Abstract
Childhood obesity has reached epidemic proportions in many countries. Pediatric obesity is associated with the development of cardiovascular (CV) risk factors including type 2 diabetes, hypertension, dyslipidemia, and the metabolic syndrome. It is also associated with an increased risk of CV disease (CVD) in adulthood. Moreover, obesity and CVD risk factors in obese youth tend to track into adulthood, further increasing the risk of adult CVD. Consequently, the treatment and prevention of childhood overweight and obesity has become a public health priority. Proper nutrition and increased physical activity are the main focus of these efforts; however, few studies have shown positive results. Treatment options for obesity in youth also include pharmacotherapy and surgery. While pharmacotherapy appears promising, additional evidence is needed, especially with respect to the long-term impact, before it becomes a widespread treatment option in the pediatric population.
Introduction
In the past three decades the prevalence of overweight and obesity among youth in North America has doubled and tripled, respectively (CitationOgden et al 2002; CitationTjepkema and Shields 2004). Childhood obesity is important from a public health perspective for many reasons. First and foremost, obesity during childhood and adolescence is associated with a number of cardiovascular disease (CVD) risk factors. Some of these risk factors include type 2 diabetes mellitus (T2DM), hypertension, and dyslipidemia. Second, obesity and many of the associated CVD risk factors have a strong tendency to persist into adulthood. Thus, obesity during childhood and adolescence increases adult risk of CVD. Accordingly, a considerable amount of research resources have been devoted to this topic in recent years. This review will discuss the prevalence of childhood and adolescent overweight and obesity, the way in which obesity is classified, and the cardiovascular (CV) health risks associated with it. This review will also speak to current prevention and treatment options for obesity in youth, including the effects weight loss may have on vascular health.
Prevalence of overweight and obesity
Since the 1970s, countries around the world, developed and developing alike, have experienced an increase in the prevalence of overweight and obesity among children and adolescents (CitationChinn and Rona 2001; CitationStrauss and Pollack 2001; CitationTremblay et al 2002; CitationLissau et al 2004). For instance, in the US the prevalence of adolescent (12 to 19 years old) obesity increased from 5% in 1976–1980 to 15% at the turn of the century (CitationOgden et al 2002). Similarly, the prevalence of obesity in Canadian youth (12 to 17 years old) has increased almost 3-fold from 3% in the late 1970's to 8% in 2004 (CitationTjepkema and Shields 2004).
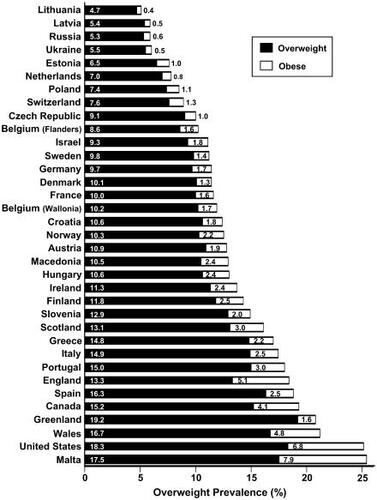
A recent study (2001 to 2002) measured the prevalence of overweight and obesity in 10 to 16 year old children from 34 countries across North America and Europe using the international obesity classification system () (CitationJanssen et al 2005). One of the primary observations of that study is that the childhood obesity epidemic is a global issue: in 77% of the countries examined, at least 10% of youth were overweight and in 20% of the countries at least 3% were obese. A second key finding of that study is that there are regional differences in obesity. The prevalence of overweight and obese youth is particularly high in countries in North America, Great Britain, and southwestern European countries such as Greece, Italy, and Spain.
Figure 1 Ranking of 34 countries according to the prevalence of overweight youth in 2001–2002 using the international classification system. Adapted from Janssen I, Katzmarzyk PT, Boyce WF, et al. 2005. Comparison of overweight and obesity prevalence in school-aged youth from 34 countries and their relationships with physical activity and dietary patterns. Obes Rev, 6:123–32. Copyright © 2005.
Classification of overweight and obesity
The CV health problems associated with obesity are believed to be in large measure explained by the excess body fat in obese individuals. While body fat can be accurately measured using a number of techniques (eg, hydrodensitometry, dual energy X-ray absorptiometry), these methods are far too sophisticated, time consuming, and expensive to employ in the clinical setting (CitationEllis 2000). Instead, adiposity status is assessed in the clinical setting using simple and practical anthropometric measures such as the body mass index (BMI) and waist circumference. BMI describes relative height for weight and is calculated as weight (kg)/height squared (m2). Studies have shown that BMI is highly correlated to total body fat in children and adolescents (CitationRoche et al 1981; CitationDeurenberg et al 1991; CitationNeovius et al 2005). As in adults, waist circumference is a marker of both total and abdominal fat in children and adolescents (CitationRankinen et al 1999; CitationRodriguez et al 2004; CitationNeovius et al 2005). Compared with other anthropometric measures, waist circumference is the best overall indicator of abdominal visceral fat levels (CitationRankinen et al 1999). Abdominal visceral fat is arguably the most clinically relevant fat depot and is associated with metabolic complications such as hypertension, hyperinsulinemia, T2DM, and dyslipidemia in young people (CitationOwens et al 1998; CitationFreedman et al 1999; CitationGoran and Gower 1999). However, the quantity of visceral fat in children, even when considered as a percentage of total fat, is quite low in comparison with that of adults (CitationSeidell et al 1988).
BMI values of 25 kg/m2 and 30 kg/m2 are used almost universally to define overweight and obesity, respectively, in adult populations (CitationWHO 1997). Conversely, in children and adolescents, the determination of adiposity status is challenging as BMI and waist circumference change considerably with normal growth and maturation in addition to adiposity status (CitationGuo et al 1997; CitationFreedman et al 1999; CitationCole et al 2000). For example, CitationCole and colleagues (2000) have shown that the 50th percentile for BMI in British males changes from approximately 16 kg/m2 at 6 years of age to 21 kg/m2 at 18 years of age. Similarly, waist circumference values increase during the growing years and are higher in males than females (CitationKatzmarzyk 2004). Therefore, age- and gender-specific BMI and waist circumference thresholds are required to identify overweight and obese children and adolescents. Thresholds for overweight and obesity are often defined based on Caucasian populations. Caution must be used when applying such thresholds universally, as percentile thresholds vary with race and ethnicity (CitationDudeja et al 2001). Further, evidence in children and adolescents suggests that for a given BMI level, CVD risk factors are different amongst different racial and ethic groups (CitationSrinivasan et al 1987; CitationKlein et al 2004).
Body mass index
BMI is the most commonly used measure of adiposity status in children and adolescents and its use has been recommended by several expert committees (CitationHimes and Dietz 1994; CitationBarlow and Dietz 1998; CitationBellizzi and Dietz 1999). Two approaches can be used to classify adiposity status in children and adolescents based on BMI. The most common method is to use the distributional approach. With this approach the 85th and 95th age- and gender-specific percentiles are used to identify children as overweight and obese, respectively (Note: some classification systems use the terms “at-risk for overweight” and “overweight” in place of “overweight” and “obese”). Many countries have developed BMI-for-age growth charts for these percentiles using representative samples of their populations (CitationCole et al 1998; CitationLeung et al 1998; CitationCole and Roede 1999; CitationMust and Strauss 1999; CitationFredriks et al 2000; CitationKuczmarski et al 2002). In the US, the Centers for Disease Control and Prevention (CDC) have developed BMI growth charts using data from several representative surveys collected from 1963 to 1994 (CitationKuczmarski et al 2002). It should be noted that ethnic minority groups were over-sampled in these surveys. In addition, the BMI growth curves for children and adolescents were primarily developed using BMI values from older surveys (1963–1980) to account for the recent population trends in BMI. The CDC growth charts (http://www.cdc.gov/growthcharts/) are now widely employed in clinical practice in the US and Canada.
The second approach commonly used to identify overweight and obese children and adolescents is the method of CitationCole and colleagues (2000). The development of these BMI thresholds was endorsed by an expert committee convened by the International Obesity Task Force (IOTF), and consequently is often referred to as the IOTF method. For the IOTF method the percentile levels corresponding to a BMI of 25 kg/m2 (overweight) and 30 kg/m2 (obese) at age 18 were identified and projected backwards into childhood using a large (n=97 876) sample of youth from 6 countries (Britain, US, Holland, Singapore, Hong Kong, Brazil). Thus, the IOTF thresholds are anchored to the adult thresholds for overweight and obesity, and are a reflection of the relationship between BMI and health risks in adulthood rather than the relationship between BMI and health in childhood per se.
It is important to note that the CDC BMI growth curves are not equivalent to the BMI growth curves developed in other countries or the IOTF curves. illustrates the differences between the CDC and IOTF classification systems. The obese IOTF threshold is higher than the CDC threshold at most ages. This results in consistently higher obesity prevalence based on the CDC classification system than the IOTF classification system, with these differences being particularly large in the younger age ranges (CitationFlegal et al 2001).
