Abstract
Hypertension is the most important cardiovascular risk factor for stroke. Blood pressure reduction by antihypertensive treatment is clearly efficacious in the prevention of stroke (both primary and secondary), although no clear differences have yet been observed between antihypertensive drug classes. However, a recent study reported the clear superiority of the angiotensin-receptor blocker eprosartan over the calcium channel blocker nitrendipine in cardiovascular protection of hypertensive patients with a previous stroke. Comparative studies using angiotensin-receptor blockers have also suggested the superiority of this class of drugs on primary stroke prevention. This effect may be linked to their beneficial actions on left ventricular hypertrophy, atrial enlargement, and supraventricular arrhythmias, endothelial dysfunction, inflammation, and remodelling, as well as a direct neuroprotective effect mediated through the stimulation of the angiotensin II type-2 receptor. In addition, a sympathoinhibition observed with the renin–angiotensin system blockers and particularly demonstrated with eprosartan, may help to explain the better cardiovascular and cerebrovascular protection in comparison with the calcium antagonist nitrendipine.
Introduction
Cardiovascular disease is the leading cause of death and disability in developed countries and arterial hypertension is one of the most powerful risk factors for developing such cardiovascular complications (CitationLewington 2002). The prevalence of hypertension is increasing and reaches more than 50% in people aged over 60 (CitationWolf-Maier et al 2003). The residual life-time risk for developing hypertension is higher than 90% (CitationVasan et al 2002).
The pathogenesis and pathophysiology of essential hypertension is complex and involves both genetic and environmental aspects. However, it has become clear that both the renin–angiotensin system (RAS) and the sympathetic nervous system (SNS) play important roles in the development and maintenance of elevated blood pressure (BP) values and in the pathogenesis of target organ damage. Bearing this pathogenetic complexity in mind, therapeutic approaches for hypertension and cardiovascular diseases include the use of various, very different drug classes, including diuretics, beta-blockers, calcium channel blockers, angiotensin-converting enzyme (ACE) inhibitors, and angiotensin-receptor blockers (ARB) (CitationChobanian et al 2003; CitationGC 2003).
Angiotensin-receptor blockers selectively antagonize the angiotensin II type 1 (AT1) receptor and counteract most of the deleterious actions of angiotensin II. Eprosartan is an ARB with a special chemical structure that may be relevant to its mechanism of action. The pharmacological properties and clinical efficacy and safety of eprosartan have been previously reviewed (CitationPlosker and Foster 2000; CitationRobins and Scott 2005).
In June 2005, an important study reported the superiority of eprosartan over the calcium channel blocker nitrendipine in cardiovascular protection of hypertensive patients with a previous stroke (CitationSchrader et al 2005). The present paper reviews the main findings of this trial and tries to answer some questions posed after its publication. The importance of stroke prevention by ARB in general and eprosartan in particular are also discussed.
The importance of stroke and the MOSES study
Stroke is the most frequent cardiovascular complication in hypertensive patients older than 60. A retrospective analysis of clinical trials in hypertensive patients published from 1991 to 2000 that included 59 550 randomized patients revealed that the total number of strokes (2533 events; 4.25%) clearly exceeded coronary events (1927 events; 3.24%) (CitationKjeldsen et al 2001). Blood pressure reduction and control is extremely important to prevent both stroke appearance (CitationCollins et al 1990; CitationStaessen et al 2000) and recurrence (PROGRESS 2000). Comparative trials and meta-analyses suggest that among different antihypertensive treatments, calcium channel blockers seem to represent the most powerful option for stroke prevention (CitationTurnbull 2003; CitationAngeli et al 2004).
No comparative trials between different antihypertensive drug classes were reported before the Morbidity and Mortality after Stroke, Eprosartan compared with Nitrendipine for Secondary Prevention (MOSES) study. The MOSES investigators hypothesized that for the same BP reduction, the ARB eprosartan would be superior to the calcium channel blocker nitrendipine in the cardiovascular protection of hypertensive patients with a previous stroke. Nitrendipine was chosen as a comparative drug on the basis of the cardiovascular and cerebrovascular protection observed in two trials of patients with isolated systolic hypertension (CitationStaessen et al 1997; CitationWang et al 2000) and, as mentioned above, due to the fact that calcium channel blockers seem to be more protective against stroke than other antihypertensive drug classes.
