Abstract
Objective
Diagnosis of pulmonary embolism (PE) remains difficult and is often missed in the elderly due to nonspecific and atypical presentation. Diagnostic algorithms able to rule out PE and validated in young adult patients may have reduced applicability in elderly patients, which increases the number of diagnostic tools use and costs. The aim of the present study was to analyze the reported clinical presentation of PE in patients aged 65 and more.
Materials and Methods
Prospective and retrospective English language studies dealing with the clinical, instrumental and laboratory aspects of PE in patients more than 65 and published after January 1987 and indexed in MEDLINE using keywords as pulmonary embolism, elderly, old, venous thromboembolism (VTE) in the title, abstract or text, were reviewed.
Results
Dyspnea (range 59%–91.5%), tachypnea (46%–74%), tachycardia (29%–76%), and chest pain (26%–57%) represented the most common clinical symptoms and signs. Bed rest was the most frequent risk factor for VTE (15%–67%); deep vein thrombosis was detected in 15%–50% of cases. Sinus tachycardia, right bundle branch block, and ST-T abnormalities were the most frequent ECG findings. Abnormalities of chest X-ray varied (less than 50% in one-half of the studies and more than 70% in the other one-half). Arterial blood gas analysis revealed severe hypoxemia and mild hypocapnia as the main findings. D-Dimer was higher than cut-off in 100% of patients in 75% of studies. Clinical usefulness of D-Dimer measurement decreases with age, although the strategies based on D-Dimer seem to be cost-effective at least until 80 years.
Conclusion
Despite limitations due to pooling data of heterogeneous studies, our review could contribute to the knowledge of the presentation of PE in the elderly with its diagnostic difficulties. A diagnostic strategy based on reviewed data is proposed.
Introduction
Despite modern guidelines, ruling out or diagnosing pulmonary embolism (PE) represents one of the main medical problem in clinical geriatric practice (Rogers 2007). PE remains in fact an under-diagnosed disease in old people, even though its incidence, prevalence, morbidity, and mortality increase steadily with age (CitationKniffin et al 1994; CitationHansson et al 1997; CitationSilverstein et al 1998; CitationGoldhaber et al 1999; Heit et al 1999; CitationWhite 2003; CitationStein et al 2004). It has been reported that PE represented the main cause of death that is less suspected by physicians in the elderly (CitationLeibovitz et al 2001). About 40% of PE found at necropsy in older persons were not suspected ante mortem (CitationLeibovitz et al 2001).
The diagnostic process of PE starts from clinical suspicion both in young adults and in elderly patients (CitationTapson et al 1999; CitationESC 2000; CitationACEP 2003; CitationBTS 2003; CitationGoldhaber and Elliott 2003; CitationStein et al 2006). Assessment of clinical probability represents the first step to reach a prompt diagnosis of PE and to prevent delays in the diagnostic work-up and initiation of appropriate treatment. Assessment of clinical probability derives from an integration of history, analysis of risk factors for venous thromboembolism (VTE), symptoms and signs with first level investigations such as systolic blood pressure, 12-leads electrocardiography (ECG), chest X-ray, and arterial blood gas analysis (ABG). Clinical pre-test probability (PTP) should be evaluated by using one of the available and validated score, such as the Wells’ score or the Geneva score (CitationWells et al 1998; CitationTapson et al 1999; CitationESC 2000; CitationACEP 2003; CitationBTS 2003; CitationGoldhaber and Elliott 2003; CitationLe Gal et al 2006; CitationStein et al 2006). After assessment of clinical probability, D-Dimer measurement is often the next proposed step in diagnostic strategies for suspected PE (CitationStein et al 2004). However, D-Dimer assay should be performed only in nonhigh PTP (low or moderate PTP) (CitationBTS 2003). PE may be ruled out when nonhigh PTP is associated to negative D-Dimer (<500 μg/L) (CitationTapson et al 1999; CitationESC 2000; CitationACEP 2003; CitationBTS 2003; CitationGoldhaber and Elliott 2003; CitationPerrier et al 2005; CitationChristopher Study Investigators 2006; CitationStein et al 2006). In the other cases, PE should be confirmed with helical pulmonary angio-computer tomography (angio-CT), preferably multidetector type, lung scan or pulmonary angiography (CitationTapson et al 1999; CitationESC 2000; CitationACEP 2003; CitationBTS 2003; CitationGoldhaber and Elliott 2003; CitationStein et al 2006). The use of lung scan for confirming PE has been reduced because of the major availability of helical angio-CT, and in reason of the important proportion of inconclusive lung scan, in particular in elderly patients. Legs ultrasonography is noninvasive, and is able to detect deep vein thrombosis (DVT). The presence of a recent DVT is enough to rule in the diagnosis of PE and DVT and start anticoagulation (CitationLe Gal et al 2006). Combination of PTP with different levels of D-Dimer could reduce the number of unnecessary legs ultrasonography for ruling out DVT in patients with symptomatic PE (CitationYamaki et al 2007). Trans thoracic echocardiogram (TTE), is particularly useful in suspected massive PE, when unstability of patient precludes complicated diagnostic algorithms. Moreover it could offer information for prognosis stratification and aid the choice of treatment, as biomarkers (B natriuretic peptides and cardiac troponins) (CitationTapson et al 1999; CitationESC 2000; CitationGoldhaber 2002; CitationACEP 2003; CitationBTS 2003; CitationGoldhaber and Elliott 2003; CitationKucher et al 2003; CitationPieralli et al 2006; CitationStein et al 2006; CitationBecattini et al 2007).