Figure 2 Comparison between the Centers for Disease Control and Prevention (CDC) and International Obesity Task Force (IOTF) body mass index classification systems for overweight and obesity in youth.
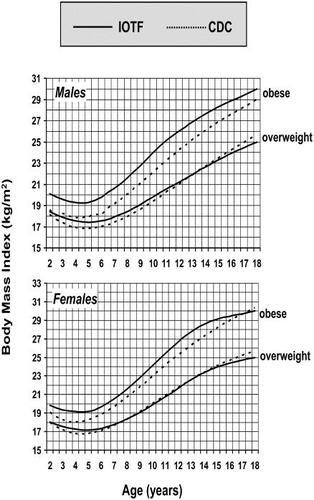
Two recent studies have directly compared the ability of the CDC and IOTF classification systems to predict CVD risk factors (CitationKatzmarzyk et al 2004; CitationJanssen et al 2005b). In both studies the CDC and IOTF obesity thresholds had similar sensitivity (correctly identifying those with high risk values) and specificity (correctly identifying those without high risk values) for identifying children and adolescents with elevated CVD risk factors; however, the IOTF obesity threshold demonstrated slightly higher specificity and slightly lower sensitivity than the CDC obesity threshold.
With respect to the clinical management of adolescent obesity, the physical exam should include an accurate measurement of BMI that should be compared with the age and gender appropriate BMI curves as recommended by the CDC (http://www.cdc.gov/growthcharts/). Equally as important as the physical exam is the assessment of patient and family history. Secondary causes of obesity should be identified or excluded so that the appropriate treatment can be recommended. Secondary causes of obesity, although rare, include endocrine (hypothyrodism and Cushing's disease) and genetic disorders (mutation of the melanocortin-4-receptor and leptin deficiency) (CitationMontague et al 1997; CitationFarooqi et al 2003). Most obese children and adolescents will have “common obesity” with no endocrine or genetic aetiology.
In patients who are obese, obesity-related health consequences need to be identified and treated. These may include non-CV comorbidities (orthopaedic abnormalities, neurological and gastroentintestinal problems, asthma, and sleep apnea) as well as CVD comorbidities (T2DM, hypertension, and dyslipidemia) (CitationMust and Strauss 1999). In pediatric patients who are not obese, a complete patient and family history will also aid in determining risk factors for the development of obesity. Risk factors include: parental obesity, increased birth weight, history of childhood cancer, sedentary lifestyle, and poor eating habits. Appropriate preventative measures should be taken before overweight or obesity develops. These measures are discussed below.
Waist circumference
Using the percentile growth chart approach, reference data for waist circumference in children and adolescents have been developed in many countries such as Cuba (CitationMartinez et al 1994), Italy (CitationZannolli and Morgese 1996), Spain (CitationMoreno et al 1999), the UK (CitationMcCarthy et al 2001), the US (CitationFernandez et al 2004), and Canada (CitationKatzmarzyk 2004). In Canada, a recommendation has been made to use the age- and gender-specific 90th percentile of waist circumference to identify overweight adolescents (). Using a percentile approach is completely arbitrary (eg, why not use the 89th percentile instead of the 90th percentile?), and there have been limited attempts to develop waist circumference thresholds in children and youth that are based on relationships with CVD risk (CitationMoreno et al 2002; CitationKatzmarzyk et al 2004). Thus, a priority for future research is the investigation of the clinical utility of existing waist circumference percentiles, and the development and validation of health-based waist circumference thresholds.
Figure 3 Waist circumference growth curves for the 5th, 10th, 25th, 75th, 90th, and 95th percentiles for (a) males and (b) females 11–18 years of age. Data source was the 1981 Canada Fitness Survey. Katzmarzyk PT. 2004. Waist circumference percentiles for Canadian youth 11–18 y of age. Eur J Clin Nutr, 58:1011-15. Copyright © 2004.
Although it has been recommended that waist circumference be used in conjunction with BMI measurements (CitationBellizzi and Dietz 1999), there has only been a single attempt in the pediatric population to determine how BMI and waist circumference measurements could be used in combination to predict obesity-related health risk (CitationJanssen et al 2005a). When BMI (normal, overweight, or obese) and waist circumference (low or high) values were categorized, as would be done in a clinical setting, a high waist circumference provided additional information regarding CVD risk factors than that provided by BMI alone (CitationJanssen et al 2005a). For example, in the overweight BMI category, children with a high waist circumference were 2.3 times more likely to have the metabolic syndrome than children with a low waist circumference. This study provides the first evidence to support the combined use of BMI and waist circumference in children and adolescents. Additional studies are warranted.
Cardiovascular health consequences of obesity
Although the most severe complications of obesity do not manifest until later in life, CV health consequences may already be evident at a young age (CitationRaitakari et al 2003). Childhood and adolescent obesity are associated with increased rates of hypertension, hyperlipidemia, T2DM, and early development of atherosclerotic lesions. The presence of these CVD risk factors does not necessarily represent morbidity at a young age, but the increased risk of developing CVD in adulthood. The focus of this section will be on the association between childhood and adolescent obesity and risk of CVD; however, it is important to mention that obesity in young people is associated with a number of other immediate and long-term health outcomes that fall outside of the scope of this review.
Type 2 diabetes mellitus
Formerly considered an adult disease, T2DM has increased alarmingly among adolescents (CitationFagot-Campagna et al 2000). In 1994, T2DM accounted for one third of the newly diagnosed diabetes cases among 10 to 19 year olds (CitationPinhas-Hamiel et al 1996). Ninety percent of those T2DM cases had BMI values at or above the 90th percentile for their age and gender.
T2DM usually develops over many years and consequently does not display itself until adulthood. Impaired glucose tolerance and insulin resistance are intermediate stages in the development of T2DM (CitationEdelstein et al 1997). Many studies have found that impaired glucose tolerance is presenting early in life among overweight and obese children and adolescents (CitationPinhas-Hamiel et al 1996; CitationSinha et al 2002; CitationWeiss et al 2005). This suggests that the metabolic process is accelerated in these individuals and the transition between impaired glucose tolerance and diabetes is shortened. For example, impaired glucose tolerance was detected in 25% of obese children and adolescents and T2DM was found in 4% (CitationSinha et al 2002).
Hyperinsulinemia, a marker of insulin resistance, is also strongly associated with obesity during adolescence (CitationCaprio et al 1996). Hyperinsulinemia influences blood pressure (through the renin–angiotensin system) and serum lipoprotein concentrations (via increased lipolysis), and often results in hypertension and dyslipidemia. The presence of these conditions, in addition to obesity, has been clinically recognized as the metabolic syndrome.
Hypertension
Blood pressure values change naturally as a function of age and gender (CitationMengetti et al 1999). illustrates the gender, age, and height specific blood pressure values corresponding to the 95th percentile. In children and adolescents, systolic and/or diastolic blood pressure values at or above the 95th percentile denote hypertension (CitationNHBPEP 2004). The association between hypertension and childhood overweight and obesity has been documented in several studies (CitationGuillaume et al 1996; CitationChu et al 1998; CitationRosner et al 2000; CitationKatzmarzyk et al 2003; CitationGenovesi et al 2005). CitationRosner and colleagues (2000) conducted a meta-analysis that included over 47 000 children to describe the relationship between blood pressure and body size. Compared with normal weight children, those with a BMI ≥90th percentile were 2.5 to 3.7 times more likely to have hypertension. Furthermore, CitationNawrot and colleagues (2004) report that systolic blood pressure increases by 0.8 mm Hg per 1 kg/m2 increase in BMI in 15 to 19 year old males and by and 1.2 mm Hg per 1 kg/m2 increase in BMI in 15 to 19 year old females.
Table 1 Hypertension cut-points (corresponding to the 95th blood pressure percentiles) for males and females according to age and height percentiles. Adapted from tables published in CitationNational High Blood Pressure Education Program 2004
In general, blood pressure values have increased among American youth over the last decade in parallel with the rise in obesity (CitationMuntner et al 2004). As a result, more children and adolescents are falling into hypertensive ranges. This is of notable concern since blood pressure values tend to track from adolescence into adulthood, especially among those who are overweight or obese (CitationLauer et al 1988; CitationMahoney et al 1991; CitationBao et al 1995; CitationSrinivasan et al 1996). In the Muscatine Study, obese children had a 10 times greater risk of developing hypertension as young adults than did non-obese children (CitationLauer et al 1988). Similarly, in the Bogalusa Heart Study youth with BMI values >75th percentile were 8.5 times more likely to become hypertensive as adults than were their lean counterparts (p<0.0001) (CitationSrinivasan et al 1996).
