Abstract
Sildenafil is a selective inhibitor of phosphodiesterase type 5 (PDE-5). Its chronic administration has been shown to improve exercise capacity, World Health Organization functional class, and haemodynamics in patients with symptomatic pulmonary arterial hypertension (PAH). There is however, no data describing the clinical consequences of sudden cessation of sildenafil treatment. In this series, 9 patients with NYHA Class II–IV PAH who were stable on 2 months of sildenafil monotherapy, had their sildenafil ceased to accommodate a 2-week washout period, required for enrollment in research involving an endothelin receptor antagonist. Six minute walk distance (SMWD) and clinical assessments were performed before cessation of sildenafil, and again 2 weeks later. Over the course of this 2-week washout period, 6 of the 9 patients reported increased breathlessness and fatigue, 1 of these was hospitalized with worsening right heart failure. The SMWD fell in 6 patients, with falls of greater than 100 m recorded in 4 patients. This was accompanied by a worsening of NYHA Class from 2.5 ± 0.2 to 3.1 ± 0.1 (mean ± SEM, p = 0.01). These data indicate that sudden cessation of sildenafil monotherapy, in patients with PAH, carries with it a significant and unpredictable risk of rapid clinical deterioration. We recommend that if sildenafil needs to be ceased, it would be more prudent to consider concurrent vasodilator therapy before the gradual cessation of sildenafil.
Introduction
Sildenafil is a selective inhibitor of phosphodiesterase type 5 (PDE-5). This is the predominant phosphodiesterase isoform in the lungs (CitationRabe et al 1994). Sildenafil inhibits the breakdown of cGMP, and enhances the ability of endothelial nitric oxide to vasodilate the pulmonary arteries, reducing intravascular calcium, relaxing smooth muscle cells and reducing pulmonary vascular resistance (PVR) (CitationCorbin et al 1999).
Acutely administered sildenafil assists weaning from nitric oxide (CitationAtz and Wessel 1999), prolongs the effect of inhaled iloprost (CitationWilkens et al 2001; CitationGhofrani et al 2002), reduces mean pulmonary artery pressure (MPAP) and PVR in the post heart transplant setting (CitationKulkarni et al 2004; CitationJabbour et al 2007), enhances the reduction in PVR when used concomitantly with iNO (CitationMichelakis et al 2002; CitationLepore et al 2002) and modifies pulmonary arterial hypertension (PAH) secondary to acute hypoxia in normal volunteers (CitationZhao et al 2001). Chronic administration of sildenafil has been shown to improve exercise capacity, WHO functional class, and haemodynamics in patients with symptomatic PAH (CitationGalie et al 2005). Similarly, hemodynamic and functional benefit has been demonstrated in a small group of patients with PAH secondary to chronic thromboembolic disease (CitationSheth et al 2005). It is now established as a treatment for pulmonary hypertension in these patients. Though extensive data exist regarding the safety and efficacy of sildenafil therapy in PAH, there are no data describing the clinical consequences of sudden cessation of sildenafil treatment.
Methods
In this series, 9 patients with NYHA Class II-IV PAH who were stable after 2 months of sildenafil monotherapy 50mg, 4 times daily were followed. This dose was chosen prior to the publication of research that demonstrated the efficacy of sildenafil 20 mg, 3 times daily in the treatment of PAH (CitationGalie et al 2005). The average age of patients was 42 ± 13 years and the male to female ratio 5:4. Five patients were NYHA Class II, 3 patients were NYHA Class III, and 1 patient was NYHA Class IV. Six patients had idiopathic PAH (iPAH) and 3 had chronic thromboembolic pulmonary hypertension (CTEPH).
Around this time a separate clinical trial of bosentan, an endothelin receptor antagonist was to commence. This trial required a 2-week washout period of previous PAH-specific therapy including sildenafil. Nine patients wished to participate in the bosentan study and had their sildenafil therapy ceased. In order to investigate the consequences of sildenafil cessation, six minute walk distance (SMWD) and clinical assessments were performed before cessation of sildenafil, and again 2 weeks after cessation, before commencing bosentan. The study was approved by the St Vincent’s Hospital Human Research Ethics Committee and no external financial support was received. Informed consent was given by all subjects. Importantly, there were no access arrangements for ongoing sildenafil use for PAH, either as monotherapy or combination therapy in Australia at the time of study.
Results
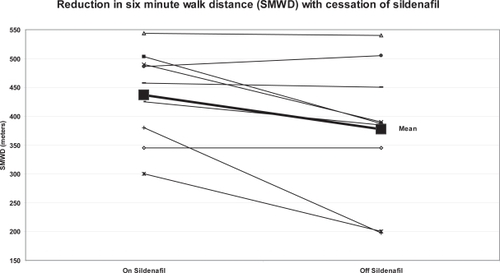
Over the course of this 2-week washout period 6 of the 9 patients reported increased breathlessness and fatigue, one was hospitalized with worsening right heart failure. The SMWD fell in 6 patients (3 with CTEPH and 3 with iPAH), with falls of greater than 100 m recorded in 4 patients (). This was accompanied by a worsening of NYHA Class from 2.5 ± 0.2 to 3.1 ± 0.1 (mean ± SEM, p = 0.01). Deterioration was unrelated to the initial NYHA Class on sildenafil. Fortunately, the condition of 4 of the 6 patients was stabilised with commencement of bosentan therapy. Two of the patients with CTEPH however, continued to deteriorate, one resumed sildenafil and her condition restabilized, the other went on to have a successful pulmonary thromboendarterectomy (PTE) 2 months later. Three patients reported no change in their symptoms which correlated with stable SMWD.
