Abstract
Objective
An ulcer categorized as Fontaine’s stage IV represents a chronic wound, risk factor of arteriosclerosis, and co-morbidities which disturb wound healing. Our objective was to analyze wound healing and to assess potential factors affecting the healing process.
Methods
199 patients were included in this 5-year study. The significance levels were determined by chi-squared and log-rank tests. The calculation of patency rate followed the Kaplan-Meier method.
Results
Mean age and co-morbidities did not differ from those in current epidemiological studies. Of the patients with ulcer latency of more than 13 weeks (up to one year), 40% required vascular surgery. Vascular surgery was not possible for 53 patients and they were treated conservatively. The amputation rate in the conservatively treated group was 37%, whereas in the revascularizated group it was only 16%. Ulcers in patients with revascularization healed in 92% of cases after 24 weeks. In contrast, we found a healing rate of only 40% in the conservatively treated group (p < 0.001). Revascularization appeared more often in diabetic patients (n = 110; p < 0.01) and the wound size and number of infections were elevated (p = 0.03). Among those treated conservatively, wound healing was decelerated (p = 0.01/0.02; χ2 test).
Conclusions
The success of revascularization, presence of diabetes mellitus, and wound treatment proved to be prognostic factors for wound healing in arterial ulcers.
Introduction
The underlying cause of arterial ulceration is arteriosclerosis obliterans resulting in tissue ischemia in 90% of cases. The ulcer itself is categorized as stage IV in the Fontaine classification system (Rutherford category 3 and 4). Only a few articles discuss the complex treatment of these wounds or show the influence of revascularization, wound management, and risk factor assessment. This study aimed to evaluate the factors involved in complex wound treatment.
Subjects and methods
Patients
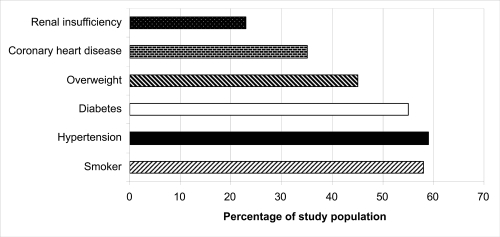
Over a 5-year period (1997–2001), 199 patients with stage IV peripheral arterial occlusive disease (PAOD) were studied. Inclusion criteria were length of hospital stay, course of therapy, outpatient monitoring, and wound assessment/treatment (inpatient and outpatient). Risk factors, co-morbidities, and the different treatment groups were also evaluated ().
Vascular status/vascular surgery therapy
Imaging procedures such as angiography or magnetic resonance angiography (in cases with renal insufficiency or contrast agent allergy) were used to ascertain an objective status of the vascular system. The decision to perform angioplasty/reconstruction was based on the Trans-Atlantic Inter-Society Consensus guidelines (CitationTrans Atlantic Inter-Society Consensus I 2000).
Wound assessment
To characterize the wound we assessed data on latency, localization, size, and type of wound. Localization fell into three categories: foot and toe, lower leg, foot and lower leg. A lattice grid was used to measure the wound size. A wound with a spread of less than 5 cm2, or with a single extension radiating from the wound, was classified as a “small wound”. A “medium-size wound” was 5–10 cm2, or with 2–4 toes involved. The category of “large wound” included those with a spread beyond 10 cm2, and those with the involvement of the entire forefoot. The depth was categorized using the Knighton classification (CitationKnighton et al 1986). Ulceration was defined as tissue damage which could clinically be described as necrosis or gangrene.
The diagnosis of neuropathy resulted from the known factors (CitationMorbach et al 2004; CitationLobmann 2005).
Wound treatment
Wounds were treated according to Vollmar’s IRA principle (treatment of infection, revascularization and minor amputation in the necrobiotic wound margin; CitationVollmar 1996). Necrosis (ie, of the toes) was not removed or debrided before revascularization. A gangrenous or phlegm-filled status required surgical intervention to control wound infection (eg, incision, drainage, toe amputation) with accompanying antibiotic treatment and local application of antiseptics (CitationKramer et al 1998; CitationSchmidt et al 2000). The general wound treatment followed the revised TIME principles of wound bed preparation (CitationBendow et al 1999; CitationSchultz et al 2003) and did not differ from current recommendations (CitationHopf et al 2006). Ulcer healing, and wound borderline amputation that healed well, were considered successful outcomes.