Dyslipidemia
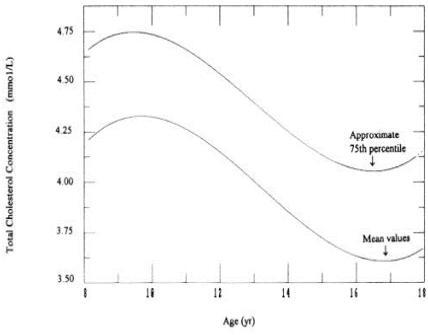
Similar to blood pressure values, lipoprotein concentrations vary with age and gender (CitationLabarthe et al 1997; CitationFreedman et al 1999; CitationSrinivasan et al 2002). An example of this effect for total cholesterol is shown in . Nonetheless, current lipid and lipoprotein clinical guidelines do not reflect these changes. illustrates the current clinical thresholds used by pediatricians in the US to diagnose dyslipidemia. Obese children and adolescents have consistently been observed to have a more unfavourable lipid and lipoprotein profile than children and adolescents with a normal body weight (CitationTeixeira et al 2001; CitationGlowinska et al 2003; CitationLi et al 2004; CitationGarces et al 2005). CitationGlowinska and colleagues (2003), have shown that obese adolescents have significantly higher low-density lipoprotein (LDL) cholesterol (2.59 mmol/L vs 2.32 mmol/L, p<0.05) and triglyceride concentrations (1.26 mmol/L vs 0.88 mmol/L, p<0.05) and significantly lower high-density lipoprotein (HDL) cholesterol concentrations (1.12 mmol/L vs 1.24 mmol/L, p<0.05) than age matched, lean controls. Further, 52% of obese children 8 to 12 years old were found to have elevated total cholesterol concentrations compared with a prevalence of 16% in non-obese children (p<0.05) (CitationFriedland et al 2002).
Figure 4 Total cholesterol growth curves for the 50th and 75th percentiles for male and female children 8–15 years of age. Labarthe DR, Nichaman MZ, Harrist RB, et al. 1997. Development of cardiovascular risk factors from ages 8 to 18 in Project Heart Beat! Study design and patterns of change in plasma total cholesterol concentration. Circulation, 95:2636-42. Copyright © 1997.
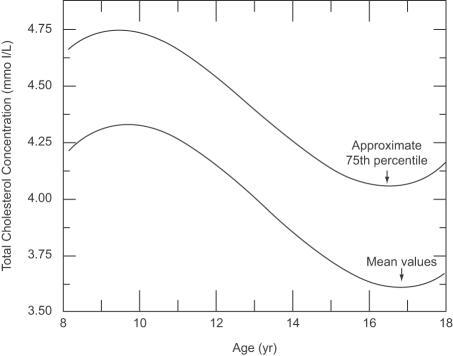
Table 2 Classification of TC, LDL-C, HDL-C, and TG concentrations in children and adolescents 2–19 years of age as defined by the CitationNCEP 2001
The slow development of atherosclerosis, a marker of CVD, begins naturally at an early age; however, the rate of progression is directly related to plasma lipoprotein concentrations (CitationMcGill et al 1997). Given that a strong relationship has been documented between adolescent overweight/obesity and abnormal serum lipoprotein concentrations (CitationLauer et al 1988; CitationCaprio et al 1996), these individuals are at increased risk of CVD later in life.
At-risk lipoprotein concentrations during the growing years are also of particular concern because they tend to track into adulthood (CitationNicklas et al 2002). As demonstrated in the Bogalusa Heart Study, the best predictor of young adult total cholesterol concentrations was measurements taken 12 years prior (CitationWebber et al 1991). Approximately 50% of children and adolescents who had total cholesterol or LDL-cholesterol concentrations above the 75th percentile had elevated concentrations at follow-up in young adulthood (CitationWebber et al 1991). In addition, overweight adolescents who remained overweight in adulthood had a 2.4, 3, and 8 times greater prevalence of abnormal LDL-cholesterol, triglycerides, and HDL-cholesterol concentrations, respectively, than did those who remained lean (p<0.05 to p<0.01) (CitationSrinivasan et al 1996).
CVD risk factor clustering and the metabolic syndrome
Overweight and obesity are strongly associated with numerous CVD risk factors. Consequently, those who are overweight tend to develop multiple risk factors. This phenomenon is known as clustering and has been documented among children and adolescents in several studies (CitationRaitakari et al 1994; CitationSrinivasan et al 1996; CitationChu et al 1998; CitationRibeiro et al 2004). Data from a nationally representative sample of adolescents in the US revealed that 23% of overweight and 56% of obese youth presented with at least 2 CVD risk factors (CitationCook et al 2003). In Taiwan, the prevalence of two or more CVD risk factors was 4 to 5 times greater in overweight adolescents compared with lean adolescents; 22% of those who were overweight had two or more risk factors (CitationChu et al 1998). Similar results were reported in Canada (CitationKatzmarzyk et al 2003), Portugal (CitationRibeiro et al 2004), and Finland (CitationRaitakari et al 1994).
The clustering of multiple CVD risk factors is known as the metabolic syndrome. In adults, two clinical definitions are used to diagnose the metabolic syndrome, that of the National Cholesterol Education Program (NCEP) Adult Treatment Panel III (ATP-III) (CitationNCEP 2001) and that of the International Diabetes Federation (IDF) (CitationAlberti et al 2005). The NCEP defines the metabolic syndrome in adults as having at least 3 of the following 5 criteria: elevated blood pressure, elevated triglycerides, low HDL-cholesterol, elevated fasting glucose levels and, a high waist circumference. The IDF has defined the metabolic syndrome as having a high waist circumference in addition to 2 of the remaining 4 criteria listed above.
An established definition of the metabolic syndrome has not yet been established for children and adolescents. A number of studies have investigated the metabolic syndrome in this age group and have either extrapolated from the NCEP adult guidelines or have directly applied the adult definition (CitationCook et al 2003; Citationde Ferranti et al 2004). An example of the adolescent guidelines used by Citationde Ferranti and colleagues (2004) are shown in . It is important to note that the thresholds for each of the metabolic syndrome components (eg, elevated blood pressure) are lower than if the disease (eg, hypertension) were being diagnosed. For example, the 90th or 95th percentile for waist circumference is typically used to diagnose abdominal obesity in children (CitationKatzmarzyk et al 2004); however, as a metabolic syndrome criterion the 75th percentile has been recommended (Citationde Ferranti et al 2004).
Table 3 Proposed pediatric and adult definitions of the metabolic syndrome. Adapted from de Ferranti SD, Gauvreau K, Ludwig DS, et al. 2004. Prevalence of the metabolic syndrome in American adolescents: findings from the Third National Health and Nutrition Examination Survey. Circulation, 110:2494-7. Copyright © 2004
Recent estimates indicate that the metabolic syndrome is present in 29% of obese adolescents (BMI ≥95th percentile) compared with 7% of overweight adolescents (BMI 85th to 95th percentile) and 0.6% of adolescents with a normal BMI (p<0.001) (CitationCook et al 2003). This is of concern because the presence of multiple metabolic disorders persists from childhood into adulthood 25%–60% of the time (CitationBao et al 1994; CitationRaitakari et al 1994) and because the metabolic syndrome is a strong predictor of T2DM and CVD in adulthood (CitationPearson et al 2002).
Adult obesity
The persistence of obesity from childhood or adolescence into adulthood has been consistently demonstrated in the literature and is associated with increased risk of CVD (CitationGuo et al 1994; CitationSrinivasan et al 1996; CitationPower et al 1997; CitationWhitaker et al 1997). Data from the Bogalusa Heart Study indicate that 58% of adolescents who had a BMI >75th percentile remained overweight 12 to 14 years later (CitationSrinivasan et al 1996). Similarly, in a study conducted by CitationWhitaker and colleagues (1997), 64% of the study participants who were classified as obese during early adolescence remained obese in adulthood.
The likelihood that obesity will persist into adulthood is related to both the severity of obesity and the age at which it is present. CitationPower and colleagues (1997) found that the correlations for BMI at ages 7 and 33 years were not very strong; however, the correlations increased with increasing age during adolescence. Similarly, CitationGuo and colleagues (1994) found that BMI at age 18 was a stronger predictor of overweight status at age 35 than was BMI at age 13. It should also be noted that many lean adolescents develop overweight or obesity during adulthood (CitationSrinivasan et al 1996; CitationPower et al 1997). These individuals are at increased CVD risk (CitationVan Itallie 1985; CitationRaitakari et al 1994), indicating that the focus of overweight treatment and prevention in adults should not only be specific to those who were obese as children and adolescents.
In adults, evidence suggests that the duration of overweight and obesity has a detrimental effect on obesity-related comorbidities (CitationMuscelli et al 1998; CitationWannamethee and Shaper 1999; CitationJanssen et al 2004). For instance, CitationJanssen and colleagues (2004) demonstrated that by comparison with women with a normal BMI, the likelihood of having T2DM was increased 3-fold in women who were overweight for less than 10 years and by 7-fold in women who were overweight for 10 years or longer (p<0.001). It can be inferred from these results that the development of overweight or obesity in adolescence and its persistence into adulthood may be associated with a higher risk of CVD compared with adult onset obesity. The importance of targeting obesity early on should therefore be emphasized in efforts to decrease adult risk of CVD.