A total of 1405 patients with a previous cerebrovascular event (ischemic stroke, transitory ischemic attack, or cerebral hemorrhage) who were hypertensive (by both clinical measurements and ambulatory BP monitoring) were randomized to receive eprosartan 600 mg once daily or nitrendipine 10 mg once daily. Higher doses or combination therapy (excluding ARB and calcium channel blockers) were used in order to achieve a target BP lower than 140/90 mmHg. The primary endpoint was the composite of total mortality and all cardiovascular and cerebrovascular events, including all recurrent events.
The principal results of the MOSES trial revealed the superiority of eprosartan over nitrendipine in the primary endpoint (). There were 206 primary endpoints in the eprosartan group (incidence density per 100 person-years [ID] of 13.25) and 255 primary endpoints in the nitrendipine group (ID 16.71). The risk reduction for eprosartan was 21% with confidence limits of 4% to 34% (p = 0.014). Separate analysis of the different components of the primary endpoint also revealed a superiority of eprosartan over nitrendipine in the total number of cerebrovascular events, including recurrent events (relative risk reduction of 25% with confidence limits between 3% and 42%; p = 0.026) and, although nonsignificant, in the total number of cardiovascular events, including recurrent events (relative risk reduction of 25%; p = 0.061).
Figure 1 Effect of eprosartan compared with nitrendipine in various endpoints in the MOSES study.
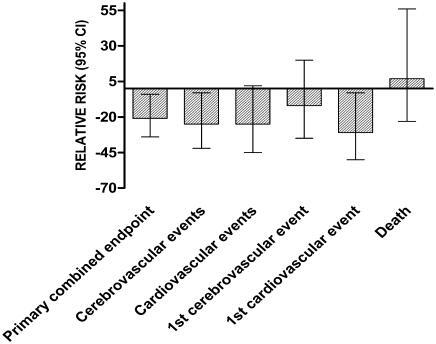
In addition to the analysis of the total number of events occurred, MOSES investigators also analyzed the first occurrence of events in each category. There were no significant differences between eprosartan and nitrendipine in the first-time occurrence of cerebrovascular events and death from any cause, but, once more, eprosartan was superior to nitrendipine in the prevention of the first cardiovascular event (risk reduction of 31% with confidence limits between 3% and 50%; p = 0.031). This better protection was essentially due to fewer myocardial infarctions and new cases of heart failure.
Reasons for better cardiovascular protection in hypertensive stroke patients
Evidence-based medicine has demonstrated a superior effect of eprosartan over nitrendipine on cardiovascular protection. This is proven, although the explanation remains speculative. Some of the reasons for this superiority may be linked to a theoretical class effect of ARB, which have demonstrated a good profile in both the primary prevention of stroke and their impact on several risk factors that are clearly implicated in stroke development and recurrence (CitationSierra and de la Sierra 2005). However, before exploring these reasons, the effects of differences in BP or a negative effect of nitrendipine, which might also have influenced the results, should be ruled out. The MOSES investigators reported that the effect of two treatment regimens on BP values were essentially the same, as were the number of patients reaching BP goals at both 3 months of treatment and at the end of follow-up. Moreover, the number of patients receiving combination therapy and the median number of drugs in each group were also the same.
With respect to a possible negative effect of nitrendipine on cerebrovascular protection in patients with a previous stroke, there are no reports on the effect of calcium channel blockers on secondary stroke prevention. However, as mentioned above, recent meta-analyses of comparative trials of antihypertensive agents found a superior effect of calcium channel blockers on primary stroke prevention (CitationTurnbull 2003; CitationAngeli et al 2004), while nitrendipine was the basis of active treatment in patients with isolated systolic hypertension demonstrating a clear benefit on stroke prevention (CitationStaessen et al 1997; Wang et al 2000). Thus, it would not be reasonable to suppose that a drug with a proven benefit on primary prevention would not have the same beneficial properties on secondary prevention of the same cardiovascular event.