Statistical analysis
The chi-squared and log-rank tests were used to establish the statistical significance of the determinant factors. The patency rate was calculated according to the Kaplan-Meier method. All statistical tests were performed with SPSS 11.0 for Windows (Chicago, IL, USA).
Results
Patient characteristics
The average age of the 132 men (66%) and 67 women (34%) was 65.4 years. Thirty-two percent of the patients were younger than 60 years. Diabetic patients were significantly older than nondiabetic patients with PAOD (p = 0.03; χ2 test). Nicotine abuse was found among 72% of men and among 26% of women. Using the Body Mass Index (BMI) calculation we found that 90 patients (45%) were overweight (BMI: 25–30) or obese (BMI: >31). Arterial hypertension was seen in 77% of the women and 49% of the men; of these groups 84% and 60% were overweight, respectively. There were 110 patients (55%) with diabetes mellitus. This patient group had a greater number of previous revascularization treatments on the extremities (p < 0.01; χ2 test) than nondiabetic patients. Women more often showed the risk factor combination of arterial hypertension, diabetes mellitus, and obesity (p = 0.02; χ2 test). There were 46 patients (23%) with chronic renal insufficiency (27 needed dialysis). Of all risk factors, only diabetes mellitus showed a correlation with poor wound healing ().
Ulcer characteristics and treatment
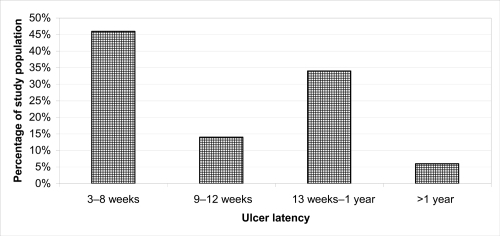
We found angiopathic ulcers in 89 (45%) patients without diabetes mellitus, whereas among the diabetic patients, we found angiopathic or angiopathic-neuropathic ulcers in 110 (55%). Diabetic patients presented significantly larger wounds (p = 0.03; χ2 test) and there was a higher occurrence of phlegmonous infection (p = 0.03; χ2 test). Wound localization and necrotic status or gangrene did not differ significantly between the two groups (PAOD patients with/without diabetes mellitus) (). After ulcer duration of more than 13 weeks, 40% of the patients were presented for vascular surgery (). Pre- and post-operative antibiotic therapy was administered to 67% of the patients because of signs of local or systemic infection (germ spectrum: 40% Staphylococcus [3% MRSA], 24% Enterococcus, 20% Enterobacter, 10% Pseudomonas, and 6% other). Local antiseptics were applied in 58% of the cases. Sixty-seven percent of the ulcers were surgically debrided. If a patient did not have the option of revascularization, or had a small superficial ulcer, a conservative debridement was performed. During the hospitalization, 33% received modern occlusion bandaging, and in 10% a biological covering of the wound (mesh graft, n = 14; plastic flap, n = 5) was applied. In 37% of the cases minor amputation (toe amputation) was performed after revascularization. An inactive dressing was placed on the necrotic tissue until a necrobiotic borderline had developed.
Table 1 Wound characterization (n = 199)
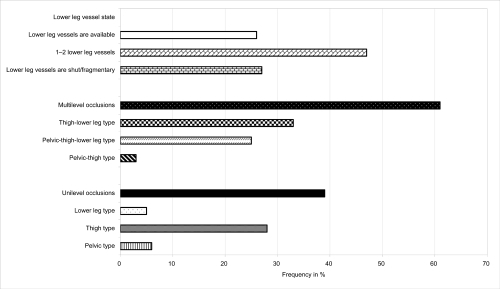
Vascular situation/treatment
Twenty-three percent of the cases had undergone previous vascular surgery on the affected extremity (10% on the contralateral extremity). Major amputation was required in 2% of the ipsilateral (lower leg) and 4% of the contralateral (lower leg and upper leg) cases.