Prevention of obesity
Adolescence is a critical period of biologic, social, and psychological development. It is also a transitional period in which increasing independence is gained and adult patterns and health behaviours are established. Thus, it is a pivotal time in which to intervene and prevent the development of overweight and obesity. Given the continuously increasing rates of adolescent overweight and obesity, it is clear that recent prevention strategies have been ineffective (CitationSummerbell et al 2005).
Gaining control of the increasing prevalence of overweight and obesity in youth has become a public health priority. In the US, the Institute of Medicine (IOM) Committee on Prevention of Obesity in Children and Youth has recently made several recommendations as part of an action plan to decrease the prevalence of obesity in children and adolescents (CitationKoplan et al 2005). The ten recommendations focus on the following aspects: federal government, marketplace, media, local communities, and school and home environments (). The IOM committee also recognized that in order to achieve their goals, changes will have to occur at many levels of society and these changes will require coordination of federal and state governments, local communities, and the private sector (CitationKoplan et al 2005).
Table 4 Recommendations made by the Institute of Medicine Committee on Prevention of Obesity in Children and Youth
Population-wide measures advocating energy balance, including regular physical activity and healthy eating behaviors, are the most common methods proposed to prevent obesity in young people (CitationReilly and McDowell 2003). Since most 5–17 year olds are enrolled in school, the school setting is ideal for health promotion education among this age group. In a recently published Cochrane Database systematic review, 19 of 22 childhood obesity prevention trials were school-based (CitationSummerbell et al 2005). While 3 school-based trials found a reduced prevalence of obesity in the intervention group, the remaining 16 failed to find such a relationship.
The 3 successful school-based intervention trials tended to be large-scale with an intervention component lasting for at least 12 months (CitationSummerbell et al 2005). For example, Planet Health was a school-based randomized control trial carried out over a 2 year period (CitationGortmaker et al 1999). The study population consisted of 1295 children in 10 schools and the intervention used existing physical education programs and teachers to target diet, physical activity, and sedentary behaviors. The Planet Health study reported significant declines in obesity prevalence (odds ratio [OR]=0.47, p=0.03) and greater remission of preexisting obesity (OR=2.16, p=0.04) among females in the intervention group compared with those in the control group. Conversely, New Moves was a short-term (24 weeks) trial conducted in 201 physically inactive, overweight girls (CitationNeumark-Sztainer et al 2003). The intervention addressed personal and behavioral factors and included physical activity four times per week and nutrition and social support sessions ever other week for 16 weeks. Despite positive changes in behavior, no significant difference in BMI was noted between the intervention and control groups at followup (CitationNeumark-Sztainer et al 2003).
One of the major challenges in preventing increases in obesity is identifying a program that will induce sustained effects after the intervention is completed. To be successful, an intervention strategy will likely need to incorporate other aspects of youth life outside the classroom. This could be achieved through community-based efforts; however, there are few studies of this nature (CitationFitzgibbon et al 2002; CitationColeman et al 2005). The El Paso Coordinated Approach to Child Health (CATCH) was a community-based effort designed to use the framework of the national CATCH program (CitationLuepker et al 1996); however, the participating El Paso schools were encouraged to change the program to fit their specific needs (CitationColeman et al 2005). While the original CATCH program did not succeed in influencing overweight outcomes, the El Paso CATCH intervention significantly slowed the increase in risk of overweight and obesity compared with that was seen in the control schools (2% vs 13%). One of the reasons given for the discrepancy between the original and the El Paso CATCH interventions was the clinical versus community nature of the trials respectively (eg, each school was able to tailor the CATCH program to suit the children in their schools).
The Hip Hop to Health Jr. program is another ongoing community-based trial (CitationFitzgibbon et al 2002). This program was initiated in 2002 and is a 5-year trial that aims to alter the trajectory towards overweight and obesity in African American and Latino preschool children through a 14-week dietary/physical activity curriculum (CitationFitzgibbon et al 2002). The 2-year follow-up of the Hip Hop Jr. trial has shown positive results (CitationFitzgibbon et al 2005). The intervention children had significantly smaller increases in BMI at the 1-year (0.06 kg/m2 vs 0.59 kg/m2, p=0.01) and 2-year (0.54 kg/m2 vs 1.08 kg/m2, p=0.02) follow-up periods.
Parents should also be targeted for intervention since they contribute to adolescent's home life. Several family-based obesity prevention programs exist (CitationStolley and Fitzgibbon 1997; CitationEpstein et al 2001; CitationBaranowski et al 2003), but few have proved successful (CitationRobinson et al 2003).
Treatment of obesity
Treatment strategies for childhood and adolescent obesity should be multidisciplinary, supportive, and ongoing. Parents should play an integral role in supporting the treatment process and being active role models with respect to eating behaviors and physical activity.
The adolescent age group can be a very difficult population to treat for any illness or condition, including obesity. Although treatment goals for overweight adolescents are similar to those recommended for adults (dietary modification and physical activity), weight loss per se is not necessarily the best strategy (CitationDaniels et al 2005). In general, there is a lack of information regarding the longterm consequence and safety of weight loss in children and adolescents. Therefore, even a slowing of weight gain can be beneficial, especially if the growth and maturation process is still ongoing. For example, CitationWeiss and colleagues (2004) found that a slowed weight gain in obese adolescents was associated with a delay in the development of obesity-related metabolic disorders such as T2DM.
Dietary management and physical activity
The American Heart Association (AHA) has recently issued a scientific statement titled “Overweight in Children and Adolescents” that focused on the pathophysiology, consequences, prevention, and treatment of overweight in youth (CitationDaniels et al 2005). This next section is based in large measure on the AHA statement. According to the AHA, dietary modification combined with enhanced physical activity is the preferred treatment strategy for obesity in young people. The goals in dietary management are to provide appropriate calorie intake, optimum nutrition to facilitate normal growth, and to develop and sustain healthy eating habits (CitationDaniels et al 2005). Successful weight loss and maintenance includes the incorporation of regular physical activity into the treatment plan. The current recommendation is for children to accumulate a minimum of 30–60 minutes of physical activity every day.
The AHA indicated that dietary management should emphasize balance, variety, and adequacy of overall eating behaviors. For 4–18 year olds, the most recent Dietary Reference Intakes recommend a fat intake of 25%–35% kcal, a carbohydrate intake of 45%–65% kcal, and a protein intake of 10%–30% kcal (CitationDaniels et al 2005). Additional recommendations include eating a variety of foods high in fruit and vegetables and paying special attention to age-appropriate portion sizes. Food choices should be low in saturated fat, total fat, and cholesterol. In addition, counseling and recommendations should be made within the context of the family's culture, living environment, and socio-economic status (CitationDaniels et al 2005).
The AHA scientific statement also recognized that physical activity is vital to the success of weight loss and management. It should be incorporated into a healthy lifestyle and maintained throughout life. In order to achieve this, the emphasis should be on active living rather than strenuous exercise. Active living includes walking with friends or walking the dog, dancing, bicycling, jump rope, and skateboarding. These types of activities can be easily integrated into daily life and should not be performed simply to lose weight. Recommended activities should be fun and enjoyable, as well as adaptable to their lifestyle and schedule (CitationDaniels et al 2005).
With respect to physical activity intervention in the treatment of pediatric obesity, evidence is limited (CitationReilly and McDowell 2003). In a systematic review conducted by CitationReilly and McDowell (2003), only two high-quality studies of this nature were identified (CitationEpstein et al 1995, Citation2000). In the first study, CitationEpstein and colleagues (1995) compared the “traffic light” diet with one of 3 randomly allocated treatments: 1) reduction in sedentary behavior, 2) increases in physical activity, and 3) a combination of treatment 1 and 2. The sedentary behavior treatment group showed the greatest change in percent overweight at the 12-month follow-up compared with the activity treatment group (−20% vs −12%, p<0.05). This study highlights the potential value of targeting sedentary behavior in the treatment of childhood obesity. These results were confirmed in the more recent study conducted by CitationEpstein and colleagues (2000).
In contrast to what has been recommended by the AHA, CitationDorsey and colleagues (2005) found that physician-based treatment strategies most commonly focused on dietary changes and less often on increasing physical activity. Advice on dietary changes was often general (eg, alter current dietary practices) and rarely specific (eg, avoid particular foods and control portion sizes) (CitationDorsey et al 2005). Rarely was there a documented plan to follow-up on behavioral changes. Although there are several treatment strategies that target diet and physical activity behaviors, these approaches are not being translated into clinical practice (CitationDorsey et al, 2005). Thus, efforts to treat childhood and adolescent obesity may be better executed with the adoption of standard diagnostic and treatment practices.