The MOSES design was not able to completely rule-out a possible effect of the add-on therapy on the outcome. As this add-on therapy was left to the discretion of each investigator, the type of added medications was not identical between groups. In fact, although diuretics and beta-blockers were similarly distributed, more patients in the eprosartan group received other calcium channel blockers (14.4% versus 7.5% in the nitrendipine group) whereas ACE inhibitors were less frequently used (11.3% versus 21% in the nitrendipine group). Although it seems difficult to attribute to this imbalance an important role in the differences in cardiovascular protection observed in the MOSES trial, a contribution to the differences cannot be discarded.
ARB and stroke prevention
Three studies have compared ARB with other types of antihypertensive therapy in primary stroke prevention. The Losartan Intervention For Endpoint reduction (LIFE) study (CitationDahlöf et al 2002) compared losartan and atenolol in hypertensive patients older than 55 who had electrocardiographically detected left ventricular hypertrophy. Losartan significantly reduced the total number of cardiovascular events (13%) with minimal differences in BP changes between treatments. The benefit of losartan was mainly due to a decrease in the rate of stroke (25% reduction; p = 0.001).
The Study on Cognition and Prognosis in the Elderly (SCOPE) included hypertensive patients aged 70–89 who were randomly assigned to candesartan or placebo with open-label active antihypertensive treatment added as needed (CitationLithell et al 2003). The primary composite endpoint, a combination of cardiovascular death, stroke, and myocardial infarction was reduced by 10.9%, which did not reach statistical significance. Of all the components of the primary endpoint, only the reduction in non-fatal stroke (27.8%; 95% confidence interval [CI]: 1.3–47.2; p = 0.04) was statistically significant. However, there were marked differences in BP reduction (3.2/1.6 mmHg) between candesartan and placebo-treated patients.
Finally, the largest study with ARB in hypertensive patients was the Valsartan Antihypertensive Long-term Use Evaluation (VALUE) trial. The VALUE trial (CitationJulius et al 2004) compared two active antihypertensive treatments (valsartan and amlodipine) in high-risk hypertensives older than 50 years. At the end of the study there were no differences in the primary endpoint, which occurred in 10.6% of valsartantreated patients and in 10.4% of amlodipine-treated patients. Some of the prespecified secondary endpoints were favourable to amlodipine with respect to valsartan, including myocardial infarction and stroke, whereas valsartan slightly reduced the development of heart failure.
The VALUE trial showed important differences in the BP reduction achieved by the two treatment regimens. Blood pressure differences were especially apparent during the first part of the study (4/2.1 mmHg in the first month) and were maintained at more than 1mmHg in favour of amlodipine during the entire follow-up.
Therefore, two of the three above-mentioned trials of ARB in hypertensive patients suggested a protective effect of these drugs in the primary prevention of stroke. In fact, the cardiovascular protection observed in the LIFE trial was almost entirely due to stroke prevention. Moreover, although the primary-endpoint results of the SCOPE trial were not significant, the rate of non-fatal stroke was lower in the candesartan group. These results, combined with the MOSES results with eprosartan, suggest better cerebrovascular protection in hypertensive patients treated with ARB.
Another complementary evidence of a protective effect of ARB in cerebrovascular prevention comes from the Acute Candesartan Cilexetil Therapy in Stroke Survivors (ACCESS) study (CitationSchrader et al 2003). Hypertensive patients with an acute ischemic stroke were randomized to early candesartan or placebo, although all except two patients in the placebo group were then treated with candesartan 7 days after the stroke. Treatment was maintained during 12 months. The ACCESS trial demonstrated a beneficial effect of early candesartan on mortality (2.9% versus 7.2%; p = 0.07) and in the number of vascular events (9.8% versus 18.7%; p = 0.026), without significant differences in the level of BP between groups.
Possible mechanisms of cerebrovascular protection with ARB
Several different (and probably complementary) mechanisms have been proposed to explain the better cerebrovascular outcome in patients treated with ARB, including left ventricular hypertrophy regression, protection against atrial enlargement and supraventricular arrhythmias, effects on endothelial function, risk biomarkers and vascular remodelling, and a specific neuroprotection mediated through angiotensin II and the angiotensin II type 2 (AT2) receptor.