Discussion
These data indicate that sudden cessation of sildenafil monotherapy in patients with PAH carries with it a significant and unpredictable risk of rapid clinical deterioration. “Rebound” pulmonary hypertension, which has been reported after withdrawal from calcium-antagonists (CitationRich and McLaughlin 1999) and prostacyclin (CitationChannick et al 2001) refers to a worsening of PAH over and above what would be expected simply from the cessation of active treatment. To date, no such reports exist regarding sildenafil. The theory that sildenafil cessation may cause rebound PAH warrants further investigation with close hemodynamic monitoring, given the dramatic deterioration of the majority of patients in our series.
The ongoing deterioration of the 2 patients with CTEPH highlights another issue. Recent data presented at the European Society of Cardiology 2007 Congress by Lang and colleauges (BENEFiT Study subgroup analysis) demonstrated that bosentan improved hemodynamics but had no significant effect on exercise capacity (6MWD) in patients with inoperable CTEPH and those with post-pulmonary endarterectomy PAH. Research into the effectiveness of bosentan in treating the broader group of patients with CTEPH is ongoing. In our series, the restabilization of the two patients with CTEPH, after PTE and sildenafil therapy respectively, is consistent with current evidence-based management (CitationKlepetko et al 2004; CitationSheth et al 2005). It is important to note that this series observed patients over a period of unavoidable cessation of sildenafil monotherapy to gather valuable clinical information and was not designed to assess the effectiveness of bosentan therapy in rescuing patients off pulmonary vasodilator therapy.
In conclusion, we recommend that if sildenafil needs to be ceased, that clinicians and patients should be aware of the potential risk of deterioration and patients should be closely monitored during this period. It may be more prudent to consider concurrent vasodilator therapy before the gradual cessation of sildenafil.
Disclosure
The authors report no conflicts of interest in this work.
References
- AtzAMWesselDL1999Sildenafil ameliorates effects of inhaled nitric oxide withdrawalAnesthesiology913071010422958
- ChannickRNSimonneauGSitbonO2001Effects of the dual endothelin-receptor antagonist bosentan in patients with pulmonary hypertension: a randomised placebo-controlled studyLancet35811192311597664
- CorbinJDFrancisSH1999Cyclic GMP phosphodiesterase-5: target of sildenafilJ Biol Chem274137293210318772
- GalieNGhofraniHATorbickiA2005Sildenafil citrate therapy for pulmonary arterial hypertensionN Engl J Med35321485716291984
- GhofraniHAWiedemannRRoseF2002Combination therapy with oral sildenafil and inhaled iloprost for severe pulmonary hypertensionAnn Intern Med1365152211926786
- JabbourAKeoghAHaywardC2007Chronic sildenafil lowers transpulmonary gradient and improves cardiac output allowing successful heart transplantationEur J Heart Fail9674717347040
- KlepetkoWMayerESandovalJ2004Interventional and surgical modalities of treatment for pulmonary arterial hypertensionJ Am Coll Cardiol4373S8015194182
- KulkarniASinghTPSarnaikA2004Sildenafil for pulmonary hypertension after heart transplantationJ Heart Lung Transplant231441415607676
- LeporeJJMarooAPereiraNL2002Effect of sildenafil on the acute pulmonary vasodilator response to inhaled nitric oxide in adults with primary pulmonary hypertensionAm J Cardiol906778012231108
- MichelakisETymchakWLienD2002Oral sildenafil is an effective and specific pulmonary vasodilator in patients with pulmonary arterial hypertension: comparison with inhaled nitric oxideCirculation105239840312021227
- RabeKFTenorHDentG1994Identification of PDE isozymes in human pulmonary artery and effect of selective PDE inhibitorsAm J Physiol266L536437515580
- RichSMcLaughlinVV1999The effects of chronic prostacyclin therapy on cardiac output and symptoms in primary pulmonary hypertensionJ Am Coll Cardiol341184710520810
- ShethAParkJEOngYE2005Early haemodynamic benefit of sildenafil in patients with coexisting chronic thromboembolic pulmonary hypertension and left ventricular dysfunctionVascul Pharmacol4241515722248
- WilkensHGuthAKonigJ2001Effect of inhaled iloprost plus oral sildenafil in patients with primary pulmonary hypertensionCirculation10412182211551870
- ZhaoLMasonNAMorrellNW2001Sildenafil inhibits hypoxiainduced pulmonary hypertensionCirculation104424811468204