Many obesity-related CVD comorbidities can be resolved after significant weight loss in obese youth. For example, CitationReinehr and colleagues (2005) conducted a 1-year intervention study in which children were advised by a multidisciplinary team as to a suitable diet and necessary physical activity and behavior patterns. They demonstrated that a reduction in BMI standard deviation score greater than 0.5 was associated with a significant decrease in systolic and diastolic blood pressure (p<0.001) and triglycerides (TG) (p<0.012), and a significant increase in HDL cholesterol (p<0.023) (CitationReinehr et al 2005). More specifically, systolic and diastolic blood pressure decreased by a mean of 11 mm Hg and 9 mm Hg respectively, in children who were hypertensive at baseline. In those who were dyslipidemic at baseline LDL cholesterol decreased by a mean of 28 mg/dL, TG decreased by a mean of 82 mg/dL, and HDL cholesterol increased by a mean of 9 mg/dL after the 1-year intervention program (CitationReinehr and Andler, 2004).
In support of these findings, CitationWeiss and colleagues (2004) followed 77 children over a two year period examining the prevalence of the metabolic syndrome at baseline and again at year 2. At baseline, 34 obese subjects met the criteria for the metabolic syndrome; at follow-up only 24 subjects met the criteria. The 10 subjects who no longer met the criteria for the metabolic syndrome had gained significantly less weight (3.74±2.6 kg vs 11.93±2.9 kg, p=0.05) over the 2-year period.
This evidence suggests that treatment of CVD risk factors in obese youth can be accomplished via weight management. However, weight loss and management in children is a contentious issue; as children and adolescents mature their body weight and BMI will increase naturally (CitationCole et al 2000). Thus, it is encouraging that increasing physical activity even in the absence of weight loss improves CVD risk. In adults, physical fitness is associated with improved CVD risk factor status (CitationGibbons et al 1983, CitationTakemura et al 1999) and reduced CVD mortality (CitationFarrell et al 1998) independent of other potential confounding risk factors such as adiposity. Limited evidence in children also indicates that fitness and physical activity are related to CVD risk factors independent of BMI and body fat (CitationTolfrey et al 1999). In addition, physical activity participation during adolescence predicts physical activity levels (CitationTelama et al 2005) and CVD risk factor profile (CitationTwisk et al 2002) in adulthood. Together, these findings imply that participation in physical activity during childhood and adolescence will positively impact CVD risk in adulthood independent of any effects physical activity has on body weight and body composition.
Pharmacological therapy
Two weight loss medications have been employed in adolescent patients: sibutramine and orlistat. Both drug therapies were originally developed for weight loss and management in obese adults, and are intended to be used in conjunction with behavioural therapy (including diet and physical activity). Sibutramine acts directly on the central nervous system by stimulating noradrenergic and serotonergic activity, thereby causing appetite suppression (CitationVan Gaal et al 1998). It is currently being used in the adolescent population for experimental purposes only and has not yet been approved by the US Food and Drug Administration (FDA) for use in this age group. In two experimental trials to date, sibutramine was associated with a significant weight reduction compared with placebo (CitationBerkowitz et al 2003; CitationGodoy-Matos et al 2005). In the original sibutramine trial, conducted by CitationBerkowitz and colleagues (2003), 82 obese (BMI between 32 kg/m2 and 44 kg/m2) male and post-menarcheal females, 12–17 years of age, were randomized to either sibutramine plus behavioural therapy (including diet and exercise) or to placebo plus behavioural therapy. The sibutramine group experienced a mean weight loss of 7.8 kg compared with a more modest weight loss of 3.2 kg in the placebo group. More than twice as many of those in the sibutramine group reduced their initial BMI by 10% and 15% compared with those receiving placebo (CitationBerkowitz et al 2003).
Similar findings were confirmed in a second randomized control trial conducted by CitationGodoy-Matos and colleagues (2005). At the end of the 6-month intervention, the participants assigned to sibutramine lost an average of 10.3 kg while the participants in the placebo group lost 2.4 kg. Approximately 25% of adolescents in the sibutramine group reduced their initial weight by at least 15% compared with 0% in the placebo group.
In both sibutramine trials, no differences between the two groups were found with respect to systolic and diastolic blood pressures, heart rate, and biochemical parameters (CitationBerkowitz et al 2003; CitationGodoy-Matos et al 2005), with the exception of TG in one of the studies which was significantly reduced in the sibutramine group alone (p<0.05) (CitationGodoy-Matos et al 2005). Both trials reported sibutramine to be relatively well tolerated in the obese adolescent population and no participant withdrew due to adverse effects (CitationBerkowitz et al 2003; CitationGodoy-Matos et al 2005). The only significantly different adverse event between the two groups was constipation, which occurred in 40% of the participants in the sibutramine group compared with 13% of those in the placebo group (p=0.039) (CitationGodoy-Matos et al 2005).
Orlistat is the most recent anti-obesity drug on the market; contrary to sibutramine, it has been approved by the FDA for use in adolescents aged 12 and older (CitationFDA 2003). Orlistat is a lipase inhibitor, which reduces fat absorption in the gastrointestinal tract. It acts by inhibiting pancreatic and gastric lipase secretion thus reducing lipid breakdown. The unabsorbed fat is excreted in feces. As a result, the drugs' adverse side effects include fecal incontinence, flatulence, and oily spotting. These effects are enhanced with consumption of fatty foods and orlistat may therefore contribute to weight loss via the aversion of fatty foods.
An initial non-randomized study published in 2002 examined the tolerability and effectiveness of orlistat over 3 months in a sample of 20 adolescents (CitationMcDuffie et al 2002). The adverse effects were generally mild, limited to gastrointestinal effects, and decreased with time. Body weight decreased by 4.4 kg (p<0.001). Orlistat use was associated with significant improvements in total and LDL-cholesterol, fasting insulin and glucose, and insulin sensitivity (p<0.02).
CitationChanoine and colleagues (2005) conducted the first long-term study investigating the safety and efficacy of orlistat in the pediatric population. Obese male and female adolescents (12 to 16 years of age) were eligible if their BMI was at least 2 units above the respective age- and sex-specific 95th percentile of the CDC growth curves (CitationChanoine et al 2005). In total, 539 adolescents were randomized to receive orlistat or placebo in a one year long intervention. All participants were instructed to maintain a hypocaloric diet designed to produce a weight loss of 0.5 kg to 1.0 kg per week as well as encouraged to engage in regular physical activity (CitationChanoine et al 2005). The orlistat group was instructed to take 120 mg of the lipase inhibitor 3 times per day. The placebo was administered in a similar fashion.
During the first 12 weeks of intervention, the orlistat and placebo groups experienced a mean weight loss of approximately 2.3 kg and 0.5 kg, respectively (CitationChanoine et al 2005). Weight loss stabilized thereafter in those receiving orlistat while those taking placebo began to gain weight. By the end of the year-long intervention, both groups had gained weight beyond their initial baseline weight, although the placebo group gained significantly more (+0.53 kg vs +3.14 kg). This effect is illustrated in . The orlistat group had a significantly greater decrease in waist circumference (−1.33 cm vs +0.12 cm) as well as greater fat loss (−2.53 kg vs +0.6 kg) compared with the placebo group (CitationChanoine et al 2005). Moreover, 26% of subjects in the orlistat group experienced a 5% or larger decrease in BMI and 13% experienced a 10% or larger decrease in BMI (compared with 16% and 4% of those in the placebo group).
Figure 5 The change in weight throughout a 52-week intervention of orlistat (• symbols) and placebo (○ symbols). Lifestyle modification was prescribed to both groups. Chanoine JP, Hampl S, Jensen C, et al. 2005. Effect of orlistat on weight and body composition in obese adolescents: a randomized controlled trial. JAMA, 293:2873-83. Copyright © 2005.
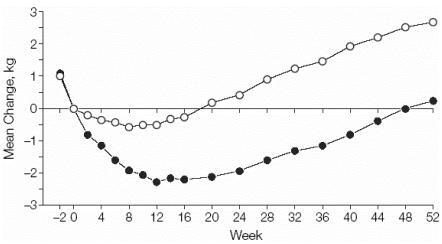
This evidence suggests that a phamacotherapy approach to the treatment of adolescent obesity is effective in the short to medium term (1 year); however, what happens after the first year of use is unclear. In the orlistat trial the weight of those taking orlistat stabilized after 12 weeks and then began to increase (CitationChanoine et al 2005), which leads to several questions. Is the weight regained once drug therapy is discontinued? Does an obese adolescent have to remain on medication to maintain weight loss long term? If that is the case, are there long-term side effects?