In the LIFE trial, the cardiovascular protection observed was related to left ventricular hypertrophy regression (CitationDevereux et al 2004; CitationOkin et al 2004). Patients in whom both the Cornell product and Sokolow-Lyon voltage, (the electrocardiographic criteria used to define left ventricular hypertrophy), were reduced exhibited lower rates of the primary composite endpoint (strokes, myocardial infarctions and cardiovascular deaths). This included between 10% and 20% reduction in stroke rates (CitationOkin et al 2004). Losartan-induced changes in these parameters were significantly more pronounced than those observed in atenolol-treated patients. These data have been confirmed in the substudy of LIFE in patients with left ventricular hypertrophy assessed by echocardiography. In this substudy, left ventricular mass regression was accompanied by a 24% risk reduction in the rate of stroke (CitationDevereux et al 2004). This effect on the regression of left ventricular hypertrophy can also be linked to better protection against atrial fibrillation. Supraventricular arrhythmias are frequent in hypertensive patients with diastolic dysfunction related to the increase in ventricular mass, which promotes atrial enlargement. It is recognized that atrial fibrillation is one of the main risk factors for stroke, especially when accompanied by hypertension, older age, or left ventricular dysfunction. A post-hoc analysis of the LIFE trial revealed that rates of new onset atrial fibrillation were significantly reduced in losartan-treated patients compared with those who received atenolol (CitationWachtell et al 2005). This suggests a specific effect of this class of drugs on myocardium that is not dependent on BP. Moreover, experimental data show that ARB can have a direct effect on atrial electrical remodelling (Nakashima et al 2000). Although differences in new onset atrial fibrillation in the LIFE trial were too small to account for stroke differences, these effects of ARB on left ventricular hypertrophy regression and probably a better protection against arrhythmias represent advantages in terms of general cardiovascular protection, including stroke.
Endothelial dysfunction is one of the most important mechanisms involved in the development of atherosclerosis and is present in patients with various cardiovascular risk factors, including hypertension, hypercholesterolemia, and type 2 diabetes, as well as in patients with coronary artery disease. Endothelial dysfunction has important prognostic implications in these groups of patients (CitationSchächinger et al 2000; CitationPerticone et al 2001). Blocking RAS with ARB clearly ameliorates endothelial dysfunction, an effect that is not totally dependent on BP reduction. In an elegant study (CitationSchiffrin et al 2000), resistance arteries obtained from gluteus subcutaneous biopsies from a small group of hypertensive patients and normotensive controls were studied by measuring the endothelium-dependent and independent responses and the cross-sectional area. Patients were then randomized to losartan or atenolol for one year and the procedures repeated. The results showed that patients treated with losartan normalized acetylcholine-dependent vasorelaxation and also reduced the ratio of the media/lumen diameter. No changes were observed in atenolol-treated patients despite a similar reduction in BP.
The effect of treatment on atherosclerosis biomarkers is closely linked to endothelial function. Several of these biomarkers, including acute-phase reactants such as C-reactive protein and adhesion molecules and selectins that mediate vascular inflammation, have been implicated in the prognosis of patients at risk or those with cardiovascular diseases, especially coronary artery disease (CitationBlankenberg et al 2001; CitationLibby et al 2002). Various studies have shown an improvement in these parameters by blocking the effects of angiotensin II. Two months of candesartan therapy promoted reductions in oxidative stress (malondialdehyde), inflammatory biomarkers (monocyte chemotactic protein, tumor necrosis factor-α), and thrombotic factors (plasminogen activator inhibitor type-1) in 45 hypertensive patients independently of BP changes (CitationKon et al 2003). Moreover, C-reactive protein, interleukin-6, and monocyte chemotactic protein-1 (MCP-1) were reduced in patients after olmesartan treatment (CitationFliser et al 2004), while, in the only comparative study of eprosartan against hydrochlorothiazide (CitationRahman et al 2002), decreases in MCP-1, soluble vascular cell adhesion molecule-1 (sVCAM-1), and superoxide anion generation were only observed in patients treated with eprosartan despite similar BP reductions.
