerJBlood pressure, stroke and coronary heart disease. Part 1, prolonged differences in blood pressure: prospective observational studies corrected for regression dilution biasLancet1990335765741969518
- MannucciPMvon Willebrand factor: a marker of endothelial damage?Arteriscler Thromb Vasc Biol199818135962
- MartinRPLerakisSContrast for vascular imagingCardiol Clin2004223132015158942
- MaseriAL'AbbateABaroldiGCoronary vasospasm as a possible cause of myocardial infarction: a conclusion derived from the study of “preinfarction” anginaN Eng J Med197822912717
- MatsuoSMatsumotoTTakashimaHThe relationship between flow mediated brachial artery vasodilation and coronary vasomotor responses to bradykinin: comparison with those to acetylcholineJ Cardiovasc Pharmacol2004441647015243296
- McGrathBPLiangYLKotsopoulosDImpact of physical and physiological factors on arterial functionClin Exp Pharmacol Physiol2001281104711903326
- McNeillAMRosamondWDGirmanCJPrevalence of coronary heart disease and carotid arterial thickening in patients with the metabolic syndrome (The ARIC study)Am J Cardiol20049412495415541239
- McVeighGEBrennanGMJohnstonGDImpaired endothelium-dependent and independent vasodilatation in patients with type 2 (non-insulin dependent) diabetes mellitusDiabetologia19923577161511805
- McVeighGEBurnsDEFinkelsteinSMReduced vascular compliance as a marker for essential hypertensionAm J Hypertens19914245512043302
- MeaumeSBenetosAHenryOFAortic pulse wave velocity predicts cardiovascular mortality in subjects >70 yrs of ageArterioscler Thromb Vasc Biol20012120465011742883
- MillerJALeverAFBurkeVPulse pressure as a risk factor for cardiovascular events in the MRC Mild Hypertension TrialJ Hypertens19991710657210466460
- MillasseauSCStewartADPatelSJEvaluation of carotid-femoral pulse wave velocity: influence of timing algorithm and heart rateHypertension200545222615642772
- MillasseauSCKellyRPRitterJMDetermination of age-related increases in large artery stiffness by digital pulse contour analysisClin Sci (Lond)2002103371712241535
- MorikawaYCharacteristic pulse wave caused by organic nitratesNature196721384124961986
- MokelkeEADietzNJEckmanDMDiabetic dyslipidaemia and exercise affect coronary tone and differential regulation of conduit and microvessel K+ currentAm J Physiol Heart Circ Physiol2005288H12334115528227
- NicholsWWClinical measurement of arterial stiffness obtained from non-invasive pressure waveformsAm J Hypertens20051831015691610
- NicholsWWO'RourkeMFMcDonald's blood flow in arteries: theoretical, experimental and clinical principles1998LondonEdward Arnold
- NicholsWWO'RourkeMFMcDonald's blood flow in arteries: theoretical, experimental and clinical principles20055th EdLondonEdward Arnold
- NiliNZhangMStraussBHBiochemical analysis of collagen and elastin synthesis in the balloon injured rat carotid arteryCardiovasc Pathol200211272612361837
- NitenbergAPaychaFLedouxSCoronary artery responses to physical stimuli are improved by deferoxamine but not by L-arginine in non-insulin-dependent diabetic patients with angiographically normal coronary arteries and no other risk factorsCirculation199897736439498536
- NorataGDTontiLRomaPApoptosis and proliferation of endothelial cells in early atherosclerotic lesions: possible role of oxidised LDLNutr Metab Cardiovasc Dis20021229730512616810
- OhshitaKYamaneKIshidaKPost-challenge hyperglycaemia is an independent risk factor for arterial stiffness in Japanese menDiab Med2004216369
- O'LearyDHPolakJFKronmalRACarotid-artery intima and media thickness as a risk factor for myocardial infarction and stroke in older adults. Cardiovascular Health Study Collaborative GroupN Eng J Med19993401422
- OliverJWebbDNoninvasive assessment of arterial stiffness and risk of atherosclerotic eventsArterioscler Thromb Vasc Biol2003235546612615661
- O'RourkeMFGallagherDEPulse wave analysisJ Hypertens199614Suppl 5147578728290
- O'RourkeMFKellyRPWave reflection in the systemic circulation and its implications in ventricular functionJ Hypertens199311327378390498
- O'RourkeMFPulsatile arterial haemodynamics in hypertensionAust N Z J Med19766S24081067826
- ParhamiFFangZTFogelmanAMMinimally modified low density lipoprotein-induced inflammatory responses in endothelial cells are mediated by cyclic adenosine monophosphateJ Clin Invest19939247188392092
- PaucaALWallenhauptSTKonNDDoes radial artery pressure accurately reflect aortic pressure?Chest1992102119381395767
- PearsonACGuoROrsinelliDATransesophageal echocardiographic assessment of the effects of age, gender, and hypertension on thoracic aortic wall size, thickness, and stiffnessAm Heart J1994128344518037102