Surgery
Regardless of age, surgical management of obesity should only be performed after intensive multidisciplinary programs, including psychological support, have failed (CitationFlodmark et al 2004). Furthermore, surgery should only be performed in centers equipped to deal with the psychological and medical complications of the procedure. These centers should include specialists with expertise in adolescent obesity evaluation and management, psychology, nutrition, and physical activity instruction (CitationInge et al 2004).
The two most common forms of bariatric surgery in adolescents are Roux-en-Y gastric bypass (RYGB) and adjustable gastric banding (AGB). In a review of bariatric surgery for adolescents, CitationInge and colleagues (2004) outlined the criteria that should be met in selecting an adolescent for surgery (). Some of these criteria include morbid obesity, severe obesity-related comorbidities such as T2DM and hypertension, an understanding of the surgical procedure, and commitment to postoperative nutritional guidelines (CitationInge et al 2004; CitationDaniels et al 2005).
Table 5 Selection criteria for adolescents to undergo bariatric surgery as a treatment for obesity. Reproduced with permission from Inge TH, Krebs NF, Garcia VF, et al. 2004. Bariatric surgery for severely overweight adolescents: concerns and recommendations. Pediatrics, 114:217-23. Copyright © 2004
There are both advantages and disadvantages of bariatric surgery. Possibly, the greatest advantage is weight loss and reduction of associated comorbidities (CitationChapman et al 2004). The disadvantages, however, are far more numerous. Potential complications of bariatric surgery include intestinal leakage, incision hernia, thromboembolitic disease, symptomatic cholelithiasis, small bowel obstruction, and macro- and micro-nutrient deficiencies (CitationSugerman et al 2003; CitationChapman et al 2004). Due to the latter, micronutrients, such as calcium, folate, thiamine, iron, vitamin B12, and multivitamins must be supplemented long-term after surgery.
Roux-en-Y gastric bypass is the most common bariatric surgery for the treatment of obesity among children and adolescents. It is the safest and most appropriate surgical option for this age group and has been approved by the US FDA (CitationInge et al 2004). RYGB divides the stomach into 2 unequal portions, leaving approximately 5% for food consumption. RYGB is performed laproscopically promoting less pain, faster recovery, and quicker discharge from the hospital. In a review of 33 adolescent patients who underwent RYGM, CitationSugerman and colleagues (2003) reported successful weight reduction in most of the patients, although 15% of the patients regained the lost weight within 5–10 years of surgery. Furthermore, most obesity-related comorbidities were resolved within one year (CitationSugerman et al 2003).
Adjustable gastric banding is not currently approved by the FDA for use in children and adolescents. Thus, it has only been performed in adolescents in experimental settings (CitationStanford et al 2003; CitationWidhalm et al 2004; CitationHorgan et al 2005). Briefly, AGB involves creating a small pouch in the upper portion of the stomach with a controlled and adjustable band. The band is adjustable; the size of the entrance-way from the pouch to the stomach can be altered to allow more or less food through at one time. In a case report of 4 morbidly obese adolescents (17 to 19 years of age), AGB was successful in each case and significant weight loss was achieved (CitationHorgan et al 2005). Follow-up time for each patient varied; however, at 30 months one patient had lost 57% of their initial weight and at 12 months another patient had experienced a 34% weight loss (CitationHorgan et al 2005). Comparable results have been documented in other studies (CitationStanford et al 2003; CitationWidhalm et al 2004). Randomized control trials are needed before AGB is considered a safe and effective method of obesity treatment in adolescents. Regardless of the surgical method chosen, the potential complications such as weight regain and nutrient deficiencies lend to the importance of a team approach.
Conclusions
Key summary recommendations on how clinicians and other healthcare practitioners can use this information contained in this review are contained within . As the prevalence of overweight and obese children and adolescents continues to rise, so will the risk of weight-related CV complications. Although behavioral modification, including increased physical activity and proper nutrition, is the preferred method of treatment in the adolescent age group, little evidence exists to suggest this method is effective. Pharmacotherapy is gaining popularity in adulthood and is also looking promising for obese adolescents. It is important that drug treatment be carried out in combination with dietary modifications and increased physical activity to give youth the proper tools and information needed to maintain weight loss throughout adulthood. Furthermore, increasing physical activity levels among adolescents will reduce many CVD risk factors that are not necessarily affected by weight loss (CitationPate et al 1996; CitationBoreham et al 1997; CitationCarrel et al 2005). Additional large-scale randomized control trials assessing the long-term impact of drug treatment in the pediatric population are required before it becomes widely accepted.
Table 6 Key recommendations of review
References
- AlbertiKGZimmetPShawJIDF Epidemiology Task Force Consensus GroupThe metabolic syndrome – a new worldwide definitionLancet200536610596216182882
- BaoWSrinivasanSRWattigneyWAPersistence of multiple cardiovascular risk clustering related to syndrome X from childhood to young adulthood. The Bogalusa Heart StudyArch Intern Med1994154184278053753
- BaoWThreefootSASrinivasanSREssential hypertension predicted by tracking of elevated blood pressure from childhood to adulthood: the Bogalusa Heart StudyAm J Hypertens19958657657546488
- BaranowskiTBaranowskiJCCullenKWThe fun, food, and fitness project (FFFP): the Baylor GEMS pilot studyEthn Dis200313S30912713209
- BarlowSEDietzWHObesity evaluation and treatment: Expert Committee recommendations. The Maternal and Child Health Bureau, Health Resources and Services Administration and the Department of Health and Human ServicesPediatrics1998102E299724677
- BellizziMCDietzWHWorkshop on childhood obesity: summary of the discussionAm J Clin Nutr199970173S175S
- BerkowitzRIWaddenTATershakovecAMBehavior therapy and sibutramine for the treatment of adolescent obesity: a randomized controlled trialJAMA200328918051212684359
- BorehamCATwiskJSavageMJPhysical activity, sports participation, and risk factors in adolescentsMed Sci Sports Exerc199729788939219207
- CaprioSBronsonMSherwinRSCo-existence of severe insulin resistance and hyperinsulinaemia in pre-adolescent obese childrenDiabetologia1996391489978960831
- CarrelALClarkRRPetersonSEImprovement of fitness, body composition, and insulin sensitivity in overweight children in a school-based exercise program: a randomized, controlled studyArch Pediatr Adolesc Med2005159963816203942
- ChanoineJPHamplSJensenCEffect of orlistat on weight and body composition in obese adolescents: a randomized controlled trialJAMA200529328738315956632
- ChapmanAEKiroffGGamePLaparoscopic adjustable gastric banding in the treatment of obesity: a systematic literature reviewSurgery20041353265114976485
- ChinnSRonaRJPrevalence and trends in overweight and obesity in three cross sectional studies of British children, 1974–94BMJ200132224611141148
- ChuNFRimmEBWangDJClustering of cardiovascular disease risk factors among obese schoolchildren: the Taipei Children Heart StudyAm J Clin Nutr199867114169625086
- ColeTJBellizziMCFlegalKMEstablishing a standard definition for child overweight and obesity worldwide: international surveyBMJ20003201240310797032
- ColeTJFreemanJVPreeceMABritish 1990 growth reference centiles for weight, height, body mass index and head circumference fitted by maximum penalized likelihoodStat Med199817407299496720
- ColeTJRoedeMJCentiles of body mass index for Dutch children aged 0–20 years in 1980 – a baseline to assess recent trends in obesityAnn Hum Biol199926303810462152
- ColemanKJTillerCLSanchezJPrevention of the epidemic increase in child risk of overweight in low-income schools: the El Paso coordinated approach to child healthArch Pediatr Adolesc Med20051592172415753263
- CookSWeitzmanMAuingerPPrevalence of a metabolic syndrome phenotype in adolescents: findings from the third National Health and Nutrition Examination Survey, 1988–1994Arch Pediatr Adolesc Med2003157821712912790
- DanielsSRArnettDKEckelRHOverweight in children and adolescents: pathophysiology, consequences, prevention, and treatmentCirculation20051111999201215837955
- de FerrantiSDGauvreauKLudwigDSPrevalence of the metabolic syndrome in American adolescents: findings from the Third National Health and Nutrition Examination SurveyCirculation20041102494715477412