There is growing experimental evidence suggesting that some actions directly related to the stimulation of the AT2 receptor may be involved in the cerebroprotection of ARB. Several angiotensin receptors mediate angiotensin II actions. Most of the deleterious effects of angiotensin II are mediated by the AT1 receptor, which is selectively blocked by ARB. Conversely, stimulation of the AT2 receptor by the same angiotensin II seems to promote vasodilation, natriuresis and apoptosis and impairs cellular hyperplasia (CitationFournier et al 2004). Some preliminary data support the idea that the AT2 receptor is expressed more intensively in the brain than in the heart and that this expression is enhanced in patients with target organ damage, especially when cerebral ischemia occurs (CitationDe Gasparo et al 2000). In experimental models, AT2 receptor stimulation protects brain tissue from ischemia (CitationLi et al 2005). Treatment with ARB would increase angiotensin II concentration (CitationStruck et al 2002), thus promoting the availability of this angiotensin II to bind the AT2 receptor and to mediate the previously-mentioned beneficial actions. Other forms of RAS blockade, such as treatment with ACE inhibitors, would decrease angiotensin II and thus would not share the beneficial effects mediated through AT2 receptor stimulation.
Eprosartan: an ARB with a dual mechanism of action
In addition to the RAS, the SNS seems to play an important role in the pathogenesis of essential hypertension, metabolic syndrome, and target organ damage related to elevated BP. Sympathoinhibitors, such as moxonidine, peripheral alpha-blockers, or beta-blockers have been widely used to treat high BP. In addition, it has been shown that blocking the RAS with ACE inhibitors or ARB decreases SNS activity in hypertensive and renal patients (CitationLigtenberg et al 1999; CitationStruck et al 2002; CitationKlein et al 2003). In fact, CitationStruck et al (2002) have demonstrated a clear inhibition of SNS by valsartan, but not nitrendipine. These results may help to explain the BP-independent cardiovascular protective effects of the ARB.
Angiotensin II type 1 receptors located postjunctionally in the vascular bed promote vasoconstriction, whereas those located prejunctionally increase norepinephrine outflow to the junctional area, thus contributing to further vasoconstriction. Studies in animal models have also shown that ARB suppress angiotensin II-induced sympathetic outflow, with differences in affinity for AT1 receptor sites evident between individual agents within this drug class (CitationOhlstein et al 1997; CitationBalt et al 2001; CitationGuimaraes et al 2001). The effect of eprosartan, candesartan, valsartan, and embusartan on presynaptically- and postsynaptically-located AT1 receptors was investigated in the pithed rat model. Whereas the effect on postsynaptic receptors was dose-dependent for all ARB, the sympathoinhibitory potency was clearly superior for eprosartan compared with the other ARB (CitationBalt et al 2001). Moreover, another study comparing eprosartan and losartan on both sympathoinhibitor and direct contractile responses in the canine pulmonary artery (CitationGuimaraes et al 2001) found a parallel effect of both eprosartan and losartan on direct contractile responses induced by angiotensin II, whereas at the prejunctional level, while eprosartan antagonized the facilitatory effect on noradrenaline release at the same doses that were effective postjunctionally, losartan was ineffective even at concentrations 10 times higher than those used to block the receptor postjunctionally.
These results have been recently confirmed in humans. In a comparative study against valsartan, eprosartan significantly reduced several hemodynamic parameters obtained after adrenergic and noradrenergic stress (CitationArosio et al 2005).
Effects of eprosartan on vasculature
Eprosartan is able to reduce several markers of vascular pathology in both experimental animal models and humans. In stroke-prone spontaneously hypertensive rats (SHR-SP) fed with a high-fat, high-salt diet, low doses of eprosartan (30 mg/Kg/day) induced a significant decrease in myocardial proinflammatory chemokine MCP-1 expression (CitationBehr et al 2004). This effect was accompanied by reduced morbidity and mortality. In a previous study by the same group, SHRSP treated with higher doses of eprosartan (60 mg/Kg/day) showed no mortality at 18 weeks, whereas all those treated with vehicle died by week 9 (CitationBarone et al 2001).