Sixty-one percent of the patients had a multilevel occlusive disease; the thigh-lower leg occlusion type was predominant (). The mean ABI (ankle/brachial index) improved by 0.37 to 0.90 (excluding 20% of the diabetic patients, who could not be analyzed). In 53 patients (27%), the lower leg arteries were either partially or completely closed up. Whenever vascular re-connection was not possible, a conservative treatment was performed (prostaglandin infusion, acetylsalicylic acid, heparin, and pain treatment). The rate of amputation was 37% in this conservatively treated group. Vascular surgery was performed on 146 (73%) of the patients. A total of 178 surgical interventions was necessary, ie, angioplasty and bypass/endarterectomy, endarterectomy and bypass, thrombolysis. Because of the relatively small number of cases, and the variation in surgical procedures and vascular status, the patency rate is not meaningful for evaluating the outcome of treatment (CitationLeng et al 2000). A saphenous vein bypass, as opposed to a prosthetic bypass, was more advantageous in the upper as well as in the lower leg (p = 0.01; log-rank test). In the revascularized group the amputation rate was only 16% (n = 24).
Outcome
The average hospital stay was 22 days (range: 12–29 days). The time delay until the vascular operation was determined by the status of the infection and time needed for assessment and treatment of the polymorbidities (median: 5 days; range: 1–10 days). To assess wound treatment we monitored 150 wounds (117 patients of the revascularized group and 33 patients of the conservatively treated group). The amputated (n = 43) and the patients who died during their first hospital stay (n = 6) were not included in the analysis.
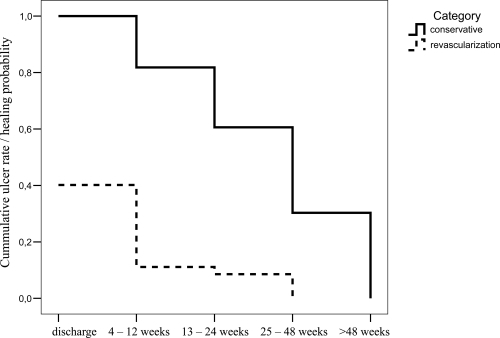
During our 5-year follow up, 22 patients (11%) died. At the time of discharge, a total of 47% (n = 70) of the 150 wounds had healed. Within 24 weeks, 92% of ulcers in the revascularizated group healed, whereas only 40% in the conservatively treated group showed complete wound healing at this time point ().
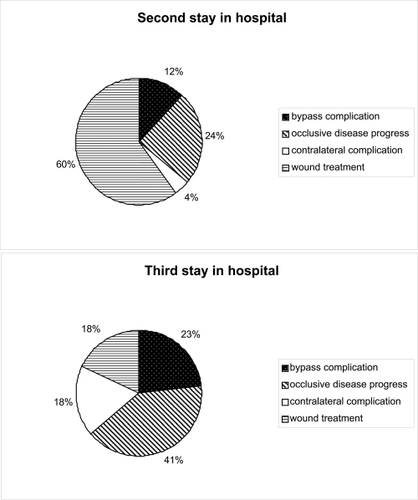
Diabetic patients, and patients treated conservatively, needed an extended healing time (p = 0.01/0.001; χ2 test). A second hospital stay was necessary for 67 patients and in 60% the wound treatment was responsible for hospitalization (ie, borderline amputation/minor amputation, debridement). Major reasons for a third hospital stay (n = 17) were progress of arteriosclerosis or bypass complications (). In 78% (of all patients) the leg could be preserved.
Discussion
General epidemiological data for Germany confirm that 2.5 million patients have PAOD, and 800,000 of these have clinically significant symptoms. Of the stage III and IV patients, 25% suffer a substantial disease progression during the time of treatment. The vascular component is the leading reason for 20,000 major amputations per year in Germany (CitationSpengel 2001; CitationgetABI Study Group 2002; CitationCetin and Baumgartner 2004; CitationEckstein and Knipfer 2007).