Since the evidence showed difficulties in diagnosing of PE in the elderly, the clinical, instrumental and laboratory presentation of PE in elderly patients are reviewed in the present article.
Sources were obtained from articles indexed in MEDLINE database from January 1987 to August 2007 searching terms “pulmonary embolism”, “elderly”, “old”, “venous thromboembolism” in the title, abstract and/or text. Additional references were identified by reviewing the bibliographies of retrieved articles. Only prospective and retrospective English language studies dealing with the clinical, instrumental and/or laboratory presentation of PE patients aged more than 65 years were considered for the review. Studies were included if they reported patients with confirmed PE. We did not perform a systematic review, but we reported data of more relevant articles.
Results
Symptoms, risk factors of VTE, first line instrumental examinations, and arterial blood gas analysis (ABG)
These data derived from twelve selected articles (CitationBusby et al 1988; CitationStein et al 1991; CitationJones et al 1993; CitationGisselbrcht et al 1996; CitationMasotti et al 2000; CitationRamos et al 2000; CitationCeccarelli et al 2003; CitationTimmons et al 2003; CitationKokturk et al 2005; CitationLe Gal et al 2005; CitationPunukollu et al 2005; CitationChung et al 2006). From ten of them, we derived data for acute mortality, symptoms, signs and risk factors for VTE (CitationBusby et al 1988; CitationStein et al 1991; CitationGisselbrcht et al 1996; CitationMasotti et al 2000; CitationRamos et al 2000; CitationCeccarelli et al 2003; CitationTimmons et al 2003; CitationKokturk et al 2005; CitationLe Gal et al 2005; CitationPunukollu et al 2005); from seven articles we derived data for 12-leads ECG (CitationStein et al 1991; CitationMasotti et al 2000; CitationRamos et al 2000; CitationCeccarelli et al 2003; CitationTimmons et al 2003; CitationKokturk et al 2005), from six data for chest X-ray (CitationBusby et al 1988; CitationStein et al 1991; CitationMasotti et al 2000; CitationRamos et al 2000; CitationCeccarelli et al 2003; CitationLe Gal et al 2005), from four data for TTE and from seven data for ABG (CitationStein et al 1991; CitationJones et al 1993; CitationGisselbrcht et al 1996; CitationMasotti et al 2000; CitationRamos et al 2000; CitationCeccarelli et al 2003; CitationKokturk et al 2005).
Dyspnea (range 59%–91.5%), tachypnea (46%–74%), tachycardia (29%–76%), and chest pain (range 26%–59%) represented the main symptoms reported in clinical studies about PE in the elderly. Bed rest (range 15%–67%) and DVT (range 15%–50%) were the main risk factors for VTE ().
Table 1 Main clinical aspects of elderly patients with PE
Sinus tachycardia (range 18%–62.5%), right bundle branch block (4.5%–40.5%) and ST-T abnormalities (9%–37%) were the most represented 12-leads-ECG findings; the typical S1Q3/S1Q3T3 ECG pattern was found in 4.5%–14% of patients.