- DeurenbergPWeststrateJASeidellJCBody mass index as a measure of body fatness: age- and sex-specific prediction formulasBr J Nutr199165105142043597
- DorseyKBWellsCKrumholzHMDiagnosis, evaluation, and treatment of childhood obesity in pediatric practiceArch Pediatr Adolesc Med2005159632815996996
- DudejaVMisraAPandeyRMBMI does not accurately predict overweight in Asian Indians in northern IndiaBr J Nutr2001861051211432771
- EdelsteinSLKnowlerWCBainRPPredictors of progression from impaired glucose tolerance to NIDDM: an analysis of six prospective studiesDiabetes199746701109075814
- EllisKJHuman body composition: in vivo methodsPhysiol Rev2000806498010747204
- EpsteinLHPaluchRAGordyCCDecreasing sedentary behaviors in treating pediatric obesityArch Pediatr Adolesc Med2000154220610710017
- EpsteinLHPaluchRARaynorHASex differences in obese children and siblings in family-based obesity treatmentObes Res200197465311743058
- EpsteinLHValoskiAMVaraLSEffects of decreasing sedentary behavior and increasing activity on weight change in obese childrenHealth Psychol199514109157789345
- Fagot-CampagnaAPettittDJEngelgauMMType 2 diabetes among North American children and adolescents: an epidemiologic review and a public health perspectiveJ Pediatr20001366647210802501
- FarooqiISKeoghJMYeoGSClinical spectrum of obesity and mutations in the melanocortin 4 receptor geneN Engl J Med200334810859512646665
- FarrellSWKampertJBKohlHW3rdInfluences of cardiorespiratory fitness levels and other predictors on cardiovascular disease mortality in menMed Sci Sports Exerc1998308999059624649
- [FDA] United States Food and Drug AdministrationCDER Report to the Nation [online]2003 Accessed 25 October 2005. URL: http://www.fda.gov/cder/reports/rtn/2003/rtn2003-1.HTM
- FernandezJRReddenDTPietrobelliAWaist circumference percentiles in nationally representative samples of African-American, European-American, and Mexican-American children and adolescentsJ Pediatr20041454394415480363
- FitzgibbonMLStolleyMRDyerARA community-based obesity prevention program for minority children: rationale and study design for Hip-Hop to Health JrPrev Med2002342899711817926
- FitzgibbonMLStolleyMRSchifferLTwo-year follow-up results for Hip-Hop to Health Jr.: a randomized controlled trial for overweight prevention in preschool minority childrenJ Pediatr20051466182515870664
- FlegalKMOgdenCLWeiRPrevalence of overweight in US children: comparison of US growth charts from the Centers for Disease Control and Prevention with other reference values for body mass indexAm J Clin Nutr20017310869311382664
- FlodmarkCELissauIMorenoLANew insights into the field of children and adolescents' obesity: the European perspectiveInt J Obes Relat Metab Disord20042811899615365581
- FredriksAMVan BuurenSBurgmeijerRJContinuing positive secular growth change in The Netherlands 1955–1997Pediatr Res2000473162310709729
- FreedmanDSSerdulaMKSrinivasanSRRelation of circumferences and skinfold thicknesses to lipid and insulin concentrations in children and adolescents: the Bogalusa Heart StudyAm J Clin Nutr199969308179989697
- FriedlandONemetDGorodnitskyNObesity and lipid profiles in children and adolescentsJ Pediatr Endocrinol Metab20021510111612199328
- GarcesCGutierrez-GuisadoJBenaventeMObesity in Spanish schoolchildren: relationship with lipid profile and insulin resistanceObes Res2005139596315976136
- GenovesiSGiussaniMPieruzziFResults of blood pressure screening in a population of school-aged children in the province of Milan: role of overweightJ Hypertens200523493715716688
- GibbonsLWBlairSNCooperKHAssociation between coronary heart disease risk factors and physical fitness in healthy adult womenCirculation198367977836831681
- GlowinskaBUrbanMKoputANew atherosclerosis risk factors in obese, hypertensive and diabetic children and adolescentsAtherosclerosis20031672758612818410
- Godoy-MatosACarraroLVieiraATreatment of obese adolescents with sibutramine: a randomized, double-blind, controlled studyJ Clin Endocrinol Metab2005901460515613431
- GoranMIGowerBARelation between visceral fat and disease risk in children and adolescentsAm J Clin Nutr199970149S156S
- GortmakerSLPetersonKWiechaJReducing obesity via a school-based interdisciplinary intervention among youth: Planet HealthArch Pediatr Adolesc Med19991534091810201726
- GuillaumeMLapidusLBeckersFCardiovascular risk factors in children from the Belgian province of Luxembourg. The Belgian Luxembourg Child StudyAm J Epidemiol1996144867808890665
- GuoSSChumleaWCRocheAFAge- and maturity-related changes in body composition during adolescence into adulthood: the Fels Longitudinal StudyInt J Obes Relat Metab Disord1997211167759426385
- GuoSSRocheAFChumleaWCThe predictive value of childhood body mass index values for overweight at age 35 yAm J Clin Nutr199459810198147324
- HimesJHDietzWHGuidelines for overweight in adolescent preventive services: recommendations from an expert committee. The Expert Committee on Clinical Guidelines for Overweight in Adolescent Preventive ServicesAm J Clin Nutr199459307168310979
- HorganSHoltermanMJJacobsenGRLaparoscopic adjustable gastric banding for the treatment of adolescent morbid obesity in the United States: a safe alternative to gastric bypassJ Pediatr Surg2005408690 discussion 90-115868564
- IngeTHKrebsNFGarciaVFBariatric surgery for severely overweight adolescents: concerns and recommendationsPediatrics20041142172315231931
- JanssenIKatzmarzykPTBoyceWFComparison of overweight and obesity prevalence in school-aged youth from 34 countries and their relationships with physical activity and dietary patternsObes Rev200561233215836463
- JanssenIKatzmarzykPTRossRDuration of overweight and metabolic health risk in American men and womenAnn Epidemiol2004145859115350959
- JanssenIKatzmarzykPTSrinivasanSRCombined influence of body mass index and waist circumference on coronary artery disease risk factors among children and adolescentsPediatrics2005a11516233015930225
- JanssenIKatzmarzykPTSrinivasanSRUtility of childhood BMI in the prediction of adulthood disease: comparison of national and international referencesObes Res2005b1311061515976154
- KatzmarzykPTWaist circumference percentiles for Canadian youth 11–18 y of ageEur J Clin Nutr20045810111515220942
- KatzmarzykPTSrinivasanSRChenWBody mass index, waist circumference, and clustering of cardiovascular disease risk factors in a biracial sample of children and adolescentsPediatrics2004114e19820515286257
- KatzmarzykPTTremblayAPerusseLThe utility of the international child and adolescent overweight guidelines for predicting coronary heart disease risk factorsJ Clin Epidemiol2003564566212812820
- KleinDJAronson FriedmanLHarlanWRObesity and the development of insulin resistance and impaired fasting glucose in black and white adolescent girls: a longitudinal studyDiabetes Care2004273788314747217
- KoplanJPLivermanCTKraakVIPreventing childhood obesity: health in the balance: executive summaryJ Am Diet Assoc2005105131815635359
- KuczmarskiRJOgdenCLGuoSS2000 CDC Growth Charts for the United States: methods and developmentVital Health Stat2002111190
- LabartheDRNichamanMZHarristRBDevelopment of cardiovascular risk factors from ages 8 to 18 in Project HeartBeat! Study design and patterns of change in plasma total cholesterol concentrationCirculation1997952636429193432
- LauerRMLeeJClarkeWRFactors affecting the relationship between childhood and adult cholesterol levels: the Muscatine StudyPediatrics198882309183405659
- LeungSSColeTJTseLYBody mass index reference curves for Chinese childrenAnn Hum Biol199825169749533516
- LiSLiuXOkadaTSerum lipid profile in obese children in ChinaPediatr Int200446425815310307
- LissauIOverpeckMDRuanWJBody mass index and overweight in adolescents in 13 European countries, Israel, and the United StatesArch Pediatr Adolesc Med2004158273314706954
- LuepkerRVPerryCLMcKinlaySMOutcomes of a field trial to improve children's dietary patterns and physical activity. The Child and Adolescent Trial for Cardiovascular Health. CATCH collaborative groupJAMA1996275768768598593
- MahoneyLTClarkeWRBurnsTLChildhood predictors of high blood pressureAm J Hypertens19914608S610S1789940
- MartinezEDevesaMBacallaoJPercentiles of the waist-hip ratio in Cuban scholars aged 4.5 to 20.5 yearsInt J Obes Relat Metab Disord199418557607951477
- McCarthyHDJarrettKVCrawleyHFThe development of waist circumference percentiles in British children aged 5.0–16.9 yEur J Clin Nutr200155902711593353
- McDuffieJRCalisKAUwaifoGIThree-month tolerability of orlistat in adolescents with obesity-related comorbid conditionsObes Res2002106425012105286
- McGillHCJrMcMahanCAMalcomGTEffects of serum lipoproteins and smoking on atherosclerosis in young men and women. The PDAY Research Group. Pathobiological Determinants of Atherosclerosis in YouthArterioscler Thromb Vasc Biol199717951069012643