Studies performed in hypertensive patients have consistently shown a significant effect of eprosartan on several markers of vascular damage and dysfunction. In a non-comparative study of 30 hypertensive patients, eprosartan significantly reduced platelet activation and platelet calcium mobilization from baseline (CitationLabios et al 2004). In two comparative studies against losartan (CitationMakris et al 2004) or enalapril (CitationLeu et al 2004), eprosartan favourably influenced several markers of coagulation/fibrinolysis (reduction in plasminogen activator inhibitor-1 [PAI-1] and increase in tissue plasminogen activator [tPA] antigen), platelet activation, and endothelial function. These effects were comparable between eprosartan and enalapril, but superior to losartan. Finally, as mentioned above, in a comparative study against hydrochlorothiazide, eprosartan significantly reduced superoxide generation, MCP-1 and VCAM-1, despite a similar BP reduction (Rahman et al 2001).
Clinical profile of eprosartan
The clinical efficacy of eprosartan has been evaluated in randomized trials. Eprosartan has been compared with ACE inhibitors and other ARB (for reviews see CitationPlosker and Foster 2000; CitationRobins and Scott 2005). In patients with mild-tomoderate hypertension, eprosartan has been demonstrated to be equally effective compared with enalapril (CitationElliott 1999; CitationRuilope et al 2001). However, in a study that included patients with severe hypertension, eprosartan was significantly more effective than enalapril in reducing systolic BP (−29.1 versus −21.1; p < 0.05) (CitationSega 1999). Moreover, in comparative studies against losartan (CitationGarcia Puig et al 1999) or telmisartan (CitationDe Rosa et al 2004), no differences were observed in BP reduction.
Conclusion
The ARB eprosartan has been shown to be superior to the calcium channel blocker nitrendipine in preventing cardiovascular disease in hypertensive stroke patients. Angiotensin-receptor blockers are able to favourably affect left ventricular hypertrophy regression, endothelial function, and markers of vascular inflammation and remodelling, as well as exert beneficial actions on sympathetic nervous activity and on brain tissue through the stimulation of the AT2 receptor. All these actions help to explain the better outcome observed in the comparison between eprosartan and nitrendipine in hypertensive stroke patients.
Disclosure
Dr de la Sierra has received honoraria from Solvay Pharmaceuticals for speaker's presentations.
References
- AngeliFVerdecchiaPReboldiGPCalcium channel blockade to prevent stroke in hypertension: a meta-analysis of 13 studies with 103,793 subjectsAm J Hypertens2004178172215363825
- ArosioEDe MarchiSPriorMHaemodynamic effects of eprosartan and valsartan in hypertensive patients during isometric and mental stressJ Hypertens2005231923716148617
- BaltJMathyMJPfaffendorfMInhibition of facilitation of sympathetic neurotransmission and angiotensin II-induced pressor effects in the pithed rat: comparison between valsartan, candesartan, eprosartan and embusartanJ Hypertens20011922415011725169
- BaroneFCCoatneyRWChandraSEprosartan reduces cardiac hypertrophy, protects heart and kidney, and prevents early mortality in severely hypertensive stroke-prone ratsCardiovas Res20015052537
- BehrTMWilletteRNCoatneyRWEprosartan improves cardiac performance, reduces cardiac hypertrophy and mortality and downregulates myocardial monocyte chemoattractant protein-1 and inflammation in hypertensive heart diseaseJ Hypertens2004225839215076165
- BlankenbergSRupprechtHJBickelCCirculating cell adhesion molecules and death in patients with coronary artery diseaseCirculation200110413364211560847
- ChobanianAVBakrisGLBlackHRThe Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood PressureJAMA200328925607212748199
- CollinsRPetoRMacMahonSBlood pressure, stroke, and coronary heart disease. Part 2, short-term reductions in blood pressure: overview of randomised drug trials in their epidemiological contextLancet1990335827381969567