Three studies reported abnormalities in less of one half of patients at chest X-ray (CitationBusby et al 1988; CitationRamos et al 2000; CitationLe Gal et al 2005) while in other three studies more than 70% of patients had abnormalities (CitationStein et al 1991; CitationMasotti et al 2000; CitationCeccarelli et al 2003). Cardiomegaly (range 22%–64%), pleural effusion (15.8%–57%), and (8.5%–71%) were the most frequent reported aspects. More than 50% of patients had features of right heart overload at TTE (CitationMasotti et al 2000; CitationCeccarelli et al 2003; CitationKokturk et al 2005; CitationChung et al 2006).
A severe hypoxemic respiratory failure was found as main ABG pattern. In five studies, this pattern was associated to low arterial carbon dioxide partial pressure (PaCO2). In three studies the alveolar-arterial oxygen gradient, D(A-a)O2, was analyzed (CitationJones et al 1993; CitationMasotti et al 2000; CitationCeccarelli et al 2003), and was found to be elevated (range 44.8–46.6 mmHg).
summarizes the first line instrumental findings.
Table 2 12-leads electrocardiography, chest X-ray, arterial blood gas analysis findings 12-leads ECG
Pre-test clinical probability and D-Dimer
Two studies have analyzed the field of applicability of PTP combined with D-Dimer for ruling out PE in the elderly (CitationRighini et al 2004; CitationSöhne et al 2005). These studies have reported that the percentage of high PTP increases in elderly compared to younger patients, whereas the percentage of low PTP decreases. One study suggested that Geneva score seemed to perform better in elderly patients compared to Wells score (CitationRighini et al 2004). One of these studies has demonstrated that the sensitivity and negative predictive value of a combination of low PTP and negative D-Dimer were high in elderly patients. Unfortunately the prevalence of elderly having the association non high PTP-negative D-Dimer is low (14% of age over than 75 years) (Sühne et al 2005). However a strategy combining PTP and D-Dimer is still cost-effectiveness at least until 80 years (CitationRighini et al 2007).
The specificity of D-Dimer in patients with suspected PE decreases steady with age. One study has demonstrated that the specificity of ELISA D-Dimer (VIDAS, Biomerieux, France) in suspected VTE reduces from 70.5% in patients under 40 years to 4.5% in patients over 80 years (CitationHarper et al 2007). Similar specificity (5%) was found in another study in patients over 80 years with nonhigh PTP by using the same ELISA D-Dimer method (CitationRighini et al 2000). The very low specificity of D-Dimer in the elderly has led to suggest an increased cut-off value of D-Dimer. Two series have concluded that an increased cut-off of D-Dimer reduced the false positives but increased the percentage of false negatives. Conversely, another study has demonstrated that increasing the cut-off from 500 microg/L to 750 microg/L and 1000 microg/L, led to a rise in D-Dimer specificity in patients over 80 years (from 4.5% to 13.1% and 27.3%, respectively) without loss of sensibility (CitationAguilar et al 2001; CitationRighini et al 2001; CitationHarper et al 2007).
One study (CitationMasotti et al 2000) has shown that 86% of patients with PE had D-Dimer >500 μg/L measured with latex agglutination. In another study D-Dimer, measured by immunoturbidimetric method, was over the cut-off value in 98.5% of patients (Sühne et al 2005). Four studies demonstrated that all patients (100%) had D-Dimer values higher than cut-off (CitationTardy et al 1998; CitationBarro et al 1999; CitationMasotti et al 2000; CitationCeccarelli et al 2003).
Instrumental examinations for confirming PE
Two studies have analyzed the effect of age on the diagnostic performance of helical angio-CT to diagnose PE. Either by single detector or multidetector helical pulmonary angio-CT, the sensitivity, specificity, positive, and negative predictive values are not influenced by age, making applicable and safe the diagnostic strategies based on these investigations (CitationRighini et al 2004; CitationStein et al 2007).
In selected elderly patients without previous cardiopulmonary diseases ventilation/perfusion (V/Q) lung scan has similar applicability in the elderly compared with younger patients (CitationStein et al 1996). In unselected patients, rate of non diagnostic lung scan is higher in elderly patients (CitationCalvo-Romero et al 2005). The diagnostic yield of lung scan decreases from 68% in patients under 40 years to 42% in the patients aged 80 years and older (CitationRighini et al 2000).