- MenghettiEVirdisRStrambiMBlood pressure in childhood and adolescence: the Italian normal standards. Study Group on Hypertension of the Italian Society of PediatricsJ Hypertens19991713637210526895
- MontagueCTFarooqiISWhiteheadJPCongenital leptin deficiency is associated with severe early-onset obesity in humansNature199738790389202122
- MorenoLAFletaJMurLWaist circumference values in Spanish children – gender related differencesEur J Clin Nutr1999534293310403577
- MorenoLAPinedaIRodriguezGWaist circumference for the screening of the metabolic syndrome in childrenActa Paediatr20029113071212578286
- MuntnerPHeJCutlerJATrends in blood pressure among children and adolescentsJAMA200429121071315126439
- MuscelliECamastraSGastaldelliAInfluence of duration of obesity on the insulin resistance of obese non-diabetic patientsInt J Obes Relat Metab Disord19982226279539195
- MustAStraussRSRisks and consequences of childhood and adolescent obesityInt J Obes Relat Metab Disord199923Suppl 2S21110340798
- NawrotTSHoppenbrouwersKDen HondEPrevalence of hypertension, hypercholesterolemia, smoking and overweight in older Belgian adolescentsEur J Public Health200414361515542870
- [NCEP] National Cholesterol Education Program; Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in AdultsExecutive Summary of The Third Report of The National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, And Treatment of High Blood Cholesterol In Adults (Adult Treatment Panel III)JAMA200128524869711368702
- NeoviusMLinneYRossnerSBMI, waist-circumference and waisthip-ratio as diagnostic tests for fatness in adolescentsInt J Obes (Lond)200529163915570312
- Neumark-SztainerDStoryMHannanPJNew Moves: a school-based obesity prevention program for adolescent girlsPrev Med200337415112799128
- [NHBPEP] National High Blood Pressure Education ProgramThe fourth report on the diagnosis, evaluation, and treatment of high blood pressure in children and adolescentsPediatrics20041145557615286277
- NicklasTAVon DuvillardSPBerensonGSTracking of serum lipids and lipoproteins from childhood to dyslipidemia in adults: the Bogalusa Heart StudyInt J Sports Med200223Suppl 1S394312012261
- OgdenCLFlegalKMCarrollMDPrevalence and trends in overweight among US children and adolescents, 1999–2000JAMA200228817283212365956
- OwensSGutinBFergusonMVisceral adipose tissue and cardiovascular risk factors in obese childrenJ Pediatr19981334159672508
- PateRRHeathGWDowdaMAssociations between physical activity and other health behaviors in a representative sample of US adolescentsAm J Public Health1996861577818916523
- PearsonTABlairSNDanielsSRAHA Guidelines for Primary Prevention of Cardiovascular Disease and Stroke: 2002 Update: Consensus panel guide to comprehensive risk reduction for adult patients without coronary or other atherosclerotic vascular diseases. AHA Science Advisory and Coordinating CommitteeCirculation20021063889112119259
- Pinhas-HamielODolanLMDanielsSRIncreased incidence of non-insulin-dependent diabetes mellitus among adolescentsJ Pediatr1996128608158627431
- PowerCLakeJKColeTJBody mass index and height from childhood to adulthood in the 1958 British-born cohortAm J Clin Nutr19976610941019356525
- RaitakariOTJuonalaMKahonenMCardiovascular risk factors in childhood and carotid artery intima-media thickness in adulthood: the Cardiovascular Risk in Young Finns StudyJAMA200329022778314600186
- RaitakariOTPorkkaKVViikariJSClustering of risk factors for coronary heart disease in children and adolescents. The Cardiovascular Risk in Young Finns StudyActa Paediatr199483935407819690
- RankinenTKimSYPerusseLThe prediction of abdominal visceral fat level from body composition and anthropometry: ROC analysisInt J Obes Relat Metab Disord199923801910490780
- ReillyJJMcdowellZCPhysical activity interventions in the prevention and treatment of paediatric obesity: systematic review and critical appraisalProc Nutr Soc2003626111914692597
- ReinehrTAndlerWChanges in the atherogenic risk factor profile according to degree of weight lossArch Dis Child2004894192215102630
- ReinehrTDe SousaGAndlerWLongitudinal analyses among overweight, insulin resistance, and cardiovascular risk factors in childrenObes Res20051318243316286531
- RibeiroJCGuerraSOliveiraJBody fatness and clustering of cardiovascular disease risk factors in Portuguese children and adolescentsAm J Hum Biol2004165566215368603
- RobinsonTNKillenJDKraemerHCDance and reducing television viewing to prevent weight gain in African-American girls: the Stanford GEMS pilot studyEthn Dis200313S657712713212
- RocheAFSievogelRMChumleaWCGrading body fatness from limited anthropometric dataAm J Clin Nutr198134283187315784
- RodriguezGMorenoLABlayMGBody composition in adolescents: measurements and metabolic aspectsInt J Obes Relat Metab Disord200428Suppl 3S54815543220
- RosnerBPrineasRDanielsSRBlood pressure differences between blacks and whites in relation to body size among US children and adolescentsAm J Epidemiol200015110071910853640
- SeidellJCOosterleeADeurenbergPAbdominal fat depots measured with computed tomography: effects of degree of obesity, sex, and ageEur J Clin Nutr198842805153181112
- SinhaRFischGTeagueBPrevalence of impaired glucose tolerance among children and adolescents with marked obesityN Engl J Med20023468021011893791
- SrinivasanSRBaoWWattigneyWAAdolescent overweight is associated with adult overweight and related multiple cardiovascular risk factors: the Bogalusa Heart StudyMetabolism199645235408596496
- SrinivasanSRFreedmanDSWebberLSBlack-white differences in cholesterol levels of serum high-density lipoprotein subclasses among children: the Bogalusa Heart StudyCirculation19877627293608116
- SrinivasanSRMyersLBerensonGSDistribution and correlates of non-high-density lipoprotein cholesterol in children: the Bogalusa Heart StudyPediatrics2002110e2912205279
- StanfordAGlascockJMEidGMLaparoscopic Roux-en-Y gastric bypass in morbidly obese adolescentsJ Pediatr Surg200338430312632362
- StolleyMRFitzgibbonMLEffects of an obesity prevention program on the eating behavior of African American mothers and daughtersHealth Educ Behav199724152649079575
- StraussRSPollackHAEpidemic increase in childhood overweight, 1986–1998JAMA20012862845811735760
- SugermanHJSugermanELDemariaEJBariatric surgery for severely obese adolescentsJ Gastrointest Surg200371027 discussion 107-812559191
- SummerbellCWatersEEdmundsLInterventions for preventing obesity in childrenCochrane Database Syst Rev2005CD00187116034868
- TakemuraYKikuchiSInabaYThe protective effect of good physical fitness when young on the risk of impaired glucose tolerance when oldPrev Med19992814199973583
- TeixeiraPJSardinhaLBGoingSBTotal and regional fat and serum cardiovascular disease risk factors in lean and obese children and adolescentsObes Res200194324211500523
- TelamaRYangXViikariJPhysical activity from childhood to adulthood: a 21-year tracking studyAm J Prev Med2005282677315766614
- TjepkemaMShieldsMNutrition: findings from the Canadian Community Health Survey – overweight Canadian children and adolescents2004Statistics Canada
- TolfreyKCampbellIGJonesAMSelected predictor variables and the lipid-lipoprotein profile of prepubertal girls and boysMed Sci Sports Exer19993115507
- TremblayMSKatzmarzykPTWillmsJDTemporal trends in overweight and obesity in Canada, 1981–1996Int J Obes Relat Metab Disord2002265384312075581
- TwiskJWKemperHCVan MechelenWPrediction of cardiovascular disease risk factors later in life by physical activity and physical fitness in youth: general comments and conclusionsInt J Sports Med200223Suppl 1S44912012262
- Van GaalLFWautersMADe LeeuwIHAnti-obesity drugs: what does sibutramine offer? An analysis of its potential contribution to obesity treatmentExp Clin Endocrinol Diabetes1998106Suppl 235409792480
- Van ItallieTBHealth implications of overweight and obesity in the United StatesAnn Intern Med198510398384062130
- WannametheeSGShaperAGWeight change and duration of overweight and obesity in the incidence of type 2 diabetesDiabetes Care19992212667210480769
- WebberLSHarshaDWPhillipsGTCardiovascular risk factors in Hispanic, white, and black children: the Brooks County and Bogalusa Heart studiesAm J Epidemiol1991133704142018025
- WeissRDziuraJBurgertTSObesity and the metabolic syndrome in children and adolescentsN Engl J Med200435023627415175438
- WeissRTaksaliSETamborlaneWVPredictors of changes in glucose tolerance status in obese youthDiabetes Care200528902915793193
- WhitakerRCWrightJAPepeMSPredicting obesity in young adulthood from childhood and parental obesityN Engl J Med1997337869739302300
- WidhalmKDietrichSPragerGAdjustable gastric banding surgery in morbidly obese adolescents: experiences with eight patientsInt J Obes Relat Metab Disord200428Suppl 3S42515543218
- [WHO] World Health OrganizationObesity: preventing and managing the global obesity epidemic1997Geneva
- ZannolliRMorgeseGWaist percentiles: a simple test for atherogenic disease?Acta Paediatr199685136898955469