- DahlöfBDvereuxRBKjeldsenSECardiovascular morbidity and mortality in the Losartan Intervention For Endpoint reduction in hypertension study (LIFE): a randomised trial against atenololLancet2002359995100311937178
- De GasparoMCattKJInagamiTInternational Union of Pharmacology. XXIII. The angiotensin II receptorsPharmacol Rev2000524157210977869
- De RosaGRagonesiPDMugelliniAEffects of telmisartan compared with eprosartan on blood pressure control, glucose metabolism and lipid profile in hypertensive, type 2 diabetic patients: a randomized, double-blind, placebo-controlled 12-month studyHypertens Res2004274576415302981
- DevereuxRBWachtellKGerdtsEPrognostic significance of left ventricular mass change during treatment of hypertensionJAMA20042922350615547162
- ElliottWJDouble-blind comparison of eprosartan and enalapril on cough and blood pressure in unselected hypertensive patientsJ Human Hypertens1999134131710408592
- FliserDBuchholzKHallerHAntiinflammatory effects of angiotensin II subtype 1 receptor blockade in hypertensive patients with microinflammationCirculation20041101103715313950
- FournierAMesserliFHAchardJMCerebroprotection mediated by angiotensin II: a hypothesis supported by recent randomized clinical trialsJ Am Coll Cardiol2004431343715093864
- Garcia PuigJMateosFBuñoAEffect of eprosartan and losartan on Eric acid metabolism in patients with essential hypertensionJ Hypertens1999171033910419078
- [GC] Guidelines CommitteeEuropean Society of Hypertension-European Society of Cardiology guidelines for the management of arterial hypertensionJ Hypertens20032110115312777938
- GuimaraesSPinheiroHTavaresPDifferential effects of eprosartan and losartan at prejunctional angiotensin II receptorsNaunyn-Schmiedebergs Arch Pharmacol20013635091411383711
- JuliusSKjeldsenSEWeberMOutcomes in hypertensive patients at high cardiovascular risk treated with regimens based on valsartan or amlodipine: the VALUE randomised trialLancet200436320223115207952
- KjeldsenSEJuliusSHednerTStroke is more common than myocardial infarction in hypertension: analysis based on 11 major randomized intervention trialsBlood Pr2001101902
- KleinIHLigtenbergGOeyPLEnalapril and losartan reduce sympathetic hyperactivity in patients with chronic renal failureJ Asm Soc Nephrol20031442530
- KohKKAhnJYHanSHPleiotropic effects of angiotensin II receptor blocker in hypertensive patientsJ Am Coll Cardiol2003429051012957441
- LabiosMMartinezMGabrielFEffect of eprosartan on cytoplasmic free calcium mobilization, platelet activation, and microparticle formation in hypertensionAm J Hypertens2004177576315363816
- LeuHBCharngMJDingPYA double blind randomized trial to compare the effects of eprosartan and enalapril on blood pressure, platelets, and endothelium function in patients with essential hypertensionJpn Heart J2004456233515353873
- LewingtonSClarkeRQizilbashNProspective Studies CollaborationAge-specific relevance of usual blood pressure to vascular mortality: a meta-analysis of individual data for one million adults in 61 prospective studiesLancet200236019031312493255
- LiJCulmanJHortnaglHAngiotensin AT2 receptor protects against cerebral ischemia-induced neuronal injuryFASEB J2005196171915665034
- LibbyPRidkerPMMaseriAInflammation and atherosclerosisCirculation200210511354311877368
- LigtenbergGBlankestijnPJOeyPLReduction of sympathetic hyperactivity by enalapril in patients with chronic renal failureN Engl J Med19993401321810219067
- LithellHHanssonLSkoogIThe Study on Cognition and Prognosis in the Elderly (SCOPE): principal results of a randomized double-blind intervention trialJ Hypertens2003218758812714861
- MakrisTKStavroulakisGPapadoppoulosDPEprosartan effect on fibrinolytic/hemostatic variables in arterial hypertension: a comparative study to losartanDrugs Exp Clin Res2004301253215366789