In this study, the risk factors of PAOD are similar to those shown in published data (CitationTreiman et al 2000; CitationgetABI Study Group 2002; CitationShammas 2007). In diabetic patients we found more severe infections, greater wound size, and longer healing times. The high prevalence of ischemia, infection, and serious co-morbidity in diabetic foot syndrome was confirmed in the Eurodiale study (CitationPrompers et al 2007).The extrinsic and intrinsic factors leading to decreased healing capacity in diabetic patients were determined (CitationLobmann 2005). PAOD is not an independent condition in diabetic patients (CitationMorbach et al 2004; Scherbaum et al 2004). The high rate (22%) of younger patients (<60 years) who were developing arterial ulcers highlights the demographic changes compared with previous data, and therefore the need for new strategies of prevention.
The long latency period until the patient can be seen in a specialized center for vascular surgery indicates deficiencies in outpatient care and underlines the need to apply the established guidelines (CitationBendow et al 1999; CitationSpengel 2001; CitationHopf et al 2006). Other possible risk factors were not evident in our study (CitationTreiman et al 2000; CitationMarston et al 2006; CitationInce et al 2007). A timely evaluation and treatment can reduce the mortality of this disease (11%–30% of patients in 3–5 years in the literature) (CitationgetABI Study Group 2002; Cetin and Baumgartner 2002).
Whether the lower mortality of the presented group (11%) depended on this specialized treatment in a university hospital setting, is speculative and was not further analyzed. The cause of death of admitted patients was of cardiovascular origin.
According to statistical data, 25% of patients suffering from PAOD stage IV (Fontaine) receive a medication therapy, 25% undergo a primary amputation, and in 50% a revascularization is possible (CitationTrans Atlantic Inter-Society Consensus I: TASC I, 2000; CitationSpengel 2001).
According to the TASC II, critical limb ischemia within one year is associated with an amputation rate of 30% and a mortality of 25% (Norgren et al 2007). In our 5-year study, the total amputation rate over all patients was 22%. However 37% of patients were receiving conservative treatment, and only 16% of the revascularized patients, were affected.
CitationMarston and colleagues (2006) reported an amputation rate of 23% over a 12-month period with similar parameters, and in 52% of these patients complete wound healing was achieved within one year. As a factor of influence the size of the wound was stated; even in our own study, only small wounds healed completely in the conservatively treated group. The effectiveness of prostanoid therapy is a controversial international topic (CitationSpengel 2001; CitationHopf et al 2006; CitationMinar and Schillinger 2007; Norgren et al 2007). The time needed for healing of the ulcers under study was less than reported in current literature, depending on the criteria for patient inclusion. Ince et al reported an 86% rate for 52 weeks (CitationInce et al 2007) and CitationHumphreys and colleagues (2007) reported a rate of 87% of complete healing of ulcers without PAOD, 68% with minimal PAOD, and 53% with severe PAOD. All revascularized ulcers healed within 36 weeks. CitationChung and colleagues (2006) reported a healing rate of 75% within 12 months. CitationTreiman and colleagues (2000) showed comparable healing rates of 73% within 24 weeks and a leg conservation rate of 86% over 3 years. For all authors the positive outcome of revascularization was the key parameter for success. Our own study however also shows that an extended primary hospital stay for wound treatment, followed by several consequent hospital stays for wound care (including minor and forefoot amputations, debridement), played an important role. Studies on modern treatment of arterial ulcer wounds, which include recommendations of a wound covering, are not available (CitationBendow et al 1999; CitationTautenhahn and Piatek 2006; CitationNelson and Bradley 2007). The principle of wound bed preparation is none the less valid for all chronic wounds. It takes into account the status of the infection, the treatment of gangrene before revascularization of the arterial ulcers, as well as subsequent wound therapy (CitationBendow et al 1999; CitationSchmidt et al 2000; CitationSchultz et al 2003; CitationHopf et al 2006; CitationTautenhahn and Piatek 2006).
Revascularization, diabetes mellitus, and wound therapy prove to be prognostic factors for the pace and efficiency of arterial ulcer wound healing. Further factors and other co-morbidities did not appear to have an influence, even in a large patient study group. In agreement with current literature the progress of arteriosclerosis, which is also the underlying cause of the ulcer, contributes to the higher mortality of this group of patients.