Sensitivity of legs ultrasonography for detection of DVT increase with age, whereas specificity does not change with age, close to 100% (CitationRighini et al 2000).
Sensitivity and specificity of pulmonary angiography remain similar to young adults but this procedure could be limited by higher risk of acute renal failure due to iodinate contrast (CitationStein et al 1991).
A recent meta-analysis on prognostic values of cardiac troponins has shown that elevated levels of troponins identify high risk patients for death and adverse outcomes, even though in the studies concerning patients with mean age ≥65 years. (CitationGiannitsis et al 2000; CitationEnea et al 2004; CitationHsu et al 2006; CitationKaczynska et al 2006; CitationBecattini et al 2007). One study has evaluated the prognostic role of BNP in the elderly, and concluded that this biomarker was not a solid indicator of complicated PE (CitationRay et al 2006).
Discussion and implications for clinical practice
The two crucial questions about PE in the elderly are: in which patients should PE be suspected and searched for, and which diagnostic procedures and algorithms could be safely performed.
PE represents one of the main causes of acute respiratory failure (ARF) in the elderly patients. In a recent observational study on 514 elderly patients with ARF, 18% of them had confirmed PE. An inappropriate initial treatment due to uncorrected diagnosis was associated to an increased mortality (CitationRay et al 2006). PE was one of the main causes incorrectly diagnosed (CitationRay et al 2006).
In elderly patients, making the difference between PE symptoms and other cardio-respiratory diseases such as congestive heart failure, pneumonia and/or COPD (chronic obstructive pulmonary disease) exacerbation could be very challenging because of the frequent similar clinical picture and coexistence of diseases (CitationRay et al 2006). As shown in the present study, the most frequent symptoms and signs of confirmed PE in elderly patients are dyspnea, tachypnea, tachycardia, and chest pain. All these symptoms and signs are nonspecific and similar to that of PE in younger patients (CitationPIOPED Investigators 1990; CitationMiniati et al 1996; CitationGoldhaber et al 1999). Chest pain seem to be less frequent and tachycardia and syncope more frequent in the elderly compared with nonelderly patients (CitationBusby et al 1988; CitationStein et al 1991; CitationGisselbrcht et al 1996; CitationKokturk et al 2005; CitationPunukollu et al 2005). Bed rest is the most frequent risk factors for PE in the elderly, together with surgery and cancer. Evident implication is that primary prophylaxis using mechanical or pharmacological measures should be carefully evaluated in elderly bedridden patients. (CitationPIOPED Investigators 1990; CitationMiniati et al 1996; CitationGoldhaber et al 1999).
The specificity of instrumental and laboratory examinations is low both in elderly and nonelderly patients: 12-leads-ECG, chest X-ray, and ABG do not increase the suspicion of PE in the elderly.
ABG could reveal an hypoxemic respiratory failure associated to normal or mildly reduced PaCO2 and increased D(A-a)O2 similarly to congestive heart failure and pneumonia. It should be kept in mind that in two studies enrolling patients with previous cardio-pulmonary diseases, mean values of PaCO2 were in normal range. Only one third of patients had respiratory alkalosis (CitationMasotti et al 2000; CitationCeccarelli et al 2003), suggesting an impaired response to acute stress in elderly patients. Compared with younger patients, ABG in elderly patients seems to reveal lower hypoxemia and higher values of alveolar-arterial oxygen gradient (CitationPIOPED Investigators 1990).
The role of D-Dimer is well recognized to rule out PE when it is negative and associated to a non-high PTP. However, the specificity and the clinical usefulness of D-Dimer decrease with age because of high percentage of elderly patients with D-Dimer higher than cut-off. Unfortunately increasing cut-off of D-Dimer could lead to increase the percentage of patients wrongly considered negatives, and is therefore considered unsafe.