- NakashimaHKumagaiKUrataHAngiotensin II antagonist prevents electrical remodeling in atrial fibrillationCirculation10126121710840013
- OhlsteinEHBrooksDPFeuersteinGZInhibition of sympathetic outflow by the angiotensin II receptor antagonist, eprosartan, but not by losartan, valsartan or irbesartan: relationship to differences in prejunctional angiotensin II receptor blockadePharmacology199755244519399334
- OkinPMDevereuxRBJernSRegression of electrocardiographic left ventricular hypertrophy during antihypertensive treatment and the prediction of major cardiovascular eventsJAMA20042922343915547161
- PerticoneFCeravoloRPujiaAPrognostic significance of endothelial dysfunction in hypertensive patientsCirculation2001104191611447085
- PloskerGLFosterRHEprosartan: a review of its use in the management of hypertensionDrugs20006017720110929934
- [PROGRESS] PROGRESS Collaborative GroupRandomised trial of a perindopril-based blood-pressure-lowering regimen among 6105 individuals with previous stroke or transient ischaemic attackLancet200135810334111589932
- RahmanSTLautenWBKhanQAEffects of eprosartan versus hydrochlorothiazide on markers of vascular oxidation and inflammation and blood pressure (renin-angiotensin system antagonists, oxidation, and inflammation)Am J Cardiol2002896869011897210
- RobinsGWScottLJEprosartan. A review of its use in the management of hypertensionDrugs20056523557716266204
- RuilopeLMJagerBPrichardBEprosartan versus enalapril in elderly patients with hypertension: a double-blind randomized trialBlood Pr2001102239
- SchächingerVBrittenMZeiherAMPrognostic impact of coronary vasodilator dysfunction on adverse long-term outcome of coronary heart diseaseCirculation2000101189990610779454
- SchiffrinELParkJBIntenganHDCorrection of arterial structure and endothelial dysfunction in human essential hypertension by the angiotensin receptor antagonist losartanCirculation20001011653910758046
- SchraderJLüdersSKulchewskiAThe ACCESS study. Evaluation of acute candesartan cilexetil therapy in stroke survivorsStroke200334169970312817109
- SchraderJLüdersSKulschewskiAMorbidity and mortality after stroke, eprosartan compared with nitrendipine for secondary prevention. Principal results of a prospective randomized controlled study (MOSES)Stroke20053612182615879332
- SierraCde la SierraAAntihypertensive, cardiovascular, and pleiotropic effects of angiotensin-receptor blockersCurr Opin Nephrol Hypertens2005144354116046901
- SegaREfficacy and safety of eprosartan in severe hypertensionBlood Pr1999811421
- StaessenJAFagardRThijsLRandomised double-blind comparison of placebo and active treatment for older patients with isolated systolic hypertensionLancet1997350757649297994
- StaessenJAGasowskiJWangJGRisks of untreated and treated isolated systolic hypertension in the elderly: meta-analysis of outcome trialsLancet20003558657210752701
- StruckJMuckPTrübgerDEffects of selective angiotensin II receptor blockade on sympathetic nerve activity in primary hypertensive subjectsJ Hypertens2002201143912023684
- TurnbullFBlood Pressure Lowering Treatment Trialists' CollaborationEffects of different blood-pressure-lowering regimens on major cardiovascular events: results of prospectively-designed overviews of randomised trialsLancet200336215273514615107
- VasanRSBeiserASeshadriSResidual lifetime risk for developing hypertension in middle-aged women and men: The Framingham Heart StudyJAMA200228710031011866648
- WachtellKLehtoMGerdtsEAngiotensin II receptor blockade reduces new-onset atrial fibrillation and subsequent stroke compared to atenolol: the Losartan Intervention For End Point Reduction in Hypertension (LIFE) studyJ Am Coll Cardiol2005457121915734615
- WangJGStaessenJAGongLChinese trial on isolated systolic hypertension in the elderly. Systolic Hypertension in China (Syst-China) Collaborative GroupArch Intern Med1602112010647760
- Wolf-MaierKCooperRSBanegasJRHypertension prevalence and blood pressure levels in 6 European countries, Canada, and the United StatesJAMA20032892363912746359