- PhilippeFChemalyEBlacherJAortic pulse pressure and the extent of coronary artery disease in percutaneous transluminal coronary angioplasty candidatesAm J Hypertens200215672712160188
- RamseyMGoodfellowJJonesCEndothelial control of arterial distensibility is impaired in chronic heart failureCirculation1995923212197586306
- RidkerPMCannonCPMorrowDC-reactive protein levels and outcomes after statin therapyN Engl J Med200535273515635116
- RidkerPMHigh-sensitive C-reactive protein: potential adjunct for global risk assessment in the primary prevention of cardiovascular diseaseCirculation200210318131811282915
- RidkerPMStampferMJRifaiNNovel risk factors for systemic atherosclerosis; a comparison of C-reactive protein, fibrinogen, homocysteine, lipoprotein(a), and standard cholesterol screening as predictors of peripheral arterial diseaseJAMA20012852481511368701
- RossRThe pathogenesis of atherosclerosis: a perspective for the 1990sNature199336280198479518
- SalomaaVRileyWKarkJNon-insulin dependent diabetes mellitus and fasting glucose and insulin concentrations are associated with arterial stiffness indexes. The ARIC Study. Atherosclerosis Risk in Communities StudyCirculation1995911432437867184
- SalonenJTSalonenRUltrasound B-mode imaging in observational studies of atherosclerotic progressionCirculation199387II56658443925
- SchachingerVBrittenMBZeiherAMPrognostic impact of coronary vasodilator dysfunction on adverse long-term outcome of coronary heart diseaseCirculation20001011899190610779454
- Schini-KerthVBDual effects of insulin-like growth factor-I on the constitutive and inducible (NO) synthase-dependent formation of NO in vascular cellsJ Endocrinol Invest1999225 Suppl82810442576
- Schmidt-LuckeCRossigLFichtlschererSReduced number of circulating endothelial progenitor cells predicts future cardiovascular events: proof of concept for the clinical importance of endogenous vascular repairCirculation20051112981715927972
- SengstockDMVaitkeviciusPVSupianoMAArterial stiffness is related to insulin resistance in nondiabetic hypertensive older adults;J Clin Endocrinol Metab2005902823715728211
- SinghTPGroehnHKazmersAVascular function and carotid intimal-medial thickness in children with insulin-dependent diabetes mellitusJ Am Coll Cardiol200341661512598080
- SilvaGVLitovskySAssadJAMesenchymal stem cells differentiate into an endothelial phenotype, enhance vascular density, and improve heart function in a canine chronic ischaemia modelCirculation2005111150615642764
- SmithAKarallieddeJDe AngelisLAortic pulse wave velocity and albuminuria in patients with type 2 diabetesJ Am Soc Nephrol20051610697515743996
- SmithJCEvansLMWilkinsonIEffects of GH replacement on endothelial function and large-artery stiffness in GH-deficient adults: a randomized, double-blind, placebo-controlled studyClin Endocrinol (Oxf)20025649350111966742
- SmithJCLaneHALewisJEndothelial function and coagulant factors in growth hormone-treated hypopituitary adults receiving desmopressinJ Clin Endocrinol Metab2003882152612727969
- SuhHSParkYWKangJHVascular endothelial dysfunction tested by blunted response to endothelium-dependent vasodilation by salbutamol and its related factors in uncomplicated pre-menopausal obese womenInt J Obes (Lond)2005292172215570314
- Sutton-TyrrellKNajjarSSBoudreeauRMElevated aortic pulse wave velocity, a marker of arterial stiffness, predicts cardiovascular events in well-functioning older adultsCirculation200511133849015967850
- SzmitkoPEWangCHWeiselRDNew markers of inflammation and endothelial cell activationCirculation200310819172314568885
- TakazawaKTanakaNFujitaMAssessment of vasoactive agents and vascular ageing by the second derivative of photophlesysmograph waveformHypertension199832365709719069
- ter AvestEHolewijnSStalenhoefAFVariation in non-invasive measurements of vascular function in healthy volunteers during daytimeClin Sci20051084253115636580
- ThomasGNChookPOiaoMDeleterious impact of “high normal” glucose levels and other metabolic syndrome components on arterial endothelial function and intima-media thickness in apparently healthy Chinese subjects: the CATHAY studyArteriscler Thromb Vasc Biol20042473943
- ThompsonSGKienastJPykeSDHemostatic factors and the risk of myocardial infarction or sudden death in patients with angina pectoris. European Concerted Action on Thrombosis and Disabilities Angina Pectoris Study GroupN Eng J Med199533263541
- TioRAMonninkSHAmorosoGSafety evaluation of routine intracoronary acetylcholine infusion in patients undergoing a first diagnostic coronary angiogramJ Investig Med2002501339