Recently, the first diagnostic algorithm, not validated, for suspected PE in the elderly has been reported (CitationRighini et al 2005). The most important findings of this diagnostic strategy are represented by the non invasivity of first-line investigation (PTP evaluation, and legs ultrasonography), and angio-CT as confirming examination. In this algorithm D-Dimer is not widely recommended; its assay should be reserved to selected conditions (limited availability of other diagnostic tests or presence of high risk of adverse reactions due to instrumental examinations with contrast). However, more recently the same Authors demonstrated that in elderly outpatients the strategies based on PTP evaluation, and D-Dimer assay are cost-effectiveness at least until 80 years and that strategies with legs ultrasonography are more expensive but not safer. Therefore, measuring D-dimer in outpatients more than 80 years may be differently appreciated. On one side, one could argue that the clinical usefulness is so limited that D-dimer measurement is not indicated. On the other side, D-dimer measurement does not increase the costs of diagnostic strategies. To avoid complicated recommendations or age-adapted diagnostic strategies (for example not dosing D-dimer in elderly patients), a systematic measurement may be proposed, at least in outpatients. Moreover, D-dimer might still be justified in patients above 80 years when the availability of other diagnostic tests is limited or when the risk of imaging using hCT is higher because of impaired renal function.
Helical pulmonary angio-CT should be encouraged in the elderly since it has been proved to be safe and accurate in the oldest and since lung scan has limited accuracy in this subset of patients. (CitationStein et al 1996; CitationRighini et al 2000, Citation2004; CitationCalvo-Romero et al 2005; CitationStein et al 2007).
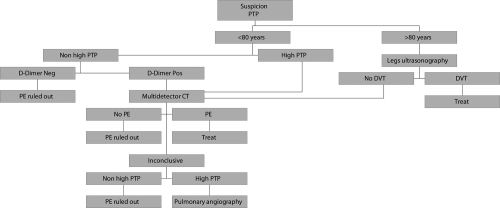
shows an algorithm for elderly patients with suspected PE derived from the most recent evidence of literature.
Figure 1 Diagnostic algorithm for elderly patients with suspected PE derived from literature evidence.
Limits of the study
We are aware of some limitations of our review. First we pooled data from heterogeneous studies with different methodology. This review was not systematic and could be scientifically subjected to criticism. Studies about diagnostic strategy for diagnosing PE in the elderly are lacking, and our conclusions are based upon small series. summarizes the implications of this review in the clinical practice.
Table 3 Implications for clinical geriatric practice
Conclusion
PE is a potentially life-threatening condition, difficult to diagnose in elderly patients. Misdiagnosis is more frequent in the elderly patients Clinical signs of PE are neither sensitive nor specific enough to rule in or out the diagnosis. Our review suggests that PE should be suspected in any elderly patient at risk with unexplained dyspnea, tachypnea, or tachycardia. However these findings are highly nonspecific, which reduces the diagnostic value.
References
- [ACEP] American College of Emergency Physicians Clinical Policies Committee; Clinical Policies Committee Subcommittee on Suspected Pulmonary EmbolismClinical policy: critical issues in the evaluation and management of adult patients presenting with suspected pulmonary embolismAnn Emerg Med2003412577012548278
- AguilarCMartinezAMartinezADiagnosis of deep vein thrombosis in the elderly: a higher D-Dimer cut-off value is better?Haematologica200186E2811602435
- BarroCBossonJLPernodGD-Dimer testing improves the management of thromboembolic disease in hospitalized patientsThrob Res1999952639
- BecattiniCAgnelliGAcute pulmonary embolism: risk stratification in the emergency departmentIntern Emerg Med200721192917619833
- BecattiniCVedovatiMCAgnelliGPrognostic value of troponins in acute pulmonary embolism. A meta-analysisCirculation20071164273317606843
- [BTS] British Thoracic SocietyBritish Thoracic Society guidelines for the management of suspected acute pulmonary embolismThorax2003584708412775856
- BusbyWBayerAPathyJPulmonary embolism in he elderlyAge Ageing19881720593389249