References
- BendowMBurgGCamacho MartinezFGuidelines for the outpatient treatment of chronic wounds and burns1999Berlin WienBlackwell
- CetinCBaumgartnerIDie periphere arterielle VerschlusskrankheitSchweiz Med Forum2004421623
- ChungJBartelsonBBHiattWRWound healing and functional outcomes after infrainguinal bypass with reversed saphenous vein for critical limb ischemiaJ Vasc Surg20064311839016765235
- EcksteinHHKnipferECurrent status of vascular surgery. In vascular medicine and general surgeryChirurg20077858292
- getABI Study GroupGerman epidemiological trial on ankle brachial index for elderly patients in family practice to detect peripheral arterial disease, significant marker for high mortalityVasa200231241812510548
- HopfHWUenoCAslamRGuidelines for the treatment of arterial insufficiency ulcersWound Rep Reg200614693710
- HumphreysMLStewartAHGohelMSManagement of mixed arterial and venouse leg ulcersBr J Surg200711 Epub ahead of print
- IncePGameFLJeffcoateWJRate of healing of neuropathic ulcers of the foot in diabetes and its relationship to ulcer duration and ulcer areaDiabetes Care2007a36603
- KnightonDRFiegelVDAustinLLClassification and treatment of chronic nonhealing wounds. Succsessful treatment with autologous platelet-derived wound healing factorsAnn Surg198620432293753059
- KramerAVAdrianPRudolphSExplantationstest mit Haut und Peritoneum der neonatalen Ratte als Voraussagetest zur Verträglichkeit lokaler Antiinfektiva für Wunden und KörperhöhlenChirurg19986984059782400
- LengGCDavisMBakerDBypass surgery for lower limb ischemiaCochrane Database Syst Rev20003CD00200010908520
- LobmannRLobmannREckardtAPathogenese, Epidemiologie und Klassifikation des diabetischen FußsyndromesDer diabetische Fuß – Interdisziplinäre Diagnostik und Therapie2005Berlin New YorkSpringer111
- MarstonWADaviesSWArmstrongBNatural history of limbs with arterial insufficiency and chronic ulceration treated without revascularistionJ Vasc Surg2006441081416828434
- MinarESchillingerMTASC II – Kommentar aus Sicht des AngiologenZ Gefässmed200741417
- MorbachSMüllerEReikeHDiagnostik, Therapie, Verlaufskontrolle und Prävention des diabetischen FußsyndromsDiabetes und Stoffwechsel200413930
- NelsonEABradleyMDDressings and topical agents for arterial leg ulcersThe Cochrane Database Syst Rev20073CD002000
- PrompersLHuijbertMApelqvistJHigh prevalence of ischaemia infection and serious comorbidity in patients with diabetic foot disease in Europe. Baseline results from the Eurodiale studyDiabetolgia2007501825
- SchmidtKDebusESJessbergerSBacterial population of chronic crural ulcers: is there a difference between the diabetic the venous and the arterial ulcer?Vasa200029627010731891
- SchultzGSSibbaldRGFalangaVWound bed preparation: a systematic approach to wound managementWound Rep Reg200311123
- ShammasNWEpidemiology, classification, and modifiable risk factors of peripheral arterial diseaseVasc Health Risk Manag200732293417580733
- SpengelFALeitlinen zur Diagnostik und Therapie der arteriellen Verschlusskrankheit der Becken-Beinarterien - Deutsche Gesellschaft für Angiologie und GefäßmedizinVasa20013031911284088
- TautenhahnJPiatekSLippertHArterielle UlzerationenWundatlass2006Stuttgart New YorkThieme21320
- Trans Atlantic Inter-Society Consensus (TASC I)Management of peripheral Arterial DiseaseEur J Vasc Endovasc Surg200019125010706826
- TreimanGSOderichGSAshrafiAManagement of ischemic heel ulceration and gangrene: An evaluation of factors associated with successful healingJ Vasc Surg20003111101810842147
- VollmarJRekonstruktive Chirurgie der Arterien1996Stuttgart New YorkThieme