- TreasureCBKleinJLWeintraubWSBeneficial effects of cholesterol-lowering therapy on the coronary endothelium in patients with coronary artery diseaseN Engl J Med199533248177830728
- TsimikasSBergmarkCBeyerRWTemporal increases in plasma markers of oxidized low-density lipoprotein strongly reflect the presence of acute coronary syndromesJ Am Coll Cardiol2003413607012575961
- TsimikasSWitztumJMeasuring circulating oxidized LDL to evaluate coronary riskCirculation20011031930211306518
- TsuchiyaMSuzukiEEgawaKStiffness and impaired blood flow in lower-leg arteries are associated with severity of coronary artery calcification among asymptomatic type 2 diabetic patientsDiabetes Care20042724091515451909
- VaneJRAnggardEEBottingRMRegulatory functions of the vascular endotheliumN Engl J Med199032327362113184
- VanhouttePMEndothelium and control of vascular functionHypertension198913658672661425
- VasaMFichtlschererSAicherANumber and migratory activity of circulating endothelial progenitor cells inversely correlate with risk factors for coronary artery diseaseCirc Res200189E1711440984
- VermaSWangCHLonnECross-sectional evaluation of brachial artery blood flow-mediated dilatation and C-rective protein in healthy individualsEur Heart J20042517546015451155
- VermaSWangCHLiSHA self-fulfilling prophecy: C-reactive protein attenuates nitric oxide production and inhibits angiogenesisCirculation20021069131912186793
- VermaSLiSHBadiwalaMVEndothelin antagonism and interleukin-6 inhibition attenuate the pro-atherogenic effects of C-reactive proteinCirculation20021051890611997273
- VitaJAKeaneyJFJrLarsonMGBrachial artery vasodilator function and systemic inflammation in the Framingham Offspring StudyCirculation20041103604915569842
- VogelRACorrettiMCEstrogens, progestins, and heart disease: can endothelial function divine the benefit?Circulation199897122369570189
- WahlqvistMLoCMyersKPutative determinants of arterial wall compliance in NIDDMDiabetes Care198811787903073068
- WatsonADLeitingerNNavabMStructural identification by mass spectrometry of oxidized phospholipids in minimally oxidized low density lipoprotein that induce monocyte/endothelial interactions and evidence for their presence in vivoJ Biol Chem199723135976079153208
- WangCHLiSHWeiselRDC-reactive protein upregulates angiotensin type 1 receptors in vascular smooth muscleCirculation200310717839012665485
- WendelhagIWiklundOWikstrandJArterial wall thickness in familial hypercholesterolemia. Ultrasound measurement of intimamedia thickness in the common carotid arteryArterioscler Thromb1992127071731860
- WidlanskyMEGokceNKeaneyJFJrThe clinical implications of endothelial dysfunctionJ Am Coll Cardiol20034211496014522472
- WilhelmsenLSvardsuddKKorsan-BengtsenKFibrinogen as a risk factor for stroke and myocardial infarctionN Engl J Med198431150156749207
- WilliamsILWheatcroftSBShahAMObesity, atherosclerosis and the vascular endothelium: mechanisms of reduced nitric oxide bioavailability in obese individualsInt J Obes Relat Metab Disord2002267546412037644
- WilliamsSBCuscoJARoddyMAImpaired nitric oxide-mediated vasodilatation in patients with non-insulin dependent diabetes mellitusJ Am Coll Cardiol199627567738606266
- WilkinsonIBHallIRMcCallumHPulse wave analysis: clinical evaluation of a non-invasive, widely applicable method for assessing endothelial functionArterioscler Thromb Vasc Biol2002221475211788475
- WilkinsonIBMacCallumHFlintLThe influence of heart rate on augmentation index and central arterial pressure in humansJ Physiol20005252638010811742
- WilkinsonIBMcEnieryCMArterial stiffness, endothelial function and novel pharmacological approachesClin Exp Pharmacol Physiol200431795915566396
- WilkinsonIBMohammadNHTyrrellSHeart rate dependency of pulse pressure amplification and arterial stiffnessAm J Hypertens200215243011824855
- WilkinsonIBPrasadKHallIRIncreased central pulse pressure and augmentation index in subjects with hypercholesterolemiaJ Am Coll Cardiol20023910051111897443
- WilsonAMO'NealDNelsonCLComparison of arterial assessments in low and high vascular disease risk groupsAm J Hypertens2004172859115062880
- YeungACVekshteinVIKrantzDSThe effect of atherosclerosis on the vasomotor response of coronary arteries to mental stressN Engl J Med1991325155161944439
- YildizAOflazHPusurogluHLeft ventricular hypertrophy and endothelial dysfunction in chronic hemodialysis patientsAm J Kidney Dis2003416162312612985
- ZeiherAMDrexlerHWollschlagerHModulation of coronary vasomotor tone in humans: progressive endothelial dysfunction with different early stages of coronary atherosclerosisCirculation1991833914011991363