- Calvo-RomeroJMLima-RodriguezBMBureo-DacalPPredictors of an intermediate ventilation/perfusion lung scan in patients with suspected pulmonary embolismEur J Emerg Med2005121293115891446
- CeccarelliEMasottiLBarabesiLPulmonary embolism in very old patientsAging Clin Exp Res2003151172212889842
- ChungTEmmettLKhouryVAtrial and ventricular echocardiographic correlates of the extent of pulmonary embolism in the elderlyJ Am Soc Echocardiogr2006193475316500500
- EneaICeparanoGMazzarellaGBiohumoral markers and right ventricular dysfunction in acute pulmonary embolism: the answer to thrombolytic therapyItal Heart J Suppl20045293515253142
- [ESC] ESC Task ForceGuidelines on diagnosis and management of acute pulmonary embolismEur Heart J20002113013610952823
- GiannitsisEMuller-BardoffMKurowskiVIndependent prognostic value of cardiac troponin T in patients with confirmed pulmonary embolismCirculation20001022111710889133
- GisselbrchtMDiehlJMeyerGClinical presentation and results of thrombolytic therapy in older patients with massive pulmonary embolism: a comparison with non-elderly patientsJ Am Geriatr Soc199644189938576511
- GoldhaberSZElliottCGAcute pulmonary embolism: part I. Epidemiology, pathophysiology, and diagnosisCirculation20031082726914656907
- GoldhaberSZVisaniLDe RoseMfor ICOPERAcute pulmonary embolism: clinical outcomes in the International Cooperative Pulmonary Embolism Registry (ICOPER)Lancet19993531386910227218
- GoldhaberSZEchocardiography in the management of pulmonary embolismAnn Intern Med200213669170011992305
- HanssonPOWelinLTibblinGDeep vein thrombosis and pulmonary embolism in the general population. The study of men born in 1913Arch Intern Med19971571665709250227
- HarperPLTheakstoneEAhmedJD-Dimer concentration increases with age reducing the clinical value of the D-Dimer assay in the elderlyIntern Med J2007376071317543005
- HeitJASilversteinMDMohrDNPredictors of survival after deep vein thrombosis and pulmonary embolism. A population-based cohort studyArch Intern Med1594455310074952
- HsuJTChuCMChangSTPrognostic role of right ventricular dilatation and troponin I elevation in acute pulmonary embolismInt Heart J2006477758117106148
- JonesJSVanDeelenNWhiteLAlveolar-arterial oxygen gradient in elderly patients with suspected pulmonary embolismAnn Emerg Med1993221177818517570
- KaczynskaAPelsersMMBochowiczAPlasma heart-type fatty acid binding protein is superior to troponin and myoglobin for rapid risk stratification in acute pulmonary embolismClin Chim Acta200637111712316698008
- KniffinWDJrBaronJABarrettJThe epidemiology of diagnosed pulmonary embolism and deep venous thrombosis in the elderlyArch Intern Med199415486168154949
- KokturkNOguzulgenIKDemirNDifferences in clinical presentation of pulmonary embolism in older vs younger patientsCirc J200569981616041171
- KucherNWallmannDCaroneAIncremental prognostic value of troponin I and echocardiography in patients with acute pulmonary embolismEur Heart J2003241651614499227
- Le GalGRighiniMRoyPMDifferential value of risk factors and clinical signs for diagnosing pulmonary embolism according to ageJ Thromb Haemost2005324576416241944
- Le GalGRighiniMRoyPMPrediction of pulmonary embolism in the emergency department: the revised Geneva scoreAnn Intern Med20061441657116461960
- LeibovitzABlumenfeldOBaumoehlYPostmortem examinations in patients of a geriatric hospitalAging Clin Exp Res2001134069
- MasottiLCeccarelliECappelliRPlasma D-Dimer levels in elderly patients with suspected pulmonary embolismThromb Res200098577910907939
- MasottiLCeccarelliECappelliRPulmonary embolism in the elderly: clinical, instrumental and laboratori aspectsGerontology2000462051110859460
- MiniatiMPistolesiMMariniCValue of perfusion lung scan in the diagnosis of pulmonary embolism: results of Prospective Investigative Study of Acute Pulmonary Embolism Diagnosis (PISA-PED)Am J Critic Care Med1996154138793
- PerrierARoyPMSanchezOMultidetector-row computed tomography in suspected pulmonary embolismN Eng J Med200535217608
- PieralliFOlivottoIVanniSUsefulness of bed-side testing for brain natriuretic peptide to identify right ventricular dysfunction and outcome in normotensive patients with acute pulmonary embolismAm J Cardiol20069713869016635617
- PunukolluHKhanIAPunukolluGAcute pulmonary embolism in elderly: clinical characteristics and outcomeInt J Cardiol2005992131615749178
- RamosAMurillasJMasciasCInfluence of age on clinical presentation of acute pulmonary embolismArch Gerontol Geriat20003018998
- RayPBirolleauuSLefortYAcute respiratory failure in the elderly: etiology, emergency diagnosis and prognosisCrit Care200610R8216723034
- RayPMaziereFMedimaghSEvaluation of B-type natriuretic peptide to predict complicated pulmonary embolism in patients aged 65 years and older: brief reportAm J Emerg Med200624603716938601
- RighiniMBounemeauxHPerrierAEffect of age on the performance of single detector helical computer tomography in suspected pulmonary embolismThromb Haemost200491296914961157
- RighiniMde MoerloosePReberGShould the D-Dimer cut off value be increased in elderly patients suspected of pulmonary embolism?Thromb Haemost20018574411341515
- RighiniMGoehringCBounameauxHEffect of age on the performance of common diagnostic tests for pulmonary embolismAm J Med20001093576111020391
- RighiniMLe GalGPerrierAEffect of age on the assessment of clinical probability of pulmonary embolism by prediction rulesJ Thromb Haemost200421206815219218
- RighiniMLe GalGTerrierAThe challenge of diagnosing pulmonary embolism in elderly patients: influence of age in commonly used diagnostic tests and strategiesJ Am Geriatr Soc20055310394415935031
- RighiniMNendazMLe GalGInfluence of age on the cost-effectiveness of diagnostic strategies for suspected pulmonary embolismJ Thromb Haemost2007518697717596141
- RogersRLVenous thromboembolic disease in the elderly patients: atypical, subtle, and enigmaticClin Geriatr Med234132317462526
- SilversteinMDHeitJAMohrDNTrends in the incidence of deep vein thrombosis and pulmonary embolism. A 25-years population-based studyArch Intern Med1998158585939521222
- SöhneMKamphuisenPWvan MierloPJDiagnostic strategy using a modified clinical decision rule and D-Dimer test to rule out pulmonary embolism in elderly in- and outpatientsThromb Haemost2005942061016113805
- SteinPDBeemathAQuinnDAUsefulness of multidetector spiral computed tomography according to age and gender for diagnosis of acute pulmonary embolismAm J Cardiol2007991303517478162
- SteinPDGottschalkASaltzmanHADiagnosis of acute pulmonary embolism in the elderlyJ Am Coll Cardiol199118145271939945
- SteinPDHenryJWRelyeaBElderly patients with no prior cardiopulmonary disease show ventilation/perfusion lung scan characteristics that are sensitive and specific for pulmonary embolismAm J Geriatr Cardiol19965364011416400
- SteinPDHullRDKayaliFVenous thromboembolism according to age: the impact of an aging populationArch Intern Med20041642260515534164
- SteinPDHullRDPatelKCD-Dimer for the exclusion of acute venous thrombosis and pulmonary embolism. A systematic reviewAnn Intern Med200414058960215096330
- SteinPDWoodardPKWegJGDiagnostic pathways in acute pulmonary embolism: recommendations of the PIOPED II investigatorsAm J Med200611910485517145249
- TapsonVFCarrollBADavidsonBLThe diagnostic approach to acute venous thromboembolism. Clinical practice guideline. American Thoracic SocietyAm J Respir Crit Care Med199916010436610471639
- TardyBTardy-PancetBViallonAEvaluation of D-Dimer ELISA test in elderly patients with suspected pulmonary embolismThromb Haemost19987938419459319
- The PIOPED InvestigatorsValue of the ventilation/perfusion scan in acute pulmonary embolism. Results of the Prospective Investigation of Pulmonary Embolism Diagnosis (PIOPED)JAMA19902632753592332918
- TimmonsSKingstonMHussanMPulmonary embolism: differences in presentation between older and younger patientsAge Ageing200332601514600000
- WellsPSGinsbergJSAndersonDRUse of a clinical model for safe management of patients with suspected pulmonary embolismArch Intern Med19981299971005
- WhiteRHThe epidemiology of venous thromboembolismCirculation2003107Suppl 1I41812814979
- Writing Group for Christopher Study InvestigatorsEffectiveness of managing suspected pulmonary embolism using an algorithm combining clinical probability, D-dimer testing, and computer tomographyJAMA2006295172916403929
- YamakiTNozakiMSakuraiHUses of different D-dimer levels can reduce the need for venous duplex scanning to rule out deep vein thrombosis in patients with symptomatic pulmonary embolismJ Vasc Surg2007465263217826240